Abstract
Pulmonary rehabilitation is recommended to restore chronic obstructive pulmonary disease (COPD) patients’ abilities to the highest level of independency and functionality. Telehealth has the potential to improve rehabilitation programs and to enhance patients’ participation. However, little is known about the potential benefits of using telehealth in providing rehabilitation for COPD patients at home. The purpose of this review was to provide a narrative synthesis of literature of studies, which use telehealth with video components to provide real-time pulmonary rehabilitation for COPD patients. An electronic database search was performed in the Ovid Medline, CINAHL, and PubMed databases. Seven eligible studies were included based on the inclusion criteria. Based on the included studies, using telehealth to provide real-time interactive pulmonary rehabilitation for COPD patients at home is feasible and acceptable, and can provide clinical and social positive benefits. A knowledge gap regarding feasibility, acceptance, and benefits of using telehealth to provide real-time pulmonary rehabilitation services still exists.
Keywords: Chronic obstructive pulmonary disease, pulmonary rehabilitation, real-time home monitoring, real-time telerehabilitation, telehealth
Abstract
ملخص البحث: يعتبر التأهيل الرئوي من أهم طرق العلاج للمرضى الذين يعانون من مرض الانسداد الرئوي المزمن، وذلك للتمكن من التغلب على أعراض المرض ولزيادة قدرة المريض على التعايش معه ورفع أدائه الوظيفي والحيوي من جهة أخرى. برز حديثاً فكرة تقديم الرعاية الصحية للمرضى في المنزل عن طريق استخدام الانترنت وتقنية الاتصالات. تتيح هذه التقنية لمقدمي الرعاية الصحية العمل على تطوير برامجهم وجعلها أكثر ملاءمة للمريض من حيث الوقت وسهوله الوصول، مما يساعد على رفع معدلات المشاركة في هذه البرامج والاستفادة منها. يهدف هذا البحث لجمع وتلخيص ما توصلت إليه الأبحاث والدراسات بخصوص استخدام الانترنت وبالفيديو لتقديم برامج التأهيل الرئوي للمرضى في المنزل. اعتمد البحث على ما نشر في المجلات العلمية المحكمة فقط. وبين البحث الالكتروني سبعه دراسات مطابقة لهدف الباحث. واعتمادا على ملخص هذه الدراسات يمكن استنتاج إمكانية استخدام الانترنت لتقديم برامج تأهيل رئوي للمرضى في المنزل. وكان استخدام الانترنت في جلسات التأهيل الرئوي مقبولا من قبل المرضى ومقدمي الخدمة . ولازالت الحاجة قائمة لمزيد من الأبحاث للتعمق في مدى قبول المستخدمين لهذه التقنية وفوائدها المستقبلية على المرضى ولمقدمي الخدمة ، وعلى النظام الصحي ككل.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema, can be defined as “a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. The airflow limitation associated with COPD is usually progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.”[1] COPD is one of the major causes of morbidity and mortality worldwide.[2] According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases became the third leading cause of death in the USA in 2011.[3] More than half of all COPD patients (51%) have reported that their COPD condition disturbs their sleep, limits their ability to work, limits their physical activities, and limits their family and social activities.[4] The direct medical cost of COPD in the USA, in 2005, was estimated between $2700 and $5900 USD and between $6100 and $6600 USD for excess costs, which are those costs in excess of the average annual per patient expenditures.[1] The estimated high cost of COPD can be caused by medications, health-care provider services, hospital admissions, home-based health care services, and emergency department visits.[5]
Pulmonary rehabilitation is a multidisciplinary intervention that includes disease-related education, cardiopulmonary and muscle strengthening exercises, and psychological support designed to minimize disease symptoms and complications. Pulmonary rehabilitation is recommended to be a part of any treatment plan for patients with chronic pulmonary diseases. The overall goal of pulmonary rehabilitation is to restore the patient's abilities to the highest level of independence and personal functions.[6] Benefits of pulmonary rehabilitation include optimizing functional status, improving quality of life, reducing health-care cost by stabilizing or reversing systemic manifestation of the disease, and by reducing emergency visits and days of admission for COPD patients.[7,8,9] Pulmonary rehabilitation services can be offered as in-patient hospital-based[10] or community-based outpatient programs in group settings, lasting usually for 8–12 weeks.[10,11] Self-monitored, home-based pulmonary rehabilitation is an alternative method that can be more convenient and accessible to deliver pulmonary rehabilitation services compared to in-patient programs.[12]
Only 1–2% of COPD patients receive pulmonary rehabilitation services each year, despite the well-documented benefits. Reasons for such low utilization rate include poor access to a rehabilitation program, lack of transportation, and inconvenient timing of the program.[13] Aiming to improve patients’ participation and adherence to pulmonary rehabilitation programs, additional tools, such as using the Internet and telecommunication technologies to supervise patients at home, have just recently been proposed as a new way to improve home-based rehabilitation programs. Remote real-time supervision during pulmonary rehabilitation sessions has the potential to minimize anxiety in both patients and health-care providers, provide accurate exercise prescriptions, and aid patients’ recovery progression.[14]
The aim of this review is to provide a narrative synthesis of studies which have used telehealth mediums with video components to provide real-time interactive pulmonary rehabilitation services for COPD patients at home. This review will provide a summary of the benefits of using telehealth in delivering pulmonary rehabilitation services for COPD patients at home. The review will also describe the pulmonary rehabilitation services that have been provided via the Internet and what types of telehealth technology have been used in the included studies.
REVIEW METHODS
An extensive systematic search of the literature with multiple search strategies was performed by the author using an electronic database search in the Ovid MEDLINE, CINAHL, and PubMed databases. The specific search terms used were Pulmonary rehabilitation and COPD in conjunction with each of the following terms: Telehealth, telemedicine, telecare, telehomecare, videoconferencing, ehealth, and real-time telerehabilitation. Multiple Internet search engines (e.g., Google Scholar and Bing) were used to search for additional articles and keywords. In addition, the bibliographies of the retained articles were examined to identify studies that were not originally captured in the electronic database search. The review included studies published from 1995 to 2014. The year 1995 was chosen as a starting date for this search because since then, telecommunication equipment cost has decreased and its use has become more common for health-care providers and individual patients.
For the purpose of this review, the inclusion criteria were (a) English-language publications (b) research studies that involved patients with COPD (c) research studies that used telehealth technology with a video component to provide home-based real-time pulmonary rehabilitation services (pilot studies that examined only one pulmonary rehabilitation service are also included) and (d) research studies published between 1995 and September 2014. Research studies that examined store and forward telemonitoring technology or used simple communication technologies such as phone calls and e-mails to follow-up with patients or to transfer patients’ data were excluded from the review. This review focuses on real-time telehealth because it is the most appropriate type of telehealth based on the nature of pulmonary rehabilitation. Providing rehabilitation services includes providing immediate advice and real-time instructions for the patients at home. Figure 1 outlines the review of screening process based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement.
Figure 1.
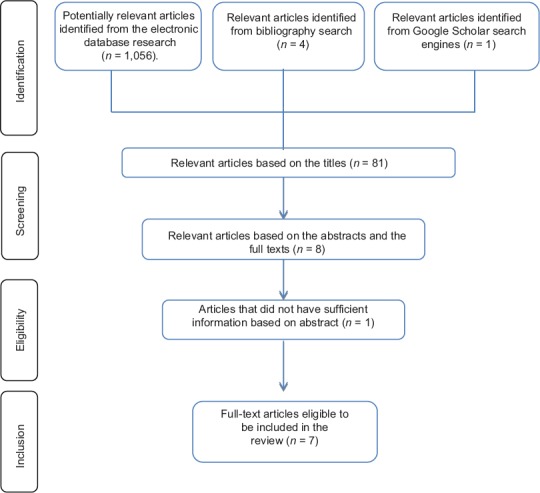
Flowchart of study selection process
FINDINGS
The electronic searches resulted in over than 1000 articles. Based on title screening, only 81 articles met the inclusion criteria. Then, full text copies of the 81 articles were reviewed, and only eight studies met the inclusion criteria based on the studies’ descriptions. One of the final eight studies was excluded because it had insufficient information about the method of delivering pulmonary rehabilitation services in the study. Each study was graded for the level of evidence based on the hierarchy developed by Melnyk and Fineout-Overholt.[15] Table 1 provides more detailed information about the rating system. Of the reviewed studies, two studies were scored as evidence level II, one study was scored as evidence level III, and four studies were scored as evidence level IV.[16,17,18,19,20]
Table 1.
Rating system for hierarchy of evidence
| Level | Description |
|---|---|
| I | Evidence from a systematic review or meta-analysis of all relevant RCTs or evidence-based clinical practice guidelines based on systematic reviews of RCTs |
| II | Evidence from at least one well-designed RCT |
| III | Evidence from well-designed controlled trials without randomization |
| IV | Evidence from well-designed case-control and cohort studies |
| V | Evidence from systematic reviews of descriptive and qualitative studies |
| VI | Evidence from a single descriptive or qualitative study |
| VII | Evidence from the opinion of authorities and/or reports or expert committees |
RCTs – Randomized controlled trials. (Source: Melnyk and Fineout-Overholt)[15]
This review included seven studies that explored the use of telehealth (Internet and computers) to provide real-time and home-based pulmonary rehabilitation for patients with COPD at home. Table 2 provides a summary of purposes, sample size, variables, provided services, and findings for each of the seven studies. Four of the included studies investigated delivering comprehensive pulmonary rehabilitation services, including cardiopulmonary exercise, breathing techniques, and disease-related education.[18,19,20,21] The other three studies investigated the effects of delivering only one or two pulmonary rehabilitation services for COPD patients at home.[16,22,23] The seven studies explored different aspects of using telerehabilitation that include feasibility, acceptance, safety, and clinical and social benefits.
Table 2.
Summary of studies purposes, technology used, samples, designs, provided services, variables, and findings
| Author (s), date, location | Level of evidence | Purpose of the study | Technology used | Sample size | Design | Provided service | Variables | Findings |
|---|---|---|---|---|---|---|---|---|
| Burkow et al. 2013, Norway | IV | Assess patients’ acceptability of an Internet-enabled program for comprehensive pulmonary rehabilitation program | A prototype Internet-connected system. User’s interface at home consisted of user’s own TV connected to a computer, the residential patient device, and remote control | 5 participants | A trial with an Internet-enabled program based on home groups for comprehensive pulmonary rehabilitation | Education sessions about COPD and long-term oxygen treatment, group exercising, and individual consultation | Patient acceptability | The Internet-enabled program for home-based groups in pulmonary rehabilitation and diabetes education were generally well accepted by the participantss |
| Holland et al. 2013, Australia | IV | Evaluate safety and establish the feasibility and acceptability of real-time, home-based pulmonary rehabilitation program | A cycle ergo meter, a pulse oximeter, and a tablet computer, and videoconferencing video collaboration software (VSee). The tablet was connected to Internet through a wireless 3G modem | 8 participants | Patients performed supervised aerobic training twice a week for 8 weeks, with a physiotherapist attending each class through videoconferencing from separate locations | Cycling exercise training supervised by a physiotherapist and education about self-management of COPD | Adverse events, feasibility, and acceptability. Clinical outcomes: Functional exercise capacity, health-related quality of life, and dyspnea improvement | A simple model of telerehabilitation using readily available equipment is safe and feasible in patients with COPD |
| Nield and Hoo 2012, USA | II | Determine the feasibility and efficacy of using real-time interactive voice and video telehealth for teaching PLB for patients with CORD | A laptop computer, headphone, and pulse oximeter. A free web-based software program (Skype) enabled synchronous audiovisual communication through Internet | 22 participants. Nine patients in the intervention group | A randomized control study with repeated measures to compare a 1-time PLB education session to a PLB education plus a 4-week telehealth PLB program | One component of a dyspnea self-management program PLB | Social support and dyspnea level | Real-time interactive voice and video telecommunication between health-care providers and the chronically ill patients is feasible, and can improve social support, access to health care, and delivery of effective health education |
| Paneroni et al. 2015, Italy | III | Explore the feasibility, adherence, and satisfaction of a home-based telerehabilitation program | Interactive TV software, oximeter, steps counter, a bicycle, and remote control to interact with the application | 18 participants in the intervention group | A multicenter, prospective, controlled, nonrandomized pilot study lasted for a maximum for 40 days | Strength exercise, telemonitored cycle training, educational sessions to promote an appropriate life style and self-management, and video-assistance and phone-calls | V^lking capacity, dyspnea level, and quality of life For the feasibility and adherence: number of adverse effects, number of hospitalization or emergency visits, sessions attended, platform interactions | Telerehabilitation for COPD patients at home is feasible and well accepted by patients Telerehabilitation seems to improve walking capacity, dyspnea, quality of life, and daily physical activity |
| Tabaket al. (2014), Netherlands | II | Investigate the use of a telerehabilltatlon program and explored the satisfaction of the participants’ with the received care Explore the clinical measures of telerehabilitation compared to the usual care | Activity coach application (three-dimensional-accelerometer with smartphone) for ambulant activity registration and real-time feedback A web portal with a symptom dairy for self-treatment of exacerbations | 29 participants. (14 participants in the intervention group) | A randomized controlled trial for 9 months | A web-based exercise program of the web portal, activity coach for ambulant activity registration and improvement, self-management education, and teleconsultation | Treatment days that patients visited the web portal in, satisfaction, number and duration of hospitalizations, emergency room visits, and number of exacerbations | Telerehabilitation for COPD patients at home is feasible and showed high satisfaction among participants. The self-management module was highly used, while the use of the exercise module was critically low |
| Tousignant, et al. 2012, Canada | IV | Investigate the efficacy of in-home pulmonary rehabilitation for people with COPD | A telerehabilitation platform consisted Videoconferencing system Liquid crystal display screen Router and modem connecting to the Internet Sensors and external devices Clinician computer and screen display | 3 participants | A pre-experimental pilot study with pre-and post-tests with no control group | Cardiopulmonary exercises | Functional exercise capacity, locomotor function and quality of life | Telehealth seems to be a practical way, both clinically and technically, to provide rehabilitation services for patients with CORD |
| Zanaboni et al. 2013, Norway | IV | Investigate the feasibility of a long-term telerehabilitation service | A treadmill, a pulse oximeter, a tablet computer used to perform videoconferencing and access the project’s website | 10 participants | The program was designed as a long-term intervention, with a 2-year follow-up with weekly videoconferencing sessions supervised by the physiotherapist | Exercise training, telemonitoring and education/ self-management | Hospital admission rate, long-term exercise maintenance, adherence to the exercise program, hospital length-of-stay, health care cost, quality of life | Telerehabilitation for COPD patients at home is feasible and it could reduce healthcare utilization |
Feasibility of using telehealth in pulmonary rehabilitation
Findings from six studies concluded that telerehabilitation was a feasible and successful way to conduct real-time pulmonary rehabilitation sessions for COPD patients in their home settings.[16,17,18,20,21,22] Feasibility of the proposed systems was assessed by either counting the number of sessions attended or the programs’ completion rates by the participants.
Acceptance of using telehealth in pulmonary rehabilitation
Five studies reported that patients with COPD accepted the use of a telerehabilitation system to receive pulmonary rehabilitation services at home.[17,18,19,20,21] Patients’ acceptance was measured using the System Usability Scale (which is used widely to document users’ experiences of technology), the Clinical Satisfaction Questionnaire, or by conducting interviews. Two studies reported that computer skills and previous Internet experience of the participants did not affect their level of accepting telerehabilitation programs.[16,19]
Safety of using telehealth in pulmonary rehabilitation
Two studies evaluated the safety of exercise sessions for patients with COPD at home that were supervised by a telerehabilitation program.[18,21] Both studies concluded that using telerehabilitation was safe with no major or moderate adverse events.
Benefits of using telehealth in pulmonary rehabilitation for patients with chronic obstructive pulmonary disease
Exercise capacity
Three studies evaluated the functional exercise capacity for patients with COPD who attended a telerehabilitation program.[18,21,22] In two studies, the exercise capacity of participants improved, but not to the extent to be clinically significant.[21,22] Results from Paneroni et al. (2015) showed a significant gain in walking capacity of the participants of the telerehabilitation program.
Dyspnea
Three studies measured the effect of using telerehabilitation in dyspnea among patients with COPD.[16,18,21] All the studies reported that dyspnea intensity was decreased among participants, but was not statistically significant.
Health-related quality of life
Health-related quality of life was measured in three studies.[18,21,22] Participants in the telerehabilitation programs showed improvements in two of the four dimensions of quality of life (dyspnea and fatigue) on the Chronic Respiratory Questionnaire (CRQ).[21] Tousignant et al. reported that all the participants showed a trend toward better quality of life based on the CRQ. Paneroni et al. (2015) reported that the quality of life improved in both the intervention and the control group of four points above the mean minimal detectable clinical changes improvement on the Saint George's Respiratory Questionnaire (SGRQ).
Social support
Two studies evaluated the impact of the real-time telerehabilitation on the sense of social support among patients with COPD. Participants’ sense of social support increased when receiving regular interactive sessions with a live person interested in their health status or during the in-group exercise sessions.[16,19]
Reduced health care utilization
From their preliminary results, Zanaboni et al. concluded that using telerehabilitation appears to be promising in reducing the utilization of the health-care systems.
Pulmonary rehabilitation services provided through telehealth
Overall, the seven research studies included in this review gave detailed information about how they conducted the telerehabilitation sessions. Four of the telerehabilitation trials provided educational instructions regarding self-management of COPD and long-term oxygen therapy.[17,18,19,20] Educational sessions about performing pursed-lip breathing techniques to relieve dyspnea were provided in two programs.[16,17] Four programs provided cardiopulmonary exercises for participants using stationary bikes at home.[18,20,21,22] In addition to the cardiopulmonary training, three trials provided supervised resistance training sessions intended to strengthen upper and lower extremities and to increase thorax muscle flexibility of COPD patients.[17,18,19] Tabak et al.'stelerehabilitation program included relaxation, mobilization, and mucus clearance for individual patients. In this study, the physiotherapy in the monitoring center utilized a program called “the Condition Coach” to monitor the patients and provide feedback. The Condition Coach consists of four modules (1) activity coach for ambulant activity monitoring and real-time coaching (2) web-based exercise program for home exercising (3) self-management of COPD exacerbations and (4) teleconsultation.
The telehealth technologies used in telerehabilitation
All the seven trials used the Internet to connect participants at home to the rehabilitation centers. Four trials used specially developed telerehabilitation interface systems for COPD patients at home and for health-care providers at the rehabilitation centers.[17,18,19,22] The other three trials used commercially available equipment (personal computers and tablets with built-in webcam) for free video calling software programs (Skype™ VSee™, and LifeSize ClearSea) or equipment from an existing pulmonary rehabilitation program (pulse oximeter devices and ergometers).[16,20,21]
DISCUSSION
This narrative review of seven studies is the first that explored the use of real-time telerehabilitation for COPD patients at home. Findings of this review suggested that providing pulmonary rehabilitation using specially designed or commercially available telecommunication equipment is feasible, accepted, and safe. The conclusions from this review propose that using telerehabilitation for COPD patients at home was associated with positive clinical outcomes that include improvements in quality of life, exercise capacity, dyspnea level, and the sense of social support. In regards to the effect of telerehabilitation on exercise capacity, Tousignant et al. reported that one participant, out of the three participating in the study, had an exacerbation during the last week of the program, which affected the final results. However, this patient showed a significant clinical improvement in the four domains of quality of life. In this study, the other two participants showed a significant clinical improvement in motor function and the four domains of quality of life.
Several studies in this review suffered from many methodological issues including the small sample sizes (e.g., three, five, and up to eighteen participants), the use of weak research designs with no control groups, and bias in recruitment procedures. Tabak et al. reported that recruiting patients was difficult because of the strict inclusion and exclusion criteria that included the need for a computer with Internet access at home, which was not always possible for elderly patients. In a study by Tabak et al., only two (24%) participants were able to continue the study in the control group, and only nine (66%) patients were able to finish the 9-month program. In addition, exacerbation data for the control group were lost during follow-up and were not available for analysis. Based on the available data, the telerehabilitation group had four hospitalizations with a median duration of 5.5 days, while the control group had five hospitalizations with a median duration of 7.0 days. Tousignant et al. reported that patients who agreed to participate in the study were self-motivated and willing to explore new methods of delivering rehabilitation services. The selection bias may inflate the outcomes, and reduce the possibility to draw a sound conclusion.
For this review, only studies that explored the use of real-time telerehabilitation systems for COPD patients at home were included. Studies that used asynchronous telecommunication technology to monitor and follow up patients at home were excluded. Moreover, studies that utilized real-time telerehabilitation systems to facilitate the delivery of rehabilitation services for COPD patients in sites rather than homes (e.g., community-based clinics) were also excluded. An example of an excluded study is a large controlled trial conducted by Stickland et al. in 2011, which compared the clinical outcomes from a center-based telerehabilitation program that included 147 COPD patients with 262 COPD patients attending a standard pulmonary rehabilitation program. Findings of this study indicated that the telerehabilitation program resulted in similar clinically and statistically significant improvements in quality of life and exercise capacity for COPD patients, compared with standard pulmonary rehabilitation. This center-based model was able to improve access to pulmonary rehabilitation services for COPD patients living in rural areas, but does not solve other barriers of pulmonary rehabilitation utilization, such as transportation and high cost of traditional rehabilitation services.[24]
CONCLUSION
It is evident from this review that the topic of using telehealth in delivering pulmonary rehabilitation services for COPD patients at home has not been investigated sufficiently by researchers in the health-care field. This narrative review of research uniquely contributes to the current state of knowledge of using telehealth technology to provide real-time pulmonary rehabilitation services for COPD patients at home. This narrative review highlights, based on the available resources, that using telehealth to deliver real-time interactive pulmonary rehabilitation services for COPD patients at home is feasible and acceptable. Simple, low-cost models of telerehabilitation systems, using available equipment and free videoconferencing software programs, are safe to use and can improve access to pulmonary rehabilitation services, especially for patients living in rural areas. It is worth noting that participants’ computer literacy level has no effect on acceptability or on the utilization of the tele-pulmonary rehabilitation systems.[16]
A knowledge gap regarding the benefits of using telerehabilitation for COPD patients still exists. Interestingly, the seven studies in this review are recent, published in 2012, 2013, and 2014 indicating that using telehealth in pulmonary rehabilitation is a relatively new practice. Further research with a high level of evidence investigating the use of telehealth in pulmonary rehabilitation is needed. There is a critical need to explore telerehabilitation acceptance of all users, including patients and health-care professionals prior to implementing such programs in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mannino DM, Buist AS. Global burden of COPD: Risk factors, prevalence, and future trends. Lancet. 2007;370:765–73. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 2.Karapolat H, Atasever A, Atamaz F, Kirazli Y, Elmas F, Erdinç E. Do the benefits gained using a short-term pulmonary rehabilitation program remain in COPD patients after participation? Lung. 2007;185:221–5. doi: 10.1007/s00408-007-9011-4. [DOI] [PubMed] [Google Scholar]
- 3.What is COPD?. CDC-COPD Home Page - Chronic Obstructive Pulmonary Disease (COPD) 2016 from http://www.cdc.gov/copd/index.html . [Google Scholar]
- 4.surname>Chronic Obstructive Pulmonary Disease (COPD) Fact Sheet – American Lung Association. 2015 [Google Scholar]
- 5.Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance – United States, 1999-2011. Chest. 2013;144:284–305. doi: 10.1378/chest.13-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kyung KA, Chin PA. The effect of a pulmonary rehabilitation programme on older patients with chronic pulmonary disease. J Clin Nurs. 2008;17:118–25. doi: 10.1111/j.1365-2702.2006.01712.x. [DOI] [PubMed] [Google Scholar]
- 7.Dillon A, Morris MG. User Acceptance of Information Technology: Theories and Models. Annual Review of Information Science and Technology (ARIST) 1996;31:3–32. [Google Scholar]
- 8.Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13–64. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 9.Golmohammadi K, Jacobs P, Sin DD. Economic evaluation of a community-based pulmonary rehabilitation program for chronic obstructive pulmonary disease. Lung. 2004;182:187–96. doi: 10.1007/s00408-004-3110-2. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein RS, Gort EH, Guyatt GH, Feeny D. Economic analysis of respiratory rehabilitation. Chest. 1997;112:370–9. doi: 10.1378/chest.112.2.370. [DOI] [PubMed] [Google Scholar]
- 11.Pruitt B. Coming Together for Pulmonary Rehabilitation.RT. J Respir Care Pract. 2011;24:18–20. [Google Scholar]
- 12.Maltais F, Bourbeau J, Shapiro S, Lacasse Y, Perrault H, Baltzan M, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: A randomized trial. Ann Intern Med. 2008;149:869–78. doi: 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 13.Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8:89–99. doi: 10.1177/1479972310393756. [DOI] [PubMed] [Google Scholar]
- 14.Tang J, Mandrusiak A, Russell T. The feasibility and validity of a remote pulse oximetry system for pulmonary rehabilitation: A pilot study. Int J Telemed Appl 2012. 2012:798791. doi: 10.1155/2012/798791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melnyk BM, Fineout-Overholt E. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2005. Evidence-based Practice in Nursing & Healthcare: A Guide to Best Practice. [Google Scholar]
- 16.Nield M, Hoo GW. Real-time telehealth for COPD self-management using Skype™. Copd. 2012;9:611–9. doi: 10.3109/15412555.2012.708067. [DOI] [PubMed] [Google Scholar]
- 17.Tabak M, Brusse-Keizer M, van der Valk P, Hermens H, Vollenbroek-Hutten M. A telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: A pilot randomized controlled trial. Int J Chron Obstruct Pulmon Dis. 2014;9:935–44. doi: 10.2147/COPD.S60179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paneroni M, Colombo F, Papalia A, Colitta A, Borghi G, Saleri M, et al. Is Telerehabilitation a Safe and Viable Option for Patients with COPD? A Feasibility Study. COPD. 2015;12:217–25. doi: 10.3109/15412555.2014.933794. [DOI] [PubMed] [Google Scholar]
- 19.Burkow TM, Vognild LK, Østengen G, Johnsen E, Risberg MJ, Bratvold A, et al. Internet-enabled pulmonary rehabilitation and diabetes education in group settings at home: A preliminary study of patient acceptability. BMC Med Inform Decis Mak. 2013;13:33. doi: 10.1186/1472-6947-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zanaboni P, Lien LA, Hjalmarsen A, Wootton R. Long-term telerehabilitation of COPD patients in their homes: Interim results from a pilot study in Northern Norway. J Telemed Telecare. 2013;19:425–9. doi: 10.1177/1357633X13506514. [DOI] [PubMed] [Google Scholar]
- 21.Holland AE, Hill CJ, Rochford P, Fiore J, Berlowitz DJ, McDonald CF. Telerehabilitation for people with chronic obstructive pulmonary disease: Feasibility of a simple, real time model of supervised exercise training. J Telemed Telecare. 2013;19:222–6. doi: 10.1177/1357633x13487100. [DOI] [PubMed] [Google Scholar]
- 22.Tousignant M, Marquis N, Pagé C, Imukuze N, Métivier A, St-Onge V, et al. In-home telerehabilitation for older persons with chronic obstructive pulmonary disease: A Pilot Study. Int J Telerehabil. 2012;4:7–14. doi: 10.5195/ijt.2012.6083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao J, Zhai YK, Zhu WJ, Sun DX. Effectiveness of telemedicine for controlling asthma symptoms: A systematic review and meta-analysis. Telemed J E Health. 2015;21:484–92. doi: 10.1089/tmj.2014.0119. [DOI] [PubMed] [Google Scholar]
- 24.Stickland M, Jourdain T, Wong EY, Rodgers WM, Jendzjowsky NG, Macdonald GF. Using telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J. 2011;18:216–20. doi: 10.1155/2011/640865. [DOI] [PMC free article] [PubMed] [Google Scholar]


