Abstract
Introduction:
The objective of the study was to evaluate the prevalence of dermatophytoses in human immunodeficiency virus (HIV) patients as well as to analyze the influence of CD4+ T-cell level in the Dermatology and STD Outpatient Department of Shadan Institute of Medical Sciences Teaching Hospital and Research Centre, Himayat sagar road, Hyderabad (Telangana state). The patients were tested for dermatophytic infections, as well as for the CD4+ T-cell counts. A total of 120 HIV-seropositive patients were included in this study, among which 38 were diagnosed of dermatophytosis. A majority of patients were in the 21–30 years’ age group. Tinea cruris was seen in majority of the cases, with Trichophyton rubrum being the most common culprit.
Background:
Cutaneous fungal infections have been reported worldwide as being one of the most common human infectious diseases in clinical practice. Dermatophytoses in individuals with HIV infection seem to manifest with atypical, multiple, or extensive lesions more frequently.
Aims:
The aim of this study was to determine the prevalence of dermatophytic infections among HIV-seropositive patients and their relation with CD4 count.
Materials and Methods:
This single-center prospective study was conducted in all HIV-seropositive patients (by double ELISA methods) who attended the Dermatology and STD Outpatient Department of Shadan Institute of Medical Sciences Teaching Hospital and Research Centre, Himayat sagar road, Hyderabad (Telangana state), from March 2015 to September 2016. They were screened for cutaneous fungal infections and those who tested positive were recruited for this study.
Results:
A total of 120 HIV-seropositive patients were included in this study, among which 38 were diagnosed of dermatophytosis. Most patients were in the 21–30 years’ age group. Tinea cruris was the most common variant, and T. rubrum was the most common offending pathogen. It was also found that the CD4+ T-cell count does not influence the occurrence of dermatophytoses.
Conclusion:
Superficial fungal infections are a common yet significant problem in HIV infection. They are characterized by the diversity of clinical aspects; the lesions are mostly caused by T. rubrum. It is essential that optimum treatment should be administered.
Keywords: Dermatophytes, human immunodeficiency virus, tinea cruris
INTRODUCTION
Cutaneous fungal infections have been reported worldwide as being one of the most common human infectious diseases in clinical practice. In spite of therapeutic advances in the last decades, the prevalence of cutaneous mycoses is still increasing. The skin constitutes the main site of recognizable fungal infections in humans.[1] Human immunodeficiency virus (HIV) infection is accompanied by increasing immunodeficiency, which increases the risk of various infectious diseases, including mycoses.[2]
Aim
The objective of the study was to evaluate the prevalence of dermatophytoses in HIV patients as well as to analyze the influence of CD4+ T-cell level.
MATERIALS AND METHODS
The study was conducted in all HIV-seropositive patients (by double ELISA methods) who attended the Dermatology and STD Outpatient Department from March 2015 to September 2016. They were screened for cutaneous fungal infections and those tested positive for dermatophytoses were recruited for this study.
A detailed history including marital and sexual histories was taken and the patients were subjected to a thorough physical examination, with particular reference to duration of the disease, site of involvement, and morphology of the lesions. The clinical diagnosis was supplemented with laboratory procedures such as microscopic examination (potassium hydroxide [KOH] preparation) and Gram-staining. Routine hematological, biochemical, and radiological investigations were performed to rule out systemic involvement wherever felt necessary. The patients were staged according to the Center for Disease Control and Prevention classification system for HIV infections (1986).[3] The cutaneous changes were recorded which correlated with various clinical parameters. Results were tabulated and analyzed.
RESULTS
A total of 120 HIV-seropositive patients were included in this study, among which 38 were diagnosed of dermatophytosis, with a prevalence of 31.66%. Out of the 38 cases, 28 were male and 10 were female patients, with a male-to-female ratio of 2.8:1.
Patients were divided into five age groups as follows: <20, 21–30, 31–40, 41–50, and >50 years of age. The largest number of patients in our study (20 [52.63%]) was in the 21–30 years’ age group followed by 31–40 years’ age group (21.05%), 41–50 years’ age group (13.15%), >50 years’ age group (7.89%), and <20 years’ age group (5.26%).
The ratio of male-to-female cases was 2.03:1.
Out of the males, 20 (71.42%) declared that they are heterosexuals, 2 (7.14%) are homosexuals, and 6 (21.42%) are bisexuals. In the female group, all the ten patients declared their heterosexuality.
The distribution of cases according to the site of lesion, i.e., according to clinical types, is tinea cruris in majority, i.e., 16 (42.10%) patients, followed by tinea corporis, i.e., 7 (18.42%) patients; tinea corporis with cruris, i.e., 6 (15.78%); tinea pedis, i.e., 3 (7.89%); tinea manuum and tinea unguium, i.e., 2 (5.26%) [Figure 1] each; and tinea faciei [Figure 2] and tinea capitis, i.e., 1 (2.63%) each [Table 1].
Figure 1.

Tinea unguium
Figure 2.

Tinea faciei
Table 1.
Distribution of cases according to site of involvement
![]()
Fungal elements (hyphae and/or arthrospores) could be demonstrated in scrapings from 33 out of the 38 cases (86.84%). Culture positivity was seen in 31 out of the 38 cases (81.57%) [Table 2]. Among the KOH-positive cases, culture positivity was seen in 31 cases (93.93%) and 2 cases were culture negative (6.06%). In all clinical patterns, Trichophyton rubrum (58.6%) [Figure 3] was the predominant species isolated followed by Trichophyton mentagrophytes (19.35%) [Figure 4], Trichophyton violaceum (12.90%), Microsporum audouinii (6.45%), and Microsporum canis (3.22%).
Table 2.
The species of dermatophytes isolated from various clinical sites
![]()
Figure 3.
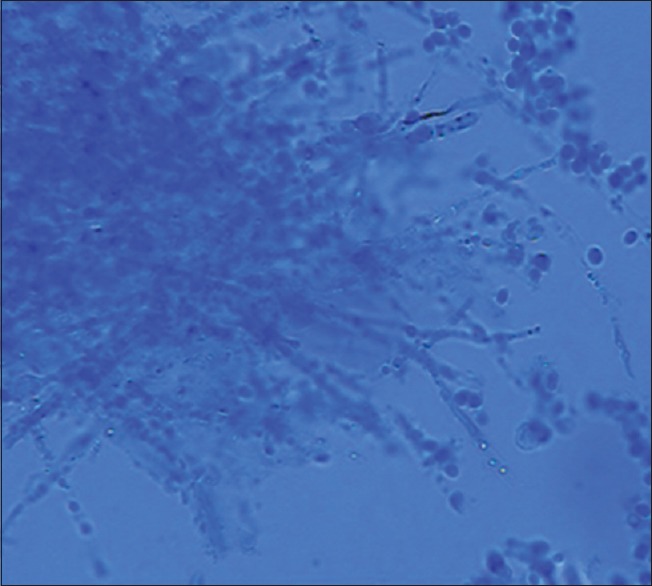
Trichophyton rubrum
Figure 4.
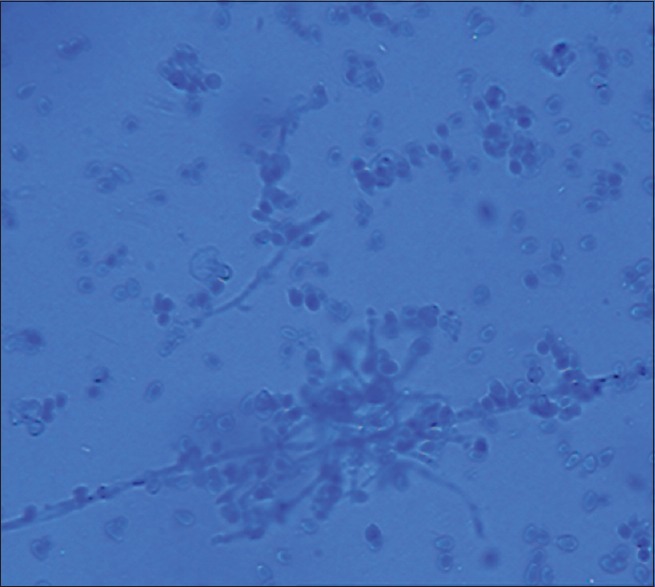
Trichophyton mentagrophytes
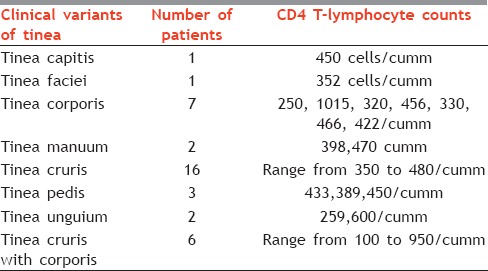
At the clinical materials to mycological examination sampling moment, the number of CD4 varied from 100/μl to 1015/μl. Patients with CD4+ T-cell count between 200/μl and 499/μl dominated. It was also found that the number of CD4+ T-cells does not influence the occurrence of dermatophytosis [Table 3].
Table 3.
Relation of CD4 count with the tinea infections
DISCUSSION
The frequency of dermatophytosis in patients with HIV infection is reported in the literature to be similar to that of the general population; however, these superficial mycoses seem to occur with greater variability in clinical presentation in these individuals.
In this study, a predominance of tinea cruris was observed, a finding which is in disagreement with that of Aly and Berger,[4] who described tinea pedis as the most common form in HIV-positive patients, and also in disagreement with that of Kaviarasan et al.,[5] who described tinea corporis to be the predominant.
T. rubrum was the most frequent dermatophyte species isolated from HIV-positive and AIDS patients. This finding agreed with results from previous studies.[2,6,7,8,9,10,11]
In a study by Lohoué Petmy et al.,[11] the study group comprised of 148 patients (84 males and 64 females) with HIV infection. Seventy-nine (53%) patients presented with at least one mycosis (44 males and 35 females; age range: 18–63 and 14–49 years, respectively), whereas in our study, out of the 120 patients reported, 38 (23.75%) had at least one mycosis (28 males and 10 females, with age range of 18–58 years).
Gregory[12] claims that decrease of CD4 count causes occurrence of various skin lesions, for example, onychomycosis develops at CD4 count around 450/μl. Similarly, Aly and Berger[4] and Gupta et al.[7] established that onychomycosis occurs at the early stage of HIV infection, at CD4 count around 400/μl. In our study, no significant statistical relationship was found between the presence of dermatophytes in foot interdigital spaces and CD4 count (Fisher's exact test, P = 0.4452), which is similar to the study by Rodwell et al.[2] However, dermatophytes were more often present in patients with CD4 <500/μl.
Of the total 305 individuals in a study by Costa et al., 60 (18.3%) had lesions with a clinical suspicion of dermatophytosis. Of the 60 patients, 20 (33%) had confirmed the initial diagnosis through a mycological study and only 2 of whom were females.[13] In our study of 120 patients, a total of 38 patients had clinical findings of dermatophytic infections.
The clinical evaluation of the patients had shown that 70% (14/20) had tinea corporis, 35% (7/20) had tinea unguium, 25% (5/20) had tinea cruris, and 5% (1/20) had tinea pedis. Seven patients presented with two different clinical types of tinea, simultaneously.[13] In our study, 42% of the patients had tinea cruris followed by tinea corporis in 18% of the cases. Co-existing T cruris and tinea corporis was seen in 15% of the cases.
The etiologic agents identified were T. rubrum, T. tonsurans, T. mentagrophytes, and Epidermophyton floccosum.
In 55% (11/20) of the patients alone, the genus Trichophyton was identified. T. rubrum was isolated from 5 patients, T. tonsurans from 2 patients, T. mentagrophytes from 1 patient, E. floccosum from 1 patient, and Trichophyton species from 1 patient.[13] In our study as well, T. rubrum was the most commonly found organism, appearing in 58% of the cases followed by T. mentagrophytes in 19.35% and T. violaceum in 12% of the cases.
CONCLUSION
Superficial fungal infections are a common yet significant problem in HIV infection. They are characterized by the diversity of clinical aspects; the lesions are mostly caused by T. rubrum. Optimum treatment should be administered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hanumanthappa H, Sarojini K, Shilpashree P, Muddapur SB. Clinicomycological study of 150 cases of dermatophytosis in a tertiary care hospital in South India. Indian J Dermatol. 2012;57:322–3. doi: 10.4103/0019-5154.97684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodwell GE, Bayles CL, Towersey L, Aly R. The prevalence of dermatophyte infection in patients infected with human immunodeficiency virus. Int J Dermatol. 2008;47:339–43. doi: 10.1111/j.1365-4632.2008.03416.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control (CDC) Classification system for human T-lymphotropic virus type III/lymphadenopathy-associated virus infections. MMWR Morb Mortal Wkly Rep. 1986;35:334–9. [PubMed] [Google Scholar]
- 4.Aly R, Berger T. Common superficial fungal infections in patients with AIDS. Clin Infect Dis. 1996;22(Suppl 2):S128–32. doi: 10.1093/clinids/22.supplement_2.s128. [DOI] [PubMed] [Google Scholar]
- 5.Kaviarasan PK, Jaisankar TJ, Thappa DM, Sujatha S. Clinical variations in dermatophytosis in HIV infected patients. Indian J Dermatol Venereol Leprol. 2002;68:213–6. [PubMed] [Google Scholar]
- 6.Garman ME, Tyring SK. The cutaneous manifestations of HIV infection. Dermatol Clin. 2002;20:193–208. doi: 10.1016/s0733-8635(01)00011-0. [DOI] [PubMed] [Google Scholar]
- 7.Gupta AK, Taborda P, Taborda V, Gilmour J, Rachlis A, Salit I, et al. Epidemiology and prevalence of onychomycosis in HIV-positive individuals. Int J Dermatol. 2000;39:746–53. doi: 10.1046/j.1365-4362.2000.00012.x. [DOI] [PubMed] [Google Scholar]
- 8.Cambuim II, Macêdo DP, Delgado M, Lima Kde M, Mendes GP, Souza-Motta CM, et al. Clinical and mycological evaluation of onychomycosis among Brazilian HIV/AIDS patients. Rev Soc Bras Med Trop. 2011;44:40–2. doi: 10.1590/s0037-86822011000100010. [DOI] [PubMed] [Google Scholar]
- 9.Cribier B, Mena ML, Rey D, Partisani M, Fabien V, Lang JM, et al. Nail changes in patients infected with human immunodeficiency virus. A prospective controlled study. Arch Dermatol. 1998;134:1216–20. doi: 10.1001/archderm.134.10.1216. [DOI] [PubMed] [Google Scholar]
- 10.Venkatesan P, Perfect JR, Myers SA. Evaluation and management of fungal infections in immunocompromised patients. Dermatol Ther. 2005;18:44–57. doi: 10.1111/j.1529-8019.2005.05001.x. [DOI] [PubMed] [Google Scholar]
- 11.Lohoué Petmy J, Lando AJ, Kaptue L, Tchinda V, Folefack M. Superficial mycoses and HIV infection in Yaoundé. J Eur Acad Dermatol Venereol. 2004;18:301–4. doi: 10.1111/j.1468-3083.2004.00924.x. [DOI] [PubMed] [Google Scholar]
- 12.Gregory N. Special patient populations: Onychomycosis in the HIV-positive patient. J Am Acad Dermatol. 1996;35:S13–6. doi: 10.1016/s0190-9622(96)90064-x. [DOI] [PubMed] [Google Scholar]
- 13.Costa JE, Neves RP, Delgado MM, Lima-Neto RG, Morais VM, Coêlho MR, et al. Dermatophytosis in patients with human immunodeficiency virus infection: Clinical aspects and etiologic agents. Acta Trop. 2015;150:111–5. doi: 10.1016/j.actatropica.2015.07.012. [DOI] [PubMed] [Google Scholar]


