Abstract
Objectives:
This cadaveric study sought to evaluate the accuracy of syndesmotic reduction using direct visualization via an anterolateral approach compared to palpation of the syndesmosis through a laterally based incision.
Methods:
Ten cadaveric specimens were obtained and underwent baseline CT scans. Subsequently, a complete syndesmotic injury was simulated by transecting the anterior inferior tibiofibular ligament (AITFL), posterior tibiofibular ligament (PITFL), transverse ligament, interosseous membrane, and deltoid ligament. Three orthopaedic trauma surgeons were then asked to reduce each syndesmosis using direct visualization via an anterolateral approach. Specimens were then stabilized and underwent post-reduction CT scans. Fixation was then removed, the anterolateral exposure closed, and the surgeons were then asked to reduce the syndesmosis using palpation only via a direct lateral approach. Specimens were again instrumented and underwent post-reduction CT scans. Two tailed paired t-tests were used to compare reductions with baseline scans with significance set at p<0.05.
Results:
There was no statistically significant difference between reduction via direct visualization or palpation via lateral approach when compared with baseline scans. Although measurements did not reach significance, there was a tendency towards external rotation, and anteromedial translation with direct visualization and a trend towards fibular external rotation and posterolateral translation with palpation.
Conclusions:
There is no difference in reduction quality using direct visualization or palpation to assess the syndesmosis. Surgeons may therefore choose either technique when reducing syndesmotic injures based on personal preference and other injury factors.
Introduction
Injuries to the syndesmosis are particularly challenging to treat as indications and treatment techniques continue to evolve. Such injuries are commonly seen by orthopedists, either as an isolated ligamentous injury or in combination with an associated ankle fracture. 1–3 In both situations, the resulting shift of the tibio-talar articulation can dramatically change contact mechanics of the ankle joint. 4,5 Historically, syndesmosis injuries have been associated with long-term dysfunction6 and malreduction is associated with worse functional outcomes 7,8; however, the threshold at which a malreduction becomes clinically relevant remains controversial. 9,10 Regardless, malreduction of the syndesmosis has been reported as high as 52%, leading to abundant research and innovation regarding the optimal technique for syndesmotic reduction. 11
Previously described techniques to optimize reduction include fluoroscopic comparison of the contralateral side, intra-operative computed tomography (CT) scan, and direct visual assessment at the time of surgery. 11–17 After surgery, CT assessment is considered the gold standard for assessing reduction quality.7,9,11,18–20
Open reduction of the syndesmosis means different things to different surgeons. Some advocate an anterolateral approach to the ankle which facilitates visualization of the fibula within the incisura as well as the articular congruity of the distal tibia, distal fibula, and talus while others consider the optimal open reduction strategy to involve accessing the incisura through a lateral or posterolateral fibular incision which allows the surgeon to palpate the reduction between tibia, fibula, and talus but does not allow for direct visualization. Each technique has distinct advantages and disadvantages but the comparative accuracy of these techniques is unknown. The purpose of this study was to evaluate the accuracy of syndesmotic reduction using direct visualization via an anterolateral approach compared to palpation of the syndesmosis though a laterally based incision. Our null hypothesis was that there would be no significant differences in reduction quality using these two techniques.
Materials and Methods
Ten cadaveric below knee specimens with the proximal tibiofibular joint intact (8 male, 2 female, avg 72.5 years old [range: 69–88 years old]) were obtained. All specimens underwent baseline imaging with a C-arm cone-beam computed tomography (CBCT) system (Artis Zeego, Siemens Healthcare GmbH, Forchheim, Germany) with 0.2 mm axial cuts.
A 0.062 in K-wire was used to mark the level 1 cm above the joint level as a reference point to ensure that reduction assessment was consistently evaluated using the same axial level. The deltoid ligament was exposed via direct medial approach and completely transected. The anterior inferior tibiofibular ligament (AITFL) was then exposed via an anterolateral approach and completely transected. That same approach was then extended proximally to the proximal fibular head and the interosseous ligament was transected completely. Lastly, the posterior inferior tibiofibular ligament (PITFL) and transverse ligaments were exposed via a posterolateral approach and completely transected completing the simulated syndesmotic injury. After sectioning of the syndesmotic ligaments the fibula was grossly unstable on our exam. Next, three fellowship trained orthopaedic trauma surgeons reduced the syndesmosis on each specimen using direct visualization via anterolateral approach (Fig. 1). Reductions were stabilized with one 0.062 in K wire and an axial CT scan was obtained. Next, the anterolateral incision was closed and these same surgeons destabilized and then reduced the syndesmosis by palpation through a lateral incision (Fig 2). Reductions were again stabilized with one 0.062 in K wire and axial CT scans were performed to assess reduction quality (Fig 3). The fibula was manually displaced prior to each reduction attempt.
Fig 1.

Direct visualization of the anterior syndesmosis was used via an anterolateral approach to assess reduction quality and the reduction was fixed with a K wire.
Fig 2.

After initial reduction with direct visualization, the anterolateral incision was closed and the ankle approached from direct lateral incision. Finger palpation was then used to assess reduction quality and reduction was fixed with a K wire.
Fig 3.
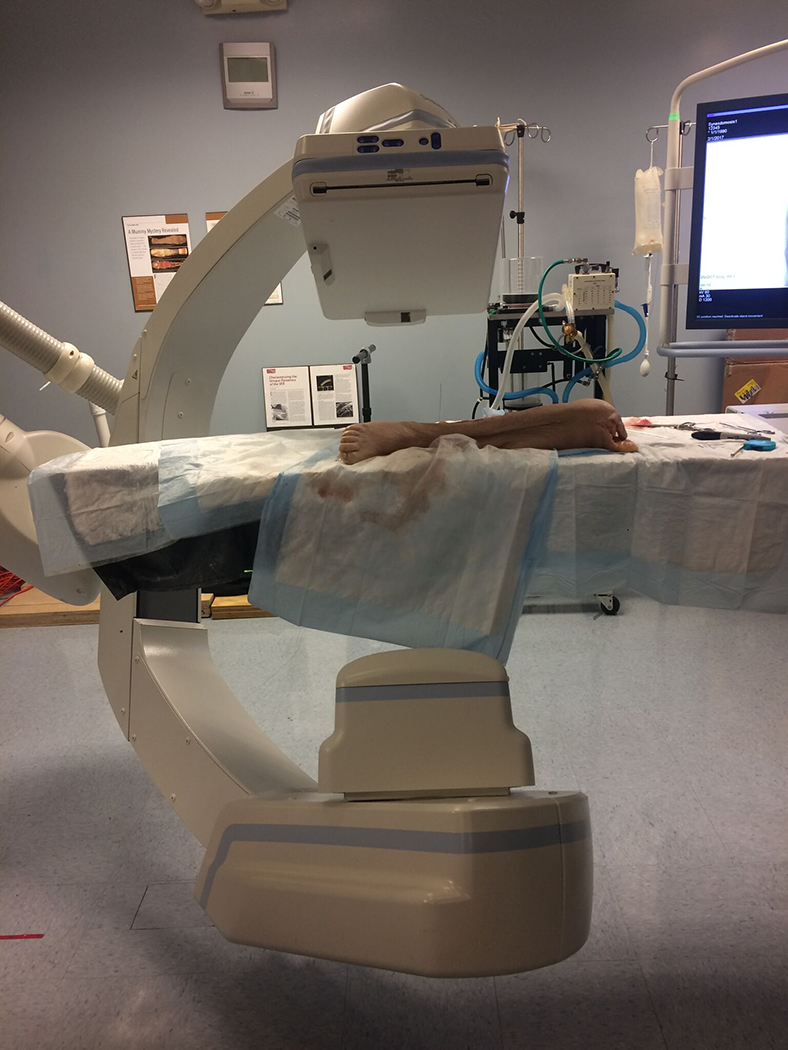
Image demonstrating CBCT system used to obtain axial imaging for assessment of reduction quality.
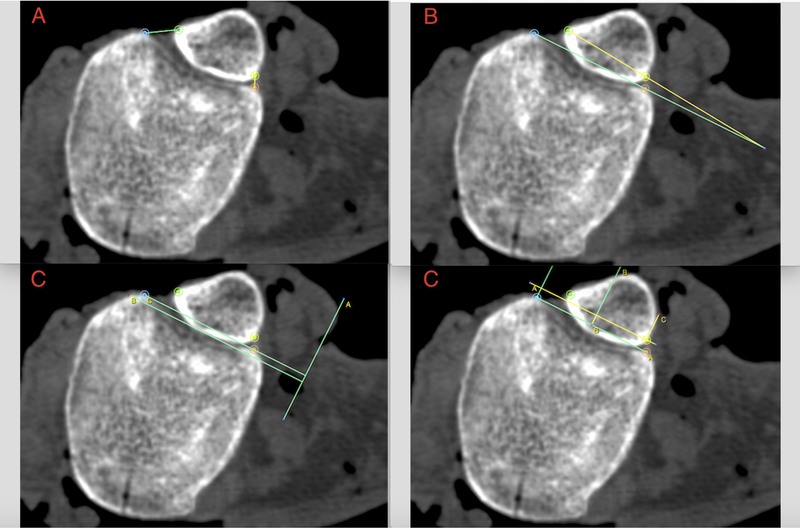
Reduction quality was evaluated using the following methods:
Rotation was measured by the ratio of the distance between the most anterior and posterior points of the fibula and tibia at the incisura (Fig 4a). 9,11
Rotation was measured by the angle between a line tangential to the anterior and posterior tibial tubercles and a line through the anterior and posterior fibular tubercles (Fig 4b).9,11,19
Lateral translation was measured as the distance between the medial fibula and tibia at the level of incisura (Fig 4c). 9,19
Anterior-posterior translation was measured as the distance between a line bisecting a line from the most anterior/posterior portions of the incisura and the most posterior portion of the fibula (Fig 4d). 18
Fig 4.
(a) Rotation assessed by ratio of distance between the most anterior and posterior points on the fibula and tibia. (b) Rotation assessed by angle between the tangential to the anterior and posterior tibial tubercles and the line through the anterior and posterior fibular tubercles. (c) Lateral translation measured as distance between medial fibula and tibia. (d) Anterior-posterior translation assessed as distance between a line bisecting the incisura and the most posterior portion of the fibula.
Baseline imaging and each reduction attempt by each surgeon were evaluated blindly and independently by two orthopaedic surgery residents using the four methods described above.
Statistical Analysis
The intraclass correlation coefficient was used to assess reliability between reviewers for each method, and the average measurement between the two observers was used for analysis. Reduction quality amongst surgeons for each method was compared using intraclass correlation coefficient to assess reliability across surgeons for each measurement. The measurements made by the three surgeons were averaged for each technique and used for comparison to baseline scans. For each method, the difference between the average measurements amongst the surgeons and baseline scans were compared using two tailed paired t-tests with significance set at p<0.05.
Results
Comparing direct visualization to the baseline scans, there was no statistically significant difference in any of the measures used to assess accuracy of reduction (p>0.05) (see Table, Supplemental Digital Content 1, which demonstrates mean differences of measurements between reduction by direct visualization and baseline measurements). Although not statistically significant, using direct visualization to assess reduction did lead to more external rotation of the fibula using both measurement techniques 1 (0.7+/− 0.3 vs 0.7 +/− 0.2, p = 0.17) and method 2 (9.6° +/− 6.6 vs 9.9° +/− 4.5°, p = 0.85). Using the third measurement technique, there was more medial translation (1.4mm +/− 1.4 mm vs 1.4 mm +/− 0.8 mm, p = 0.09). Lastly, using the fourth measurement technique, there was more anterior translation (8.1 mm +/− 1.3 mm vs 8.9 +/−1.4mm, p = 0.10).
Similarly, reduction using palpation showed no statistically significant differences in rotation or translation when compared to baseline scans (p>0.05) (see Table, Supplemental Digital Content 2, which demonstrates mean differences of measurements between reduction by palpation and baseline measurements). Reductions using palpation showed a tendency to externally rotate the fibula using measurement methods 1 (0.8 +/− 0.5 vs. 0.7 +/− 0.2, p = 0.50) and 2 (9.6° +/− 7° vs 9.9° +/− 4.5°, p=0.90). Using method 3, the fibula was more laterally translated (1.2 mm +/− 1.5 mm vs 1.4 mm +/− 0.8 mm, p= 0.66). Lastly, using method 4, the fibula was more posteriorly translated (9.0mm +/− 2.2 mm vs 8.9mm +/−1.4 mm, p = 0.81).
The interobserver reliability for each method of evaluation between the two observers is shown in Table 1. The intraclass correlations indicated good to excellent reliability between the observers; therefore, we averaged their measurements during our analysis. We also examined reliability among the three surgeons with intraclass correlations indicating good to excellent agreement. Because the quality of reduction between the surgeons was similar we averaged their scores to examine differences between open reduction and palpation.
Table 1.
Interobserver reliability between observers measuring the scans was good to excellent.
| Method | Reliability of Raters |
|---|---|
| Rotation Ratio | 0.71 |
| Rotation angle | 0.83 |
| Lateral Translation | 0.84 |
| Anterior-Posterior Translation | 0.83 |
Discussion
Our study revealed that syndesmotic reduction via anterolateral approach with direct visualization or via palpation through a lateral incision resulted in equivalent and high-quality reductions. Surgeons may therefore choose either approach when reducing syndesmotic injures based on personal preference and other injury details. For instance, when a lateral or posterolateral approach has already been performed for fibular reduction and fixation, syndesmotic reduction by palpation may be most appropriate to avoid additional incisions. However, if the surgeon is foregoing fibular reduction and fixation in favor of reducing and stabilizing only the syndesmosis, an anterolateral approach may make it easier to simultaneously judge translation, rotation and length. Combing either of these approaches with well described intra-operative fluoroscopic evaluation should optimize outcome. 15,21–23
Our results are consistent with previous research demonstrating that open reduction improves the accuracy of syndesmotic stabilization. Miller et al reported diminished rates of incongruity with direct visualization of the anterior incisura compared to fluoroscopic reduction alone (18% [17/97] vs 52% [13/25]). 24 Sagi et al retrospectively reviewed patients with syndesmosis injuries and also reported a reduced rate of malreduction using open visualization compared to closed or indirect methods (15% [2/13] vs 44% [24/55]). Although this difference did not reach statistical significance, the authors recommended the use of open visualization for syndesmosis reduction. 7
Furthermore, both reduction methods used in this study utilized manual reduction of diastasis rather than using a clamp. Using a clamp to obtain and hold a reduction is a commonly used technique. Recent studies demonstrate that the clamp use may predispose to iatrogenic malreduction depending on the orientation of the clamp. Additionally, clamp use can lead to significant syndesmosis overcompression. 13,14,17 Although recent evidence suggests that small degrees of malreduction may be well tolerated clinically10, the high rate of iatrogenic malreduction with clamping has led the authors to recommend manual reduction techniques as used in this study.
There are a number of limitations to our study. Our use of a cadaveric model may not fully simulate the instability experienced in vivo and therefore may affect the ease and/or quality of reduction. We recognize that our study design may introduce bias due to the lack of randomization of specimens and the reuse of specimens for each reduction technique. To minimize any bias introduced by previous reduction attempts we ensured that each reduction was not performed sequentially and attendings did not have access to the imaging attempts until data collection was complete. We did not create fibula fractures in our models and therefore assumed an anatomic fibular reduction. Syndesmosis reduction and fixation with an unreduced or malreduced fibula may have yielded different results. Accurate fibular reduction remains important in the treatment of syndesmosis injuries. Furthermore, the syndesmoses in this study were reduced by surgeons who treat a high volume of ankle fractures and their reductions may not be generalizable to all orthopaedic surgeons. Additionally, reductions were supported with a single 0.062 in K wire. In our clinical practice it is our standard protocol to manually reduce the syndesmosis and fix it with a single tricortical or quadricortical 0.062 in K wire rather than 2 K wires or other means of fixation. We have found this to be sufficient in holding our reductions and therefore used this technique in this study. Additionally, definitive fixation with a screw or suture device was not performed. Although unlikely, it is possible that definitive fixation could have altered the accuracy of reduction. Finally, although we created a clinically relevant cadaveric model of a syndesmosis injury, the implication of syndesmosis malreduction remains controversial. While some studies support the importance of reduction quality for achieving good outcomes, 7,8,25 others have found lower correlations between reduction accuracy and clinical outcome. 9,10Given the available clinical data, some surgeons believe that there is a threshold value below which minor syndesmosis malreductions are not clinically relevant. Despite the fact that some degree of malreduction may be tolerated by the patient, anatomic reduction should remain the goal of the surgeon.
Ours is the first study to directly compare reductions of the syndesmosis obtained via direct visualization versus palpation. Our study showed no difference between these techniques, indicating that either is adequate in accomplishing a near anatomic reduction. Surgeon preference and other details therefore have a role in this clinical situation. Future research should explore the clinical implications of these distinct approaches on patients treated surgically for syndesmotic injury.
Supplementary Material
Mean difference between reductions using direct visualization and baseline measurements showed no significant differences in any measurement.
Mean difference between reductions using palpation and baseline measurements showed no significant differences in any measurement.
References
- 1.Hunt KJ., George E., Harris AH., et al. Epidemiology of syndesmosis injuries in intercollegiate football: incidence and risk factors from National Collegiate Athletic Association injury surveillance system data from 2004–2005 to 2008–2009. Clin J Sport Med 2013;23(4):278–282. [DOI] [PubMed] [Google Scholar]
- 2.Waterman BR., Belmont PJ, Cameron KL, et al. Risk Factors for Syndesmotic and Medial Ankle Sprain: Role of Sex, Sport, and Level of Competition. Am J Sports Med 2011;39(5):992–8. Doi: 10.1177/0363546510391462. [DOI] [PubMed] [Google Scholar]
- 3.Hopkinson WJ., Pierre PS., Ryan JB., et al. Syndesmosis sprains of the ankle. Foot Ankle 1990;10(6):325–330. [DOI] [PubMed] [Google Scholar]
- 4.Ramsey P, Hamilton W Changes in tibiotalar contact caused by lateral talar shift. J Bone Jt Surg Am 1976;58(3):356–7. [PubMed] [Google Scholar]
- 5.Lloyd J, Elsayed S, Hariharan K, et al. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int 2006;27(10):793–796. [DOI] [PubMed] [Google Scholar]
- 6.Gerber JP., Williams GN., Scoville CR., et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int 1998;19(10):653–660. [DOI] [PubMed] [Google Scholar]
- 7.Sagi HC., Shah AR., Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma 2012;26(7):439–443. [DOI] [PubMed] [Google Scholar]
- 8.Weening B, Bhandari M Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 2005;19(2):102–108. [DOI] [PubMed] [Google Scholar]
- 9.Warner SJ., Fabricant PD., Garner MR., et al. The Measurement and Clinical Importance of Syndesmotic Reduction After Operative Fixation of Rotational Ankle Fractures. J Bone Jt Surg 2015;97(23):1935–44. Doi: 10.2106/JBJS.O.00016. [DOI] [PubMed] [Google Scholar]
- 10.Cherney SM., Cosgrove CT., Spraggs-Hughes AG., et al. Functional Outcomes of Syndesmotic Injuries Based on Objective Reduction Accuracy at a Minimum 1-Year Follow-Up: J Orthop Trauma 2018;32(1):43–51. Doi: 10.1097/BOT.0000000000001000. [DOI] [PubMed] [Google Scholar]
- 11.Gardner MJ., Demetrakopoulos D., Briggs SM., et al. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int 2006;27(10):788–792. [DOI] [PubMed] [Google Scholar]
- 12.Gardner MJ., Graves ML., Higgins TF., et al. Technical Considerations in the Treatment of Syndesmotic Injuries Associated With Ankle Fractures 2015;23(8):510–518. [DOI] [PubMed] [Google Scholar]
- 13.Phisitkul P, Ebinger T, Goetz J, et al. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg Am 2012;94(24):2256–61. Doi: 10.2106/JBJS.K.01726. [DOI] [PubMed] [Google Scholar]
- 14.Cherney SM., Haynes JA., Spraggs-Hughes AG., et al. In Vivo Syndesmotic Overcompression After Fixation of Ankle Fractures With a Syndesmotic Injury. J Orthop Trauma 2015;29(9):414–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Summers HD., Sinclair MK., Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma 2013;27(4):196–200. [DOI] [PubMed] [Google Scholar]
- 16.Grenier S, Benoit B, Rouleau D, et al. APTF- anteroposterior tibiofibular ratio, a new reliable measure to assess syndesmotic reduction..pdf. J Orthop Trauma 2013;27(4):207–11. [DOI] [PubMed] [Google Scholar]
- 17.Miller AN., Barei DP., Iaquinto JM., et al. Iatrogenic syndesmosis malreduction via clamp and screw placement. J Orthop Trauma 2013;27(2):100–6. Doi: 10.1097/BOT.0b013e31825197cb. [DOI] [PubMed] [Google Scholar]
- 18.Nault M, Hebert-Davies J, Laflamme G, et al. CT scan assessment of the syndesmosis- a new reproducible method.pdf. J Orthop Trauma 2013;27(11):638–41. [DOI] [PubMed] [Google Scholar]
- 19.Dikos GD., Heisler J., Choplin RH., et al. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma 2012;26(7):433–438. [DOI] [PubMed] [Google Scholar]
- 20.Davidovitch RI., Weil Y., Karia R., et al. Intraoperative Syndesmotic Reduction: Three-Dimensional Versus Standard Fluoroscopic Imaging. J Bone Jt Surg 2013;95(20):1838–43. Doi: 10.2106/JBJS.L.00382. [DOI] [PubMed] [Google Scholar]
- 21.Schreiber JJ., McLawhorn AS., Dy CJ., et al. Intraoperative Contralateral View for Assessing Accurate Syndesmosis Reduction. Orthopedics 2013;36(5):360–1. Doi: 10.3928/01477447-20130426-03. [DOI] [PubMed] [Google Scholar]
- 22.Loizou CL., Sudlow A., Collins R., et al. Radiological assessment of ankle syndesmotic reduction. The Foot 2017;32:39–43. Doi: 10.1016/j.foot.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Reb CW., Hyer CF., Collins CL., et al. Clinical Adaptation of the “Tibiofibular Line” for Intraoperative Evaluation of Open Syndesmosis Reduction Accuracy: A Cadaveric Study. Foot Ankle Int 2016;37(11):1243–1248. [DOI] [PubMed] [Google Scholar]
- 24.Miller AN., Carroll EA., Parker RJ., et al. Direct Visualization for Syndesmotic Stabilization of Ankle Fractures. Foot Ankle Int 2009;30(05):419–26. Doi: 10.3113/FAI.2009.0419. [DOI] [PubMed] [Google Scholar]
- 25.Naqvi GA., Cunningham P., Lynch B., et al. Fixation of Ankle Syndesmotic Injuries: Comparison of TightRope Fixation and Syndesmotic Screw Fixation for Accuracy of Syndesmotic Reduction. Am J Sports Med 2012;40(12):2828–35. Doi: 10.1177/0363546512461480. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mean difference between reductions using direct visualization and baseline measurements showed no significant differences in any measurement.
Mean difference between reductions using palpation and baseline measurements showed no significant differences in any measurement.