Introduction
Lipedematous alopecia (LA) and lipedematous scalp (LS) are 2 rare conditions of unknown etiology that are thought by some to be 2 stages on a spectrum of a single scalp disorder.1 LA was first described by Coskey et al2 in 1961, and in 2007, the term spongy scalp was used to describe LA and LS.3 Both LA and LS conditions are characterized by a localized or diffusely thickened, boggy scalp, but LS lacks alopecia. Associated pruritus and soreness can occur with LA, but most LS patients are asymptomatic.4 Both conditions are characterized pathologically by a measurable hyperplasia of the subcutaneous tissue.5
Case report
A 46 year-old African-American woman presented to the urgent care center for evaluation of her scalp on multiple occasions. For at least 6 months, she complained of mild scalp tenderness and pruritus and noticed substantial decreased hair growth and hair loss. She had applied ketoconazole shampoo to her scalp, which did not improve her symptoms. The patient denied any history of trauma, surgery, or medication use, and she did not have a family history of hair loss.
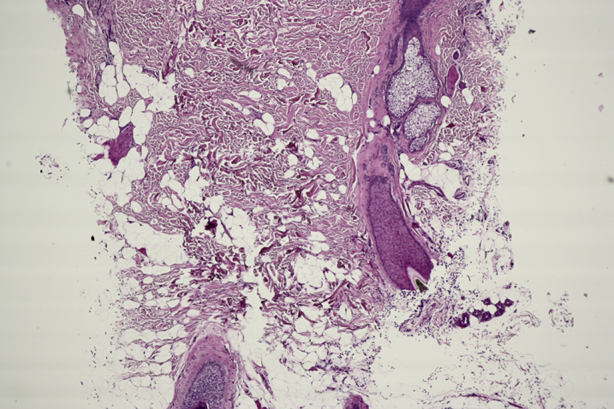
On physical examination, the patient had a 1- to 2-cm scalp hair length with evidence of predominantly nonscarring alopecia diffusely over the scalp. Palpation of the scalp found marked bogginess and thickening (Fig 1) that instantly returned to normal after releasing pressure. No rash, scale, or evidence of trauma was noted on the head. Computed tomography scan found increased subcutaneous tissue of the scalp measuring 14 mm in thickness, more prominent at the vertex of the scalp. There was no trauma to the skull or cerebrospinal fluid leak. Hematoxylin-eosin stain of the scalp found decreased hair follicle density and a pauci-inflammatory process with thickening of collagen bundles and increased space between bundles suggestive of edema (Fig 2). No scar or mucin was present, and 1 anagen follicle was noted (Fig 3).
Fig 1.

Clinical features of LA. Note the thickening of scalp with alopecia.
Fig 2.

Histopathologic stain with hematoxylin-eosin stain. Note thickening of subcutaneous tissue.
Fig 3.
Close-up image of hair follicle in a patient with LA.
Discussion
Clinical, radiographic, and histologic findings of our patient show features consistent with LA. Lipedematous alopecia is a rare, nonscarring alopecia characterized by “an increase in thickness of the subcutaneous layer of the scalp and inability to grow hairs longer than 2 cm.”2 A review by González-Guerra et al6 in 2008 found that only 17 cases of LA have been reported worldwide. In a review of 47 cases published in 2012 of LA and LS, it was found that 90% of patients were women, and the mean age of onset was 42 years; 39% of patients were white, 32% were black, 24% were Egyptian, and 5% were Asian.5
Currently, there is not a reliable link of LA with other symptoms or with genetic mutations.5 Moreover, the pathogenesis of LA and LS remains a mystery. Leptin, a hormone regulating distribution of adipose tissue, has been postulated as playing a role in causing hyperplasia of subcutaneous fat.5, 7 Another theory of LA pathogenesis involves metaplasia and displacement of adipose tissue. Because women comprise most patients with LA, hormones may also play a role, although evidence is lacking as to why this phenomenon is observed.5 Martín et al1 noted that lymphatic dilation may be the mechanism of hair loss in lipedematous alopecia.
Diagnosis of LA involves assessing the clinical presentation and excluding conditions such as cutis verticis gyrata (CVG). CVG is a condition also characterized by increased scalp thickness but has a characteristic furrowing of the affected area that resembles the gyri of the brain, distinguishing it from LA. Moreover, CVG occurs more commonly in men, and magnetic resonance imaging will show an increase in the dermis with only a minimal expansion of the subcutaneous tissue.
Histomorphologic criteria of LA and LS include a thickened layer of subcutaneous fat with variable disruption of fatty architecture, no visible panniculitis or lipoma, the absence of inflammation, and normal hair follicles and adnexae.5 Diagnostic modalities include computed tomography scan, magnetic resonance imaging, and histopathology. Normal mean thickness of the scalp is between 5 and 8 mm, and pathologic scalp thickness in LA/LS is between 9 and 19 mm.5 Our patient's scalp thickness was 14 mm. Histology usually finds a normal epidermis and dermis as well as a hyperplasia of the subcutaneous adipose tissue.
Currently, no guidelines exist for the treatment of LA and LS. Intralesional and topical steroids documented in the literature have been tried with no improvement.4, 8 Our patient received a trial of intralesional triamcinolone injection. Follow-up for our patient showed no clinical signs of improvement, and the patient did not desire additional treatment. There have been cases of successful treatment of LA. Cabrera et al8 reported in 2015 treating a patient with 10 months of oral mycophenolate mofetil, 1 g/d. After this treatment period, the patient had complete recovery of hair sustained even after 6 months of follow-up.8 Yip et al7 noted successful treatment with surgical debulking of the scalp after achieving remission of LA with no recurrence 1 year after surgery. Given the limited cases of successful treatment, further clinical evidence is needed to reach a consensus for treatment of LA.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Martín J.M., Monteagudo C., Montesinos E., Guijarro J., Llombart B., Jordá E. Lipedematous scalp and lipedematous alopecia: a clinical and histologic analysis of 3 cases. J Am Acad Dermatol. 2005;52(1):152–156. doi: 10.1016/j.jaad.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Coskey R.J., Fosnaugh R.P., Fine G. Lipedematous alopecia. Arch Dermatol. 1961;84:619–622. doi: 10.1001/archderm.1961.01580160083014. [DOI] [PubMed] [Google Scholar]
- 3.Scott M.J., Scott M.J. Lipedematous alopecia: spongy scalp syndrome. Cutis. 2007;80(4):321–324. [PubMed] [Google Scholar]
- 4.Kavak A., Yuceer D., Yildirim U., Baykal C., Sarisoy H.T. Lipedematous scalp: a rare entity. J Dermatol. 2008;35(2):102–105. doi: 10.1111/j.1346-8138.2008.00423.x. [DOI] [PubMed] [Google Scholar]
- 5.Müller C.S.L., Niclou M., Vogt T., Pföhler C. Lipedematous diseases of the scalp are not separate entities but part of a spectrum of lipomatous lesions. J Dtsch Dermatol Ges. 2012;10(7):501–507. doi: 10.1111/j.1610-0387.2011.07830.x. [DOI] [PubMed] [Google Scholar]
- 6.González-Guerra E., Haro R., Angulo J., Del Carmen Fariña M., Martín L., Requena L. Lipedematous alopecia: an uncommon clinicopathologic variant of nonscarring but permanent alopecia. Int J Dermatol. 2008;47(6):605–609. doi: 10.1111/j.1365-4632.2008.03405.x. [DOI] [PubMed] [Google Scholar]
- 7.Yip L., Mason G., Pohl M., Sinclair R. Successful surgical management of lipoedematous alopecia. Australas J Dermatol. 2008;49(1):52–54. doi: 10.1111/j.1440-0960.2007.00427.x. [DOI] [PubMed] [Google Scholar]
- 8.Cabrera R., Larrondo J., Whittle C., Castro A., Gosch M. Successful treatment of lipedematous alopecia using mycophenolate mofetil. Acta Derm Venereol. 2015;95(8):1011–1012. doi: 10.2340/00015555-2114. [DOI] [PubMed] [Google Scholar]


