Abstract
Rabies postexposure prophylaxis (PEP) is administered for rabies prevention after a human exposure to a potentially rabid animal, such as a bite. Previous studies have reported that rabies PEP is often inappropriately administered. Health professional education was proposed as one potential solution to address inappropriate PEP use. We assessed baseline knowledge, knowledge gain, and knowledge retention among health professionals in Arizona of rabies epidemiology and appropriate PEP administration. Maricopa County Department of Public Health created an online rabies PEP continuing education module and measured knowledge before and after module completion using a 10-question test. The same test was administered three times (pretest, posttest, and retention test at ≥3 months). To assess knowledge gain and retention, we compared median scores using nonparametric methods. A total of 302 respondents completed the pretest (median score, 60%) and posttest (median score, 90%; p < .001); 98 respondents completed all three tests with median scores 60% (pretest), 90% (posttest, p < .01), and 80% (retention test and compared with pretest, p < .01). Sixty-nine (70%) respondents improved their pretest to retention test score by a mean of 2.4 points out of a total 10 points (median: 2 points; range: −5 to 7 points). Only 48% of pretest respondents correctly answered that PEP should not be administered immediately to anyone bitten by a healthy dog. However, 81% and 70% answered correctly on the posttest (p < .0001) and retention test (p = .002), respectively. Respondents demonstrated rabies epidemiology and PEP knowledge gain and ≥3-month knowledge retention after completing the online continuing education module.
Keywords: continuing education, rabies, PEP, public health
Health professionals have a need to continually maintain their competencies and a range of knowledge as new research, techniques, information, or ideas are exchanged or discovered. There are several barriers to obtaining required continuing education (CE), which can include the time spent and/or travel expenses incurred to participate in traditional CE courses (Garrison, Schardt, & Kochi, 2000). However, distance-based education, which refers to the formal method of study where students and instructors do not meet in an instructional space but use the Internet or other electronic-mediated methods, is increasingly being used to deliver professional development activities (Garrison et al., 2000). Online learning modules in particular have been demonstrated to be a preferred route of education for physicians (Fordis et al., 2005). Thus, educating physicians about public health issues via online learning is a useful and effective teaching strategy. Recent efforts have culminated into distance learning, dual-degree programs such as Doctor of Medicine/Master of Public Health (MD/MPH) programs. Other strategies exist to integrate public health and local epidemiology training not only into medical school programs but during the CE phase as well (Cooper et al., 2010).
In particular, the Maricopa County Department of Public Health (MCDPH) noted that physicians were unaware of the epidemiology of rabies in Maricopa County, Arizona, based on the lack of consultation with public health officials or not knowing whom to consult about rabies risk assessments. Rabies is among the most fatal and preventable communicable diseases in the United States and globally, making it an important public health concern. Human infection with rabies virus leads to encephalitis and almost certain death without postexposure prophylaxis, highlighting the importance of preventing and correctly managing potential exposures (Heymann, 2015). From zero to three human rabies cases are reported annually in the United States (Birhane et al., 2017). During 2008 to 2015, a total of 22 cases of human rabies were reported; the majority (64%) of human cases contracted infection from animal contact such as a bite; contact with bats was the most common source of exposure (50%), and the remaining cases were from organ transplantation or unknown sources (Birhane et al., 2017).
Rabies postexposure prophylaxis (PEP) is administered for rabies prevention after a human exposure to a potentially rabid animal, most commonly a bite (Birhane et al., 2017; Centers for Disease Control and Prevention [CDC] Recommendations of the Advisory Committee on Immunization Practices [ACIP], 2010). PEP, which includes rabies immune globulin (RIG) and four rabies vaccine doses, is highly effective in preventing rabies if given in a timely manner and according to recommendations (Birhane et al., 2017; CDC ACIP, 2010). An exposure assessment should occur before rabies PEP is initiated and should include discussion between medical providers and public health officials (National Association of State Public Health Veterinarians, 2016); however, health care providers do not always consult public health officials before PEP administration. Fastidious evaluation of potential rabies exposure, evaluating factors such as animal species, type of exposure, and local rabies epidemiology, is essential to both prevent human rabies fatalities and avoid unnecessary administration of rabies PEP to those who are not at risk. Unnecessary PEP administration incurs unnecessary costs, including cost of PEP administration, cost of sero-logical testing, hospital fees, and other indirect costs (e.g., travel costs). In the United States, an estimated 40,000 to 50,000 persons receive rabies PEP annually at an estimated per-patient cost of $3,000 for a complete PEP regimen (CDC, 2015). The median risk of rabies transmission without rabies PEP for a bite exposure by a skunk, bat, cat, and dog was estimated by expert opinion to be 0.05, 0.001, 0.001, and 0.00001, respectively (Vaidya et al., 2010).
ACIP has established recommendations regarding rabies PEP to prevent human rabies (CDC ACIP, 2010). Local and state health departments and health care providers should have ready access to and a working knowledge of these recommendations and local rabies epidemiology to make correct decisions about PEP administration. This knowledge is especially needed for health care providers who work in emergency departments (ED) or urgent care settings, because they are often the first health professionals to provide patient care for an animal bite wound or possible rabid animal exposure. To assess and improve the baseline knowledge of rabies epidemiology and PEP administration among health professionals in Arizona, we created an online 1-hour rabies PEP CE module, promoted it to Arizona health care providers, and measured immediate and long-term knowledge retention after module completion.
Method
Study Population
The online rabies CE module was intended for Arizona Emergency Department physicians, nurses, and other medical and public health professionals. Physicians were initially the main target population because nurses in Arizona are not required to obtain CE credits in order to maintain their license. However, physicians in Arizona are required to obtain CE credits (40 contact hours every 2 years) in order to renew their state license, and they remain the main initiators (“prescribers”) of PEP. In 2012, a total 15,133 physicians were actively practicing in Arizona, including 759 practicing in the Emergency Medicine specialty, according to the workforce profile in the Association of American Medical Colleges’ State Physician Workforce Data Book (Association of American Medical Colleges, 2013). Historic data, relevant to our study period, are not readily available for nurses; however, the number of professionally active nurses in 2017 in Arizona was 63,955 (registered nurses and licensed practical nurses; Kaiser Family Foundation, 2017). The format was online and self-paced; the time for completion was estimated to be 1 hour. The module was accredited to offer several types of CE credits providing 1.0 contact hours of credit. The rabies CE module was promoted through multiple outlets, including professional electronic distribution lists to Arizona physicians and nurses, in-person hospital training, and website promotion. A link to the module was made publicly available on MCDPH’s website and directly through the CDC’s Training and Continuing Education Online (TCEO) web-site (https://www2a.cdc.gov/TCEOnline/). Although the training was intended for Arizona health professionals, participants from any state or county could access the module through the Internet; we included all participants who completed the module in these analyses.
Rabies Continuing Education Module
The rabies CE module content and test questions were adapted by MCDPH with permission from the Maryland Department of Health and Mental Hygiene (MDHMH) and CDC for a module they originally developed and was aligned with rabies epidemiology in Arizona, specific to Maricopa County (the rabies CE module content is available on request; Robertson & Feldman, 2014). The Maryland module was developed in collaboration with the CDC Poxvirus and Rabies Branch, and it was based on references from ACIP (CDC ACIP, 2010), the Compendium of Animal Rabies Prevention and Control (National Association of State Public Health Veterinarians, 2011), CDC Yellow Book (Brunette, 2016), and the national rabies surveillance report (Dyer et al., 2014). Our rabies CE module contained an introduction section and five case-based sections, which included a combination of rabies exposure and animal bite case scenarios: a bat in the bedroom, dog bite, fox bite, rabid bobcat attack, and stray cat scenario. Each case-based section included a picture, background information on the scenario, and relevant external links to CDC references for more information. The objectives of the introduction section included the following: define rabies clinical manifestations and describe how it is transmitted; describe the epidemiology of rabies in Arizona, the United States, and the world; and identify where to find rabies treatment and prevention guidelines. One or two objectives were presented at the beginning of each case-based section, such as the following: identify relevant considerations when assessing a patient for rabies virus exposure following a bat encounter or a bite from a wild terrestrial carnivore or a cat bite, identify relevant considerations when deciding to delay rabies PEP initiation following a dog exposure, describe proper administration of RIG or rabies vaccine for use in rabies PEP (PEP administration guidance included dosage, location on body, and frequency), identify the diagnostic method used for animal rabies testing, or determine appropriate actions to take for animal bite wound care. The rabies CE module was open for a 3-year period from September 2012 to September 2015.
Learning Assessment
The rabies CE module was implemented on September 1, 2012, and pretest data collection ended on September 30, 2015. Retention test data collection continued up to 4 months after the discontinuation date for the pretest and ended on January 30, 2016; this was to allow anyone who took the posttest on September 30, 2015, approximately one month to take the retention test since it would have only been available for those respondents starting December 30, 2015. The knowledge assessment consisted of 10 multiple choice or true or false questions, with a focus on case-based scenarios. One point was awarded for each correct response; score range was from 0 to 10. The questions were developed, tested, and validated in consultation with the CDC subject matter experts in different medical disciplines (nurse, pharmacist, and physician). The CDC assisted with the question development, and the questions were piloted with 22 professionals: the CDC group of experts, county public health professionals, emergency medicine technicians, and a group of public health university students who had been trained to perform foodborne illness interviews (Student Aid for Field Epidemiology Response Team). Pilot participants provided feedback, which was incorporated as appropriate.
The subject matter of each test question was categorized as an epidemiological or a medical question. A question was categorized as epidemiological if it included some knowledge of rabies epidemiology, even if it also discussed PEP administration. A question was categorized as medical if it tested knowledge about diagnostic testing or medical management. Five questions were categorized as epidemiological (1, 3, 4, 5, and 7), and five questions were categorized as medical (2, 6, 8, 9, and 10; see Table 1).
Table 1.
Rabies Continuing Education (CE) Knowledge Assessment Questions, Answers, and Types, and the Percentage of Health Professionals Who Scored Correctly on the CE Tests, by Question Number (N = 98), 2012 to 2015.
| No. | Question | Answer | Categorya | Pretest (%) | Posttest (%) | Retention test (%) |
|---|---|---|---|---|---|---|
| 1 | Human cases of rabies in the United States are most often associated with exposures to which mammals? | Bats | Epi | 72 | 90 | 90 |
| 2 | Which of the following statements about RIG is TRUE? | RIG provides passive immunity | Med | 40 | 92 | 46 |
| 3 | A healthy man, aged 30 years, was bit by a raccoon while emptying a garbage dumpster. The man has never been vaccinated against rabies. Which of the following best describes correct PEP for this patient? | 4 doses of rabies vaccine, each on days 0, 3, 7, and 14, with 1 dose of RIG on day 0 | Epi | 64 | 95 | 86 |
| 4 | Which of the following statements about dogs is FALSE? | PEP should be administered immediately to anyone bitten by a dog | Epi | 48 | 81 | 70 |
| 5 | A healthy woman, aged 45 years, was bitten 3 days ago by a stray cat while visiting China. Six months ago, she completed a full course of rabies preexposure vaccination. Which of the following best describes correct rabies PEP for this patient? | A 2-dose course of rabies vaccination, with no RIG | Epi | 56 | 94 | 68 |
| 6 | Which method is considered the standard for diagnosing rabies in either animals or humans? | Direct fluorescent antibody on brain tissue | Med | 61 | 80 | 79 |
| 7 | A man, aged 27 years, awoke to find a bat in his bed this morning. He does not know whether he was bitten or scratched, but he vaguely remembers feeling something brush against his face in the middle of the night. He informs you that he is human immunodeficiency virus-positive. Which of the following best describes correct rabies PEP for this patient? | A 5-dose course of rabies vaccination, with 1 dose of RIG | Epi | 65 | 84 | 81 |
| 8 | If a previously unvaccinated adult was bitten in the left arm and receives RIG in accordance with ACIP guidelines, where should his or her day 0 dose of rabies vaccine be injected? | Right deltoid | Med | 50 | 93 | 79 |
| 9 | Which of the following patients would most merit postvaccination serologic testing to verify an adequate immune response after PEP? | An immunocompromised patient who received a full course of PEP in accordance with ACIP guidelines | Med | 89 | 99 | 92 |
| 10 | Which of the following is a key component of rabies PEP, in addition to RIG and rabies vaccine? | Wound cleansing | Med | 89 | 98 | 98 |
Note. RIG = rabies immune globulin; PEP = postexposure prophylaxis; ACIP = Advisory Committee on Immunization Practices.
Epi indicates that the question tests epidemiological rabies knowledge, and Med indicates that the question tests medical rabies knowledge.
The same knowledge assessment was administered three separate times in the form of a pretest, posttest, and retention test. Information was requested about the respondent’s state of residence, work setting (e.g., hospital ED), and clinical specialty area (e.g., emergency medicine, infectious diseases, or primary care). At the start of the rabies CE module, the respondent was encouraged, but not required, to take the pretest using a link to an external survey website. After completing the rabies CE module, the respondent was given information regarding how to complete the posttest through the CDC TCEO website. If the respondent completed the posttest with a passing score of at least 70%, he or she received CE credit.
An algorithm was created using statistical analysis software SAS version 9.3 (SAS Institute Incorporated, Cary, North Carolina) to automatically send an email to respondents 3 months after the initial test date requesting the respondent take the retention test. Three months was chosen as the minimum period before testing long-term knowledge retention based on published data (Sisson, Swartz, & Wolf, 1992). The retention test was administered through the same external survey website as the pretest, and included three additional questions only for retention test takers with options to select yes or no, to assess the module’s clinical relevance to the respondent’s day-to-day work. Answers to these three additional questions did not affect the test score. After the initial email inviting the participant to take the retention test (3 months posttest), two additional reminders were sent on Days 4 and 7 of the same week. To maximize response rates, the retention test remained open regardless of when the respondent received the reminder emails and respondents could take the retention test anytime starting 3 months after the posttest.
Data Management and Analysis
The CDC reviewed this study for human subjects protection and deemed the work to be nonresearch. Only the few MCDPH investigators had access to the final data files. The name, email address, and demographic and characteristic information of respondents were reviewed to identify respondents who might have completed the pretest more than once. Duplicate and incomplete entries were removed from the analysis. A unique numerical identifier was assigned to each person who had taken the test after the data were cleaned to protect anonymity. Pretest, posttest, and retention test data were matched and manually validated by name or email address. If a respondent failed the pretest or posttest on the first attempt (scoring lower than 70% on either test) and retook the test, only the first attempt was included in the analysis.
Demographics, characteristics, and clinical relevance to practice results were analyzed as categorical variables. Continuing medical education (CME) was available only to physicians, and all others received CE credit; respondents were categorized as physicians or nonphysicians to ensure that comparisons were made among respondents with similar levels of medical training. A location was categorized as within or outside of Arizona, because the intended population was Arizona health professionals. Completion dates and times were recorded for each test; the time interval between completion dates of the pretest, posttest, and retention tests was calculated and converted into months.
P values were calculated to compare median scores and interquartile ranges for pretest, posttest, and retention test results from respondents who completed all three tests (minimum of 0 to a maximum of 10) using nonparametric tests. The Wilcoxon signed rank test was used for comparing matched samples, and the Friedman test was used as an alternative to the one-way ANOVA with repeated measures because of the use of nonpara-metric data, using SAS version 9.3. The difference between pretest and posttest scores was measured to assess knowledge gained, and the difference between pretest and retention test scores was measured to assess knowledge retention.
The difference in pretest and posttest scores for the group of respondents who did not take the retention test (pre-posttest group) was compared with the scores of those who did take the retention test (pre-post-retention test group). Also, among the group of respondents who did not take the posttest, the difference in pretest and retention test scores was compared (pre-retention test group). Trends in the percentage of respondents scoring incorrectly for each question were also assessed to identify knowledge gaps.
Results
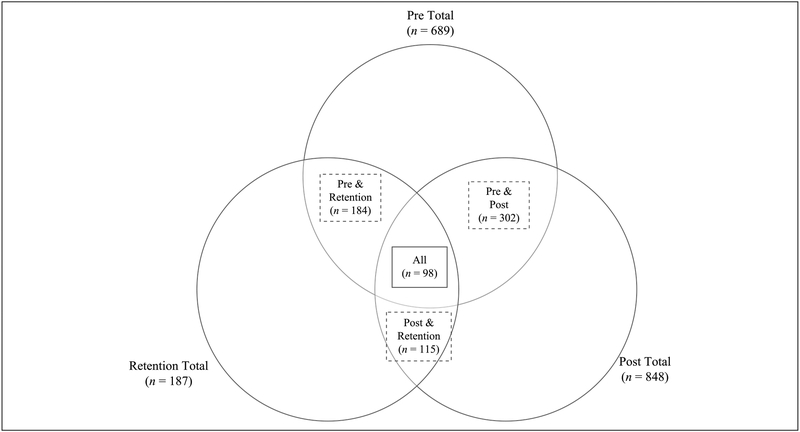
MCDPH collected pretest data for 689 respondents, posttest data for 848 respondents (available only in aggregate form from CDC), and retention test data for 187 respondents during September 2012 to December 2015 (Figure 1). No respondents completed the retention test in January 2016. A total of 302 respondents completed only the pretest and posttest. A total of 98 respondents completed all three tests; 75% of respondents completed the retention test within 1 month of the retention test being available 3–12 months after the posttest. Our analyses focused on three groups: the pre-posttest group (302 respondents), the pre-post-retention test group (98 respondents), and the pre-retention test group (184 respondents).
Figure 1.
Venn diagram of number of respondents by rabies CE module pretest, posttest, and retention test, and matched between tests, 2012 to 2015.
The median aggregate score for the pre-posttest group increased from 60% on the pretest to 90% on the posttest (p < .001), and the same increase was reported among the 98 pre-post-retention test group. Thirty physicians (10%) of 302 were in the pre-posttest group, and nine physicians (9%) of 98 were in the pre-post-retention test group; both physician groups showed 30% knowledge gained when comparing total median scores of the pre-test (median score, 70%) with the posttest (median score, 100%). Additionally, the pre-retention test group had a similar result to the pre-post-retention test group; median scores increased from 60% to 80% (p < .001).
The majority of the pre-posttest group resided outside of Arizona (76%), and the largest group was nurses (49%); among the pre-post-retention test group, 68% resided outside of Arizona, and 56% were nurses (see Table 2). Regarding clinical relevance to practice questions that were asked only in the retention test, 74 (76%) respondents reported that the module was useful for their day-to-day work, and 63 (64%) respondents reported that they would use or had used the information learned in the module. Ninety-one (93%) respondents reported that they would likely benefit in the future from using the module information. Trends in demographics and characteristics reported were similar between the pre-posttest group, compared with the 98 pre-post-retention test group, and no significant differences were calculated (p > .05 for all characteristics).
Table 2.
Characteristics of Rabies Continuing Education Respondents, 2012 to 2015.
| Characteristic | Respondents who completed all three tests (N = 98), n (%) | Respondents who completed only the pretest and posttest (N = 302), n (%) | p value |
|---|---|---|---|
| Location | |||
| Outside Arizona | 67 (68.4) | 228 (75.5) | .165 |
| Arizona | 29 (29.6) | 74 (24.5) | .317 |
| Respondent typea | |||
| Nonphysician | 89 (90.8) | 272 (90.1) | .826 |
| Nurse | 55 (56.1) | 148 (49.0) | .222 |
| Other public health professionalb | 16 (16.3) | 49 (16.2) | .984 |
| Other health care professionalc | 15 (15.3) | 51 (16.9) | .711 |
| Pharmacist | 3 (3.1) | 25 (8.3) | .078 |
| Physician | 9 (9.2) | 30 (9.9) | .826 |
Respondent type is based on the type of continuing education received.
Other public health professional such as environmental health officer or sanitarian.
Other health care professional such as physical therapist or physician assistant.
Total median scores for the pre-post-retention test group improved from a score of 60% on the pretest to 90% on the posttest (p < .01) after completion of the rabies CE module, then declined to 80% on the retention test (p < .01) 3 to 12 months after module completion; the difference between pretest knowledge assessment and retention test scores was also significant (p < .001; see Table 3). Because of the limited number of respondents who took the retention test, clinical specialties were not compared. No differences in test score results were identified when comparing questions that assessed epidemiological versus medical knowledge on all three tests. Scores did not differ significantly based on provider location (inside vs. outside of Arizona). The median pretest score was not significantly higher for physicians (70%; range: 60% to 80%) than for nonphysicians (60%; range: 60% to 70%; p = .48). However, both physicians and nonphysicians demonstrated similar improvements; posttest scores improved by a median of 30% (range: 20%−40%) from the pretest (p = .03 for physicians and p < .001 for nonphysicians), and retention test scores improved by a median score of 20% (range: 10% to 30%) from the pretest for both physicians (p = .04) and nonphysicians (p < .001).
Table 3.
Rabies Postexposure Prophylaxis Continuing Education Module Pretest, Posttest, and Retention Test Knowledge Assessment Scores by Respondent Characteristic (N = 98), 2012 to 2015.
| Characteristic (n) | Pretest median out of 10 (IQR) | Pre versus posttest, p value | Posttest median out of 10 (IQR) | Post versus retention test, p value | Retention total median out of 10 (IQR) | Pre versus retention test, p value |
|---|---|---|---|---|---|---|
| Total respondents | 6 (5–7) | .01 | 9 (8–10) | .01 | 8 (7–9) | .001 |
| Location | ||||||
| Outside of Arizona (67) | 6 (5–8) | .896 | 9 (9–10) | .777 | 8 (7–9) | .604 |
| Arizona (29) | 6 (6–7) | − | 9 (9–10) | − | 8 (7–9) | − |
| Respondent typea | ||||||
| Nurse (55) | 7 (6–8) | .513 | 9 (8–10) | .235 | 8 (7–9) | .823 |
| Other public health professionalb (16) | 6 (4.5–7) | − | 10 (8.5–10) | − | 8 (6.5–9) | − |
| Other health care professionalc (15) | 6 (4–8) | − | 9 (8–10) | − | 8 (6–9) | − |
| Physician (9) | 7 (6–8) | − | 10 (10–10) | − | 9 (8–9) | − |
| Pharmacist (3) | 6 (6–6) | − | 10 (8–10) | − | 8 (7–9) | − |
| Professional category | ||||||
| Nonphysician (89) | 6 (6–7) | .001 | 9 (8–10) | .001 | 8 (8–9) | .001 |
| Physician (9) | 7 (6–8) | .034 | 10 (10–10) | .039 | 9 (8–9) | .039 |
Note. IQR = interquartile range.
Respondent type is based on the type of continuing education received.
Other public health professional, such as environmental health officer or sanitarian.
Other health care professional, such as physical therapist or physician assistant.
Overall, 87 (89%) of 98 respondents improved their score from the pretest to the posttest by a mean of 3 points out of a possible score of 10 (median: 2.5 points; range 0–7 points). Eleven (11%) respondents earned a similar score on the pretest and posttest. None of the respondents earned a lower score on the posttest than the pretest. When reviewing each question individually, the percentage of respondents who scored correctly on each question increased when comparing pretest with posttest (see Table 1). Overall, 69 (70%) of 98 respondents improved their score from the pretest to the retention test by a mean of 2.4 points (median: 2 points; range: −5 to 7 points). Sixteen (16%) respondents earned a similar score on the pretest and retention test. Thirteen (13%) earned a lower score on the retention test than the pretest with a mean decrease of −1.7 points.
When reviewing each question individually for the pre-post-retention test group, the percentage of respondents who scored correctly on each posttest question was higher than the percentage of respondents who scored correctly on each retention test question, except for Question 10, which pertained to wound cleansing as a key component to rabies PEP; the percentage of respondents who scored correctly on Question 10 of the posttest and retention test were the same (98%; see Table 1).
Discussion
Median score improvement of 20% from the pretest to the retention test after completion of the online rabies CE module provides evidence that this module is an effective tool for increasing rabies knowledge among health care providers ≥3 months later. Although a similar online CE module was implemented in Maryland, Arizona has not previously used this tool, and ≥3 months (long-term) knowledge retention after completion of the Maryland module has not been evaluated.
We had fewer respondents than the rabies CE module developed by MDHMH and CDC (302 respondents vs. 2,300 Maryland respondents, which might be explained because MDHMH promoted their CE module through additional outlets, including CDC’s Morbidity and Mortality Weekly Report, news bulletins, social media, and nonprofit organizations). The majority of our respondents reported that they would benefit from the rabies CE module or that it was applicable to their day-to-day work, and similarly, MDHMH respondents reported 98% agreement that the knowledge gained from the module was applicable to their work (Robertson & Feldman, 2014). Robertson and Feldman also assessed the effectiveness of a 1-hour in-person lecture similar to the MDHMH online rabies PEP CE module by administering a 10-question pretest and posttest to 10 clinicians at a local university hospital (without a retention test); overall, they noted a 73% improvement from pretest to posttest scores.
Several knowledge gaps were observed among the health professional community evaluated. The questions had been divided into medical or epidemiological questions initially to identify specific knowledge gaps; given limited resources or time for education, this would target education efforts. For example, if the results showed that physicians really did know the epidemiological questions well, more emphasis could be placed on medical administration rather than local rabies epidemiology.
Initial pretest scores averaging below a passing score of 70% demonstrate a need for rabies PEP and epidemiology CE. In particular, a majority of respondents (52%) incorrectly believed that all dog bites warranted PEP, which is not recommended by CDC for bites from dogs that appear healthy occurring in the continental United States (CDC ACIP, 2010). In the United States, rabies in domestic animals is rare, with 92.4% of reported animal rabies in 2015 occurring among wildlife (Birhane et al., 2017). However, a prospective study by Moran et al. (2000) reported that domestic dog and cat exposures represented 86% of all PEP for animal exposures during 1996 to 1998, and 40% of PEP delivered was inappropriately administered. PEP recommendations differ based on the bite circumstances and the local rabies epidemiology, but more than 95% of dog bites in Arizona do not warrant rabies PEP (and the last documented case of rabies in a dog in Arizona was in 1977). Knowledge of this information was gained from the pretest to the post-test, indicating that the module was effective to inform participants about appropriate PEP administration for dog bites in the United States. Previous studies have reported that rabies PEP is often inappropriately administered. Jerrard (2004) outlines that 42% of PEP recipients received RIG in a manner contrary to ACIP guidelines. In 2011, an internal review by MCDPH in Arizona reported that 46% of persons exposed to potentially rabid animals received rabies vaccine but not RIG. However, unless these persons were previously vaccinated, protocol recommends for them to have received both PEP and RIG in order to be fully protective. Other research concludes that physicians’ basic and clinical knowledge of rabies epidemiology and PEP administration in general is insufficient, further supporting the recommendation for rabies prophylaxis educational programs designed to educate clinicians regarding the guidelines provided by the World Health Organization and ACIP (Gönen, Soysal, Topuzoğlu, & Bakir, 2011). Physician education, such as the module presented here, and coordination with public health experts, are potential solutions to encourage correct usage of PEP.
Comparisons were made between physicians and nonphysicians, which assumed that physicians would have higher baseline knowledge of rabies epidemiology and PEP administration than those who are not responsible for prescribing PEP within their scope of practice. However, few physicians participated, and physician respondents did not score significantly higher than non-physician respondents. While we did not see a difference between physicians and non-physicians, the small number of physicians responding did not provide adequate power to detect a difference. More physicians would have increased the power and could have led to a different result. Physician scores did follow a similar trend to those of nonphysicians with knowledge gained (30% increase) and knowledge retained (20% increase). The results add further support to the effectiveness of the module at improving long-term knowledge retention, regardless of the type of health professional.
A scenario-based online module was chosen to improve knowledge of rabies and PEP, because it can be easily tailored based on the rabies epidemiology of a region, and makes it easier to reach a broad range of providers in a large geographic region such as Arizona. This approach is supported by a published meta-analysis that reported that online CME courses are effective in increasing knowledge with a significant association with reported changes in provider practice (Cobb, 2004). Case-based scenarios are considered the most efficient way to increase competency in patient evaluation (Drexel et al., 2011; Tamler et al., 2011), and they were used to illustrate rabies exposure scenarios. Online learning courses have also been demonstrated to be a preferred route of education for physicians (Fordis et al., 2005), who often have limited time to get away from work to take in-person training and prefer flexible education times. These limitations likely apply to other health professionals, such as nurses; therefore, distance-based education or other online trainings should be considered as an alternative to more scheduled, in-person trainings or conferences. Additionally, knowledge of local communicable disease epidemiology is needed for optimal disease control and response. National conferences or other learning sources might include broader topics and might not be tailored to include local rabies epidemiology, thereby strengthening our argument that distance or online learning might be a better option for public health communicable disease topics, such as rabies.
This investigation has several limitations. First, no requirement was included to take all three tests, which limited our sample size and decreased power to detect differences. However, our results did demonstrate that the module was effective with significant improvement in scores comparing the pretest scores with both the posttest and retention test scores, despite the limited sample size. Additionally, this was a convenience sample, and data were not generalizable to health professionals in Arizona. Because respondents were self-selected, they might have a greater need for rabies PEP education than providers who did not complete the module or they might be more likely to encounter patients with rabies exposures. Another limitation was that the retention test could be taken anytime between 3 and 12 months after the module, and therefore, we can assume that knowledge retention would be higher if someone took the test 3 months later and knowledge retention would be lower if someone took the test 12 months later; this indicates a potential bias toward the null. Last, the module was designed for Arizona health care providers, but 67% of respondents resided outside of Arizona among those who took all three tests. Approximately 75% of respondents resided outside of Arizona among those who took only the pretest and posttest. More outreach and marketing might have resulted in more Arizona providers taking the module. However, no difference in knowledge gained or retained was identified when comparing Arizona respondents with those who reside outside of Arizona although the results did not have enough power to determine this.
Public Health Implications
Low pretest scores among respondents provide additional evidence to the growing body of literature demonstrating the need to educate health professionals about rabies PEP and could indicate a need for general public health communicable disease training (Gönen et al., 2011). Based on our findings, knowledge gaps regarding appropriate use of rabies PEP after a dog bite and location of the vaccine and RIG placement should be implemented, specifically. CE administrators should consider including rabies and other public health communicable disease topics in physician CME requirements. According to Evashwick (2013), the teaching of public health is more complicated than that of a single clinical discipline because public health is a discrete field that intersects with many others; and because public health is global and interdisciplinary, discussions about pedagogy must similarly engage representatives of multiple disciplines and locations, with the ultimate goal being to enhance the education of the current and future public health workforce to be effective in practicing public health around the world. The findings presented in this study demonstrate that this online rabies CE module with case-based scenarios was an effective tool to improve health care provider knowledge of rabies epidemiology and PEP both inside and outside of Arizona. Furthermore, this module can be easily adapted to include information about the rabies epidemiology of other geographic regions, as was done for this investigation, in addition to other public health communicable disease topics. Specifically, we recommend that health care providers take rabies CE modules relevant to their local rabies epidemiology. Because knowledge could be expected to decrease over time and recommendations for rabies prophylaxis could change over time, rabies CE should be updated regularly and education should be designed for professionals who recommend and prescribe PEP most frequently.
Acknowledgments
The authors thank the following persons for their assistance with this project: Bianca Salas, Andrew Strumpf, Miki Duruz, and Mac McCullough at Maricopa County Department of Public Health; Kristine Bisgard, Melissa Locket, Byron Robinson, and Michael (Paul) Reid at Centers for Disease Control and Prevention; Ken Komatsu at the Arizona Department of Health Services; and the developers of the original CME module that was adapted for this study.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Centers for Disease Control and Prevention, Arizona Department of Health Services, and Maricopa County Department of Public Health as part of their routine activity.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Association of American Medical Colleges. (2013). State physician workforce data book. Retrieved from https://www.aamc.org/download/362168/data/2013statephysicianworkforcedatabook.pdf [Google Scholar]
- Birhane MG, Cleaton JM, Monroe BP, Wadhwa A, Orciari LA, Yager P, … Wallace RM (2017). Rabies surveillance in the United States during 2015. Journal of the American Veterinary Medical Association, 250, 1117–1130. doi: 10.2460/javma.250.10.1117 [DOI] [PubMed] [Google Scholar]
- Brunette GW (2016). Infectious diseases related to travel: Rabies In CDC health information for international travel: The yellow book: 2016 New York, NY: Oxford University Press. [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Rabies: Cost of rabies prevention. Retrieved from https://www.cdc.gov/rabies/location/usa/cost.html [Google Scholar]
- Centers for Disease Control and Prevention Recommendations of the Advisory Committee on Immunization Practices. (2010). Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies. MMWR Recommendation Reports, 59(RR-2), 1–7. [PubMed] [Google Scholar]
- Cobb SC (2004). Internet continuing education for health care professionals: An integrative review. Journal of Continuing Education in the Health Professions, 24, 171–180. doi: 10.1002/chp.1340240308 [DOI] [PubMed] [Google Scholar]
- Cooper SP, McCormick JB, Chappell CL, Clare N, Vela L, Walker T, … Miller CS (2010). Texas needs physicians trained in public health: A new 4-year integrated MD/MPH degree program. Journal of the Texas Medical Association, 106, e1. [PubMed] [Google Scholar]
- Drexel C, Jacobson AD, Hanania N, Whitfield B, Katz J, & Sullivan T (2011). Measuring the impact of a live, case-based, multiformat, interactive continuing medical education program on improving clinician knowledge and competency in evidence-based COPD care. International Journal of Chronic Obstructive Pulmonary Disease, 6, 297–307. doi: 10.2147/copd.s18257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer JL, Yager P, Orciari L, Greenberg L, Wallace R, Hanlon CA, & Blanton JD (2014). Rabies surveil-lance in the United States during 2013. Journal of the American Veterinary Medical Association, 245, 1111–1123. doi: 10.2460/javma.245.10.1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evashwick CJ (2013). Educating the public health work-force. Frontiers in Public Health, 1, 20. doi: 10.3389/fpubh.2013.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fordis M, King JE, Ballantyne CM, Jones PH, Schneider KH, Spann SJ, … Greisinger A (2005). Comparison of the instructional efficacy of Internet-based CME with live interactive CME workshops: A randomized controlled trial. Journal of the American Medical Association, 294, 1043–1051. doi: 10.1001/jama.294.9.1043 [DOI] [PubMed] [Google Scholar]
- Garrison JA, Schardt C, & Kochi JK (2000). Web-based distance continuing education: A new way of thinking for students and instructors. Bulletin of the Medical Library Association, 88, 211–217. [PMC free article] [PubMed] [Google Scholar]
- Gönen I, Soysal A, Topuzoğlu A, & Bakir M (2011). Clinical knowledge and attitudes of Turkish physicians toward rabies caused by animal bites. Japanese Journal of Infectious Diseases, 64, 382–390. [PubMed] [Google Scholar]
- Heymann DL (2015). Control of communicable diseases manual (20th ed., pp. 497–508). Washington, DC: American Public Health Association. [Google Scholar]
- Jerrard DA (2004). The use of rabies immune globulin by emergency physicians. Journal of Emergency Medicine, 27, 15–19. doi: 10.1016/j.jemermed.2004.02.005 [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2017). Total number of professionally active nurses. Retrieved from http://www.kff.org/other/state-indicator/total-registered-nurses/?currentTimeframe=0&sortModel=%7B%22colId%22%3A%22Location%22%2C%22sort%22%3A%22asc%22%7D [Google Scholar]
- Moran GJ, Talan DA, Mower W, Newdow M, Ong S, Nakase JY, … Childs JE (2000). Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. Journal of the American Medical Association, 284, 1001–1007. doi: 10.1001/jama.284.8.1001 [DOI] [PubMed] [Google Scholar]
- National Association of State Public Health Veterinarians. (2011). Compendium of animal rabies prevention and control, 2011. Morbidity and Mortality Weekly Report, 60, 1–14. [PubMed] [Google Scholar]
- National Association of State Public Health Veterinarians. (2016). Compendium of animal rabies prevention and control, 2016. Journal of the American Veterinary Medical Association, 248, 505–517. [DOI] [PubMed] [Google Scholar]
- Robertson K, & Feldman K (2014). Clinician outreach to improve the quality of rabies postexposure prophylaxis administration: Maryland’s experience, 2010–2011. Vector-Borne and Zoonotic Diseases, 14, 454–460. doi: 10.1089/vbz.2013.1305 [DOI] [PubMed] [Google Scholar]
- Sisson JC, Swartz RD, & Wolf FM (1992). Learning, retention and recall of clinical information. Medical Education, 26, 454–461. doi: 10.1111/j.1365-2923.1992.tb00205.x [DOI] [PubMed] [Google Scholar]
- Tamler R, Green DE, Skamagas M, Breen TL, Looker HC, Babyatsky M, & Leroith D (2011). Effect of case-based training for medical residents on inpatient glycemia. Diabetes Care, 34, 1738–1740. doi: 10.2337/dc11-0517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidya SA, Manning SE, Dhankhar P, Meltzer MI, Rupprecht C, Hull HF, & Fishbein DB (2010). Estimating the risk of rabies transmission to humans in the U.S.: A Delphi analysis. BioMed Central Public Health, 10, 278. doi: 10.1186/1471-2458-10-278 [DOI] [PMC free article] [PubMed] [Google Scholar]