Abstract
Background:
Studies in neurologically intact subjects suggest that the gradual presentation of small perturbations (errors) during learning results in better transfer of a newly learned walking pattern to over ground walking. Whether the same result would be true after stroke is not known.
Objective:
To determine whether introducing gradual perturbations, during locomotor learning using a split-belt treadmill influences learning the novel walking pattern or transfer to over ground walking post-stroke.
Methods:
Twenty-six chronic stroke survivors participated and completed the following walking testing paradigm: Baseline overground walking; Baseline treadmill walking; Split-belt treadmill/Adaptation period (belts moving at different speeds); Catch trial (belts at same speed); Post overground walking. Subjects were randomly assigned to the Gradual group (gradual changes in treadmill belts speed during Adaptation) or the Abrupt group (a single, large, abrupt change during Adaptation). Step length asymmetry adaptation response on the treadmill and transfer of learning to over ground walking were assessed.
Results:
Step length asymmetry during the Catch trial was the same between groups (p=0.195) confirming that both groups learned a similar amount. The magnitude of transfer to over ground walking was greater in Gradual than Abrupt group (p=0.041).
Conclusions:
The introduction of gradual perturbations (small errors), compared to abrupt (larger errors), during a locomotor adaptation task seems to improve transfer of the newly learned walking pattern to over ground walking post-stroke. However, given the limited magnitude of transfer, future studies should examine other factors that could impact locomotor learning and transfer post-stroke.
Keywords: Stroke, Locomotion, Rehabilitation, Motor Learning
INTRODUCTION
Stroke is the third leading cause of death and the main cause of disability in adults worldwide.1 Although most subjects regain the ability to walk after stroke,2 deficits in the functions of the lower extremities frequently persist, affecting their walking ability and functional mobility.3,4 In this context, motor (re)learning is fundamental, and is the basis of post-stroke rehabilitation.5 However, the literature provides limited information about the process of locomotor relearning after stroke.
Recently, a group of studies utilizing the principles of motor adaptation applied to walking have gained interest in the rehabilitation community because of their unique ability to target specific gait deviations.6–9 In these studies, motor adaptation has a specific definition: it is the process of modifying or adjusting a movement from trial to trial on the basis of error feedback10 such that a new movement pattern is temporarily learned to respond to new task demands. Once the adaptation is complete, if the new demand is removed (post-adaptation period), movements are again erroneous, but this time in the opposite manner, because the adapted pattern remains. These initial, oppositely directed errors are termed aftereffects. With continued practice with the new task demands removed, the movement pattern returns to baseline.9
Previous studies have shown that post-stroke subjects retain the ability to make locomotor adaptations.6,11,12 A split-belt treadmill was used, which comprises two separate belts that permit the speed of each belt (i.e. each leg) to be controlled independently. In general, the stroke survivors performed similarly to healthy controls regarding symmetry responses during the adaptation period (when belts were set to different speeds) and the post-adaptation period (when belts returned to the same speeds). These findings demonstrated that stroke survivors are indeed remarkably adept at modifying their walking pattern to accommodate changing task demands.6
Critical to advancing locomotor rehabilitation after stroke is determining the factors that influence the generalizability of newly learned walking patterns from one context to the next.8 This is crucial for the design of rehabilitation interventions that will result in improved walking beyond the clinical setting. Some locomotor adaptation studies have shown minimal transfer to new environmental contexts or demands.13,14 Reisman and colleagues (2009)8 found that both stroke and neurologically intact subjects demonstrated partial transfer of the aftereffects observed on the treadmill to over ground walking following split-belt treadmill walking. However, it is noteworthy that transfer was only partial. It is thought that this partial transfer may be due to the type and size of errors that the subjects were learning to correct on the split-belt treadmill.8
Exploring this further, a recent study15 demonstrated that the type of errors experienced during the split-belt treadmill adaptation strongly affects the transfer to over ground walking in neurologically intact people. Gradual speed changes, compared to abrupt changes, decreased the adaptation response on the treadmill but increased locomotor learning transfer to over ground walking.15 That means that when errors are small enough to fall within a subject’s normal repertoire (i.e., subject’s baseline variability), the adapted walking pattern transfers to natural over ground walking. In contrast, large errors that are outside the normal range lead to an adapted pattern that does not transfer, regardless of stronger learning on the treadmill. It seems that we may be able to facilitate transfer simply by changing how we introduce errors,15 considering the effects that the error size might have during learning. Whether this same result would be true in chronic stroke survivors is still not known. Furthermore, the level of clinical impairment and its relationship to adaptive capacity post-stroke has been previously explored6 and we aimed to extend these findings by exploring the relationship between clinical impairment and transfer of learning from treadmill to over ground walking.
Therefore, the aim of this study was to determine whether introducing new perturbations gradually or abruptly during locomotor learning on a split-belt treadmill influences the adaptation response and improves transfer of learning to over ground walking in subjects post-stroke. We hypothesized that gradual, compared to abrupt, changes during locomotor adaptation would result in a similar amount of learning but better transfer to over ground walking in people post-stroke. Furthermore, we hypothesized that the transfer capacity might relate to subject’s initial clinical impairments.
METHODS
Subjects
This was a parallel-group randomized study conducted at a single center in the United States. Twenty-six subjects with post-stroke hemiparesis participated in this study. Subjects were recruited from a variety of sources including stroke support groups, physical therapy and physician offices and advertisements. The inclusion criteria were: 1) Age 21–85; 2) Single, unilateral, chronic stroke (>6 months post date of stroke), confirmed by MRI or CT scan; 3) Able to walk without assistance from another person (assistive device allowed); 4) Resting heart rate between 40–100 beats per minute, 5) Resting blood pressure between 90/60 to 170/90. Subjects were excluded if they had: 1) Evidence of cerebellar stroke on clinical MRI or CT scan, because of the role of the cerebellum in learning; 2) Other neurologic conditions in addition to stroke; 3) Inability to walk outside the home prior to the stroke; 4) Coronary artery bypass graft or myocardial infarction within past 3 months previous to participation; 5) Musculoskeletal pain that limits walking; 6) Inability to communicate with investigators; 7) Neglect as identified using the star cancellation test; 8) Unexplained dizziness in the previous 6 months.
Clinical Assessment
A clinical assessment was performed prior to the learning and transfer paradigm. The following clinical tests were performed: a) 10 meter walk test - a measure of short-distance walking speed. Subjects perform 3 trials each at their self-selected and fastest speed;16 b) lower extremity portion of the Fugl-Meyer Assessment - a test that measures coordination, reflexes and the ability to move in and out of synergy in the lower extremities;17 c) Functional Gait Assessment (FGA), a 10-item assessment of dynamic balance during various walking tasks.18 The FGA has demonstrated validity, responsiveness, and reliability for assessment of walking function in persons with stroke.19
Walking paradigm
The testing paradigm consisted of walking on a split-belt treadmill and over ground. Subjects adapted their walking pattern on a split-belt treadmill, and their response on the treadmill and transfer of this learning to over ground walking (i.e., off the treadmill) were tested. For the treadmill portion, subjects were asked to walk on a custom-built treadmill (Bertec Corporation, Columbus, OH, USA) consisting of 2 separate belts, each with its own motor that permitted the speed of each belt (ie, each leg) to be controlled independently. The speed of the belts were unique for each subject and the fast treadmill belt speed was determined by increasing the treadmill speed until: (1) the participant declined further increase in treadmill speed or (2) the researcher determined that it was unsafe to further increase the speed. The “slow” speed was half of the patient’s fast walking speed. During different testing periods, subjects walked on the treadmill with the 2 belts either moving at the same speed (“tied” configuration) or at different speeds (“split-belt” configuration). During the tied configuration, treadmill belt speeds were set at the subject’s predetermined slow speed. In the split-belt configuration, one treadmill belt was set at the subject’s slow speed whereas the other was set at the fast speed. Subjects with symmetric step length during baseline or with a greater paretic step length (compared to non-paretic side) were included. However, we standardized the SBT walking paradigm always assigning the paretic leg to the slow belt.
The gait analysis session consisted of 6 testing periods (Figure 1). In the “Over ground Baseline period,” subjects walked over ground at their self-selected gait speed for 10 trials. One trial equaled 1 pass down a 5-m walkway. In the “Treadmill Baseline period,” subjects walked on the treadmill with the belts tied at their slow speed for 2 minutes. In the “Adaptation period,” the treadmill belts were split (one belt fast and the other belt slow) for 15 minutes. After 10 minutes of Adaptation, the belts returned briefly (30 seconds) to the tied slow configuration (“Catch Trial”). Following this, the belts were split for another 5 minutes to complete the total 15 minutes of Adaptation. In the “Over ground Post-adaptation period”, all subjects walked over ground for 10 trials. Finally, the subjects walked on the treadmill in the belts-tied configuration for 5 minutes following the final trial of over ground walking (“Washout period”). This allowed us to test for washout of the treadmill aftereffect due to over ground walking.8,15 The treadmill belts were stopped between each period. Subjects were transported in a wheelchair between the treadmill and overground walking to ensure that no walking other than that collected by the motion capture system would occur between the treadmill and overground periods. Figure 1 illustrates this experimental paradigm.
Figure 1.
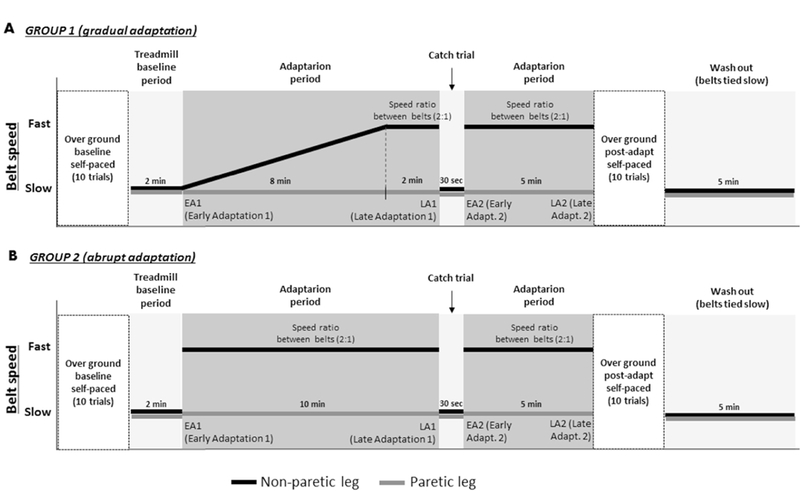
Time course for the experimental paradigm showing Baseline, Adaptation, Catch and Washout periods in over ground and treadmill walking. A) Belt speed time course for experimental group 1 (gradual adaptation). B) Belt speed time course for experimental group 2 (abrupt adaptation).
Experimental design.
To determine whether errors during adaptation can be manipulated to improve the adaptation response and transfer of walking adaptation on a treadmill to natural walking, subjects were randomly assigned, following simple randomization procedures (computerized random numbers), to one of two experimental groups:
Group 1: gradual adaptation (n=13). Subjects post-stroke adapted gradually to keep their error size small during adaptation. During the first 8 min of adaptation, the belt under the non-paretic leg linearly increased its speed from the slowest speed to the faster speed, until belts reached a 2-to-1 ratio. From the 8th to the 10th minute, the belts were kept at this 2-to-1 ratio. After the 30-sec Catch Trial period (when both belts were moving at the same speed), the belts were maintained at a 2-to-1 ratio for an additional 5 min to readapt the walking pattern (in case any washout had occurred during the Catch Trial period)15 before testing the learning transfer to over ground walking (Figure 1A).
Group 2: abrupt adaptation (n=13). Subjects post-stroke adapted with an abrupt perturbation to expose them to a large size error size during adaptation. During the entire 15 minutes of the Adaptation period, the belts were maintained at a 2-to-1 ratio, except during Catch Trial period when the belts were tied at the slow speed, as described for the gradual group (Figure 1B).
Motion capture testing.
Subjects walked on our custom-built split-belt treadmill instrumented with two 6-component force platforms (Bertec, Columbus OH) and over ground. Retro-reflective marker data was recorded with an 8 camera Vicon Motion Analysis System at a sampling frequency of 100 Hz. Markers and clusters were placed according to Tyrell et al (2014).11 Foot contact and lift-off was determined using kinematics.20 For safety purposes, all subjects held onto a front handrail while walking on the treadmill, and wore a ceiling-mounted safety harness around the upper chest during over ground and treadmill walking. The harness did not support body weight or interfere with subjects’ walking. Subjects were allowed to take rest breaks as requested during treadmill walking or between over ground walking trials.
Data Analysis
Learning and transfer magnitudes were measured using step length asymmetry as the main variable. Considering step length as the anterior–posterior distance between the ankle markers at the time when each foot contacted the ground, step length symmetry was examined according to the following:21
A step length symmetry value of 0 indicates that step lengths are equal, a positive value indicates that the paretic limb is taking longer steps, and a negative value indicates that the non-paretic limb is taking longer steps.
The average of all steps for over ground (OG) baseline and treadmill (TM) baseline were considered for analysis. The very first step was removed from all over ground conditions to avoid including step initiation. Then, the first 10 strides of split-belt walking periods were considered early adaptation (EA), whereas the last 10 strides of the split-belt treadmill walking periods were considered late adaptation (LA). The first 5 strides of the post-adaptation periods (e.g.- Catch Trial and OG Post Adaptation) were considered for analysis.6,8,22
The magnitude of learning was measured as the after-effect in step length (a)symmetry during treadmill walking (Catch Trial), minus step length (a)symmetry during treadmill baseline walking. This subtraction of baseline (a)symmetry is essential to allow comparison across subjects with varying levels of baseline step (a)symmetry.
To determine the transfer of aftereffects observed on the treadmill to over ground walking we calculated a Transfer Index:8
where OGpost is the mean of step length symmetry of the first 5 strides in the Over ground Post adaptation period, OGbase is the mean of step length symmetry of all strides in the Over ground Baseline period, TMcatch is the mean of step length symmetry of the first 5 strides during the Catch Trial, and TMbase is the mean of step length symmetry of all strides in the Treadmill Baseline period.
To determine the extent to which walking over ground walking washed out after-effects on the treadmill, we calculated a washout index:
where TMcatch is the mean of the first 5 strides during the Catch Trial, TMwash is the mean of the first 10 strides in the Washout period, and TMbase is the mean of all strides in the Treadmill Baseline period.
Custom written scripts in MATLAB (MathWorks Inc, Natick, MA) were used for all analyses.
Statistical Analysis
Data were tested for normality and homogeneity using Shapiro-Wilk and Levene tests, respectively and non-parametric statistics were used when data was found to be non-normally distributed. The independent t-test was applied to compare differences between groups regarding learning and transfer. Comparison between groups for Washout Index was performed using a Mann-Whitney test. The effect size was calculated for the variables that obtained significant difference between groups. Effect size (ES) was calculated using Cohen’s d, and was deemed small above 0.2, medium above 0.5 and high above 0.8. Its precision is shown as 95% confidence interval (95% CI).23,24 Spearman R correlations were performed to test for relationships between Transfer Index and ordinal clinical measures (eg, lower extremity Fugl-Meyer and FGA). Pearson product moment correlations were performed to test for relationships between Transfer Index and OG comfortable walking speed. The level of statistical significance for all measures were set at P < .05, and all statistical calculations were completed using SPSS version 22.0-J (IBM, Tokyo, Japan) software.
RESULTS
A total group of 62 hemiparetic subjects from the local community in Newark, Delaware, were assessed for eligibility from March, 2016 to January, 2017. Twenty-eight subjects met the inclusion criteria and agreed to participate in this study. They were randomly allocated to Abrupt Group (n=14) or Gradual Group (n=14). All participants completed the experimental procedure. Only 2 subjects were excluded from analysis. One subject lost her balance during Overground Walking (post), but was able to recover walking by herself, however, this affected her step length for several steps and these changes were unrelated to the transfer of after-effect. Another subject experienced issues with the safety harness, which was getting stuck on the track during some trials. Therefore, a total of 13 subjects were analysed and included in each group (Figure 2). No adverse effects were observed during data collection. Characteristics of both groups are presented in Table 1. No significant differences were found between groups at baseline.
Figure 2.
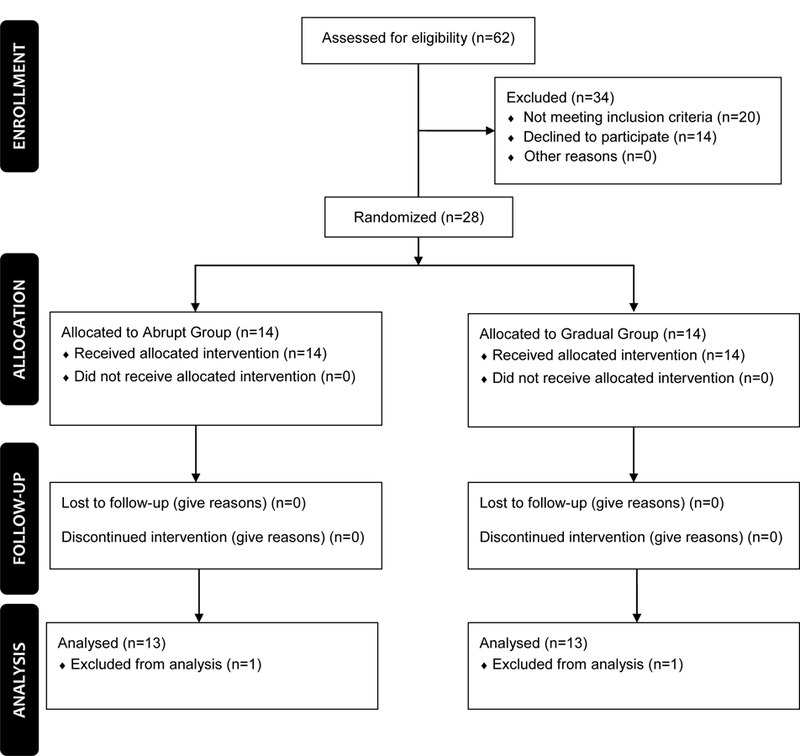
Flow diagram of study.
Table 1.
Sample characterization and comparisons between groups (Gradual X Abrupt) at baseline.
| Variables |
Gradual group (n=13) |
Abrupt group (n=13) |
P value |
|---|---|---|---|
| Age (years) | 59 (13) | 58 (13) | 0.778 |
| Gender (F/M) | 8 / 5 | 2 / 11 | --- |
| Hemiparesis Side (R/L) | 8 / 5 | 3 / 10 | --- |
| Time post-stroke (months) | 64 (23) | 66 (55) | 0.626 |
| Fugl Meyer (LE total score) | 22 (15–34) | 23 (13–34) | 0.663 |
| FGA (total score) | 17 (14–23) | 18 (11–28) | 0.519 |
| OG Comfortable Walking Speed (m/s) | 0.88 (0.26) | 0.83 (0.27) | 0.669 |
| OG Fastest Walking Speed (m/s) | 1.21 (0.35) | 1.14 (0.33) | 0.605 |
| TM Fastest Walking Speed (m/s) | 0.98 (0.27) | 0.82 (0.19) | 0.090 |
| OG baseline - Step Length Symmetry | 0.04 (0.02) | 0.07 (0.03) | 0.413 |
| TM baseline - Step Length Symmetry | 0.01 (0.02) | 0.07 (0.03) | 0.130 |
Abbreviations: F, Female; M, Male; R, Right; L, Left; LE, lower extremity; FGA, Functional Gait Assessment; OG, Over ground; TM, Treadmill. Data expressed as mean (standard deviation), except Fugl Meyer and FGA, expressed as median (minimum-maximum) and OG/TM baseline step length symmetry, expressed as mean (SE).
Learning and transfer response
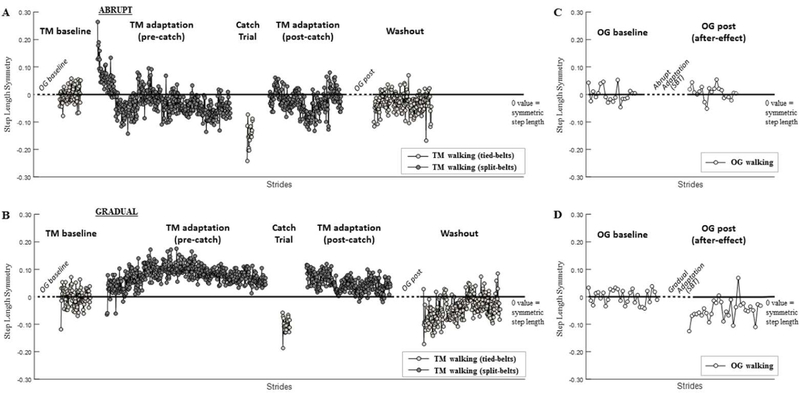
Figure 3 shows examples of step length (a)symmetry values over the course of treadmill (3A and 3B) and over ground walking (3C and 3D) from representative subjects in the Abrupt group (3A and 3C) and Gradual group (3B and 3D). Early in the Adaptation period for the Abrupt group subject, the step length is substantially more asymmetric than at baseline, but then adapts back to baseline over many steps (Figure 3A). On the other hand, at the start of the Adaptation period for the subject in the Gradual group, the step length is similar to that in the Treadmill Baseline period since the belts are still tied at the same speed (Figure 3B). Over the course of the gradual paradigm, the belts are gradually split. If the subject was able to perfectly adjust step length to adapt to the changing belt speeds, step length (a)symmetry would remain unchanged. This subject was not able to perfectly adapt and thus there are small increases in asymmetry between the beginning and end of the 10 minutes of Adaptation (Figure 3B). Both of these examples illustrate the reverse asymmetry (ie, aftereffect) in the Catch Trial period, when they returned to tied belts. A limited aftereffect is observed during the Over ground Post-adaptation period for either subject, however does appear to be greater for the subject in the Gradual group (3D) than Abrupt group (3C), i.e., the over ground walking after the gradual adaptation during treadmill walking is more asymmetric compared to baseline over ground walking for this subject).
Figure 3.
Individual representative data of step length (a)symmetry for all sequential strides taken during treadmill (3A and 3B) and over ground walking (3C and 3D). Representative subjects that underwent an abrupt split-belt paradigm (A and C) and a gradual paradigm (B and D) are shown. A value of zero represents step length symmetry (normalized by baseline). Note that the placement of the over ground walking periods are indicated in Figures 3A and 3B, but this data is shown in Figures 3C and 3D. Abbreviations: TM, Treadmill; OG post, Over ground post adaptation.
To ensure that the initial perturbation was different between groups, we compared the (a)symmetry value at early adaptation during the Adaptation period between groups (Figure 4A). As expected, the difference is greater in the Abrupt group than in the Gradual Group (ES: 1.89, 95% CI: (−0.21) – (−0.08), p<0.001), confirming that subjects in the Gradual group experienced smaller errors in step length (a)symmetry than Abrupt group. Second, to confirm if the Catch Trial period differently influenced subjects in the Gradual and Abrupt groups, we compared if the difference between the late adaptation pre-catch and the early adaptation post catch were the same across groups (Figure 4B). No differences were observed (p=0.829). In other words, the difference between step length symmetry value immediately after the Catch Trial period and immediately prior to the Catch Trial period was the same in the Gradual and Abrupt groups. Third, to understand if the adaptation response after the Catch Trial period was the same regardless the group, the difference between the early adaptation and late adaptation post catch was also compared across groups (Figure 4C). No differences were observed (p=0.536).
Figure 4.
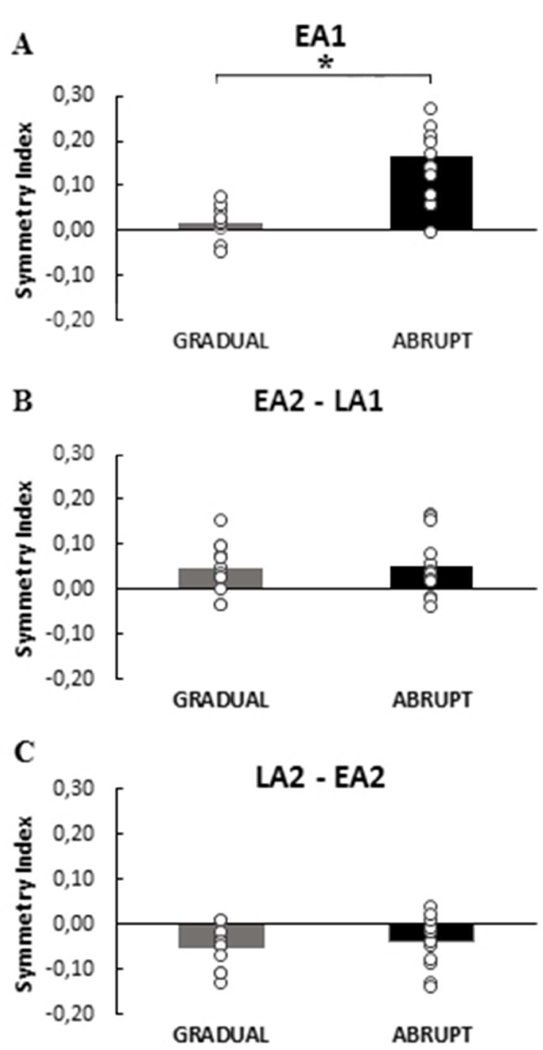
Comparisons between groups Gradual (gray bars) and Abrupt (black bars) for step length symmetry differences between time points. To ensure that the initial perturbation was different between groups, we compared the symmetry value at early adaptation (EA1) between groups (A). To confirm that the catch trial did not differently influence the groups, we compared the difference between the late adaptation pre catch (LA1) and the early adaptation post catch (EA2) between groups (B). The difference between the early adaptation (EA2) and late adaptation (LA2) post catch were also compared across groups (C). Zero on the y-axis for (A) is relative to baseline (a)symmetry and for (B) and (C) represents no difference across treadmill testing periods within the group. Error bars indicate ± standard deviation. Asterisk indicates a significant difference between groups.
Figure 5 shows the main comparisons between groups, regarding learning magnitude on the treadmill, transfer to over ground walking and washout response. Both groups showed the same magnitude of aftereffect on the treadmill, i.e., same magnitude of learning on the treadmill regardless of the split belt treadmill paradigm, gradual or abrupt (p=0.195; Figure 5A). The magnitude of transfer to over ground walking, in relation to learning during treadmill walking (Transfer Index), was greater in the Gradual group than the Abrupt group (ES: 0.86, 95% CI: 0.20 – 0.93, p=0.041; Figure 5B). No differences between groups were observed in the Washout Index (p=0.326; Figure 5C).
Figure 5.
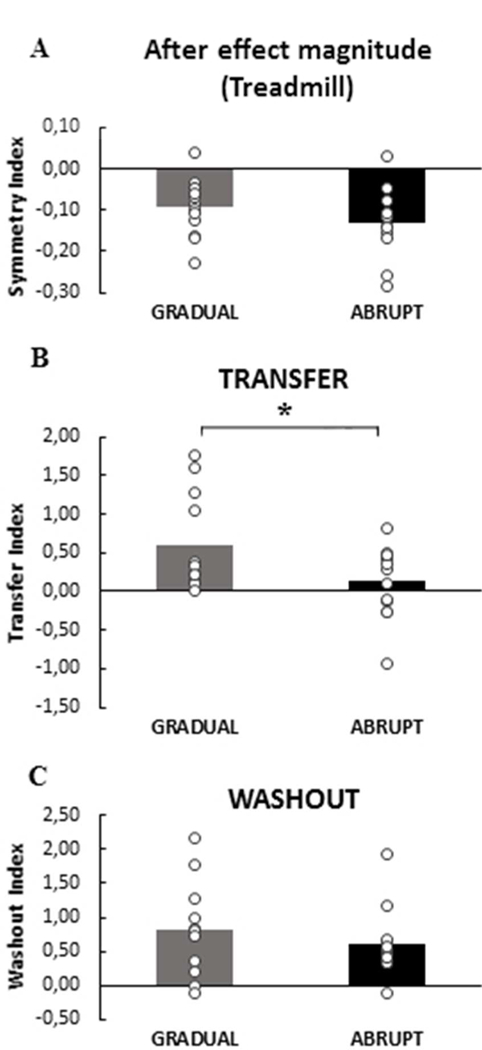
Comparisons between groups Gradual (gray bars) and Abrupt (black bars) for step length symmetry. (A) The same magnitude of aftereffect (catch trial) on the treadmill was observed between groups. Note that the after effect is normalized by step length symmetry during treadmill baseline, therefore a zero value equals no difference compared to baseline. (B) The transfer index indicates the amount of adaptation transfer from the treadmill to over ground walking in each group. (C) Washout represents if the OG walking washed out the treadmill effects on locomotor learning. A greater value equals better transfer / washout. Note that no differences were observed between groups (p>0.05). Error bars indicate ± standard deviation. Asterisk indicates a significant difference between groups.
Impairment Level and Transfer Magnitude to Over ground Walking
Correlation analyses were performed to test for relationships between stroke survivors’ impairments (clinical measures) and their locomotor learning capacity and its transfer to over ground walking. No correlations were observed between Transfer Index and Fugl Meyer LE score (p=0.617), FGA score (p=0.778) or OG comfortable walking speed (p=0.736).
DISCUSSION
In this study, we examined whether perturbations introduced gradually (small errors) or abruptly (large errors) during a locomotor learning task affect the transfer of learning to over ground walking in subjects post-stroke. Interestingly, we found that increasing the speed of one belt on a split-belt treadmill gradually, compared to abruptly, does enhance transfer to over ground walking post-stroke. The introduction of different error sizes during treadmill walking, however, did not modulate the washout of treadmill aftereffects following over ground walking. These findings provide information regarding how different types of errors experienced during a locomotor adaptation task affect learning and transfer to over ground walking after stroke.
A previous study showed that step length symmetry adaptation transfers from treadmill (abrupt perturbation) to overground walking in persons poststroke.8 In our study, however, the transfer to overground walking was not as apparent following an abrupt perturbation during SBT locomotor learning. This inconsistency might be explained by the greater variability of transfer among subjects observed in the present study compared to the previous study. There were also a number of potentially important methodological differences between the two studies, including the calculation of step length asymmetry and the inclusion of the first step of over ground walking (step initiation) in the previous study.8 In the present study, we adapted the subjects on the treadmill such that the after-effect would always occur in the same direction, which was not done in the previous study. This is important because in our previous work, we have shown that the split-belt configuration influences adaptation and after-effect magnitudes in persons with stroke.25 That is, the initial perturbation, magnitude of adaptation and after-effect is influenced by whether the belt configuration augments the subjects baseline asymmetry or induces greater symmetry when the belts are initially split. Given this finding, we opted in the present study to configure the split-belts such that the initial perturbation and the after-effects would always occur in the same direction for all subjects. This is an important difference in methodology between the two studies. The differing results between the two studies also highlight the importance of replicating studies that included a relatively small sample.
Previous studies have shown that transfer of a newly learned walking pattern in response to new demands or environmental contexts is minimal in neurologically intact subjects13 or partial in subjects post-stroke.8 Therefore, recent studies have investigated strategies to maximize locomotor learning and its transfer to other contexts. The size of error experienced during a locomotor task is one of the factors that has been investigated for its effect on transfer.15 In neurologically intact subjects, Torres-Oviedo and Bastian (2012)15 showed reduced learning but better transfer to over ground walking after a gradual introduction of a split-belt walking perturbation, compared to an abrupt perturbation. Interestingly, the present study results also showed greater transfer to over ground walking after gradual split-belt perturbation in stroke survivors.
These results may be explained in the context of the idea of credit assignment in motor learning and transfer.26 Credit assignment is the idea that the central nervous system seeks to assign an error to a specific source.26 That is, if an individual assigns an error to a particular context or environment, then the learned response to this error will not transfer to a new context or environment; conversely, if the error is assigned to themselves, individuals transfer the learned response more effectively. Recent studies in neurologically intact subjects suggest that perturbations to movement that result in small errors will likely transfer better to other contexts or environments because the nervous system ascribes the movement errors to the person rather than to another source.15,27 This has important implications for the present study of chronic stroke survivors whose natural error size (step length asymmetry) and variability is quite large.28
With this in mind, it is important to highlight that, although gradual (compared to abrupt) perturbations during split-belt treadmill walking seem to afford benefits in transfer of learning to over ground walking, the magnitude of transfer was small and variable among those post-stroke, even in the Gradual group. It is noteworthy that for more than half the subjects (9 in Gradual, 8 in Abrupt) the step length (a)symmetry during post-adaptation over ground walking was not greater than the over ground baseline step length asymmetry variability (SD). That is, for most of the subjects the “signal” (step length asymmetry) during the over ground post-adaptation period was not outside the “noise” (over ground baseline step length variability). In fact, a previous study showed that the asymmetry magnitudes need to exceed baseline over ground levels to reach conscious awareness in subjects post-stroke.29 Studies in healthy subjects suggest that perception of step length asymmetry on the split-belt treadmill does not occur until the ratio of the slow belt speed to fast belt speed is above 0.85.30 Thus, it is suggested that for locomotor pattern correction and learning in those post-stroke, the spatiotemporal asymmetry may need to be augmented beyond what these subjects usually present during walking in order to promote awareness of asymmetric gait patterns.29 It is possible, therefore, that more than half the subjects evaluated in the present study (even in the Gradual group) did not perceive their step length asymmetry during post-adaptation over ground walking as different from their usual baseline over ground, which may have limited the transfer to over ground walking.
This result may help to explain the finding that, despite differences in transfer, over ground walking washed out the treadmill learning similarly across groups (e.g.-no differences in step length asymmetry during the Washout period after over ground walking). Generally, it is expected that the washout of after-effects will follow a pattern related to the amount that was transferred15 (i.e., greater transfer would result in greater washout). This was not what was observed. Rather, despite greater transfer to over ground walking in the Gradual group, the step length asymmetry when subjects returned to the treadmill (during Washout) was the same between groups. This could be explained by the relationship between the magnitude of step length asymmetry during post-adaptation over ground walking relative to the baseline variability of step length asymmetry. As described above, despite greater transfer in the Gradual group, the magnitude of asymmetry during the Over ground Post-adaptation period for most subjects in both groups did not exceed their step length asymmetry variability during the Over ground baseline period. Without a difference in the error driving de-adaptation between subjects in the two groups, we would expect the washout of the new pattern during over ground walking to be the same between groups, which is what was observed. Interestingly , the previous study of gradual versus abrupt split-belt walking in neurologically intact subjects found the same result, greater transfer in the Gradual group, but no difference in Washout Index between groups15. In that study, the lack of between group differences in wash-out was attributed to the strong contextual cues presented by walking on the treadmill. Our results suggest an additional explanation; if the magnitude of transfer is not sufficiently large, it may not produce a meaningful error signal that would result in de-adaptation.
Another interesting finding in this study is the absence of significant correlation between the transfer of learning to over ground walking and clinical impairments. These results are in accordance with previous studies that also evaluated locomotor learning using a split-belt treadmill.6 In this sense, it could be argued that the impairment level post-stroke might not influence the locomotor learning on a split-belt treadmill. That means subjects with moderate or mild impairments post stroke would have the same capacity to adapt and transfer the locomotor learning to over ground walking, regardless if the perturbations during treadmill walking task were applied gradually or abruptly. However, it is worth mentioning that it also might be the case that the clinical tools used to assess the clinical impairments were not sensitive enough to detect functional differences that would lead to different learning level capacities. Future studies should specifically compare groups with different functional levels to confirm these hypotheses.
Given that motor learning is fundamental to neurologic rehabilitation, it is therefore essential that we develop a greater understanding of how to improve the transfer or generalization of locomotor learning after stroke. This understanding will help clinicians and researchers to develop optimal interventions to improve walking function in patients beyond the clinical setting. The results of this study suggest that if the goal is to generalize what is learned in a clinical setting to a more natural environment, it seems that error size may play a role. However, factors other than error size should also be considered. For example, a previous study examining interlimb transfer following adaptation to abrupt and gradual schedules during a reaching task in healthy subjects, suggested that the overall exposure duration seems to be a key factor impacting transfer capacity, while the magnitude of transfer did not differ between groups.31 Studies of transfer of a newly learned movement in neurologically intact subjects suggest that factors such as cognitive information, contextual information, and error timing impact transfer.32–34 The effect of these factors on transfer in persons post-stroke should be investigated.
Limitations
The results of this study must be considered in the context of its limitations. First, future studies should evaluate a greater number of subjects, comparing different levels of impairment, which could help clinicians to better understand factors that would maximize the intervention effects for a specific population. For example, including subjects with very slow walking speeds would expand our knowledge regarding adaptation capacity according to different walking impairment levels. Due to limitations in the data collection setting, the over ground walking assessment consisted of several trials instead of a long distance walk. Future studies testing over ground walking should assess gait in a context where more strides in a row are performed. In addition, during treadmill walking all subjects held onto a front handrail, which could have served as a contextual cue, and might have limited the over ground transfer and washout effect observed. If so, this effect was consistent across groups, however, still must be considered in the interpretation of the results. While it would be ideal to eliminate this potential contextual cue, in our experience only very high functioning stroke survivors are able to walk on the split-belt treadmill without handrail use.
CONCLUSIONS
Our findings suggest that introduction of gradual perturbations (small errors) compared to abrupt (larger errors) during a locomotor adaptation task improves transfer of the newly learned walking pattern to over ground walking post-stroke. However, considering that the magnitude of transfer was small and variable among subjects post-stroke, future studies should examine other factors that could impact locomotor learning and transfer in this population.
ACKNOWLEDGMENTS
Financial Support
This study was supported by the National Institutes of Health (NIH), USA (grant: NIH R01 HD078330; NIH S10RR028114-01) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Brazil (grant: 2015/19197-4).
Footnotes
Disclosures
Authors have no conflicts of interest to disclose.
REFERENCES
- 1.World Health Organization (WHO) Guidelines Approved by the Guidelines Review Committee. Prevention and Control of Noncommunicable Diseases: Guidelines for Primary Health Care in Low Resource Settings In: Geneva: 2012. [PubMed] [Google Scholar]
- 2.Preston E, Ada L, Dean CM, Stanton R, Waddington G. What is the probability of patients who are nonambulatory after stroke regaining independent walking? A systematic review. International journal of stroke : official journal of the International Stroke Society 2011;6(6):531–540. [DOI] [PubMed] [Google Scholar]
- 3.Gerrits KH, Beltman MJ, Koppe PA, et al. Isometric muscle function of knee extensors and the relation with functional performance in patients with stroke. Archives of physical medicine and rehabilitation 2009;90(3):480–487. [DOI] [PubMed] [Google Scholar]
- 4.Chisholm AE, Perry SD, McIlroy WE. Correlations between ankle-foot impairments and dropped foot gait deviations among stroke survivors. Clinical biomechanics 2013;28(9–10):1049–1054. [DOI] [PubMed] [Google Scholar]
- 5.Levin MF, Kleim JA, Wolf SL. What do motor “recovery” and “compensation” mean in patients following stroke? Neurorehabilitation and neural repair 2009;23(4):313–319. [DOI] [PubMed] [Google Scholar]
- 6.Reisman DS, Wityk R, Silver K, Bastian AJ. Locomotor adaptation on a split-belt treadmill can improve walking symmetry post-stroke. Brain 2007;130(Pt 7):1861–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanchette A, Bouyer LJ. Timing-specific transfer of adapted muscle activity after walking in an elastic force field. Journal of neurophysiology 2009;102(1):568–577. [DOI] [PubMed] [Google Scholar]
- 8.Reisman DS, Wityk R, Silver K, Bastian AJ. Split-belt treadmill adaptation transfers to overground walking in persons poststroke. Neurorehabilitation and neural repair 2009;23(7):735–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reisman DS, Bastian AJ, Morton SM. Neurophysiologic and rehabilitation insights from the split-belt and other locomotor adaptation paradigms. Physical therapy 2010;90(2):187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin TA, Keating JG, Goodkin HP, Bastian AJ, Thach WT. Throwing while looking through prisms. II. Specificity and storage of multiple gaze-throw calibrations. Brain 1996;119 ( Pt 4):1199–1211. [DOI] [PubMed] [Google Scholar]
- 11.Tyrell CM, Helm E, Reisman DS. Learning the spatial features of a locomotor task is slowed after stroke. Journal of neurophysiology 2014;112(2):480–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betschart M, Lauziere S, Mieville C, McFadyen BJ, Nadeau S. Changes in lower limb muscle activity after walking on a split-belt treadmill in individuals post-stroke. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology 2017;32:93–100. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds RF, Bronstein AM. The moving platform aftereffect: limited generalization of a locomotor adaptation. Journal of neurophysiology 2004;91(1):92–100. [DOI] [PubMed] [Google Scholar]
- 14.McVea DA, Pearson KG. Long-lasting, context-dependent modification of stepping in the cat after repeated stumbling-corrective responses. Journal of neurophysiology 2007;97(1):659–669. [DOI] [PubMed] [Google Scholar]
- 15.Torres-Oviedo G, Bastian AJ. Natural error patterns enable transfer of motor learning to novel contexts. Journal of neurophysiology 2012;107(1):346–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plummer P, Behrman AL, Duncan PW, et al. Effects of stroke severity and training duration on locomotor recovery after stroke: a pilot study. Neurorehabilitation and neural repair 2007;21(2):137–151. [DOI] [PubMed] [Google Scholar]
- 17.Fugl-Meyer AR, Jaasko L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med 1975;7(1):13–31. [PubMed] [Google Scholar]
- 18.Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Physical therapy 2004;84(10):906–918. [PubMed] [Google Scholar]
- 19.Lin JH, Hsu MJ, Hsu HW, Wu HC, Hsieh CL. Psychometric comparisons of 3 functional ambulation measures for patients with stroke. Stroke; a journal of cerebral circulation 2010;41(9):2021–2025. [DOI] [PubMed] [Google Scholar]
- 20.Zeni JA Jr., Richards JG, Higginson JS. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait & posture 2008;27(4):710–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Savin DN, Morton SM, Whitall J. Generalization of improved step length symmetry from treadmill to overground walking in persons with stroke and hemiparesis. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology 2014;125(5):1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malone LA, Bastian AJ. Spatial and temporal asymmetries in gait predict split-belt adaptation behavior in stroke. Neurorehabilitation and neural repair 2014;28(3):230–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen J Statistical Power Analysis for the Behavioral Sciences 2nd edn. Hillsdale, New Jersey: L. Erlbaum;. 1988. [Google Scholar]
- 24.Faraone SV. Interpreting estimates of treatment effects: implications for managed care. Pharmacy and Therapeutics 2008;33(12):700–711. [PMC free article] [PubMed] [Google Scholar]
- 25.Tyrell CM, Helm E, Reisman DS. Locomotor adaptation is influenced by the interaction between perturbation and baseline asymmetry after stroke. Journal of Biomechanics 2015;48(11):2849–2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berniker M, Kording K. Estimating the sources of motor errors for adaptation and generalization. Nature neuroscience 2008;11(12):1454–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei K, Kording K. Relevance of error: what drives motor adaptation? Journal of Neurophysiology 2009;101(2):655–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patterson KK, Gage WH, Brooks D, Black SE, McIlroy WE. Evaluation of gait symmetry after stroke: a comparison of current methods and recommendations for standardization. Gait & posture 2010;31(2):241–246 [DOI] [PubMed] [Google Scholar]
- 29.Wutzke CJ, Faldowski RA, Lewek MD. Individuals Poststroke Do Not Perceive Their Spatiotemporal Gait Asymmetries as Abnormal. Physical therapy 2015;95(9):1244–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lauzière S, Miéville C, Duclos C, Aissaoui R, Nadeau S. Perception threshold of lomocotor symmetry while walking on a split-belt treadmill in healthy elderly individuas. Percept Mot Skills 2014;118(2):475–490. [DOI] [PubMed] [Google Scholar]
- 31.Joiner WM, Brayanov JB, Smith MA. The training schedule affects the stability, not the magnitude, of the interlimb transfer of learned dynamics. Journal of Neurophysiology 2013;110(4):984–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fercho K, Baugh LA. It’s too quick to blame myself-the effects of fast and slow rates of change on credit assignment during object lifting. Front Hum Neurosci 2014;8:554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fercho K, Baugh LA. Cognitive attribution of the source of an error in object-lifting results in differences in motor generalization. Experimental brain research 2016;234(9):2667–2676. [DOI] [PubMed] [Google Scholar]
- 34.Kluzik J, Diedrichsen J, Shadmehr R, Bastian AJ. Reach adaptation: what determines whether we learn an internal model of the tool or adapt the model of our arm? Journal of neurophysiology 2008;100(3):1455–1464 [DOI] [PMC free article] [PubMed] [Google Scholar]