Abstract
The statewide Colorado Healthy Heart Solutions (CHHS) program provides cardiovascular disease (CVD) risk factor screening and education to the medically underserved and has been shown to improve CVD risk profiles. We aimed to enhance its effectiveness through addition of a mobile health (mHealth) intervention using SMS messaging (termed Cardio SMS). We conducted a prospective, non-randomized controlled pilot trial of this intervention implemented at 5 rural program sites (number of participants N = 204) compared with a contemporaneous propensity-score matched control group from 14 CHHS sites not receiving the intervention (N = 408) between 2012 and 2014. All participants were free of CVD at baseline, and follow-up time was 12-months. The primary outcome was program engagement, defined as the number of completed interactions with the program during the entire follow-up period. Secondary outcomes were program retention, defined as any interaction during the last two months of the study; change in self-reported healthy behaviors (physical activity, weight loss, smoking cessation, fat intake); and change in CVD risk factors. There were trends for differences between groups across multiple outcomes, but most did not reach statistical significance, except for a greater decrease in self-reported fat intake in the intervention vs. control groups (26.3% vs 10.6%, P = 0.001). In addition, a subset of surveyed participants who viewed the SMS messages as motivating showed greater program retention (P = 0.03). Given the relative ease and scalability of SMS interventions in rural underserved communities, further study of SMS as part of multicomponent strategies for CVD prevention is warranted.
Keywords: Mobile health, Cardiovascular disease, Primary prevention
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States, with a large proportion of morbidity and mortality attributable to modifiable risk factors. In this regard, the American Heart Association recently published a guideline dedicated to lifestyle management as a critical approach to decreasing CVD risk (Eckel et al., 2014). Effective primary and secondary prevention interventions generally target both lifestyle modification (tobacco use, physical inactivity, poor diet, overweight and obesity) and emphasize adherence to medical treatment of risk factors (dyslipidemia, hypertension and diabetes) to lower the rate of CVD (Krantz et al., 2013; Pearson et al., 2013).
Although Colorado has one of the lowest CVD mortality rates in the United States, rural communities have higher rates of CVD mortality compared to urban areas Colorado Department of Public Health and Environment, 2012. Those living in rural, medically underserved areas also have a higher rate of uncontrolled CVD risk factors (Pearson et al., 2013). To address these health gaps, we implemented the Colorado Healthy Heart Solutions (CHHS) statewide prevention program aimed at providing barrier-free CVD risk factor screenings and education, with strong outreach to the medically underserved (Krantz et al., 2013). Although CHHS demonstrated reduction in CVD risk factors among those participants who underwent retesting, it was characterized by low program retention, with <15% of screened patients undergoing a retest visit.
The use of mobile health (mHealth) interventions for CVD prevention has increased significantly in recent years (Burke et al., 2015; Eapen et al., 2016). Although a growing body of evidence supports the use of mobile phone short message service (SMS) for augmenting physical activity, nutrition, and smoking cessation, previous studies were limited by a focus on middle to upper income populations, and have not targeted predominantly rural communities outside the healthcare delivery system (Vodopivec-Jamsek et al., 2012; de Jongh et al., 2012; Head et al., 2013). Given this background, we hypothesized that a simple, scalable mHealth intervention using SMS text messaging to rural residents (Cardio SMS) could improve healthy behaviors and CVD risk factors by enhanced engagement and program retention. While few mobile-technology based interventions for disease management have articulated a theoretical basis (Riley et al., 2011), this intervention draws explicitly on insights from Social Cognitive Theory (Bandura, 2001), which holds that individuals' health behaviors are motivated by enhancing self-efficacy (Bandura, 1977), and that such self-efficacy is encouraged by social support (Cobb, 1976; Cohen and Wills, 1985; Franklin et al., 2006). The current program provides direct social support via community health worker interaction and this may be enhanced through simultaneous social media/mobile health messaging.
The main objectives of this pilot study were to explore the effects of Cardio SMS on program engagement and several other related outcomes; to provide estimates of the intervention's effect sizes for these outcomes; and to inform future refinement of this intervention, aimed at increasing its impact.
2. Methods
The CHHS program utilizes a Community Health Worker (CHW) chronic disease prevention model focused on CVD prevention. The present pilot study took advantage of the infrastructure of the CHHS program, which already collects outcome data and encourages participants to interact with the CHWs to create health action plans then return 6–12 months after the initial screening visit for retesting. A non-randomized controlled design was utilized to estimate the effectiveness of integrating an SMS intervention into the existing program. Participant data and CHW interactions were managed at the site level using a point-of-service decision support system which synchronizes automatically and in real time to a secure, HIPAA compliant server [Outreach Screening and Referral (OSCAR) software system (CPC Clinical Research, Aurora CO)]. The study was approved by the Colorado Multiple Institutional Review Board (COMIRB).
2.1. Cardio SMS messages
A detailed description of the development and content of SMS messages for this program has been previously published (Albright et al., 2015). Briefly, text messages were managed through a Patient Relationship Management (PRM), system. This software platform was created in partnership between Denver Health Medical Center (Denver, CO), EMC Consulting (Hopkinton, MA), and Microsoft Corporation (Redmond, WA). The PRM system was designed to automatically send unidirectional text messages to participants according to an established schedule. This technology has been piloted previously at Denver Health to evaluate the feasibility of engaging adults with diabetes in self-management behaviors between clinic visits (Fischer et al., 2012). Prior to the intervention, we conducted 2 focus groups at 2 time points with English- and Spanish-speaking participants living in rural areas of southeastern and western Colorado to evaluate sample SMS messages and inform the frequency and the timing of the messages. Messages were sent in either English or Spanish, depending on participant preference. After testing the program over a 6-week period, 3 additional focus groups and 3 in-depth interviews were conducted with CHHS participants. Results of these focus groups and interviews, as well as a detailed description of the SMS messages, have been previously described (Albright et al., 2015). Messages were designed to be practical and specific, were delivered once a day, and included advice on tactics for improving healthy eating, physical activity, and weight loss, and encouragement to contact their local CHW. Examples of SMS messages (English language version) are provided in Table 1.
Table 1.
Examples of SMS messages (modified from reference (Albright et al., 2015)).
| Goal | SMS text examples |
|---|---|
| Healthy eating |
|
| Physical activity |
|
| CHW Engagement |
|
2.2. Participant recruitment and conduct of study
A quasi-experimental design was utilized to estimate the effectiveness of the Cardio SMS intervention among five CHHS sites by enrolling consecutive participants from each site, with a target of 200 participants in the intervention group. Subjects were enrolled during screening events or from previously empaneled participants. Participants enrolled in the Cardio SMS intervention were compared with participants enrolled in 14 other CHHS sites not participating in the intervention (i.e. participants not receiving any CHHS-related SMS communication). There were no significant differences between the intervention and control sites in participant demographics, proportion without health insurance, and rural vs. urban county status. Inclusion criteria for both intervention and control groups were: >18 years of age or older, a mobile phone with SMS capabilities, Framingham Risk Score (FRS) > 10%, blood pressure (BP) ≥ 140/90 mm Hg and/or LDL-cholesterol ≥ 160 mg/dL for subjects with a FRS < 10% or ≥ 130 mg/dL for subjects with a FRS of 10–19%. Exclusion criteria were: pregnant or lactating women, individuals with co-morbid illness with life expectancy < 12 months (e.g., terminal cancer, Child's Class C hepatic cirrhosis), institutionalized individuals, or those not planning to stay in the area at least six months. We also excluded participants with pre-existing coronary artery disease, cerebrovascular disease, and diabetes.
At program entry, CHWs obtained written permission for participation. The CHW then performed health screenings, which included automated BP, weight and height using a stadiometer (to calculate body mass index, BMI). In addition, point-of-service finger-stick serum testing (Cholestech LDX, Inverness Medical, Hayward CA) was performed for all participants. Single cartridges measured serum glucose, total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, and low-density lipoprotein (LDL) cholesterol was calculated via the Friedwald estimation (Friedewald et al., 1972). The CHWs also assessed health care access, health history, dietary intake, physical activity patterns, and knowledge of CVD risk before the initial screening. The OSCAR system also captured participant demographics, health care information, health history, dietary practices, physical activity levels, health goals, participant activation measures, and risk factor values.
Finally, at the end of the 12-month study period, we conducted a mail survey among SMS participants. Response rates were tabulated and the instrument assessed perceived effects of the SMS intervention on lifestyle and health promotive behaviors including healthy eating and active living, self-motivation, and interaction with the CHHS program.
2.3. Outcomes and analyses
The primary outcome was program engagement defined as the number of completed interactions (i.e. interactions involving a response or action on the part of the participant) between the CHW and the participant. Interactions included phone calls, face-to-face visits, and/or email. Secondary outcomes included program retention, defined as the proportion with any of the aforementioned interactions during the last 2 months of the 12-month follow-up period, and changes in healthy behaviors after 12 months of follow-up compared with baseline, including smoking cessation, decreased fat intake, increased fiber intake, and increased physical activity/exercise. Among those participants who underwent a retest visit during the study period, we also assessed changes in weight, BMI, systolic BP, diastolic BP and LDL-cholesterol from baseline.
Additionally, we assessed survey responses from participants receiving the Cardio SMS intervention to determine if perceived SMS message motivation correlated with program engagement (the number of interactions with the program during the entire 12-month follow-up period), program retention (any interaction during the last two months of the 12-month follow-up period) and retesting (of CVD risk factors).
2.4. Statistical methods and power
The control group was selected by propensity score matching from participants at CHHS sites not receiving the SMS intervention, with 2:1 frequency matching on quintile of propensity and calendar quarter of enrollment in CHHS, derived from the OSCAR data repository. The propensity model included age, race, ethnicity, body mass index (BMI), systolic blood pressure (BP), and survey-based measures of access to health care, dietary and exercise habits, knowledge of risk, and readiness to change. With N = 204 participants in the SMS intervention group and N = 408 participants in the control group, we had 80% power to detect a difference of 12.5% or more in the primary outcome, with alpha = 0.05.
Differences in categorical variables between groups were assessed using the chi-squared test, Fisher's exact test, or Cochran-Mantel-Haenszel test, as appropriate. Differences in continuous variables were assessed using the Wilcoxon-Mann-Whitney test, since values were not normally distributed. In additional analyses for the primary outcome, a multivariable generalized linear mixed model (SAS PROC GLIMMIX) was performed using baseline demographic variables (age, gender) as independent variables, as well as and a random generated variable for project site, to account for the clustering of participants within project site. Candidate variables for inclusion into this model were gender, age, race, ethnicity, marital status, education and employment status. Variables with the highest p values were removed one at a time from the resulting model. A p value of <0.05 was considered significant. All analyses were performed using SAS 9.3 (SAS Inc., Cary, NC).
3. Results
A total of 204 participants received the Cardio SMS intervention across 5 CHHS sites in rural Colorado during the study period (October 1, 2012 to February 25, 2014). A total of 408 participants derived from 3400 contemporaneous participants at 14 other CHHS sites were used as comparators.
Baseline sociodemographic, and CVD risk characteristics of participants enrolled in the SMS intervention and the matched controls are shown in Table 2. A numerically higher proportion of participants self-identified as Hispanic in the SMS intervention vs. control groups (37.8% vs 30.4%, P = 0.07). The control group had lower BMI, diastolic BP and LDL cholesterol when compared to the intervention group.
Table 2.
Baseline participant characteristics. The study enrolled participants from Colorado rural counties between October 2012 and February 2014. Data are presented as percent or median.
| Control group (n = 408) % or median | SMS Intervention group (n = 204) % or median | p value | |
|---|---|---|---|
| Age, years (median) | 49.3 | 50.1 | 0.63† |
| Male gender (%) | 37.5 | 42.2 | 0.27§ |
| Marital Status (%) | 0.29§ | ||
| Single/Divorced/Separated/Widowed | 36.3 | 40.7 | |
| Married/Partnered | 63.7 | 59.3 | |
| Education (%) | 0.78§ | ||
| Unknown/Less than HS graduate | 20.6 | 20.1 | |
| High school graduate† | 27.0 | 30.9 | |
| Some college | 29.9 | 27.5 | |
| Bachelor's degree or higher | 22.6 | 21.6 | |
| Employment (%) | 0.75§ | ||
| Self/Home/Student | 19.1 | 18.1 | |
| Unknown/Unemployed | 9.6 | 12.3 | |
| Retired/Unable to work | 14.5 | 15.2 | |
| Employed | 56.9 | 54.4 | |
| Race (%) | |||
| White | 92.2 | 93.6 | |
| Non-white | 7.8 | 6.4 | 0.51§ |
| Hispanic | 30.4 | 37.8 | 0.07§ |
| CVD risk factors (medians) | |||
| Body Mass Index, kg/m2 | 27.3 | 28.4 | 0.04† |
| Systolic blood pressure, mm Hg | 124 | 124 | 0.70† |
| Diastolic blood pressure, mm Hg | 80 | 82 | 0.01† |
| LDL cholesterol, mg/dL | 107 | 125 | <0.0001† |
| Framingham risk score, % | 3.8 | 4.3 | 0.17† |
HS = high school; LDL = low density lipoprotein.
Wilcoxon-Mann-Whitney test.
Chi-squared test.
Program interactions during the study period and health promotive outcomes are shown in Table 3. There were no differences in the pre-specified primary outcome of program engagement, defined as the number of completed interactions with the CHW after baseline during the 12-month follow-up period. The proportion of participants with completed interactions (Any follow-up interaction in Table 3) was numerically higher in the SMS intervention group compared with the control group, but the effect size was small (Cohen's d = 0.08). Program retention, defined as any interaction in the last two months of the study period, was low and did not differ between SMS intervention and control groups. Among those who underwent retesting, there were no differences between the SMS and control groups in changes from baseline in BMI or weight, systolic and diastolic BP, and Framingham risk score. There was a statistically significant difference in the proportion of participants who reported a decrease in fat intake in the SMS intervention group compared with the control group (26.3% vs. 10.6%, P < 0.001), but no differences between the 2 groups in other measures of healthy behaviors. Multivariate analyses assessing whether participants had any program follow-up within 12 months from enrollment (primary outcome) including gender, age, and site as a random effect revealed a numerically higher, but not statistically significant impact of the SMS intervention [odds ratio (OR) = 1.23, 95% confidence interval (CI) 0.35–4.32]. Men were more likely than women to have had any follow-up interaction (OR = 1.50, 95% CI 1.02–2.19]. In addition, for each 5-year increment of increasing age, the odds ratio (95% CI) of having any follow-up was 1.13 (1.05–1.21).
Table 3.
Study Outcomes. Data are presented as number, percent or median.
| Outcome variables | Comparison population % or median | SMS Intervention population % or median | p value |
|---|---|---|---|
| Total N | 408 | 204 | |
| Program engagement (total number of interactions in 12 month follow-up period), % | |||
| 0 | 44.9 | 41.2 | |
| 1 | 16.7 | 26.0 | 0.80† |
| 2 or more | 38.5 | 32.8 | |
| Any follow-up interaction, % | 55.2 | 58.8 | 0.39† |
| Total number of retests in 12 month follow-up period | |||
| 0 | 69.9 | 72.1 | |
| 1 | 24.5 | 24.0 | |
| 2 or more | 5.6 | 3.9 | 0.42† |
| Any retest in 12 month follow-up period, % | 30.1 | 27.9 | 0.57† |
| Program retention (total number of interactions in last 2 months of follow-up period), % | |||
| 0 | 88.0 | 92.2 | |
| 1 | 7.1 | 5.4 | 0.09† |
| 2 or more | 4.9 | 2.5 | |
| Any interactions in last 2 months of intervention period, % | 12.0 | 7.8 | 0.11† |
| Any retests in last 2 months of intervention period, % | 3.2 | 3.9 | 0.64† |
| N with follow-up/retesting | 123 | 57 | |
| Stopped smoking, % | 2.4 | 1.8 | 0.99∥ |
| Fat intake decreased, % | 10.6 | 26.3 | 0.001† |
| Fiber intake increased, % | 8.9 | 12.3 | 0.49† |
| Readiness to change increased, % | 35.0 | 33.3 | 0.83† |
| Exercise increased, % | 21.1 | 24.6 | 0.61† |
| Change in Body Mass Index (kg/m2), median | −0.29 | −0.34 | 0.92§ |
| Change in weight (kg), median | −1.0 | −2.5 | 0.97§ |
| Change in systolic blood pressure (mm Hg), median | −1.5 | −2.0 | 0.62§ |
| Change in Diastolic Blood Pressure (mm Hg), median | −2.0 | −0.5 | 0.13§ |
| Median change in LDL-cholesterol (mg/dL), median | −2.5 | −1.5 | 0.33§ |
| Change in Framingham risk score (%), median | 0.01 | −0.08 | 0.94§ |
Cochran-Mantel-Haenszel test.
Wilcoxon-Mann-Whitney test.
Fisher's exact test.
A total of 91 participants in the SMS intervention group returned a study-end survey assessing the perceived impact of the intervention (46%). Fig. 1 shows the impact of answering “Yes” to both survey questions “Do you think CHHS text messages are motivating for you all the time?” and “Do you think CHHS text messages help you with healthy eating and active living all the time?” Those who answered yes to both questions (N = 16) had a trend for higher program engagement (P = 0.07), significantly higher retest rate (P < 0.001), and greater overall program retention (P = 0.03) compared with the rest of the SMS intervention group.
Fig. 1.
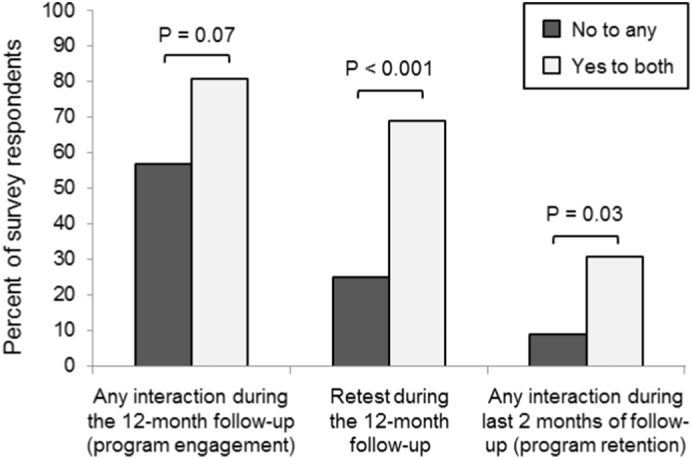
Program engagement, retention and retesting among intervention group participants who responded to the survey (N = 91, 46% of the participants in the intervention group). Higher proportions of participants who answered “Yes” to both of the questions “Do you think CHHS text messages are motivating for you all the time?” and “Do you think CHHS text messages help you with healthy eating and active living all the time?” remained engaged with the program (P = 0.07), underwent retesting (P < 0.001) and were retained in the program (P = 0.03).
4. Discussion
The present pilot study explored the effects of an mHealth intervention using SMS messages integrated into a community CVD risk reduction program involving community health workers. Although improvements in most outcomes were not statistically significant, a reduction in self-reported fat intake and greater retention among surveyed participants who viewed the SMS messages as motivating was demonstrated. Results of this study can be used to estimate effect sizes for each of the outcomes assessed, and inform the design and sample size for a larger, more definitive study of an optimized SMS intervention aimed at CVD prevention in the medically underserved. For instance, based on the effect size for the primary outcome observed in this pilot study, a larger trial using the same design would require approximately 2150 participants in each group (SMS intervention and control) to achieve 80% power to detect a significant difference in the primary outcome, with alpha = 0.05.
Of note, perceived message motivation was associated with a trend for increased engagement and significantly higher rates of retesting and overall program retention among the subset of Cardio SMS participants who completed the final study survey. This suggests that the SMS intervention could be associated with greater benefit in defined subgroups of program participants. While not definitive, these findings are compatible with other studies utilizing SMS to augment community-based programs. For example, a community-based youth development and sexual health program augmented with text messages showed effects on teen pregnancy only among a subset of participants rather than the population as a whole (Bull et al., 2016). However, it is also possible that our subset analysis may have been confounded by selection bias (with those individuals who had an overall positive experience with the intervention potentially more likely to respond to the study-end survey).
The present study is unique, as it included delivery of the SMS intervention in a predominantly rural community setting, including medically underserved individuals. While a number of studies have demonstrated improvements in CVD risk factor within the confines a healthcare delivery system (Fischer et al., 2016), much less has been published in community settings, particularly in rural areas. Another key strength of the present study is that the Cardio SMS intervention was integrated into one of the first community-based programs to demonstrate that a CHW-based initiative can reduce 10-year CVD risk (Albright et al., 2015). Our previous findings suggested that increased interactions with CHWs resulted in improvement in the Framingham Risk Scores (FRS) of program participants. Furthermore, previous results using multiple linear regression showed that participants who had a follow-up interaction with a CHW had lower 10-year CVD risk at retest than those who did not have such an interaction (P = 0.04), suggesting potential for the current Cardio SMS intervention to enhance program effectiveness (Albright et al., 2015). Although the CHHS program demonstrated reductions in CVD risk factors, only a minority of screened patients remained engaged in the program, and <15% underwent retesting. This represented the primary impetus for the current Cardio SMS intervention as a simple, straightforward program enhancement to improved participant engagement and retention.
This pilot study has a number of inherent limitations, including the small sample size, non-randomized design, overall low retest rate, and potential residual confounding not controlled by propensity matching. In addition, the control group had lower baseline BMI, diastolic BP and LDL cholesterol when compared to the intervention group. We also cannot exclude the potential contribution of social desirability bias to some of our results, including the greater decrease in self-reported fat intake in the intervention group. Finally, our Cardio SMS program had only outgoing messages, and by not being able to track participant responses to messages, we could not analyze whether specific messages resonated more or less for participants.
The use of mobile phone SMS messaging for disease prevention and management interventions has increased significantly in recent years (Vodopivec-Jamsek et al., 2012; de Jongh et al., 2012; Wei et al., 2011). A number of mHealth strategies, including mobile applications and SMS text messaging, offer the potential to shift the emphasis of primary prevention outside the walls of medical institutions and improve individualized care through positive behavior change theory (Pagoto and Bennett, 2013). By creating text messages based upon focus group feedback within predominantly rural sites, we sought to provide additional motivation for health promotive behaviors. We chose to limit our intervention to SMS messaging instead of other mobile approaches that would utilize cellular data since most cell phone plans provide unlimited SMS messaging, and SMS messaging remains the most inexpensive means of mobile communication even for those plans that do not provide unlimited SMS. Additionally, SMS messages are asynchronous and can be accessed at a time convenient for the participant. Moreover, text messages can be tailored to the individual, which is important because tailored messages have been demonstrated to be more effective for health behavior change compared to generic ones (Ryan and Lauver, 2002). In the future, a modified intervention including delivery of personalized, bi-directional messages may increase effects sizes compared to those observed in the present study.
In summary, this pilot study explored the effects of a novel mHealth intervention for CVD prevention using SMS messages delivered among medically underserved, rural communities. Given the relative ease and scalability of such interventions, further efforts directed at intervention optimization and assessment in larger studies are warranted.
Acknowledgments
Acknowledgments
This work was supported by the Agency for Healthcare Research and Quality (AHRQ). The CHHS program is supported by the Cancer, Cardiovascular and Pulmonary Disease grants program of the Colorado Department of Public Health and Environment. M. Odette Gore is supported by a career development grant (K23-HL131939) from the National Heart, Lung, and Blood Institute (NHLBI), and by a University of Colorado School of Medicine Fund to Retain Clinical Scientists (FRCS) research award from the Doris Duke Charitable Foundation.
Conflict of interest
The authors have no conflicts of interest to report.
References
- Albright K. Health promotion text messaging preferences and acceptability among the medically underserved. Health Promot. Pract. 2015;16(4):523–532. doi: 10.1177/1524839914566850. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Bull S. Text messaging, teen outreach program, and sexual health behavior: a cluster randomized trial. Am. J. Public Health. 2016;106(S1):S117–S124. doi: 10.2105/AJPH.2016.303363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E. Current science on consumer use of Mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132(12):1157–1213. doi: 10.1161/CIR.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosom. Med. 1976;38(5):300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- de Jongh T. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst. Rev. 2012;12 doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eapen Z.J. Defining a mobile health roadmap for cardiovascular health and disease. J. Am. Heart Assoc. 2016;5(7) doi: 10.1161/JAHA.115.003119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckel R.H. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S76–S99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- Fischer H.H. Care by cell phone: text messaging for chronic disease management. Am. J. Manag. Care. 2012;18(2):e42–e47. [PubMed] [Google Scholar]
- Fischer H.H. Text message support for weight loss in patients with prediabetes: a randomized clinical trial. Diabetes Care. 2016;39(8):1364–1370. doi: 10.2337/dc15-2137. [DOI] [PubMed] [Google Scholar]
- Franklin V.L. A randomized controlled trial of sweet talk, a text-messaging system to support young people with diabetes. Diabet. Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- Friedewald W.T., Levy R.I., Fredrickson D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- Head K.J. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc. Sci. Med. 2013;97:41–48. doi: 10.1016/j.socscimed.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Krantz M.J. Effectiveness of a community health worker cardiovascular risk reduction program in public health and health care settings. Am. J. Public Health. 2013;103(1):e19–e27. doi: 10.2105/AJPH.2012.301068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagoto S., Bennett G.G. How behavioral science can advance digital health. Transl. Behav. Med. 2013;3(3):271–276. doi: 10.1007/s13142-013-0234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson T.A. American Heart Association guide for improving cardiovascular health at the community level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127(16):1730–1753. doi: 10.1161/CIR.0b013e31828f8a94. [DOI] [PubMed] [Google Scholar]
- Riley W.T. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl. Behav. Med. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P., Lauver D.R. The efficacy of tailored interventions. J. Nurs. Scholarsh. 2002;34(4):331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- Vodopivec-Jamsek V. Mobile phone messaging for preventive health care. Cochrane Database Syst. Rev. 2012;12 doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J., Hollin I., Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. J. Telemed. Telecare. 2011;17(1):41–48. doi: 10.1258/jtt.2010.100322. [DOI] [PubMed] [Google Scholar]


