Abstract
Background:
Sleep problems and depression are issues that can be addressed as far as nurses are concerned. This study aimed to investigate the role of workaholism in predicting the sleep problems and depression among Iranian nurses.
Materials and Methods:
we used the cross-sectional analytic research and correlational research design. Two hundred and forty-seven nurses in Malayer participated, based on the census method, in this study, that began in January and ended in March, 2017. Workaholism scale, sleep problem scale, and Short Form of Beck's Depression Inventory were used to collect the data that were finally analyzed by independent sample t-test, Pearson correlation coefficient, and hierarchical multiple regression tests.
Results:
About 13.77% of the nurses were workaholics, and 17.83% had mild–moderate depression. The main sleep problems were difficulty in starting sleep (44.53%) and extreme daytime sleeping at work (40.48%). The effect of marital status on workaholism (t = 1.99, p < 0.05) and depression (t = −2.55, p < 0.01), the effect of educational status on sleep problems (t = 3.08, p < 0.002), and the effect of occupational ward on workaholism (t = 2.06, p < 0.04), sleep problems (t = 4.83, p < 0.001), and depression (t = 1.99, p < 0.05) were statistically significant. Workaholism was positively correlated to sleep problems (r = 0.19, p < 0.003) and depression (r = 0.13, p < 0.04), working excessively (F = 22.75, p < 0.001), working compulsively (F = 21.00, p < 0.001), educational status (F = 7.25, p < 0.03), and occupational ward (F = 9.29, p < 0.001) were also shown to be significant predictors of sleep problems, age (F = 7.11, p < 0.001) and job experience (F = 7.19, p < 0.009) turned out to be the significant predictors of depression.
Conclusions:
Attention to psychological strategies to reduce the nurses' workaholism level plays an important role in decreasing such psychological problems as sleep problems and depression.
Keywords: Depression, Iran, nurses, sleep disorders, workload
Introduction
Nursing is the first stressful work among health-related jobs.[1] The most common complaints of nurses are depression, anxiety, fatigue, compassion fatigue, and burnout.[2,3,4] The study conducted by de Carvalho, Muller, de Carvalho, and de Souza Melo (2005) indicated that 54% of nurses showed a medium-to-high stressor capacity, and 22% high stressors.[5] Many of the nurses were shown to experience the occupational stress,[6,7] which threatens their physical and mental health.[8]
Due to excessive workload, nurses suffer from sleep problems. Nurses with sleep problems were at a higher risk of job strain and burnout related to work and the clients.[9] A review of the related literature shows that 39.8% of staff nurses have an insufficient sleep (IS) ratio.[9] Furthermore, prior research studies reveal that up to 57% of shift-working nurses have sleep problems.[10] About 12.2% of nurses in Taiwan have reported sleep problems[9] and 56% of the nurses have reported being sleep deprived.[11] The shortage of sleep is the most prevalent sleep problem for Iranian nurses.[12] Up to 50% of the Iranian nurses have had low levels of sufficient sleep and sleep quality[13] and 35.5% of them have taken medicine for sleep problems.[14]
Depression can influence a person's thoughts, behavior, feelings, and well-being.[15] Depressed people suffer from many problems such as sadness, solicitousness, emptiness, hopelessness, helplessness, valuelessness, sinfulness, testiness, shamefulness, or fidgety.[16] In Korea, 7% of nurses have had severe-to-moderate depression and 3.1% severe depressive symptoms.[17] In several studies, depression has been examined among nurses in Iran. The prevalence of depression in hospital nurses in Iran has been reported to equal 20–32%.[18,19]
One of the problems related to nurses' health is workaholism. This term was first used by Oates (1971).[20] According to Oates (1971), workaholism is “…the compulsion or the uncontrollable need to work excessively.”[20] Spence and Robbins (1992) argue that high work contention and drive and low work pleasure are major features of workaholic people.[21] Workaholism affects social function[22] and job performance.[20,23] The rate of workaholism has been estimated to equal 28.5% among hospital nurses in Japan[24] and in 16% of Dutch medical residents.[25] According to Khalidi et al., 50% of nurses in Sanandaj (a province in Iran) have a high level of workaholism.[26]
Workaholic hospital nurses suffer from many sleep problems such as IS, daily sleep at work, problems with waking up, and fatigue in the morning.[21] Workaholism was correlated to sleep quality among nurses.[16] Workaholics had longer sleep latency.[27] The levels of depression are high for nurses experiencing work pressure, role overload, and a lack of tribute.[28] Workers suffering from middle and high workaholism had significantly higher levels of depression than those people with a low level of workaholism.[29] Workers with a high level of workaholism suffer from depression.[30] Workaholism was correlated to depression among Chinese university teachers.[31]
The main research questions in the present study include “How prevalent are workaholism, sleep problems and depression for nurses in Malayer?” and “Does workaholism correlate to sleep problems and depression for Iranian nurses?” Nursing is one of the stressful jobs; so, stressful environments can cause many psychological problems, including sleep problems and depression. Identifying the predictive variables regarding sleep problems and depression in nurses will allow for psychological interventions to help promote health and well-being. Workaholism is one of the problems that has gone underexplored in Iranian nurses' community; previous studies have not investigated the role of demographic variables (i.e., age, job experience, gender orientations, marital status, educational status, and occupational ward) with workaholism in predicting sleep problems and depression of nurses. Therefore, given this novelty and innovation, this study as an attempt helps expand the related literature and evoke interest from future researchers of the field.
Materials and Methods
A cross-sectional analytic research design was used to investigate the extent to which workaholism, sleep problems, and depression were prevalent for the Iranian nurses. A correlational method was also used to investigate the extent to which workaholism was related to sleep problems and depression. In this study, workaholism was considered as a predictive variable, and sleep problems and depression were deemed criterion variables. This research study was embarked on in January and ended in March, 2017. In fact, the data collection process lasted for almost 3 months.
The statistical population of this study consisted of 280 nurses in Malayer, Iran. According to the Cochran Formula,[32] a sample of 162 is required for a statistical population of ~280. Confidence level, test power, and z were considered to be 0.95%, 0.90%, and 1.96, respectively. Nonetheless, since the study was an attempt to investigate the extent to which sleep problems and depression were prevalent, a total of 280 nurses were selected by the census method among 3 hospitals in Malayer. A total of 280 self-reported questionnaires were distributed among nurses. Twenty-two distributed questionnaires were discarded for being incomplete, and 11 questionnaires were not answered and therefore excluded from the study. The final sample consisted of 247 (54.3% female and 45.7% male) nurses working for Malayer hospitals: Mehr (45.3%), Imam Hussein (33.6%), and Gharazi (21.1%). After signing the consent form, a total of 247 nurses completed the questionnaires in the nursing room for 25–30 min.
Inclusion criteria included a lack of proper mental conditions and severe physical illness, and lack of admission due to mental disorders over a year. On the contrary, exclusion criteria included incomplete answers to the items consisted in the questionnaires, not having severe infectious diseases (such as influenza) and a lack of consent to participate in this research study.
We used a 10-item workaholism scale (WS). WS was developed by Schaufeli et al.[33] It included working excessively (WE) (5 items; for instance, “I seem to be in a hurry and racing against the clock”) and working compulsively (WC) (5 items; for instance, “I feel obliged to work hard, even when it's not enjoyable”) subscales. The items were scored based on a 4-point scale from “totally disagree = 1 to totally agree = 4.”[33] This scale distinguished four quadrant groups: (1) “Relaxed workers” (low WE and WC), (2) “Compulsive workers” (low WE and high WC), (3) “Hard workers” (high WE and low WC), and (4) “Workaholics” (high WE and WC).[30] The scale was internally consistent in the Netherlands and Japan populations.[33] The convergent validity showed that the WE was positively correlated to overtime (r = 0.32, p < 0.001) and overwork (r = 0.13, p < 0.001) subscale of excess working time;[33] and the correlation coefficient of WC with overtime and overwork was 0.40 (p < 0.001) and 0.23 (p < 0.001), respectively. The Cronbach's alpha related to WE and WC was 0.78 and 0.68, respectively.[33] The present study calculated the Cronbach's alpha related to workaholism to equal 0.82, and it reported its split-half reliability to be 0.76. We also used Sleep Problem Scale to measure the sleep problems. This eight-question scale was used by Kubota et al.[24] based on previous epidemiological studies of sleep. These eight questions included difficulty in starting sleep (DSS), problem in keeping sleep (PKS), wake up early in the morning (WEM), nap during the day (NDD), IS, extreme daytime sleeping at work (EDSW), difficult awakening in the morning (DAM), and fatigue in awakening in the morning (FAM). A positive response to (1) DSS, (2) PKS, or (3) WEM questions is insomnia symptoms. The answers to DSS are based on a 5-point Likert scale: “0–10 min = 1,” “11–30 min = 2,” “31–59 min = 3,” “1–2 h = 4,” and “2 + h = 5.” The criterion response to DSS is “over 30 min.” The answers to PKS, WEM, NDD, and EDSW are based on a 6-point Likert scale: “never (or almost never) =1,” “few times a year = 2,” “more than once a month = 3,” “more than once a week = 4,” “more than three times a week = 5,” and “almost every day = 6.” The criterion response to these questions was “More than three times a week.” IS was rated on a 4-point Likert scale: “very much sufficient = 1,” “fairly sufficient = 2,” “somewhat insufficient = 3,” and “definitely insufficient = 4.” The criterion response to “IS” is “Somewhat insufficient.” DAM and FAM were scored on a 6-point Likert scale: “never (or almost never) =1,” “few times a year = 2,” “more than once a month = 3,” “more than once a week = 4,” “more than three times a week = 5,” and “almost every day = 6.” The criterion response to these questions was “More than once a week.”[24] The present study calculated the Cronbach's alpha related to sleep problems (eight self-reported questions) to be 0.67 and reported it to equal 0.68 and reported its split-half reliability as 0.61.
The present study also used Beck's Depression Inventory (BDI-13).[34] The total score ranged from 0 to 39. In a study by Beck et al. (1974),[34] the correlation coefficient between the short and long (21 items) forms of the questionnaire ranged from 0.89 to 0.97. This short form has been used in Iran, and its Cronbach's alpha, Spearman–Brown, and Guttman split-half coefficients are 0.85, 0.70, and 0.67, respectively.[32] As for the cutoff point of the scale, scores of 0–3, 4–7, 8–11, 12–15, and 16–39 indicate normal, mild, mild–moderate, moderate, and severe depression in the normal population.[35] Cronbach's alpha, test–retest reliability, and split-half reliability of this scale in Iran are 0.91, 0.94, and 0.89, respectively.[36] The present study reported its Cronbach's alpha to be 0.77. We used the 23rd version of Statistical Package for the Social Sciences software (IBM SPSS; version 23, SPSS Inc., Chicago, IL, USA) to analyze the data. The independent sample t-test was used to compare the variables according to gender, marital status, educational status, and job section; the Pearson correlation coefficient and hierarchical multiple regressions were also used to analyze the data. The significance level in this study was found to equal 0.05 or less.
Ethical considerations
Before distributing the questionnaires, the researchers explained the goals of the study to the nurses and invited them for some detailed explanations in a private room in the hospitals. Those who agreed to participate were delivered a workshop about the purpose, procedure, and ethical issues of the study. They handed in the completed form of the questionnaires to the researchers. The participants were assured that their information would not be shared with others. Furthermore, they signed a consent form and completely agreed with the publication of their information in the article. Needless to say, no one was forced to answer the questionnaires.
Results
The descriptive results showed that 213 (86.23%) had bachelor's degree and 34 (13.87%) held master's degree; 86 (34.82%) were single, but 161 (65.18%) were married; 90 (36.44%) of nurses were emergency nurses, and 157 (63.56%) were nonemergency ones. The age means (SD) of the female nurses, male nurses, and all of the nurses were 30.34 (5.40), 31.85 (5.39), and 31.03 (5.44), respectively. Moreover, the working experience means (SD) of these three groups mentioned earlier were 6.28 (4.69), 7.44 (5.05), and 6.81 (4.88), respectively.
The present study took one unit of a standard deviation higher than the mean score as the high levels of WE and WC. The mean (SD) score of WE and WC was 11.54 (3.14) and 10.84 (3.06), respectively. Nurses with scores higher than 14.68 in WE were considered as high WE and with scores higher than 13.90 in WC considered as high WC. According to these scores, 72.06% of nurses were “Relaxed workers” (low WE [>14.68] and low WC [>13.90]), 5.67% “Compulsive workers” (low WE [>14.68] but high WC [<13.90]), 8.50% “Hard workers” (high WE [<14.68] but low WC [>13.90]), and 13.77% “Workaholics” (high WE [<14.68] and high WC [<13.90]).
According to the cutoff point of the short form of the depression scale,[32] 10.12% of nurses had mild depression, 5.26% mild-to-moderate depression, and 2.43% moderate depression. No one had severe depression, and 80% had no symptoms of depression; according to results related to sleep problems, 44.53%, 17.81%, 6.07%, 19.83%, 33.60%, 40.48%, 35.22%, and 9.71% of the nurses had DSS, PKS, WEM, NDD, IS, EDSW, DAM, and FAM, respectively [Table 1]. Table 2 indicates the mean, standard deviation, and normality tests of variables.
Table 1.
Rate of workaholism, depression and sleep problems, in nurses
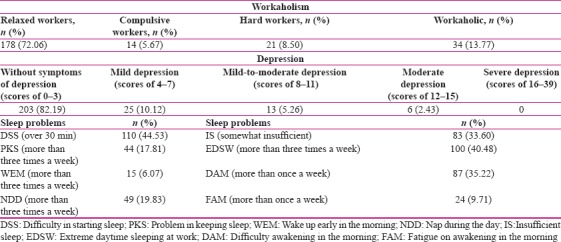
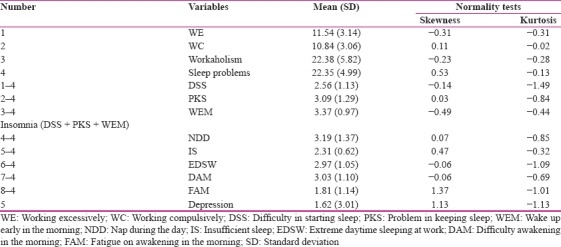
Table 2.
Mean, standard deviation, and normality tests of variables
The results in Table 3 indicated that there are not any statistically significant differences between female and male nurses suffering from workaholism, sleep problems, and depression. Workaholism was found to be higher in married nurses than the single ones. Furthermore, depression was found to be higher in single nurses than the married ones. However, there was no meaningful difference between married and unmarried nurses with sleep problems. Sleep problems were more severe for nurses with a bachelor's degree than those with a master's degree, but there was no statistically significant difference between nurses with bachelor's and master's degree with workaholism and depression. Workaholism, sleep problems, and depression for emergency nurses were higher than the nonemergency ones.
Table 3.
Comparison of workaholism, sleep problems, and depression according to gender, marital status, educational status, and occupational ward
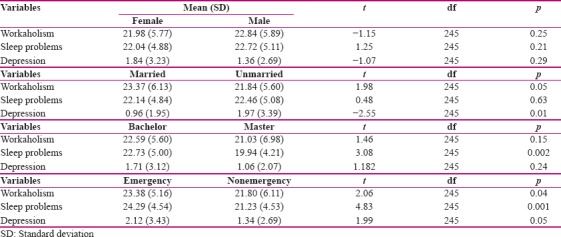
Table 4 indicates the results of Pearson's correlation coefficients. According to this table, workaholism is positively correlated to DAM (p < 0.01), FAM (p < 0.001), and sleep problems (p < 0.003) and depression (p < 0.04); WE is correlated to insomnia (p < 0.03), NDD (p < 0.03), DAM (p < 0.001), FAM (p < 0.001), and sleep problems (p < 0.001); WC is correlated to FAM (p < 0.001) and depression (p < 0.02), but there is no statistically significant correlation between WE with IS, EDS, and depression; between WC with insomnia, NDD, IS, EDSW, DAM, and sleep problems; and between workaholism with insomnia, NDD, IS, and EDSW. Age (p < 0.001) and job experience (p < 0.01) are positively correlated to depression, and there is no statistically significant correlation between age and job experience for the nurses with sleep problems.
Table 4.
Correlation of workaholism, age, and job experience with sleep problems and depression
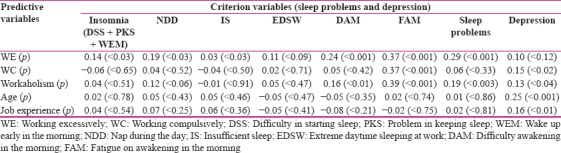
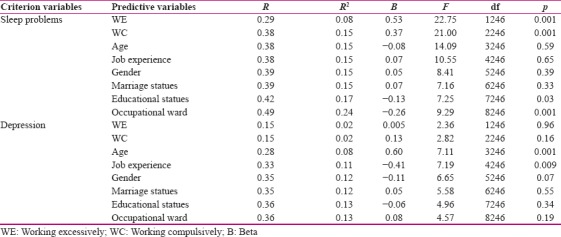
The hierarchical multiple regressions were also used to evaluate the role of workaholism dimensions (WE and WC) in predicting the sleep problems and depression for the nurses. R2 in regression model showed that the model accounts for 0.24% of variance in sleep problems, and WE (B = 0.53, p < 0.001), WC (B = 0.37, p < 0.001), educational status (B = −0.13, p < 0.03), and occupational ward (B = −0.26, p < 0.001) were statistically significant predictors of sleep problems in nurses. Furthermore, the model accounts for 0.13% of variance in sleep problems, and WE (B = 0.005, p < 0.96) and WC (B = 0.13, p < 0.16) were not statistically significant predictors of depression in nurses; but age (B = 0.60, p < 0.001) and job experience (B = -0.41, p < 0.009) were statistically significant predictors of depression [Table 5].
Table 5.
Predicting the sleep problems and depression by working excessively and compulsively, and demographic variables
Discussion
The prevalence of and correlation between workaholism, sleep problems, and depression have been the focal points of this study. Descriptive results showed that 13.77% of nurses were workaholics. Our results are similar to those obtained by Schaufeli et al.[25] who found that 16% of Dutch medical residents were workaholics. Since nurses deal with different patients and deal daily with many people with different problems, the amount of workaholism among them can be justified. Nurses are responsible for controlling and monitoring the patients on a full-time basis. The rate of workaholism in our research is lower than previous studies that showed that the rate of workaholism was 28.5% for Japanese nurses[21] and more than 50% for Iranian nurses.[23] The contradiction between this one and those by Kubota et al.[24] is probably due to the work culture in Iran and Japan. Put it another way, Japanese workers work more excessively. For example, researchers indicated that 28.15 of the population of Japan work more than 50 h/week[35] and according to Labour Force Survey, 15.7% of Japanese male workers worked more than 60 h/week in 2014.[37] In addition, working hours in Japan equal about 1800 h/year.[38] Therefore, it is likely that among the Japanese workers, the levels of workaholism are higher in comparison with the Iranian ones. However, replicating the study seems necessary. The contradiction between the results gained from this study and those by Khalidi et al.[26] is probably due to the scales used by two research studies. In effect, we used WS[33] in this study. This scale distinguishes workaholics from relaxed workers, compulsive workers, and hard workers.[33] According to this scale, workaholics are those who get high scores on both WE and WC subscales. On the other hand, Khalidi et al.[26] used Spence and Robbins[21] WS in their work and they had considered scores higher than 55 as the cutoff point for this scale.
In our study, 10.12% of nurses had mild depression, 5.26% mild-to-moderate depression, and 2.43% moderate depression. No one had severe depression. The prevalence of depression has been investigated by many researchers. For example, the prevalence of moderate-to-severe and severe levels of depression symptoms in South Korea nurses were 7.6% and 3.1%, respectively.[14] In Iran, the prevalence of depression has been reported to be in the range of 20–32%.[15,16] However, in our research, none of the participants of the study had severe depression, and the prevalence of mild-to-moderate depression was 17.81% (10.12% mild, 5.26% mild-to-moderate, and 2.43% moderate depression). We used short form of BDI-13 to assess the depression rate which shows the likelihood of bias in responding to the questions; Therefore, it is likely that this bias can affect the prevalence of depression for nurses. We should consider the effect of employment on reducing depression in the Iranian nurses, because work is identified as the most important factor affecting happiness[38] and unemployed people have higher depression than the employed individuals.[39]
As shown by the descriptive results, 44.53%, 17.81%, 6.07%, 19.83%, 33.60%, 40.48%, 35.22%, and 9.71% of the research participants had DSS, PKS, WEM, NDD, IS, EDSW, DAM, and FAM, respectively. Many studies have reported multiple sleep problems associated with nurses. For example, 39.8% of staff nurses,[9] 57% of shift-working nurses,[10] 12.2% of nurses in Taiwan,[9] and 35.5% of the Iranian nurses[14] have reported many sleep problems. As nurses work in a shift of 24 h and are forced to take care of patients, sleep problems are common among them. Previous research studies have confirmed the effects of shift work on sleep problems for nurses.[10]
The results indicated that workaholism rate was higher among the married nurses than the single ones; perhaps, one of the reasons is that married nurses try to do extra work to live a better life. In this study, depression rate was higher for the single nurses than the married ones. Interestingly enough, this result is in line with those gained by Bulloch et al.[40] Living with a spouse leads to one's mental and physical well-being, which is likely to reduce the depression rate among the married nurses. Nurses holding a bachelor's degree had more sleep problems than those holding a master's degree. This result is consistent with the results obtained by Grandner et al.[41] This may be due to better job opportunities and possibly higher salaries earned by nurses holding a master's degree. In addition, emergency nurses had a higher rate of workaholism, sleep problems, and depression than their nonemergency counterpart. To date, workaholism in emergency and nonemergency nurses has not been compared in the related literature. Because of working with emergency patients, emergency nurses usually work harder than other departments, and this can justify the difference in terms of the depression rate. Previous studies are found to refer to the high rate of depression[42] and sleep problems[43] among emergency nurses. Emergency nurses are continuously encountered with accidental patients and patients with severe physical problems; so, the pain and suffering of these patients can probably cause a lot of psychological problems, including depression and sleep problems.
Workaholism was found to be positively correlated to DAM, TAM, and sleep problems. Moreover, WE was revealed to be correlated to insomnia, NDD, DAM, FAM, and sleep problems. Furthermore, WC was shown to be correlated to FAM. According to hierarchical regression, WE, WC, educational status, and occupational ward were significant predictors of sleep problems among the nurses. The result is consistent with previous research studies which concluded that workaholism was negatively correlated to sleep quality among nurses[20] and workaholic nurses[23] were at higher risks of sleep problems. Nurses with a high rate of workaholism spend a great deal of their time in performing occupational activities in the hospital and are forced to work, which causes many sleep problems such as insomnia, NDD, IS, EDSW, DAM, and FAM. In other words, the compulsive drive to work among workaholics probably makes the nurses replace their sleep times with work and therefore suffer from IS and insomnia. Due to the predictive role of educational status and occupational ward, it can be claimed that nurses holding a master's degree may have better job salaries and benefits. In addition, as nonemergency nurses are less likely to deal with accidental patients, they may experience less sleep problems.
According to the obtained results, workaholism was positively correlated to depression, and WC was correlated to depression. In addition, according to the hierarchical regression, WE and WC did not predict the depression scores among the nurses. However, age and job experience were significant predictors of depression in this regard. The result is consistent with previous research studies which showed that workers with workaholism had higher levels of depression.[29] They indicated that nurses who experience job strain and role overload suffer from depression.[28]
Workaholics have the following three characteristics: (a) tendency to spend a lot of time in performing job activities, (b) unwillingness to abandon work and constantly think about work, and (c) desire to work beyond what is reasonably expected from them.[44] Furthermore, workaholics perform cognitive (i.e., WC) and behavioral activities (i.e., WE)[20] that may cause psychological distress, such as depression. In other words, workaholics are people who are individually responsible for a lot of work and avoid the community for their job conditions and consequently may show negative mood and depression symptoms even when they are not working. Because of the predictive role of age and job experience, it can be said that due to the identical working environments and the experience of working with different patients, despite the increase in age and job experience, symptoms of depression may increase among the nurses. The limitations of this study were related to the statistical sample and using the self-reported questionnaires as tools for measuring the variables; that is to say, the sample was limited to the hospitals in Malayer. The results should be interpreted with caution. Moreover, answering self-report questionnaires is usually associated with bias. It is suggested that future studies use interviews to measure the rates of workaholism, sleep problems, and depression.
Conclusion
The results obtained by this study support the prevalence of the workaholism, sleep problems, and depression, and the significant and positive correlation between workaholism and sleep problems and depression among Iranian nurses. Therefore, we suggest that attention to sleep problems and depression among Iranian nurses and their predictive variables (such as workaholism) is very important for those who are dealing with resolving the mental problems of nurses. In addition, the use of psychological and therapeutic strategies to solve the psychological problems of nurses can be involved in reducing their psychological problems of nurses.
Financial support and sponsorship
Malayer University, Malayer, Iran
Conflicts of interest
Nothing to declare.
Acknowledgments
This article was extracted from an internal investigation project 89-1-20267 at Malayer University, Malayer, Iran. The author would like to thank the nurses who participated in this study.
References
- 1.Rice VH. Handbook of Stress, Coping, and Health: Implications for Nursing Research, Theory, and Practice. 2nd ed. USA: SAGE Publication Inc; 2012. [Google Scholar]
- 2.Mogharab M, Nateghi K, Shamaie-Zavareh A, Sharifzadeh G. The correlation of religious orientation with depression among critical care and emergency room nurses. Mod Care J. 2016;13:e12470. [Google Scholar]
- 3.Hegney DG, Craigie M, Hemsworth D, Osseiran-Moisson R, Aoun S, Francis K, et al. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J Nurs Manag. 2014;22:506–18. doi: 10.1111/jonm.12160. [DOI] [PubMed] [Google Scholar]
- 4.Ariapooran S. Compassion fatigue and burnout in Iranian nurses: The role of perceived social support. Iran J Nurs Midwifery Res. 2014;19:279–84. [PMC free article] [PubMed] [Google Scholar]
- 5.Ariapooran S. The prevalence of secondary traumatic stress among nurses in Iran, Malayer: The predicting role of mindfulness and social support. Int J Community Based Nurs Midwifery. 2013;1:156–64. [Google Scholar]
- 6.Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015;12:652–66. doi: 10.3390/ijerph120100652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sekol MS, Kim SC. Job satisfaction, burnout, and stress among pediatric nurses in various specialty units at an acute care hospital. J Nurs Educ Pract. 2014;4:115–24. [Google Scholar]
- 8.Idris MK. Over time effects of role stress on psychological strain among Malaysian public university academics. Int J Bus Soc Sci. 2011;2:154–61. [Google Scholar]
- 9.Chien PL, Su HF, Hsieh PC, Siao RY, Ling PY, Jou HJ. Sleep quality among female hospital staff nurses. Sleep Disord 2013. 2013:283490. doi: 10.1155/2013/283490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shao MF, Chou YC, Yeh MY, Tzeng WC. Sleep quality and quality of life in female shift-working nurses. J Adv Nurs. 2010;66:1565–72. doi: 10.1111/j.1365-2648.2010.05300.x. [DOI] [PubMed] [Google Scholar]
- 11.Johnson AL, Jung L, Song Y, Brown KC, Weaver MT, Richards KC. Sleep deprivation and error in nurses who work the night shift. J Nurs Adm. 2014;44:17–22. doi: 10.1097/NNA.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 12.Sanjari M, Shirazi F, Heidari S, Maleki S, Saalemi S. Association of sleep behaviors and occupational injuries in nurses. Iran J Nurs. 2010;22:32–41. [Google Scholar]
- 13.Yazdi Z, Sadeghniiat-Haghighi K, Javadi AR, Rikhtegar G. Sleep quality and insomnia in nurses with different circadian chronotypes: Morningness and eveningness orientation. Work. 2014;47:561–7. doi: 10.3233/WOR-131664. [DOI] [PubMed] [Google Scholar]
- 14.Bagheri H, Shahabi Z, Ebrahimi H, Alaeenejad F. The association between quality of sleep and health-related quality of life in nurses. Hayat. 2006;12:13–20. [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington: American Psychiatric Association; 2013. [Google Scholar]
- 16.Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Lee HY, Kim MS, Kim O, Lee IH, Kim HK. Association between shift work and severity of depressive symptoms among female nurses: The Korea nurses' health study. J Nurs Manag. 2016;24:192–200. doi: 10.1111/jonm.12298. [DOI] [PubMed] [Google Scholar]
- 18.Taghva A, Yazdani A, Ebrahimi MR, Alizadeh K, Sakhabakhsh M. Prevalence of depression in psychiatric nurses and comparison with other parts of the AJA hospitals. J Nurs Phys War. 2014;1:11–6. [Google Scholar]
- 19.Khamse F, Ebadi A, Salimi H. Survey relationship between demographic factors and stress, anxiety and depression in nurses working in selected hospitals in Tehran city. J Holist Nurs Midwifery. 2011;21:13–21. [Google Scholar]
- 20.Kubota K, Shimazu A, Kawakami N, Takahashi M, Nakata A, Schaufeli WB. The empirical distinctiveness of work engagement and workaholism among hospital nurses in Japan: The effect on sleep quality and job performance. Cienc Trab. 2011;13:152–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Shkoler O, Rabenu E, Tziner A. The dimensionality of workaholism and its relations with internal and external factors. Rev Psicol Trabajo Organ. 2017;33:193–203. [Google Scholar]
- 22.Sussman S. Workaholism: A review. J Addict Res Ther. 2012 doi: 10.4172/2155-6105.S6-001. pii: 4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimazu A, Schaufeli WB, Taris TW. How does workaholism affect worker health and performance? The mediating role of coping. Int J Behav Med. 2010;17:154–60. doi: 10.1007/s12529-010-9077-x. [DOI] [PubMed] [Google Scholar]
- 24.Kubota K, Shimazu A, Kawakami N, Takahashi M, Nakata A, Schaufeli WB. Association between workaholism and sleep problems among hospital nurses. Ind Health. 2010;48:864–71. doi: 10.2486/indhealth.ms1139. [DOI] [PubMed] [Google Scholar]
- 25.Schaufeli WB, Bakker AB, Van der Heijden FM, Prins JT. Workaholism among medical residents: It is the combination of working excessively and working compulsively that counts. Int J Stress Manag. 2009;16:249–72. [Google Scholar]
- 26.Khalidi S, Neda Sheikhzakariaie N, Olyaee N, Moridi G, Esmaeil Nasab G, Khosravi F, et al. Relationship between workaholism and personality factors among nurses: A questionnaire-based cross-sectional study. J Chem Pharm Sci. 2016;9:3129–35. [Google Scholar]
- 27.Kubota K, Shimazu A, Kawakami N, Takahashi M. Workaholism and sleep quality among Japanese employees: A prospective cohort study. Int J Behav Med. 2014;21:66–76. doi: 10.1007/s12529-012-9286-6. [DOI] [PubMed] [Google Scholar]
- 28.Ohler MC, Kerr MS, Forbes DA. Depression in nurses. Can J Nurs Res. 2010;42:66–82. [PubMed] [Google Scholar]
- 29.Matsudaira K, Shimazu A, Fujii T, Kubota K, Sawada T, Kikuchi N, et al. Workaholism as a risk factor for depressive mood, disabling back pain, and sickness absence. PLoS One. 2013;8:e75140. doi: 10.1371/journal.pone.0075140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andreassen CS, Griffiths MD, Sinha R, Hetland J, Pallesen S. The relationships between workaholism and symptoms of psychiatric disorders: A large-scale cross-sectional study. PLoS One. 2016;11:e0152978. doi: 10.1371/journal.pone.0152978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nie Y, Sun H. Why do workaholics experience depression? A study with Chinese university teachers. J Health Psychol. 2016;21:2339–46. doi: 10.1177/1359105315576350. [DOI] [PubMed] [Google Scholar]
- 32.Nouri A, Mohammadi Y. An Action Guide to Research Humanities. Tehran: Viraiesh; 2016. [Google Scholar]
- 33.Schaufeli WB, Shimazu A, Taris TW. Driven to work excessively hard: The evaluation of a two-factor measure of workaholism in the Netherlands and Japan. Cross Cult Res. 2009;43:320–48. [Google Scholar]
- 34.Dadfar M, Kalibatseva Z. Psychometric properties of the Persian version of the short Beck Depression Inventory with Iranian psychiatric outpatients. Scientifica (Cairo) 2016. 2016:8196463. doi: 10.1155/2016/8196463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee S. Working hours gap. In: Messenger JC, editor. Working Time and Workers' Preference in Industrial Countries. London: Routledge; 2004. pp. 29–59. [Google Scholar]
- 36.Ebrahimi A, Barekatin M, Bornamanesh A, Nasiri H. Psychometric characteristics of Persian form of BDRS among patients and normal people. Iran J Psychiatry Clin Psychol. 2015;21:60–8. [Google Scholar]
- 37.Sachiko K, Isamu Y. Workers Mental Health, Long Work Hours and Workplace Management: Evidence from Workers' Longitudinal Data in Japan. The Research Institute of Economy, Trade and Industry. Discussion Paper Series. 2016;16-E-017 [Google Scholar]
- 38.Layard R. Happiness-Lessons from a New Science. 2nd ed. London: Penguin; 2011. [Google Scholar]
- 39.McGee RE, Thompson NJ. Unemployment and depression among emerging adults in 12 states, behavioral risk factor surveillance system, 2010. Prev Chronic Dis. 2015;12:E38. doi: 10.5888/pcd12.140451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bulloch AG, Williams JV, Lavorato DH, Patten SB. The depression and marital status relationship is modified by both age and gender. J Affect Disord. 2017;223:65–8. doi: 10.1016/j.jad.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 41.Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adriaenssens J, de Gucht V, Maes S. The impact of traumatic events on emergency room nurses: Findings from a questionnaire survey. Int J Nurs Stud. 2012;49:1411–22. doi: 10.1016/j.ijnurstu.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 43.Han Y, Yuan Y, Zhang L, Fu Y. Sleep disorder status of nurses in general hospitals and its influencing factors. Psychiatr Danub. 2016;28:176–83. [PubMed] [Google Scholar]
- 44.Scott KS, Moore KS, Miceli MP. An exploration of the meaning and consequences of workaholism. Hum Relat. 1997;50:287–314. [Google Scholar]


