Abstract
Introduction:
The use of mini plates as a reduction tool is an elegant technique for temporary stabilization of multifragmentary fractures. For some complex periarticular fractures with severe comminution close to the articular surface, mini plates seem to be a better option than K-wires for provisional as well as definitive fixation, because of the presence of small fragments and proximity to the joint increases the risk of additional fragmentation and articular penetration, respectively.
Case Report:
Five cases of complex periarticular fractures of the upper limb are presented. We used 2.3 mm mini plates as reduction plates for different situations, including one scapula fracture, one clavicle fracture, one distal humerus fracture, one proximal ulna fracture, and one distal radius fracture. In all cases, an excellent clinical outcome with a full return to pain-free activity was achieved after a minimum follow-up of 12 months.
Conclusion:
We feel that these mini extra-articular implants are particularly helpful as temporary reduction tools before the application of the definitive implant to a reduced and stabilized the fracture. Because they have longer screws allowing better cortical purchase and low-profile allowing plate overlap, the procedure seems to be faster and easier when compared to the use of temporary K-wires and clamps.
Keywords: Upper extremity fractures, fracture reduction, fracture fixation, intraoperative management, plate osteosynthesis
Learning Point for this Article:
The potential indications of mini plates as temporary provisional reduction tools for definitive fixation are significant because this brings to the surgeons the possibility to work with reduced fractures without clamps or K-wires during the application of definitive implants.
Introduction
Articular fractures need absolute stability, which requires anatomic reduction and rigid fixation. However, maintaining the reduction is not always easy, especially when multifragmentary and unstable fractures are involved.
In general, the reduction is held in place by multiple K-wires and pointed reduction clamps. However, the position of the wires and/or clamps may sometimes interfere with the placement of definitive implants [1]. In addition, small structural metaphyseal or metadiaphyseal fragments can be stripped off the periosteal attachment during the introduction of K-wires [1, 2, 3, 4].
More recently, small plates have been introduced as temporary tools for stabilization and reduction [2, 3, 5]. These plates improve the quality of reduction and also reduce the risks and complications related to the use of wires and clamps. The main disadvantage of this technique is the potential difficulty in adequately positioning final implants because on some occasions the temporary plate is positioned exactly where the definitive plate should go [1].
The use of mini plate systems has recently been shown to reduce this problem since the final definitive plate can be applied over mini plates with no further exposure [1, 4]. We have been using mini plates as a provisional reduction tool for many periarticular fractures of the upper and lower limbs. We always leave the plate in a position like an additional fixation device for small fragment implants, as some injuries can be extremely difficult to maintain the reduction in place with K-wires and pointed clamps alone. In addition, we feel it is much easier to correctly position definitive implants with temporary hardware fixed in place.
We present a case series of five patients with distinct complex periarticular fractures of the upper limb. Our aim in this article is to present the technique for fixing periarticular fractures of the upper limb, with illustrations from cases.
Case Series and Surgical Technique
Patient 1 - Scapula fracture: A 40-year-old male medical doctor presented with a complex multifragmentary scapula fracture involving the glenoid fossa and extending to the spine of the scapula after he felt down a horse. We preferred to approach this injury with the patient in prone position and the ipsilateral upper limb abducted at 90° on a radiolucent hand table. After exposure of the fracture fragments, we manipulated them directly using small Weber clamps, small-diameter Schanz pins, and K-wires to obtain reduction. We could have fixed the temporary reduction with smooth 1.5 mm K-wires; however, those wires often block access to sites where definitive plates are to be placed. Provisional fixation was performed using a locked 2.3 mm plate and screws. The mini-plate was contoured and applied in the best position to hold the reduced fracture. More than one plate was used in different locations to help off-load stresses while the reduction was maintained. Some K-wires were maintained until final fixation with the 3.5 mm plate(s). Final fixation was performed with a one-third tubular plate positioned at the inferior edge of the glenoid fossa and along the lateral border of the scapula (Fig. 1).
Figure 1.
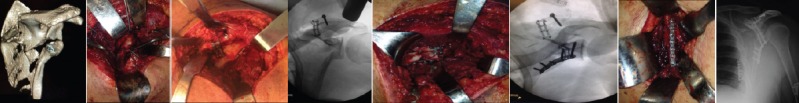
Complex scapula fracture involving the glenohumeral joint. Note the small 2.3-mm mini plates used as reduction plating, which eliminated the need to maintain the K-wires in place.
Patient 2 - Clavicle fracture: A 23-year-old male student presented with a mid-shaft clavicle fracture, with a large inferior third fragment. We felt it was important to achieve anatomical reduction of this small fragment. In this particular case, we preferred to approach the fracture with the patient in a beach chair position and the ipsilateral upper limb draped free. After a superior approach, we reduced the large third fragment with one of the main fragments, thus transforming the three-part fracture into two parts. We maintained the temporary reduction with one mini plate applied over the third fragment of the fracture. A second definitive small-fragment pre-contoured anatomical locked plate was applied to the dorsal aspect of this bone, guaranteeing rigid fixation of the fracture. Finally, the incision was closed in layers (Fig. 2).
Figure 2.
Mid-shaft complex clavicle fracture with a volar third fragment. Note the inferior 2.3 mm mini plate used as reduction plating. A second definitive small fragment pre-contoured anatomical locked plate was applied to the dorsal aspect of this bone, assuring rigid fixation of the fracture. Giordano V et al
Patient 3 - Distal humerus fracture: A 51-year-old female housewife presented with a complex 13-C3 type fracture, with coronal extension to the capitellum. She reported to fall down a stair in her house 1 day before she presented to the hospital. We decided to approach this injury with the patient in prone position and the elbow flexed at 90°. After beginning with a universal Campbell approach, the ulnar nerve was identified and protected. Then, we performed an extra-articular osteotomy of the tip of the olecranon to expose the fracture fragments. We began by directly manipulating the coronal component of the fracture using both small diameter Schanz pins and smooth K-wires to obtain reduction. We secured the temporary reduction with smooth 1.2 mm K-wires and continued with the reduction of the complex sagittal component of the Y fracture pattern. After final reduction and fixation with multiple K-wires, the coronal segment was fixed provisionally using a 2.3 mm plate and screws applied to the dorsal side of the lateral column of the distal humerus. Supplemental rigid plate fixation with pelvic reconstruction and one-third tubular plates was performed for the sagittal component of the fracture. Finally, the articular capsule and the marginal borders of the triceps tendon were sutured, and the olecranon osteotomy was fixed with an intramedullary long 3.5 mm cortical screw (Fig. 3).
Patient 4 - Proximal ulna fracture: A 33-year-old female dentist presented with a complex multifragmentary proximal ulna fracture with olecranon and coronoid involvement after a motorcycle accident. We approached the injury with the patient in prone position, and the elbow flexed at 90°. The universal Campbell approach was used both to expose the fracture fragments and to reduce the dislocations (ulnohumeral or proximal radioulnar joint). Temporary fixation was achieved with smooth 1.5 mm K-wires; however, these were not sufficient to adequately hold the comminuted fragments in place. Thus, 2.3-mm plates and screws were applied to secure the reduced fracture. We used more than one plate in different places to secure the reduction. K-wires were removed after provisional plating fixation. Stable anatomic final fixation of the ulna was performed with a long small-profile locked contoured plate positioned at the dorsal aspect of this bone. The final plating overlapped the dorsally positioned mini plate (Fig. 4). Finally, ligamentous component of the injury was addressed and repaired by transosseous reinsertion.
Patient 5 - Distal radius fracture: A 27-year-old female librarian presented with a complex articular distal radius fracture with a metaphyseal split on the volar ulnar side of the radius. She reported to fall down when she was skating. We decided to approach this injury with the patient in supine position and the upper limb on a radiolucent hand table. The Henry volar approach was used to expose the fracture fragments. We reduced the split fragment first and secured the temporary reduction with a smooth 1.2 mm K-wire passed from medial to lateral. We fixed the split fragment using a 2.3 mm plate and screws applied to the apex of the fracture to avoid shearing of this fragment. Final rigid plate fixation with a volar anatomic distal radius locked plate was performed (Fig. 5).
Figure 3.
Intraoperative images showing the application of a 2.3-mm mini plate as reduction plating for the capitellar component of a distal humerus fracture. Note the extra-articular osteotomy of the olecranon.
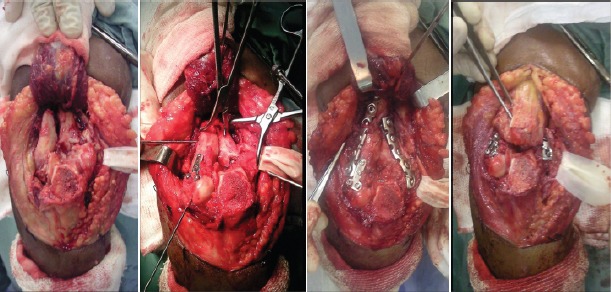
Figure 4.

Complex multifragmentary proximal ulna fracture with olecranon and coronoid involvement. In this patient, two 2.3-mm mini plates were used as reduction plating. Giordano V et al
Figure 5.
Complex distal radius fracture with both shearing on the volar ulnar side and impaction on the volar radial side. In this case, one 2.3-mm mini plate was used as reduction buttressing plating on the ulnar side. Intraoperative images showing the temporary reduction on the ulnar aspect of the distal radius with a K-wire. Note the marginal impaction on the radial side (arrow with large rounded base). We applied for a 2.3-mm mini plate as reduction plating. The scaphoid (open arrow) and volar capsule (closed arrow) can be seen distally.
Post-operative protocol
The post-operative protocol was mainly modulated by the patients’ pain. Regular subcutaneous or oral opioid drugs were administered to address post-operative pain. Early active motion was started as soon as possible under the supervision of a physical therapist. The patient with the proximal ulna fracture used an articulated elbow splint during ligament healing (around 6 weeks), but the controlled movement was allowed with the progressive increase of range of motion.
Outcome
We have not experienced intraoperative or immediate post-operative complications, including location of the final plate, loss of final fixation, or soft tissue irritation. In addition, we did not need to remove broken or prominent mini plates after the fractures had healed.
In the patient with a trans olecranon fracture-dislocation, we had to remove the implants from the ulna because the mini plate directly impinged on the proximal radioulnar joint and did not permit full rotation of the forearm. In this particular case, we needed to apply for one mini plate on the volar metaphyseal aspect of the proximal ulna, since there was severe fragmentation in this area (coronoid component). Despite a second operation to remove this implant, the patient presented a good result with an average 120° arc of motion for elbow flexion-extension and 110° for forearm rotation.
Functional restoration of the operated joints and segments was achieved in a period of 6 months post-operative for the scapula fracture and 9 months for periarticular injuries of the elbow, with a mean of 7.3 months.
Discussion
In recent years, several authors have pointed out difficulties in obtaining and maintaining reduction of some complex articular and periarticular fractures using standard reduction clamps and multiple K-wires, mainly when there is severe comminution close to the articular surface. In addition, these reduction tools require further stripping of the bone and are generally not useful when the surgeon performs limited exposure techniques.
The concept of reduction plating was introduced by Benirschke et al. and popularized by Archdeacon and Wyrick [2, 3]. The rationale is very simple but elegant and consists of the application of small diameter, low-profile plates at provisional states of reduction to maintain the reduction until definitive fixation can be applied [3]. Initially, the use of one-third tubular plates proved sufficient to control the reduction of proximal tibia fractures during intramedullary nailing and, therefore, has been expanded to routine use of reduction plating in the management of comminuted metadiaphyseal and diaphyseal fractures [2, 3, 4]. These implants have many advantages in complex shaft fractures, such as conforming and deforming to the shape of the bone [4]. However, their use can be difficult in many periarticular fractures on the upper limb because of the presence of very small fragments and due to the proximity to the joint, situations that increase the risk of more fragmentation and articular penetration, respectively.
Oh et al. proposed a modification of this technique using mini plates, theoretically reducing the potential complications of the one-third tubular plates [1]. As these authors stated, the main advantage of the modified technique is that the final definitive plate can be applied over the mini implants. These authors had no complications in their experience with 39 patients. This was the first series to highlight the advantages of mini plates as temporary fixation in various periarticular and/or metaphyseal locations with good results. Recent literature using the modified concept of reduction plating has also demonstrated satisfactory results, and we agree [5, 6].
Another advantage of the modified technique is the ability to use a variety of plates in different shapes and designs, expanding their application to fit the exact morphology of the fracture [1]. In our cases, we used straight plates, X-plates, lattice-shaped plates, and oblique L-plates, among others, which greatly facilitated temporary stabilization of structurally important fragments to restore anatomic alignment before definitive fracture fixation.
Although there is still uncertainty on how to accurately identify the ideal mini implant, we prefer to use 2.3-mm mini plates. We feel these implants are easier to handle and present a superior strength compared to smaller implants such as the 2.0-mm and 1.5-mm mini plates. Even using 2.3-mm mini plates, we often found during surgery that it was necessary to keep some of the K-wires in place to maintain the temporary reduction we achieved. In addition, 2.3-mm and other stronger plates (2.4-mm and 2.7-mm) normally have the option for longer screws in the set. In many situations, longer screws are necessary for better cortical purchase with reduction plating.
In our cases, we normally used titanium mini plates and stainless steel small fragment plates, which may raise some questions related to combining different types of metal in the fracture environment. Indeed, there have been warnings against combining different metals in orthopedic devices, since galvanic corrosion may result due to the existing electrochemical potential difference between dissimilar biomaterials. The least noble metal in a galvanic coupling is more likely to corrode, with subsequent failure of the implants and bone healing [7]. However, contrary to prior belief, it has recently been shown that mini titanium plates can be used to assist as reduction plating in combination with stainless steel plates without adversely affecting healing [8, 9]. In addition, Høl et al. demonstrated no higher weight loss or metal release in combinations of dissimilar screws and plates compared to a single-material construction, indicating comparable clinical safety [7]. In our cases, we had no bone healing problems such as delayed healing and nonunion or the development of systemic illness.
In the actual paper, we described the indications and the technique of mini plates as provisional reduction instruments for upper limb injuries, what can be seen as a potential weakness. Some may argue that this is not a new technique and thus do not consider this “innovative” or new to trauma surgeons. As a matter of fact, we believe this is still a growing technique among upper extremity and general orthopedic surgeons that deal with traumatic injuries.
Conclusion
We feel that these mini extra-articular implants are particularly helpful as temporary reduction tools before the application of the definitive implant to a reduced and stabilized the fracture. Because they have longer screws allowing better cortical purchase and low-profile allowing plate overlap, the procedure seems to be faster and easier when compared to the use of temporary K-wires and clamps.
Clinical Message
The potential indications of mini plates as temporary provisional reduction tools for definitive fixation are significant because this brings to the surgeons the possibility to work with reduced fractures without clamps or K-wires during the application of definitive implants. The use of a variety of plates in different shapes and designs expands their application to fit the exact morphology of the fracture.
Biography
Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Oh JK, Sahu D, Park JW, Oh CW, Hwang JH. Use of 2.0 mini plate system as reduction plate. Arch Orthop Trauma Surg. 2010;130:1239–42. doi: 10.1007/s00402-009-1008-4. [DOI] [PubMed] [Google Scholar]
- 2.Archdeacon MT, Wyrick JD. Reduction plating for provisional fracture fixation. J Orthop Trauma. 2006;20:206–11. doi: 10.1097/00005131-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Benirschke SK, Henley MB, Ott JW. Proximal one-third tibial fracture solutions. Orthop Transactions. 1995;18:1055–6. [Google Scholar]
- 4.Dunbar RP, Nork SE, Barei DP, Mills WJ. Provisional plating of Type III open tibia fractures prior to intramedullary nailing. J Orthop Trauma. 2005;19:415–7. doi: 10.1097/01.bot.0000153446.34484.70. [DOI] [PubMed] [Google Scholar]
- 5.Diwersi N, Babst R, Link BC. Miniplates as augmentation implants in osteosynthesis of complex distal radius fractures. Oper Orthop Traumatol. 2016;28:402–6. doi: 10.1007/s00064-016-0469-1. [DOI] [PubMed] [Google Scholar]
- 6.Scolaro JA, Beingessner D. Treatment of monteggia and transolecranon fracture-dislocations of the elbow. A critical analysis review. J Bone Joint Surg Rev. 2014;2:e3. doi: 10.2106/JBJS.RVW.M.00049. [DOI] [PubMed] [Google Scholar]
- 7.Høl PJ, Mølster A, Gjerdet NR. Should the galvanic combination of titanium and stainless steel surgical implants be avoided? Injury. 2008;39:161–9. doi: 10.1016/j.injury.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Acevedo D, Loy BN, Lee B, Omid R, Itamura J. Mixing implants of different metallic composition in the treatment of upper-extremity fractures. Orthopedics. 2013;36:e1175–79. doi: 10.3928/01477447-20130821-21. [DOI] [PubMed] [Google Scholar]
- 9.Hayes JS, Richards RG. The use of titanium and stainless steel in fracture fixation. Expert Rev Med Devices. 2010;7:843–53. doi: 10.1586/erd.10.53. [DOI] [PubMed] [Google Scholar]




