Abstract
The European Academy of Allergy and Clinical Immunology (EAACI) Task Force defines occupational rhinitis (OR) as “an inflammatory disease of the nose, which is characterized by intermittent or persistent symptoms (i.e., nasal congestion, sneezing, rhinorrea, itching), and/or variable nasal airflow limitation and/or hypersecretion arising out of causes and conditions attributable to a particular work environment and not to stimuli encountered outside the workplace.” The objectives of this review are to highlight the causes of OR in industrial settings in Saudi Arabia in order to alert primary healthcare physicians and other healthcare providers of the importance of diagnosing and managing OR to prevent further complications and present to the General Organization for Social Insurance (GOSI) evidence of the existence of OR in Saudi industrial sector. The literature search yielded no publications from Saudi Arabia that have investigated the prevalence of OR, but it is expected to be high judging from the high prevalence of allergic rhinitis in the country. The occupational groups that are at risk of developing OR include workers in the petrochemical industry, healthcare personnel, livestock and bird breeders, bakers, farmers, housewives and other occupations all of which are present in Saudi Arabia. Clinic and industry based research within Saudi Arabia is recommended to determine the prevalence of OR and to alert healthcare providers to suspect OR in all symptomatic working adults, including housewives and domestic helpers. Use of EAACI algorithm for the diagnosis and management of this condition will help to manage the condition and prevent the deterioration and further complications. Furthermore, diagnosis using internationally recognized guidelines and the results of the suggested epidemiologic surveys may convince GOSI to recognize OR as an occupational disease.
Keywords: Industry in Kingdom of Saudi Arabia, Kingdom of Saudi Arabia, occupational rhinitis, rhinitis
Abstract
ملخص البحث: لا يختلف تعريف السيلان الأنفي المهني الصادر من الهيئة الأكاديمية الأوروبية للحساسية والمناعة السريرية عن تعريف السيلان الأنفي غير المهني، سوى ان المهني تكمن أسبابه في بيئة العمل. تهدف هذه الورقة إلى تسليط الضوء على مسببات التهاب الأنف المهني والتي قد توجد في المصانع بالمملكة العربية السعودية. أثبتت البحوث العالمية انتشار هذا المرض بين العاملين في كثير من المهن مثل مربي المواشي والطيور، والخبازين ، والمزارعين، بالإضافة إلى ربات البيوت ومهن صناعية أخرى منتشرة في المملكة العربية السعودية. وعليه فمن المتوقع إن يكون التهاب الأنف المهني سائداً بين العمال في البيئة الصناعية السعودية وكذلك بين ربات المنازل، ويوصي الكاتب بإجراء الأبحاث المحلية لتحديد مدى انتشاره وذلك بغية لفت انتباه الطبيب المعالج لهذا المرض وكذلك إقناع المؤسسة العامة للتأمينات الاجتماعية لإضافته إلى قائمة الإمراض المهنية.
INTRODUCTION AND DEFINITION
Occupational rhinitis (OR) is defined by the European Academy of Allergy and Clinical Immunology (EAACI) Task Force on OR as “an inflammatory disease of the nose, which is characterized by an intermittent or persistent symptoms (i.e., nasal congestion, sneezing, rhinorrhea, itching), and/or variable nasal airflow limitation and/or hypersecretion due to causes and conditions attributable to a particular work environment and not to stimuli encountered outside the workplace.”[1] Rhinitis, with or without a latency period, may be caused by agents in the workplace, (OR), or preexisting rhinitis that is compounded by occupational exposure (work-exacerbated rhinitis). Rhinitis may also be mixed, or may arise from exposure to irritants or corrosive agents.
Primary healthcare (PHC) centers and specialist hospitals cover the entire Kingdom. The total work force of the government-owned hospitals was reported to be 166,641 in the year 2013. This is in addition to private and other hospitals and medical centers run by different ministries and other government entities.[2] All employees of these healthcare facilities are at risk of various hospital environment-related illnesses including rhinitis.
Manufacturers of basic pharmaceutical products and pharmaceutical preparations did not exist in 1974, but by 2013, 32 pharmaceutical factories were employing more than 7,800 workers.[3]
The General Organization for Social Insurance (GOSI) in Saudi Arabia does not consider OR as an occupational disease, in spite of the fact that industry in Saudi Arabia is both rapidly expanding and diversifying. Oil production, oil refining, and petrochemical industries are the primary industries. This expansion in the industry means more employees are exposed to different types of hazardous materials if proper protective measures are not adopted. According to GOSI's 1432H annual statistical report, the total number of insured employees in the private sector was approximately 15 million and slightly more than 601,000 in the government sector.[4]
Table 1 shows how major industries have developed in Saudi Arabia, other than oil production and healthcare providers, between 1974 and 2013 and the working population in each. Manufacturers of fabricated metal products, except machinery and equipment, ranked first, with providers of food products and beverages ranking second. Furniture industry came fifth with 321 establishments with a work force of 25,002 in the year 2013. The objectives of this review are first to briefly outline the epidemiology and causes of OR and list the important industries in Saudi Arabia that have a high risk of exposure to rhinitis-causing agents to alert healthcare providers in the country, especially primary healthcare physicians, to the importance of diagnosing and managing this condition to prevent progression to asthma and other possible complications. The second objective is to present to GOSI evidence based data on the presence of industries that have a high risk of OR to reconsider its decision of the noninclusion of OR as an occupational disease.
Table 1.
Comparison of examples of major industries in KSA other than oil and petrochemical industry between 1974 and 2013 with possible rhinitis triggering agents and the number of working population[3]
| Economic activity | Factories | Manpower | ||
|---|---|---|---|---|
| 1974 | 2013 | 1974 | 2013 | |
| Manufacture of fabricated metal products, except machinery and equipment | 9 | 880 | 931 | 99,488 |
| Manufacture of food products and beverages | 39 | 875 | 7,199 | 159,107 |
| Manufacture of rubber and plastics products | 11 | 807 | 1,895 | 80,905 |
| Manufacture of chemicals and its products | 9 | 629 | 2,429 | 76,295 |
| Manufacture of furniture | 17 | 321 | 1,295 | 25,002 |
| Manufacture of basic metals | 24 | 247 | 2,801 | 45,711 |
| Manufacture of paper and paper products | 9 | 213 | 843 | 31,286 |
| Manufacture of electrical equipment | 2 | 201 | 464 | 37,419 |
| Manufacture of motor vehicles, trailers and semi-trailers | 8 | 140 | 622 | 14,774 |
| Manufacture of coke, refined petroleum products | 4 | 122 | 3,487 | 27,893 |
| Manufacture of wearing apparel; dressing and dyeing | 2 | 99 | 249 | 12,612 |
| Manufacture of textiles | 1 | 88 | 60 | 14,678 |
| Manufacture of wood and of products of wood and cork, except furniture; manufacture of articles of straw and plaiting materials | 4 | 63 | 839 | 5474 |
| Manufacture of computer, electronic and optical products | 2 | 59 | 33 | 8682 |
| Manufacture of leather and related products | 2 | 37 | 50 | 3676 |
| Manufacture of basic pharmaceutical products and pharmaceutical preparations | — | 32 | — | 7836 |
Adapted from: Saudi Industrial Development Fund. Industrial Development in Saudi Arabia.[3] Available from reference: http://www.sidf.gov.sa/En/INDUSTRYINSAUDIARABIA/Pages/IndustrialDevelopmentinSaudiArabia.aspx. KSA – Kingdom of Saudi Arabia
EPIDEMIOLOGY OF OCCUPATIONAL RHINITIS
Literature is rich with reports on allergic and non-AR with varying prevalence rates. This variation, either overestimation or underestimation, may be due to differences in diagnostic methods used. A very important cause of this variation is the healthy worker effect, which is considered as “the most annoying in studies that attempt to determine the epidemiology of morbidity and mortality among the working population.”[5]
Rhinitis has been identified among the 10 most common reasons for visiting PHC centers.[6] Unfortunately, OR has received relatively little attention on the part of the scientific community worldwide, particularly in Saudi Arabia since it is not considered a serious disease in spite of the fact that it is two to four times more common than occupational asthma (OA) and more frequently precedes the development of asthma.[7]
To the best of our knowledge, no studies have been conducted to determine the prevalence of OR in Saudi Arabia or the Gulf states among the working populations. All studies that have been conducted in this region assessed the prevalence of asthma and or allergic rhinitis (AR) among the school children or adolescents, but the rate of OR was not investigated among the working population of Saudi Arabia.[8] Adding questions about the existence of AR among the parents and their jobs might have given more information about the prevalence of OR among the studied population of parents of the children. Consequently, OR remains an unrecognized health hazard and a socioeconomic problem in spite of the fact that it can be easily diagnosed and managed provided that EAACI guidelines[1] are adopted and followed. Worldwide, OR is a significant cause of loss of productivity. In the absence of this supporting data, GOSI does not recognize OR as an occupational disease that warrants compensation. This leaves several working groups at risk of developing this condition, with the consequent loss of work productivity and personal income.
THE NOSE-LUNG LINK
According to Hurwitz,[9] Galen was the first physician to point to the link between the nose and asthma. A body of literature that demonstrated the existence of a unique link between AR and asthma is now available.[10] However, not all rhinitic patients will develop asthma and conversely not all asthmatics will develop AR.[11] With this relationship in mind, it is important that the treating physician enquires about the nature of the patient's occupation and possible areas of exposure. Housewives should be considered as being employed since the home might be their sole working place.
RISK FACTORS AND CAUSES OF OCCUPATIONAL RHINITIS
After the skin, the respiratory tract ranks as the most commonly affected body part in workers exposed to respiratory insulting agents. Its function as a portal of entry of air makes it vulnerable to the effects of the contaminants in air inhaled at the workplace, which may appear as acute, subacute, or chronic changes adversely affecting the nose's function and structure.[12]
The risk factors for developing OR include atopic status of the individual, type of causative substance and extent of exposure.[1] Some chemical allergens at the workplace are more potent in causing OR than others, such as acid anhydrides, isocyanates and acrylic compounds.[13] Other reported risk factors include working as fur handlers, bakers and livestock breeders.[14] The association between smoking and the risk for developing allergic rhinitis is debatable.[15]
These agents in the working environment as well as in homes contain various types of substances that can cause allergic (immunoglobulin E [IgE] mediated or non-IgE mediated), nonallergic, irritant or corrosive rhinitis. The latter is a form of severe occupational irritant rhinitis.[1,16]
Table 2 shows examples of OR-causing agents that are expected to prevail in the Saudi Arabia working environments. For the low-molecular-weight, (LMW) substances, such as diisocyanate, plicatic acid, acid anhydrides and platinum salts to induce allergy, they must be conjugated to a protein to act as allergens.[17] Rhinitis arising from exposure to LMW agents is not severe. However, it frequently appears before OA following exposure to high-molecular-weight agents.[18]
Table 2.
Examples of occupational rhinitis-causing agents that are expected to be encountered in Saudi Arabia occupational environments
| Allergen | Occupations |
|---|---|
| High molecular weight compounds (proteins) | |
| Animal antigens (rat, mouse, rabbit, guinea pigs) | Animal handlers, farmers, veterinarians, research laboratory workers |
| Natural rubber latex | Healthcare workers, hairdressers |
| Green coffee bean and castor bean | Dock workers |
| Proteolytic enzymes | Soap and detergent workers, cosmetologist |
| Gum arabic/gum acacia | Printers, food workers |
| Psyllium | Healthcare workers, pharmacists, nurses |
| Alpha-amylase, grain and flour dust | Bakers, farmers, grain handlers, grain elevator operators |
| Insects and mites | Bakers, farmers, animal handlers, research laboratory workers |
| Mold spores | Farmers, housewives |
| Pollens and other plant allergens | Farmers, florists, greenhouse workers |
| Grain mite | Grain-store (silos’) workers |
| Fruit fly (Drosophila melanogaster) | Research laboratory workers |
| Fungal amylase | Bakers |
| Low molecular weight compounds (haptens)* | |
| Colophony fume; from soldering | Electronics workers |
| Formaldehyde, methacrylate, glutaraldehyde | Healthcare workers, pharmacists |
| Isocyanates | Boat builders, car painters, animal skin and hides tanners |
| Laundry detergents | Laundry workers |
| Persulfate salts | Hairdressers |
| Acid anhydrides: Phthalic anhydride, trimellitic anhydride, maleic anhydride | Plastics, adhesives, service coatings, epoxy resin production, and electric condenser workers |
| Platinum salts | Platinum refinery |
| Wood dust containing abietic acid and plicatic acid | Carpenters, saw mill workers, furniture making |
| Polyvinyl chloride | Manufacturing industry |
| Styrene | Plastic industry |
| Drugs: Psyllium, spiramycin, piperacillin sodium | Healthcare workers |
| Ninhydrin | Research laboratory workers |
| 1,2-benzisothiazolin-3-one | Detergents production, laboratory workers, laundry workers |
*Must be conjugated to a protein to act as an allergen[17]
Allergy following handling of laboratory animals is not uncommon. The commonest symptoms were in the nose and eye.[19] OR among bakers is estimated to be 1.5-3.4 times more than bakers’ asthma.[16] The commonest allergens are cereal flours, enzymes (α-amylase), insects (Sitophilus granarius) and fungal molds (Alternaria and Aspergillus). Bleaching agents containing persulfate, as used by hairdressers, cause rhinitis, asthma, and other allergic conditions, but the immunologic mechanism is so far not clearly understood.[20] Welders are exposed to different types of gases and fumes, the types of which depend on the base metal, the coating, the electrode used and the type of welding. An unusual case of OR was reported following exposure to welding fumes from galvanized steel. According to the authors of that publication, this was the first case to be reported arising from inhalation of such fumes. The diagnosis was confirmed by an inhalation challenge.[21]
Farm working is unique in that the farmer is exposed to different kinds of allergic and nonallergic substances besides adverse weather conditions, all of which constitute a hazard to the farmer. Storage mites and cow's dander are the commonest causes of OR in this occupational group.[22] A recent study reported for the first time OR arising from capsaicin, which is the main chemical in chili, in a worker at a red pepper grinding mill. The symptoms disappeared after the worker changed his/her job.[23]
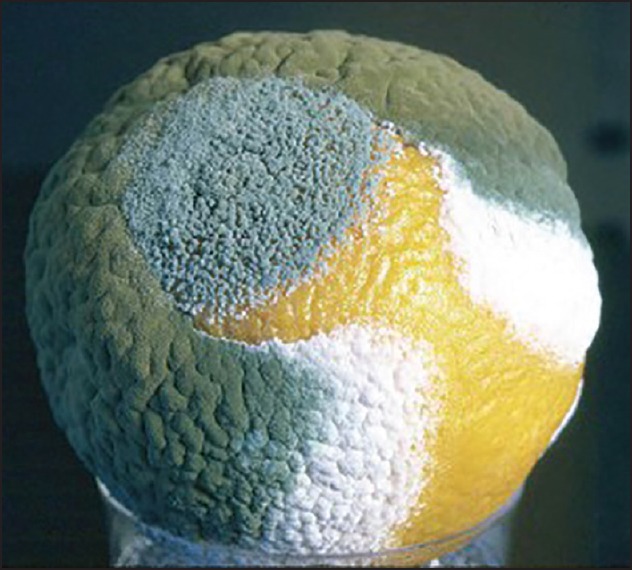
Wood working and furniture industry are very prevalent in Saudi Arabia. Studies have proven the occurrence of OR with or without bronchial asthma arising from exposure to western red cedar wood dust and several other types of wood, such as obeche, cedroarana, birch, and beech.[24] Colophony (or rosin, used as a flux in electronic industries), is obtained from pine trees containing abietic acid. OR arising from workers inhaling colophony employed in the electronic industry is more common among female workers (24%) than males (9%).[25] Healthcare workers are at risk of OR due to possible exposure to different allergens, including formaldehyde, glutaraldehyde, drugs, natural rubber latex (gloves), while working in a hospital environment. A dentist developed OR from inhaling Nobetec, which is a temporary dental filling material that contains colophony.[26] The domestic environment is home for several rhinitis-causing agents. House dust mites, pet animals, pyrethrum insecticide, molds, and other chemicals are commonly present in the domestic environment. The dominant indoor fungi are Aspergillus fumigatus [Figure 1] Aspergillus clavatus [Figure 2], Mucor [Figure 3], and Penicillium notatum [Figure 4] species.[27]
Figure 1.
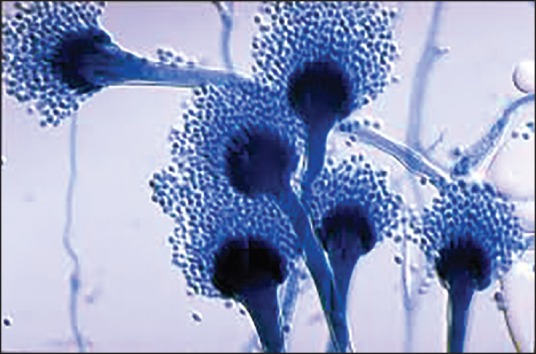
Aspergillus fumigatus. Source: http://www.pfdb.net/photo/mirhendi_h/box020909/standard/a_fumigatus_s.jpg
Figure 2.

Aspergillus clavatus. Source: https://en.wikipedia.org/wiki/Aspergillus_clavatus#/media/File:Aspergillus_clavatus.jpg
Figure 3.

Mucorfungus. Source: https://classconnection.s3.amazonaws.com/732/flashcards/2749732/png/1-1424568956D5C2FC3B1.png
Figure 4.
Penicillium notatum. Source: https://microbewiki.kenyon.edu/index.php/Penicillium
Indoor molds are a real hazard in the coastal regions of Saudi Arabia as a result of the humid environments in these areas, mainly in the summer months. Molds flourish in damp environments and can be a cause of rhinitis and other adverse health problems. A study conducted in Bangladesh, involving 548 doctor-diagnosed AR cases, revealed that 30.3% of the patients were housewives, and house dust mites were the cause of 76.3% of the cases.[28] Another study conducted in Finland found that out of a total of 369 subjects, 60 (16%) subjects exposed to molds had OR. The most common mold identified was A. fumigatus.[29] From a total of 90 patients attending an AR clinic in Malaysia, approximately 25% were housewives. The allergens investigated were house dust mite (Dermatophagoides pteronyssinus), domestic cat, Mucor (fungus), wheat flour, and some food items. Dust and food items were the most common allergens, 92.2%, and 48.9%, respectively.[30]
SYMPTOMS OF OCCUPATIONAL RHINITIS
The symptoms, which may appear as early or late responses, are less severe when LMW allergens are involved.[18] These symptoms may sometimes be associated with systemic symptoms such as fatigue,[31] and more often appear prior to the onset of OA when high-molecular-weight agents are the causative substances.[10,18]
SOCIOECONOMIC IMPACT OF OCCUPATIONAL RHINITIS
Since occupational and non-OR share the same symptoms, they most probably share the same socioeconomic impact with both direct and indirect costs. The direct costs are the use of resources in terms of consultations and prices of medications.[32] Some patients may resort to over-the-counter medications at their own expense. The indirect costs are loss of productivity, worsening of symptoms, and absenteeism.[1] The cost increases with the severity of the condition. Moreover, AR causes besides distress, and discomfort, sickness absence, and greatly affects the workers’ quality of life.[33]
More than half of 8,267 employees working in 47 United States (US) industrial sites experienced symptoms of AR on average for 52.5 days/year and absenteeism mounted to 3.6 days/ year, while being unproductive was 2.3 hours/workday when they have symptoms. Productivity losses per year per affected person due to absenteeism and presenteeism combined were nearly 600 US dollars.[34]
Adverse effects on workers’ performance were more related to the severity of the condition rather than the duration.[33] Others reported a drop in productivity by 20% on days when the symptoms are severe.[35] Nasal congestion was the one mostly blamed.[36] OR disturbs night-time sleep and consequently reduces productivity at work, thereby presenting a burden on employers.[37] Another report found that the quality of life improved after treatment of OR,[38] or on leaving the job.[38,39] Interestingly, the effect on quality of life is worse for those whose OR resulted from exposure to high-molecular-weight agents. However, the authors stated no explanation for this phenomenon.[40]
DIAGNOSIS
Accurately distinguishing OR from non-OR will preserve health and prevent unnecessary socioeconomic costs to both employers and employees. The close link between OR and asthma and its effect on quality of life, leading to absenteeism, presenteeism, in addition to the direct costs to healthcare and loss of productivity make it prudent to consider the possibility of OR in the routine clinical assessment of the condition.[41]
EAACI position paper on OR outlined a consensus diagnostic algorithm of OR that starts with a detailed clinical and medical history.[1] OR should be suspected in a patient presenting with:
Sneezing.
Nasal itching.
Congestion.
Rhinorrhea, with or without variable nasal airflow blocking and/or hypersecretion.[1]
Furthermore, such patients should always be assessed to rule out the co-existence of bronchial asthma.[42] These are considered the important components to the workup of a rhinitis patient to rule out other causes of rhinitis and establish work-relatedness.[43]
Information about the type of occupation is required. Bernardino Ramazzini, the late Italian physician and father of occupational medicine, in his book “De Morbis Artificum Diatriba” recommended asking the patient about the type of the job he or she does: “liceatquoque interrogationem hanc adiicere, and quam artem exerceat” (I may venture to add one more question: What occupation does he follow?).[44] Occupational history questions should seek to address at least the following. Some of these questions may be modified to suit a housewife:
What is the nature of his or her work? (work process).
What is the nature of the substances the patient handles? (presence of causative agents).
Has he or she been exposed to similar or other substances in the past that caused similar complaints? (past exposures).
Is there a history of head trauma? (exclude cerebrospinal fluid leak).
Did he or she suffer from an allergy or asthma before taking the current job? (past medical history/risk factors).
Is there a family history of allergy, exposure to domestic pets, animals, etc.? (risk factors).
What are the frequency and environmental level of current exposures? (current exposures).
How does he or she feel when not in the work environment; on vacation and over weekends, etc.? (work/resume pattern).
How soon after taking the job did he or she develop the symptoms? (latency period).
Do any of the coworkers have similar symptoms? (morbidity among workmates).
What is the impact of the rhinitis symptoms upon their quality of life? (assessing risk on quality of life)
Is personal protective equipment (PPE) provided in the workplace? (safety concerns).
If PPE is provided, does he or she use it regularly? (safety concerns).
In a subsequent visit, the patient may be asked to bring the safety data sheet for the substance being handled, if this is available, or in the case of a housewife, she may bring the container of the substance, which might contain information on the composition of the substance. An objective examination might require equipment which may not be available at PHC centers or at an industrial healthcare facility. In this case, patients requiring a more thorough examination should be referred to an otolaryngologist and/or allergologist.
According to Hougaard et al. the specific inhalation challenge test is the “gold standard” for the diagnosis of OR and asthma.[17] However, use of the nasal provocation test (NPT) is not recommended for diagnosing OR arising from exposures in damp and moldy workplaces because of the low sensitivity of the test.[45] Lung function testing to rule out concomitant bronchial asthma is recommended.[46] Skin testing using the extracts of specific allergens can be used, as in the case of latex allergy in employees routinely using natural rubber gloves.[ 47]
A verbal description of the task may not always give a clear picture of the hazard. For this reason a visit to the workplace (walk-through) by the attending physician, assisted by personnel experts in occupational health, is strongly advised. However, the physicians at PHC centers and hospitals may not be able to do this. This site visit may give helpful insights to the patient's exposure. It is specially recommended when NPT is not possible. If neither the workplace visit nor the nasal provocation test is possible, the patient may be asked to take days off work, but before returning to work, the patient should visit the treating physician again to provide details of the condition during this stop/resume period. Relief from the symptoms during this period supports a diagnosis of OR.[48]
MANAGEMENT
Because of the adverse effects of OR on the patient's quality of life and the possible development of asthma it behooves us, as healthcare providers, to properly manage OR to keep the affected person gainfully employed by preventing deterioration in the quality of life and the development of OA.[42] These objectives can be achieved through two management lines, nonpharmacologic and pharmacologic.
Nonpharmacological management
Primary prevention
The EAACI Task Force on OR has detailed the line of management of this condition,[1] which starts with primary prevention through complete avoidance of the causative agent by a process of elimination.[49] Primary prevention is important, and an effective means to control occupationally-related diseases to prevent cases from ever developing. It is based on performing a risk assessment of the task with the objective of anticipating exposure to the possible agent. The next step is recognition; determining the nature of the suspected agent(s) in addition to observing the work being performed. Whenever facilities are available, air samples, using personal and mobile samplers, may be collected and analyzed to determine the types of pollutants and the levels of each. The next move is evaluation and finally implementing the appropriate control measures.
For an industrial healthcare facility to have effective medical services, it is necessary that the physician go down to the shop floor to watch the industrial processes and anticipate the possible sources and types of hazards that might arise. This, together with environmental measurements, will help to design a workplace control program. If the elimination is not possible, engineering control is the alternative to reducing the concentration of the offending agent by redesigning the workplace and local exhaust ventilation. Reducing the level of substances in the workplace has proved to be successful in preventing some occupational diseases.[50] This reduction will be effective for nonallergenic agents, but does not apply to sensitizing substances since exposure to very low concentrations can trigger an attack of rhinitis once sensitization has occurred. In this case, placement of the sensitized employee in another job with no similar substance is the alternative. Administrative control may involve, after the relocation of the affected employee, re-training of the worker if need be. Use of PPE, such as masks with filters, is recommended only if first line measures are not possible or inefficient.
The usefulness of preemployment (preplacement) examination is questioned, and more evidence is required to justify its routine use. However, this generalization with respect to preplacement medical examination does not apply when the work requires a high standard of fitness to match the job requirements, or when the safety of work colleagues is of concern.[51] Its use to exclude the atopics from exposure may be viewed as discriminatory.[52]
Remediation measures should be implemented to prevent the growth of molds in damp workplaces. Occupational Safety and Health Administration, United States of America, has clear guidelines for preventing mold growth. The guidelines stress the need to regularly check the drainage systems of buildings to identify and eliminate sources of dampness and humidity and clean and dry all moldy materials.[53] Allergens in the home environment should also be controlled to control indoor allergens.[46]
Worker education is very effective in reducing and controlling OR. Workers have the right “to know” what materials they are handling, how to handle it, the possible health hazards, and ways and use of PPE.
Secondary prevention
The values of health surveillance programs, secondary prevention, go beyond enabling the early identification of possible adverse health effects on individuals. It contributes to the process of hazard and risk assessment. Such programs may include the use of questionnaires, skin prick tests with or without determination of serum specific IgE antibodies (depending upon availability), and consultation with specialized medical personnel for assessment of symptomatic workers. Whenever respiratory symptoms are present, these should be further investigated to unearth any work-relatedness. It is recommended that all those employed in high risk work sites should be examined soon after starting work, preferably within the first 2-5 years, because of the short latency period between exposure to some rhinitis-causing agents, such as laboratory rats, and the appearance of the symptoms.[54] Health surveillance of workers exposed to detergent enzymes in the soap and detergent industry is recommended to be conducted biannually for the first 2 years following employment and yearly thereafter.[55]
Consultation with an allergologist/immunologist is an opportunity for the patient to receive education on rhinitis and allergen avoidance in addition to preventing and managing asthma. This has been found to have a positive impact on compliance, quality of life, and patient's satisfaction.[46]
Pharmacologic management
It is the duty of the attending physician to understand the needs of his patient if he is to deliver comprehensive management. Pharmacotherapy is indicated as an alternative of management when elimination is not possible.[1] The use of drugs to control allergic OR is not different from pharmacotherapy of nonoccupational AR.[43] The choice of medication very much depends on the type and severity of the condition. However, when managing patients it is vital to ensure their compliance with the medication. Smell and taste of intranasal corticosteroids must be acceptable to the patient to achieve satisfactory compliance.[56]
Second-generation antihistamines are safer than the first-generation since the latter are known to cause sedation. However, some of the former group, such as cetirizine and intranasal azelastine, can sometimes cause sedation even when the recommended dose has not been exceeded, unlike desloratadine and loratadine which cause this side effect only when the recommended dose has been exceeded.[57] These sedating antihistamines should, therefore, be avoided since they are considered as a risk factor for accidents.
Allergen immunotherapy is not recommended for most patients since at present there are either no therapeutic extracts available or what is available is not safe except for natural rubber latex (NRL). Even with NRL the results were not impressive.[58] Other modalities of pharmacotherapy for allergic non-OR equally apply to allergic OR.
CONCLUSIONS AND RECOMMENDATIONS
AR is prevalent in Saudi Arabia. However, OR, on the other hand, remains underdiagnosed because of both the lack of related research within Saudi Arabia and awareness of the healthcare workers of its adverse health and socioeconomic impact on employees. Moreover, it will remain a cause of loss of productivity to industries unless its prevalence has been determined and the condition properly managed:
-
This being said, it is imperative that research be conducted in Saudi Arabia to determine its prevalence. Research can be industry and clinics-based surveys:
- SABIC industrial complexes have health records for each employee. These can be a source for preventing OR among this working population. Such a record might convince GOSI to add OR to the list of occupational diseases.
- A country-wide clinic-based data collection of representative samples of patients’ records from PHC centers and hospitals is a good source of data on rhinitis. This might initiate the researchers to conduct industry-based studies to determine the exact prevalence of this condition at the industrial level.
Regarding diagnosis and management, OR can be easily diagnosed and managed. What is required from the attending physician is to suspect OR in all symptomatic working adults, including housewives and domestic helpers. Use of the EAACI algorithm will help diagnose and manage the condition, in addition to preventing deterioration and complications. Furthermore, use of these guidelines, besides the results of epidemiologic surveys, may convince the GOSI to accept OR as an occupational disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Moscato G, Vandenplas O, Gerth Van Wijk R, Malo JL, Quirce S, et al. EAACI Task Force on Occupational Rhinitis. Occupational rhinitis. Allergy. 2008;63:969–80. doi: 10.1111/j.1398-9995.2008.01801.x. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health, Saudi Arabia. Statistical Annual Health Report, 1434 H, 2013G. [Last accessed on 2013 Dec 23]. Available from: http://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/Statistics-Book-1434.pdf .
- 3.Saudi Industrial Development Fund. Industrial Development in Saudi Arabia (Quoting Operational Industrial Projects System “OIPS”) [Last accessed on 2013 Dec 23]. Available from: http://www.sidf.gov.sa/En/INDUSTRYINSUDIARABIA/Pages/IndustrialDevelopmentinSaudiArabia.aspx .
- 4.General Organization for Social Insurance. Annual Statistical Report 1432 H. [Last accessed on 2013 Dec 23]. Available from: http://www.gosi.gov.sa/portal/web/guest/statistics/view-statistic?StatisticsId=423367 .
- 5.Li CY, Sung FC. A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 1999;49:225–9. doi: 10.1093/occmed/49.4.225. [DOI] [PubMed] [Google Scholar]
- 6.Gregory C, Cifaldi M, Tanner LA. Targeted intervention programs: Creating a customized practice model to improve the treatment of allergic rhinitis in a managed care population. Am J Manag Care. 1999;5:485–96. [PubMed] [Google Scholar]
- 7.Moscato G, Vandenplas O, Van Wijk RG, Malo JL, Perfetti L, Quirce S, et al. EAACI position paper on occupational rhinitis. Respir Res. 2009;10:16. doi: 10.1186/1465-9921-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Frayh AR, Shakoor Z, Gad El Rab MO, Hasnain SM. Increased prevalence of asthma in Saudi Arabia. Ann Allergy Asthma Immunol. 2001;86:292–6. doi: 10.1016/s1081-1206(10)63301-7. [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz B. Nasal Pathophysiology impacts bronchial reactivity in asthmatic patients with allergic rhinitis. J Asthma. 1997;34:427–31. doi: 10.3109/02770909709055385. [DOI] [PubMed] [Google Scholar]
- 10.Vandenplas O, Van Brussel P, D’Alpaos V, Wattiez M, Jamart J, Thimpont J. Rhinitis in subjects with work-exacerbated asthma. Respir Med. 2010;104:497–503. doi: 10.1016/j.rmed.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Vignola AM, Chanez P, Bousquet J. The relationship between asthma and allergic rhinitis: Exploring the basis for a common pathophysiology. Clin Exp Allergy. 2003;3:63–8. [Google Scholar]
- 12.Shusterman D. Occupational irritant and allergic rhinitis. Curr Allergy Asthma Rep. 2014;14:425. doi: 10.1007/s11882-014-0425-9. [DOI] [PubMed] [Google Scholar]
- 13.Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: Prevalence, aetiology and determinants. Clin Exp Allergy. 2000;30:1519–34. doi: 10.1046/j.1365-2222.2000.00946.x. [DOI] [PubMed] [Google Scholar]
- 14.Di Stefano F, Verna N, Di Giampaolo L, Schiavone C, Di Gioacchino G, Balatsinou L, et al. Occupational asthma due to low molecular weight agents. Int J Immunopathol Pharmacol. 2004;17(2 Suppl):77–82. doi: 10.1177/03946320040170S213. [DOI] [PubMed] [Google Scholar]
- 15.Malo JL, Lemière C, Desjardins A, Cartier A. Prevalence and intensity of rhinoconjunctivitis in subjects with occupational asthma. Eur Respir J. 1997;10:1513–5. doi: 10.1183/09031936.97.10071513. [DOI] [PubMed] [Google Scholar]
- 16.Muzembo BA, Eitoku M, Inaoka Y, Oogiku M, Kawakubo M, Tai R, et al. Prevalence of occupational allergy in medical researchers exposed to laboratory animals. Ind Health. 2014;52:256–61. doi: 10.2486/indhealth.2012-0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hougaard MG, Menné T, Søsted H. Occupational eczema and asthma in a hairdresser caused by hair-bleaching products. Dermatitis. 2012;23:284–7. doi: 10.1097/DER.0b013e318275968c. [DOI] [PubMed] [Google Scholar]
- 18.Castano R, Suarthana E. Occupational rhinitis due to steel welding fumes. Am J Ind Med. 2014;57:1299–302. doi: 10.1002/ajim.22365. [DOI] [PubMed] [Google Scholar]
- 19.Linaker C, Smedley J. Respiratory illness in agricultural workers. Occup Med (Lond) 2002;52:451–9. doi: 10.1093/occmed/52.8.451. [DOI] [PubMed] [Google Scholar]
- 20.Nam YH, Jin HJ, Hwang EK, Shin YS, Ye YM, Park HS. Occupational rhinitis induced by capsaicin. Allergy Asthma Immunol Res. 2012;4:104–6. doi: 10.4168/aair.2012.4.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schlünssen V, Sigsgaard T, Raulf-Heimsoth M, Kespohl S. Workplace exposure to wood dust and the prevalence of wood-specific Sensitization. Allergologie. 2012;8:402–12. doi: 10.5414/ALX01503E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burge PS, Edge G, Hawkins R, White V, Taylor AJ. Occupational asthma in a factory making flux-cored solder containing colophony. Thorax. 1981;36:828–34. doi: 10.1136/thx.36.11.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piirilä P, Hodgson U, Estlander T, Keskinen H, Saalo A, Voutilainen R, et al. Occupational respiratory hypersensitivity in dental personnel. Int Arch Occup Environ Health. 2002;75:209–16. doi: 10.1007/s00420-001-0302-4. [DOI] [PubMed] [Google Scholar]
- 24.Chowdary VS, Prasanna L, Sangram V, Rani S, Vinay Kumar EC. Role of Fungi (molds) in allergic airway disease — An analysis in a South Indian Otolaryngology center. Indian J Allergy Asthma Immunol. 2011;25:67–78. [Google Scholar]
- 25.Nepali R, Sigdel B, Baniya P. Symptomatology and allergen types in patients presenting with allergic rhinitis. Bangladesh J Otorhinolaryngol. 2012;18:30–5. [Google Scholar]
- 26.Karvala K, Nordman H, Luukkonen R, Nykyri E, Lappalainen S, Hannu T, et al. Occupational rhinitis in damp and moldy workplaces. Am J Rhinol. 2008;22:457–62. doi: 10.2500/ajr.2008.22.3209. [DOI] [PubMed] [Google Scholar]
- 27.Asha’ari ZA, Yusof S, Ismail R, Che Hussin CM. Clinical features of allergic rhinitis and skin prick test analysis based on the ARIA classification: A preliminary study in Malaysia. Ann Acad Med Singapore. 2010;39:619–24. [PubMed] [Google Scholar]
- 28.Cakir E, Ersu R, Uyan ZS, Oktem S, Varol N, Karakoc F, et al. The prevalence and risk factors of asthma and allergic diseases among working adolescents. Asian Pac J Allergy Immunol. 2010;28:122–9. [PubMed] [Google Scholar]
- 29.Hytönen M, Kanerva L, Malmberg H, Martikainen R, Mutanen P, Toikkanen J. The risk of occupational rhinitis. Int Arch Occup Environ Health. 1997;69:487–90. doi: 10.1007/s004200050178. [DOI] [PubMed] [Google Scholar]
- 30.Saulyte J, Regueira C, Montes-Martínez A, Khudyakov P, Takkouche B. Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: A systematic review and meta-analysis. PLoS Med. 2014;11:e1001611. doi: 10.1371/journal.pmed.1001611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quillen DM, Feller DB. Diagnosing rhinitis: Allergic vs.nonallergic. Am Fam Physician. 2006;73:1583–90. [PubMed] [Google Scholar]
- 32.Gupta R, Sheikh A, Strachan DP, Anderson HR. Burden of allergic disease in the UK: Secondary analyses of national databases. Clin Exp Allergy. 2004;34:520–6. doi: 10.1111/j.1365-2222.2004.1935.x. [DOI] [PubMed] [Google Scholar]
- 33.Camelo-Nunes IC, Solé D. Allergic rhinitis: Indicators of quality of life. J Bras Pneumol. 2010;36:124–33. doi: 10.1590/s1806-37132010000100017. [DOI] [PubMed] [Google Scholar]
- 34.Lamb CE, Ratner PH, Johnson CE, Ambegaonkar AJ, Joshi AV, Day D, et al. Economic impact of workplace productivity losses due to allergic rhinitis compared with select medical conditions in the United States from an employer perspective. Curr Med Res Opin. 2006;22:1203–10. doi: 10.1185/030079906X112552. [DOI] [PubMed] [Google Scholar]
- 35.Meltzer EO, Gross GN, Katial R, Storms WW. Allergic rhinitis substantially impacts patient quality of life: Findings from the Nasal Allergy Survey Assessing Limitations. J Fam Pract. 2012;61(2 Suppl):S5–10. [PubMed] [Google Scholar]
- 36.Storms W. Allergic rhinitis-induced nasal congestion: Its impact on sleep quality. Prim Care Respir J. 2008;17:7–18. doi: 10.3132/pcrj.2008.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stewart M, Ferguson B, Fromer L. Epidemiology and burden of nasal congestion. Int J Gen Med. 2010;3:37–45. doi: 10.2147/ijgm.s8077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saverno KR, Seal B, Goodman MJ, Meyer K. Economic evaluation of quality-of-life improvement with second-generation antihistamines and montelukast in patients with allergic rhinitis. Am Health Drug Benefits. 2009;2:309–16. [PMC free article] [PubMed] [Google Scholar]
- 39.Gerth van Wijk R, Patiwael JA, de Jong NW, de Groot H, Burdorf A. Occupational rhinitis in bell pepper greenhouse workers: Determinants of leaving work and the effects of subsequent allergen avoidance on health-related quality of life. Allergy. 2011;66:903–8. doi: 10.1111/j.1398-9995.2011.02556.x. [DOI] [PubMed] [Google Scholar]
- 40.Miedinger D, Gautrin D, Castano R. Upper airway symptoms among workers with work-related respiratory complaints. Occup Med (Lond) 2012;62:427–34. doi: 10.1093/occmed/kqs131. [DOI] [PubMed] [Google Scholar]
- 41.Moscato G, Siracusa A. Rhinitis guidelines and implications for occupational rhinitis. Curr Opin Allergy Clin Immunol. 2009;9:110–5. doi: 10.1097/aci.0b013e328328cfe7. [DOI] [PubMed] [Google Scholar]
- 42.Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen) Allergy. 2008;63(Suppl 86):8–160. doi: 10.1111/j.1398-9995.2007.01620.x. [DOI] [PubMed] [Google Scholar]
- 43.Slavin RG. Occupational rhinitis. Ann Allergy Asthma Immunol. 2003;90(5 Suppl 2):2–6. doi: 10.1016/s1081-1206(10)61640-7. [DOI] [PubMed] [Google Scholar]
- 44.Franco G. Ramazzini and workers’ health. Lancet. 1999;354:858–61. doi: 10.1016/S0140-6736(99)80042-7. [DOI] [PubMed] [Google Scholar]
- 45.Karvala K, Nordman H, Luukkonen R, Nykyri E, Lappalainen S, Toskala E. Occupational rhinitis in damp and moldy workplace. J Allergy Clin Immunol. 2008;121(Suppl 1):S182. doi: 10.2500/ajr.2008.22.3209. [DOI] [PubMed] [Google Scholar]
- 46.Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, et al. The diagnosis and management of rhinitis: An updated practice parameter. J Allergy Clin Immunol. 2008;122(2 Suppl):S1–84. doi: 10.1016/j.jaci.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 47.Archambault S, Malo JL, Infante-Rivard C, Ghezzo H, Gautrin D. Incidence of sensitization, symptoms, and probable occupational rhinoconjunctivitis and asthma in apprentices starting exposure to latex. J Allergy Clin Immunol. 2001;107:921–3. doi: 10.1067/mai.2001.114116. [DOI] [PubMed] [Google Scholar]
- 48.Moscato G, Pignatti P, Yacoub MR, Romano C, Spezia S, Perfetti L. Occupational asthma and occupational rhinitis in hairdressers. Chest. 2005;128:3590–8. doi: 10.1378/chest.128.5.3590. [DOI] [PubMed] [Google Scholar]
- 49.LaMontagne AD, Radi S, Elder DS, Abramson MJ, Sim M. Primary prevention of latex related sensitisation and occupational asthma: A systematic review. Occup Environ Med. 2006;63:359–64. doi: 10.1136/oem.2005.025221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sarlo K. Control of occupational asthma and allergy in the detergent industry. Ann Allergy Asthma Immunol. 2003;90(5 Suppl 2):32–4. doi: 10.1016/s1081-1206(10)61646-8. [DOI] [PubMed] [Google Scholar]
- 51.Pachman J. Evidence base for pre-employment medical screening. Bull World Health Organ. 2009;87:529–34. doi: 10.2471/BLT.08.052605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilken D, Baur X, Barbinova L, Preisser A, Meijer E, Rooyackers J, et al. What are the benefits of medical screening and surveillance? Eur Respir Rev. 2012;21:105–11. doi: 10.1183/09059180.00005011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Occupational Safety and Health Administration. U.S. Department of Labor. Preventing Mold-Related Problems in the Indoor Workplace. A Guide for Building Owners, Managers and Occupants. OSHA 3304-04N. 2006. [Last accessed on 2014 Dec 30]. Available from: https://www.osha.gov/Publications/preventing_mold.pdf .
- 54.Cullinan P, Cook A, Gordon S, Nieuwenhuijsen MJ, Tee RD, Venables KM, et al. Allergen exposure, atopy and smoking as determinants of allergy to rats in a cohort of laboratory employees. Eur Respir J. 1999;13:1139–43. doi: 10.1034/j.1399-3003.1999.13e33.x. [DOI] [PubMed] [Google Scholar]
- 55.Nicholson PJ, Newman Taylor AJ, Oliver P, Cathcart M. Current best practice for the health surveillance of enzyme workers in the soap and detergent industry. Occup Med (Lond) 2001;51:81–92. doi: 10.1093/occmed/51.2.081. [DOI] [PubMed] [Google Scholar]
- 56.Mahadevia PJ, Shah S, Leibman C, Kleinman L, O’Dowd L. Patient preferences for sensory attributes of intranasal corticosteroids and willingness to adhere to prescribed therapy for allergic rhinitis: A conjoint analysis. Ann Allergy Asthma Immunol. 2004;93:345–50. doi: 10.1016/S1081-1206(10)61393-2. [DOI] [PubMed] [Google Scholar]
- 57.Simons FE, Simons KJ. H1 antihistamines: Current status and future directions. World Allergy Organ J. 2008;1:145–55. doi: 10.1186/1939-4551-1-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nettis E, Colanardi MC, Soccio AL, Marcandrea M, Pinto L, Ferrannini A, et al. Double-blind, placebo-controlled study of sublingual immunotherapy in patients with latex-induced urticaria: A 12-month study. Br J Dermatol. 2007;156:674–81. doi: 10.1111/j.1365-2133.2006.07738.x. [DOI] [PubMed] [Google Scholar]


