Abstract
Background:
The failure to detect “red flag” signs in patients presenting with acute low back pain can adversely affect the outcome of management. This can seriously affect the quality of life and productivity of the patient.
Objective:
The present questionnaire-based study was performed to assess the knowledge and awareness of red flag signs among primary health care physicians managing patients with acute back pain in Riyadh, Saudi Arabia.
Materials and Methods:
The study sample size was comprised of 80 subjects. The level of knowledge was assessed by means of a new structured self-administered questionnaire. The design of this questionnaire was based on the Agency for Health Care Research and Policy (AHCRP) guidelines for detection of red flag signs. Physicians were asked about red flag signs that indicate the presence of tumor, infection, spinal fracture, or cauda equina syndrome.
Results:
Sixty-eight (85% of total) physicians were aware of red flag signs. Of the 68 physicians who were aware of the red flag signs, 58 (72%) were aware of neurological deficit, 36 (45% of total) were aware of extremes of age (<10 years and >50 years), and 33 (41% of total) were aware of and routinely inquired about the history of spinal trauma, whereas only 24 (30% of total) were aware of and inquired about constitutional symptoms in their patients with acute back pain.
Conclusion:
Although low back pain is extremely common, knowledge and awareness of red flag signs of primary health care physicians managing patients with acute back pain in Riyadh appear to be inadequate. This indicates a lack of adherence to the international guidelines. Specific educational programs should target these deficiencies and increase awareness.
Keywords: Low back pain, primary care, red flags
Abstract
ملخص البحث : تهدف هذه الدراسة المبنية على الاستبانة إلى تقصي معرفة العلامات الدالة للمرضى المصابين بألم الظهر الحاد لدى أطباء الرعاية الصحية الأولية في مدينة الرياض. شملت الدراسة 80 طبيبا. ووضحت أن %68 من الأطباء كانوا على علم وتعرف %17 من هؤلاء على كل علامات الخطورة بينما تعرف %72,5 منهم لعلامات الخطورة للعجز العصبي و %41 كانوا على معرفة بالأسئلة الروتينية للتاريخ المرضى لإصابات الظهر وتعرف %30 منهم على الأعراض العامة لدى المرضى المصابين بألم الظهر الحاد.
INTRODUCTION
Low back pain is the second most common reason for individuals to seek medical advice. Eighty percent of individuals experience back pain in their lifetime,[1] and this is associated with significant work disability.[2] The estimated cost of low back pain in the United States in 1998 was $90.7 billion, making it a major burden on health care resources.[3] Because of the magnitude of the problem, several evidence-based guidelines have been developed to provide effective treatment for low back pain. Some such are the Agency for Health Care Research and Policy (AHCRP) guidelines formulated in 1994 and have been accepted worldwide.[4] Several guidelines have also been put forward following the introduction of the AHCRP guidelines, but they are, however, not much different from the AHCRP guidelines.[5]
Almost all guidelines established to date[4,5,6] have focused on one major component; the recognition of red flag signs in patients presenting with low back pain. Red flag signs such as the history of trauma, constitutional symptoms, or neurologic deficits are believed to be present in approximately 5% of patients with back pain.[4] Detection of these signs on the outset is essential because their presence is an absolute indication that immediate care is required, and further investigations are necessary for appropriate management.[5] Delays in the detection of these signs often have serious consequences, leading to significant morbidity.[6] It is, therefore, mandatory to follow the established guidelines for the prompt detection of red flag signs to avoid adverse outcomes in patients presenting with back pain. However, there are sufficient data to suggest that the recommended guidelines are not followed in day-to-day clinical practice in various countries,[7,8] which may significantly contribute to the morbidity associated with acute back pain.
The present questionnaire-based study was done to assess the awareness and knowledge about red flag signs of primary care practitioners who treat patients presenting with acute back pain (lasting <6 weeks).
MATERIALS AND METHODS
The questionnaire was designed to assess the awareness and knowledge of red flag signs among general health practitioners in Riyadh, the capital city of the Kingdom of Saudi Arabia. They were distributed to primary health care physicians in 11 Primary Care Centers in Riyadh. Since very few private health institutions in Riyadh employ family physicians - the target of our study, only a few centers qualify as Primary Care Centers. Therefore, only public centers were targeted. The questions were specifically designed in accordance with the AHCRP guidelines to elicit physician responses to a section on red flag signs that indicate the presence of a tumor, infection, spinal fracture, or cauda equina syndrome. Convenience sampling was also done to select subjects of primary care clinics. The study sample size was 80 subjects which was calculated statistically by considering the following variables: Estimated prevalence, sample error, and level of confidence were 50%, 8%, and 95%, respectively. Inclusion and exclusion criteria were used to select participants to ensure their relevance to the study purpose and to obtain optimum results.
Inclusion criteria
Primary care physicians of both genders - general practitioner (GP), specialists and consultants.
Fluency in English.
Exclusion criteria
Residents in-training.
The questionnaire primarily focused on whether the physicians were aware of red flag signs. There were questions on the four major aspects of red flag signs including some on constitutional symptoms, extremes of age (i.e., <10 years of age or >50 years of age), history of spinal trauma, and neurological deficit. Questions on the awareness of constitutional symptoms included physician responses to the presence of fever, malaise, anorexia, and weight-loss. Questions about awareness of neurological deficit were designed to extract knowledge of any urinary or bowel incontinence and motor or sensory loss. The validity of the questionnaire was done before data collection in a pilot study on 20 individuals not included in the final study. The questionnaires were given to 80 primary health care physicians during personal visits.
RESULTS
All the physicians completed and returned the survey during the visits, giving a response rate of 100%. Most respondents were qualified family physicians (71%). The rest were either specialists (8%) or GPs (20%). The majority worked in Ministry of Health Centers (46%) while others were employed in military centers (31%) or centers attached to academic institutions (23%).
Of all the respondents, 68 (85% of total) were aware of red flag signs [Figure 1]. Of the 12 (15%) physicians who were not aware of the signs, four were only aware of the term "red flag signs" but had no knowledge of what these signs are.
Figure 1.
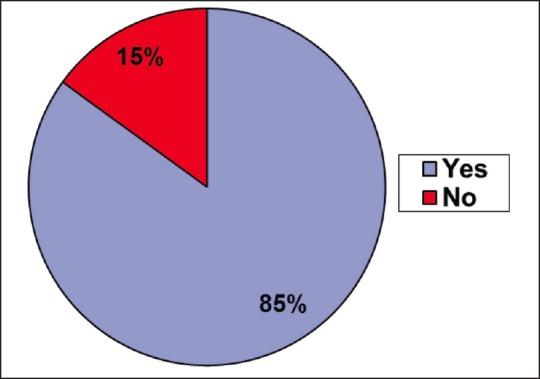
Percentage of respondents who were aware of ‘red flag signs’ in spinal pathology
A majority, 58 of the physicians, who had knowledge of red flag signs were aware of neurological deficit as a red flag (72.5% of total, 85% of sub-group), followed by 36 (45% of total, 53% of sub-group) physicians who were aware of the risks at the extremes of age (<10 years of age and >50 years of age). Similarly, 33 out of 68 (41.3% of total, 49% of sub-group) physicians were aware of and routinely inquired about the history of spinal trauma, whereas only 24 physicians (30% of total, 35% of sub-group) considered inquiry about constitutional symptoms an essential part of the initial interaction with patients presenting with acute back pain [Figure 2]. A small minority, 14 respondents (17% of total, 20% of sub-group) of the primary health care physicians had sufficient knowledge of all red flag signs.
Figure 2.
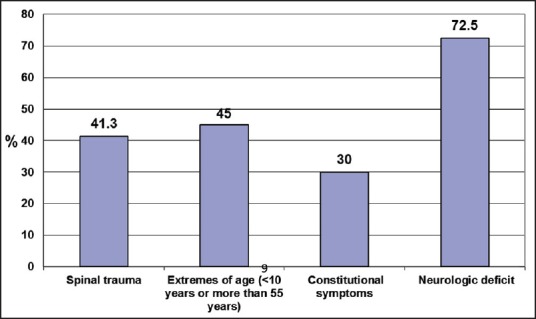
Physicians’ responses to questions about the four components of the questionnaire
DISCUSSION
The results of the present study revealed that 15% of the primary health care physicians did not have the vital information on red flag signs. A relatively small percentage had adequate knowledge. Despite the availability of several guidelines for the initial assessment of low back pain,[4,5,6] the level of awareness for the initial assessment of acute back pain varied. The most likely explanation for the varying levels of knowledge on acute back pain is either personal opinions or shared beliefs or complete disregard of the evidence-based practice recommendations in the management of the back pain.[9,10] For these reasons, the term "know-do gap," referring to the gap between what is known and what is done in practice, is gaining popularity.[11] The most likely reason behind the spread of this practice is the prevailing controversy among physicians about a unified therapeutic approach.[12]
Only 17% of primary health care physicians had sufficient knowledge of all red flag signs. This rate was considerably lower than a previous report from Italy in which 33% of physicians were able to identify all possible red flags.[13] Meticulous history taking and a physical examination of the patient, specifically directed at the detection of red flag signs in accordance with the clinical guidelines, should reduce the likelihood of missing these danger signs.[8] It is believed that the lack of adherence to existing clinical guidelines is due to a relatively low prevalence of red flags in patients presenting with low back pain. These signs have been reported as present in one in every 200 patients,[6] and a recent study has reported a prevalence of 0.9% among patients presenting with acute low back pain.[14] Because of the low prevalence of these signs, physicians are less likely to encounter them in day-to-day clinical practice and are, therefore, less likely to recognize them.
The results revealed that though the majority of the physicians in the present study were aware of neurological deficits, there was a general lack of knowledge and awareness of red flag signs. This observation, together with concerns about the reliability of red flag signs, further complicates the issue. Three red flags most frequently used in clinical practice for the identification of spinal cord and cauda equina compression include a profound motor or sensory weakness in the lower limbs, bladder and bowel dysfunction, and saddle sensory disturbance.[15] A recently published study investigating the association between three neurological red flag signs with magnetic resonance imaging only reported significant associations between bowel/urinary symptoms and saddle sensory disturbances and the findings of magnetic resonance imaging.[16] Similarly, a study investigating the diagnostic accuracy of a wide range of red flag signs and symptoms and the screening for fracture or malignancy in patients presenting with low back pain reported that the highest post-test probability for the detection of fracture was age >70 years, and for malignancy was a history of malignancy.[17] Moreover, red flag signs used to detect vertebral fractures have also been known to exhibit high false-positive rates.[14,18] These findings highlight the importance of reassessing the existing guidelines to optimize diagnostic accuracy. In addition, there appears to be a need to address the existing knowledge gap about red flag signs among primary health care physicians treating patients with acute low back pain in the local community. This knowledge gap is serious given the morbidity associated with missing red flags signs and the problem of their relatively low prevalence in patients with acute back pain. Emphasis on implementation of clinical practice guidelines in the primary care setting should help increase awareness and improve the care of the patient with back pain. As the Ministry of Health and other institutions develop their own guidelines for the management of low back pain, we should see a significant improvement in the standardization of care, which should subsequently improve the outcomes of the management of the patient with low back pain.
CONCLUSION
The findings of the present study have revealed the inadequacy of the knowledge and awareness of red flag signs among the primary health care physicians in Riyadh who treat patients with acute back pain. The majority of the physicians were not familiar with all of the red flag signs. This might have negative implications in their day-to-day clinical practice. It is, therefore, important to ensure the implementation of guidelines in the local community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine (Phila Pa 1976) 1995;20:11–9. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Cherkin D, Conrad D, Volinn E. Cost, controversy, crisis: Low back pain and the health of the public. Annu Rev Public Health. 1991;12:141–56. doi: 10.1146/annurev.pu.12.050191.001041. [DOI] [PubMed] [Google Scholar]
- 3.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 4.Bigos S, Bowyer O, Braen G, Brown K, Deyo R, Haldeman S, et al. Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services. Rockville, MD: AHCPR Publication No. 95-0642; 1994. Acute Low Back Problems in Adults: Clinical Practice Guideline No. 14. [Google Scholar]
- 5.Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: An international comparison. Spine (Phila Pa 1976) 2001;26:2504–13. doi: 10.1097/00007632-200111150-00022. [DOI] [PubMed] [Google Scholar]
- 6.Rosen M, Breen A, Hamann W, Harber P, Jayson MIV, Kelly E, et al. Management guidelines for back pain. In: Rosen M, editor. Back Pain: Report of a Clinical Standards Advisory Group Committee on Back Pain. London: HMSO; 1994. pp. 49–68. [Google Scholar]
- 7.Shen FH, Samartzis D, Andersson GB. Nonsurgical management of acute and chronic low back pain. J Am Acad Orthop Surg. 2006;14:477–87. doi: 10.5435/00124635-200608000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Little P, Smith L, Cantrell T, Chapman J, Langridge J, Pickering R. General practitioners’ management of acute back pain: A survey of reported practice compared with clinical guidelines. BMJ. 1996;312:485–8. doi: 10.1136/bmj.312.7029.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spring B, Pagoto S, Kaufmann PG, Whitlock EP, Glasgow RE, Smith TW, et al. Invitation to a dialogue between researchers and clinicians about evidence-based behavioral medicine. Ann Behav Med. 2005;30:125–37. doi: 10.1207/s15324796abm3002_5. [DOI] [PubMed] [Google Scholar]
- 10.Craig JC, Irwig LM, Stockler MR. Evidence-based medicine: Useful tools for decision making. Med J Aust. 2001;174:248–53. doi: 10.5694/j.1326-5377.2001.tb143250.x. [DOI] [PubMed] [Google Scholar]
- 11.Pablos-Mendez A, Shademani R. Knowledge translation in global health. J Contin Educ Health Prof. 2006;26:81–6. doi: 10.1002/chp.54. [DOI] [PubMed] [Google Scholar]
- 12.Poitras S, Blais R, Swaine B, Rossignol M. Management of workrelated low back pain: A population-based survey of physical therapists. Phys Ther. 2005;85:1168–81. [PubMed] [Google Scholar]
- 13.Negrini S, Politano E, Carabalona R, Mambrini A. General practitioners’ management of low back pain: impact of clinical guidelines in a non-English-speaking country. Spine (Phila Pa 1976) 2001;26:2727–33. doi: 10.1097/00007632-200112150-00021. [DOI] [PubMed] [Google Scholar]
- 14.Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60:3072–80. doi: 10.1002/art.24853. [DOI] [PubMed] [Google Scholar]
- 15.van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15(Suppl 2):S169–91. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raison NT, Alwan W, Abbot A, Farook M, Khaleel A. The reliability of red flags in spinal cord compression. Arch Trauma Res. 2014;3:e17850. doi: 10.5812/atr.17850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RW, de Vet HC, et al. Red flags to screen for malignancy and fracture in patients with low back pain: Systematic review. BMJ. 2013:347–f7095. doi: 10.1136/bmj.f7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams CM, Henschke N, Maher CG, van Tulder MW, Koes BW, Macaskill P, et al. Red flags to screen for vertebral fracture in patients presenting with low-back pain. Cochrane Database Syst Rev. 2013;1:CD008643. doi: 10.1002/14651858.CD008643.pub2. [DOI] [PubMed] [Google Scholar]


