Abstract
Purpose
Small apertures are successfully used to extend depth of focus in presbyopic patients implemented either as corneal inlays or intraocular lenses. The use of small apertures reduces retinal illuminance. In this study, we quantify the relative perceived brightness in the 2 eyes of patients implanted monocularly with a small-aperture inlay.
Design
Prospective case series.
Methods
We used a binocular adaptive optics vision simulator to determine the relative perceived brightness. Four patients implanted monocularly with the KAMRA corneal inlay (1.6 mm) and a group of control subjects participated in the study. The projected pupil on the eye implanted with the inlay alternated in diameter between 0 and 2.5 mm (effective 1.6 mm) to eliminate potential for light to project around the periphery of the inlay while the corresponding fellow eye projected pupil alternated between 0 and 3.0 mm or 0 and 4.0 mm at a frequency of 1 Hz. Alternation on both eyes was synchronized so that only 1 eye at a time had a nonblocked pupil. At equal transmittance, a flickering was perceived. Patients' task consisted of modifying the transmittance of the pupil corresponding to the fellow eye until the perceived flickering, owing to the different perceived brightness, was minimized. This equalizing transmittance (ET) value indicates the relative perceived brightness.
Results
In the KAMRA's patients, ET was found to be greater than expected considering the difference in pupil sizes and the Stiles-Crawford effect, showing an enhanced a greater brightness perception in the eye with the small aperture in comparison with the fellow eye. Compared with the control subjects, this difference was on average bigger by a factor of ×1.42.
Conclusions
Patients implanted with the small-aperture corneal inlay exhibited an enhanced brightness perception with the eye implanted, in comparison with their untreated fellow eye. The amount of this increase is much larger than what could be expected owing to the Stiles-Crawford effect and was probably attributable to a neural adaptation process. This phenomenon could explain a reported equalization of brightness between eyes in patients with unilateral inlays and implies that the expected reduction of brightness may have a less significant impact on these patients, as expected.
Presbyopia is a condition characterized by a progressive loss of the ability to focus near objects starting around the age of 40–45 years. A variety of optical-based solutions have been proposed: bifocal and progressive power lenses,1, 2, 3 multifocal phase profile designs implemented on contact lenses and intraocular lenses (IOLs),4, 5 accommodative IOLs,6, 7 and, of special relevance for this work, the use of small apertures8, 9 implemented as corneal inlays or IOLs.
A small-entrance pupil produces an increase in depth of focus (DoF). From a simple geometrical optics point of view, this can be explained by the reduction in size of the defocused blurred spot. The increased DoF allows enlarging the range at which objects can be imaged with a reasonable optical quality, being useful for imaging closer objects.
In the case of the eye, this small-aperture solution has been implemented through either a corneal inlay or an IOL (AcuFocus, Inc, Irvine, California, USA). The corneal inlay is a thin 6-μm ring with an inner aperture of 1.6 mm and outer diameter of 3.8 mm. The ring is not completely opaque (5% transmittance) but is filled with microperforations to facilitate the flow of nutrients and waste products through the cornea. Subjects are implanted monocularly in the nondominant eye, leaving the dominant eye corrected for distance.
Although the effectiveness of the small-aperture solution to increase DoF has been clinically proved,10 some concerns have been raised related to the diminished illuminance onto the retina owing to the reduced aperture. The most obvious is the potential reduction of the perceived brightness that may lead to decreased contrast sensitivity or visual acuity under low-luminance conditions. Furthermore, the interocular difference in brightness was suggested as a factor that may affect the perception of motion.11
However, it is not uncommon that patients implanted with the small aperture, asked about the difference in brightness perceived monocularly with each eye, declare that no or very little difference is perceived. This fact elicited our interest on this subject. As an initial approach to this issue, in a previous work12 we studied if even in normal subjects (not implanted with the inlay) the monocular brightness perception at reduced pupil sizes might be greater than expected, considering both the power entering the eye through the limited pupil area and the Stiles-Crawford (SC) effect,13 which accounts for the efficiency of the retina to capture the incident light at different pupil locations. Using a binocular adaptive optics vision simulator (BAOVS), we obtained results that showed an increase of 1.24× in brightness perception for a 1.6-mm pupil compared with what could be expected. These results encouraged our interest on this subject and we decided to test individuals implanted with the corneal inlay.
The aim of this work is to quantify the relative brightness perception between eyes in subjects implanted monocularly with the small-aperture corneal inlay and compare with the results obtained from normal or control subjects not having the inlay.
Methods
Subjects
This study was approved by the Ethical Committee of the Universidad of Murcia. After being informed of the purpose, all subjects agreed to participate in the present study and signed an informed consent following the tenets of the Declaration of Helsinki. A total of 4 subjects monocularly implanted with the small-aperture corneal inlay participated in the experiment with ages in the range from 55 to 61. Only subjects S#1 and S#4 showed a small degree of ametropia: Subject S#1 was a myopic individual of 2.25 diopter (D) in the treated eye and subject S#4 was myopic (1 D) in both eyes. The rest of the subjects were emmetropic and none of them needed correction for astigmatism. Regarding sex, 3 subjects were female and only subject S#1 was male. All except subject S#3 had the inlay implanted in the right eye. All subjects were employees of Acufocus Inc (Irvine, California, USA) but only 1 of them was aware of the significance of the experiment.
The control group of subjects, or subjects with no inlay implanted, was formed by 3 participants. Two of them were emmetropic and only subject SC#1 showed some degree of myopia (around 3 D in both eyes). At the time of the experiment they were 27, 30, and 45 years old. All of them were male and all had no commercial relationship to disclose. All participants in both groups, implanted with the inlay and control, were healthy volunteers with no history of relevant ocular disease that may affect the outcomes of the experiment. The study followed the guidelines of the Declaration of Helsinki and the subjects were informed in detail about the nature of the experiment and potential risks.
Instrument
The instrument employed to test the interocular difference in brightness perception was a BAOVS, which was described in greater detail in previous publications.14, 15 The instrument is composed of a display system, which binocularly delivers visual stimuli to the subject, and 2 different liquid crystal spatial light modulators (SLM), which allow us to change the phase and the amplitude of the light wavefront at the eye's pupil plane. The ability to modify the phase of the wavefront allows us to correct for the subject's ametropias. However, the most relevant feature of the BAOVS concerning this work is the ability to change the amplitude because it permits to change the effective size and transmittance of the exit pupils of the instrument, creating artificial apertures that effectively limit the light entering the subject's eyes. The liquid crystal modulator (SLM-ampl) providing this capability is a pixelated device (LC2002; Holoeye, Berlin, Germany), with a resolution of 800 × 600 pixels and driven as an external display by a control computer.
The display system employed in this experiment is composed of 2 equal pico-projectors (MPro120; 3M, St Paul, Minnesota, USA), 1 for each eye. In the path between the projectors and the eyes a bandpass filter was placed with central wavelength at 550 nm and spectral width of full width at half maximum = 40 nm. The system provided photopic conditions with a luminance of 232 cd/m2. The use of quasi-monochromatic light was noticed that facilitated the subject's task.
Procedure
To estimate the relative brightness perception between the eye implanted with the inlay and the fellow eye, we designed an experiment based on flicker detection. Artificial apertures produced on each eye by the SLM-ampl alternated between a blocked and an opened aperture, whose size was chosen on convenience. The aperture corresponding to the eye with the implanted inlay was chosen large enough to effectively limit a 1.6-mm pupil. We will refer to this as the smaller pupil. For the fellow eye, we chose a larger aperture that will be referred to as the larger pupil. The blocked-opened aperture alternation on each eye was synchronized between eyes in such a way that only 1 eye at a time had a blocked pupil. Were the brightness perceived by 1 eye greater than the other, it would be perceived as a flickering in brightness on the visual stimulus. Allowing the subject to modify the transmittance of the larger pupil, the point at which flickering perception is minimized signals the brightness equalization between eyes. At this point the ratio between the transmittance (TL) of the larger to the transmittance (TS) of the smaller pupils, or equalizing relative transmittance (ERT), is an estimate of the relative brightness perception between eyes:
| (1) |
By simple geometrical optics, taking into account the pupil areas, the ERT can be calculated as:
| (2) |
where DL and DS are the diameters of the larger and smaller pupils, respectively. Furthermore, considering the SC effect the expected ERT can be calculated using the following expression:
| (3) |
A detailed derivation of equation 3 can be found in elsewhere.13 If the measured ERT were greater than expected, it would mean that the eye with the larger pupil needs more power to match the brightness of the eye with the smaller pupil and it would indicate that the later eye shows a higher brightness perception.
After careful alignment of the subject's pupils with the exit pupils of the instrument, the focus error of the subject was subjectively corrected. The subject was given control of the focus produced by the SLM, which is capable of changing the phase of the wavefront. In steps of 0.25 D, the subject searched for the best focus on each eye as the fellow one was patched. Having similar image quality on both eyes is important to avoid the presence of distracting effects for the posterior flickering minimization task. For the same reason the edges of the circular patch that was used as a visual stimulus were smoothed by a Gaussian filter. The circular patch subtended an angle of 1 degree (maximum field of view allowed by the instrument).
Subjects were tested at 2 different luminance levels: one at the maximum luminance provided by the apparatus (232 cd/m2) and another at one tenth of the latter (23.2 cd/m2) obtained by using a neutral-density filter with OD = 1. Testing at reduced luminance is potentially interesting, as it is under this condition that subjects implanted with the small aperture may have a greater impact on vision.
For the group of subjects implanted with the inlay, the aperture corresponding to the treated eye was made to alternate between 0 mm and 2.5 mm in diameter. Although limited to 1.6 mm by the inlay, the use of a slightly greater aperture avoided vignetting between pupils and ensured that this eye's pupil was always limited solely by the inlay.
For the control subjects, the inlay was simulated simply by setting monocularly an aperture of 1.6 mm. To prevent a bias in the experiment placing the simulated inlay only on 1 particular eye, right or left, it was simulated separately on each of the 2 eyes. Furthermore, the comparison between eyes of the results obtained was expected to provide valuable information.
In both groups of subjects, 2 different sizes, 3 mm and 4 mm, were used in the alternation between the blocked and the opened aperture on the eye with the larger pupil. The alternation rate was fixed at 1 Hz. At the beginning of the session, images of the subject's natural pupils were registered using infrared light under the maximum luminance conditions that would be posteriorly used in the experiment and their diameters were estimated. This was an initial requirement to ensure that the natural pupils of the control subjects and the pupil of the nontreated eye in the subjects implanted with the inlay would always be larger than the maximum aperture size set in the measurements, that is, 4 mm. The pupil size control task was performed by taking images of both pupils using a camera available in the instrument for the alignment and control of the eye's pupils relative to the instrument. Based on a previous calibration, we know the size that each pixel on the image represents on the eye's pupil plane and then we can translate the number of pixels along any diameter of the pupil to actual millimeters. An example of the recorded images is shown in Figure 1 for 1 of the subjects implanted with the corneal inlay.
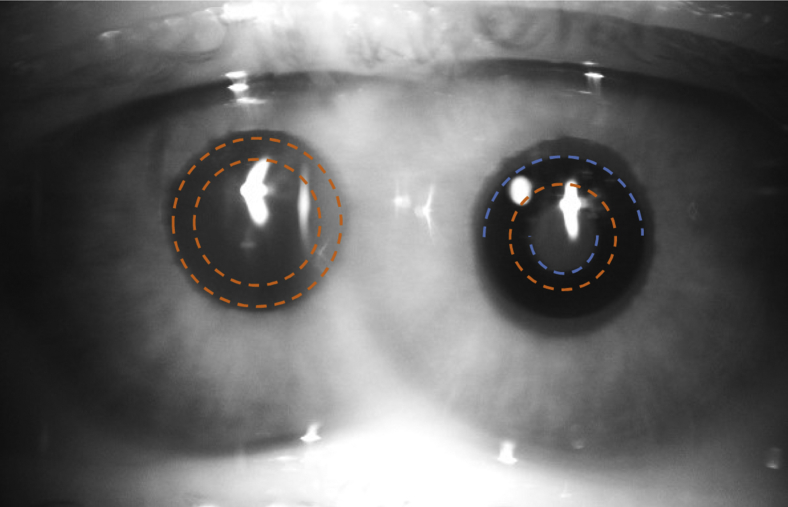
Figure 1.
Image of the pupils of Subject S#2, implanted with the small-aperture corneal inlay. Blue arcs help to visualize its contour. The orange circles show the size of the artificial apertures used: 2.5 mm on the eye with the inlay, 3 mm and 4 mm in the fellow eye. The pupil control system in the binocular adaptive optics vision simulator allows imaging both pupils simultaneously on 1 single image.
The subject's task consisted of searching for the nonflicker condition by modifying the transmittance corresponding to the eye with the larger pupil. The transmittance of the eye with the inlay, or the simulated inlay, in the case of the control subjects, was fixed at 100%. By means of a keypad connected to the SLM-amp via the control computer, the subject changed the transmittance in steps of 1%. A total of 4 different cases (combination of 2 luminance conditions and 2 pupil sizes on the larger pupil) were studied in the group of subjects implanted with the inlay and 8 cases in the control group (simulating the inlay in the right and in the left eye independently). For each case, 6 measurements were collected and averaged—half of them with the transmittance initially set at 100% and the other half set at 0%. In null-type experiments like the one used in this study, starting systematically from 1 end of the interval may produce a bias in the results because the nonflicker condition is met not just at a precise transmittance value but rather into a range of values. In any case, independently of the starting point, the subject was instructed to freely search for the nonflicker condition.
Instrument Validation
To ensure that the apparatus is performing adequately and is not inducing any error in the measurements, a number of tests and adjustments were carried out before subjects were tested.
In the first place, we fixed the apertures for each eye at the same size, and the luminance of each of the 2 pico-projectors delivering light to each eye was adjusted to equalize the luminous power at the eye's pupil plane. In the second place, because our final conclusions will be based on a comparison between experimental data obtained from subjects and theoretically expected values, it is important to objectively ensure that the instrument is in fact providing those expected values. If this were the case, then any potential mismatch between measured and expected values would suggest a physiological origin. To this end, while the size of the aperture for each eye alternated in the same way that it would later do in the experiment with subjects, the total power delivered throughout each pupil was estimated by placing a charge-coupled device camera (XC-75CE; Sony, Tokyo, Japan) at the eye's pupil plane. A previous calibration allowed the conversion from gray levels in the acquired image to luminous power. Assuming that the small-aperture inlay is located on the left eye, a video of this eye's pupil alternating between 0 and 2.5 mm with transmittance equal to 100% was recorded. Afterward the camera was moved to the right eye and videos were taken showing the alternation between the blocked and opened aperture for the 2 tested diameters, 3.0 mm and 4.0 mm, for a range of transmittance values around the expected ERT based on geometrical considerations alone. Calculated through equation 2, these values are 0.284 and 0.160, respectively, which in our case corresponds to transmittances throughout the right pupil of 28.4% and 16.0%.
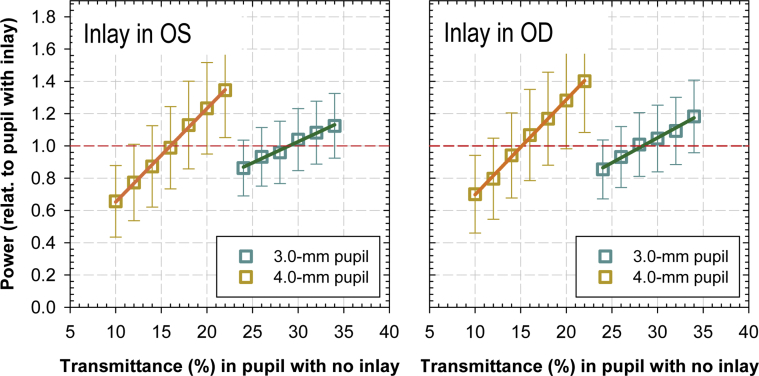
The video frames in which the aperture was opened were processed to estimate the average power over the pupil. For the videos of the smaller pupil only the inner 1.6-mm circular area within the 2.5-mm aperture was used to estimate the power, as this will be the effective pupil size. To check that the apparatus is producing no significant different effects depending on the tested pupil, the same procedure was repeated assuming that the small-aperture inlay is now located on the right eye. The obtained results are graphed in Figure 2. By fitting a linear function to the data, it was possible to estimate the transmittance of the larger pupil needed to equalize the delivered power through both eyes' pupils. This transmittance was 29.0% and 16.0% for the 3.0-mm and 4.0-mm pupils, respectively, in the case where the was is simulated on the left eye and 28.4% and 15.1% when it was simulated on the right eye. For both eyes and pupil sizes, the excellent agreement with the theoretically expected values shows that within the experimental conditions the instrument is not inducing any bias in the experiment.
Figure 2.
Simulating the small-aperture inlay on the left eye (Left) and on the right eye (Right). These graphs show the power through the pupils (3.0 and 4.0 mm) in the fellow eye relative to the power through the eye with the inlay (1.6 mm) as a function of transmittance in the fellow eye. The experimental data are fitted to a linear function (solid lines) and the intersection with relative power equal to 1 (red dashed line) signals the transmittance that equalizes the power through both eyes. Error bars represent ±1 standard deviation of the relative power estimated through frames in the recorded video.
Results
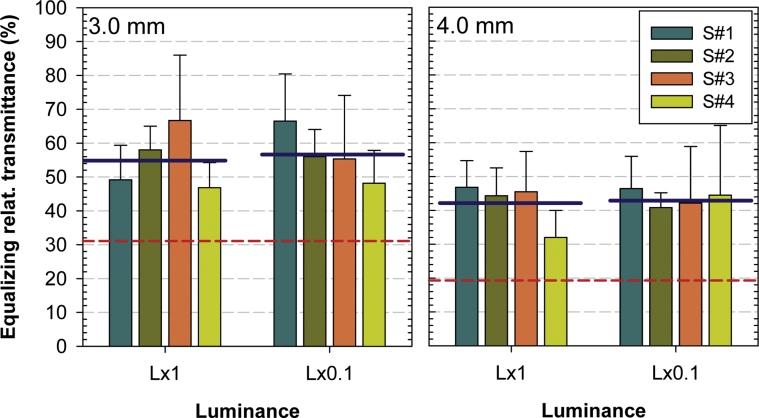
Figure 3 presents the experimental data obtained from the group of subjects implanted with the inlay. The ERT for each subject is represented for the 2 luminance conditions and the 2 studied diameters on the larger pupil, 3.0 and 4.0 mm. All subjects in all cases provided ERT values well above the theoretically expected values of 31.1% and 19.3% corresponding to the 3.0-mm and 4.0-mm pupils, respectively, obtained by making use of equation 3. The averaged value for all subjects of the ERT for the 3.0 mm pupil case were 55.2% ± 9.1% and 56.5% ± 7.6% for the maximum and 10 times lower luminance, respectively. The corresponding values for the 4.0-mm pupil were 42.2% ± 9.0% and 43.5% ± 12.8%. The statistical significance of these differences were assessed through a Student t test, providing P values always below .05.
Figure 3.
Equalizing relative transmittance (ERT) measured on those subjects with the inlay implanted monocularly. The graph shows the data for each subject (S#1-4) for the 2 luminance conditions, maximum (L×1) and 10 times lower (L×0.1), and the 2 studied pupil sizes in the fellow eye, 3.0 mm and 4.0 mm. The red dashed line shows the theoretically expected value and the solid blue line indicates the average through subjects.
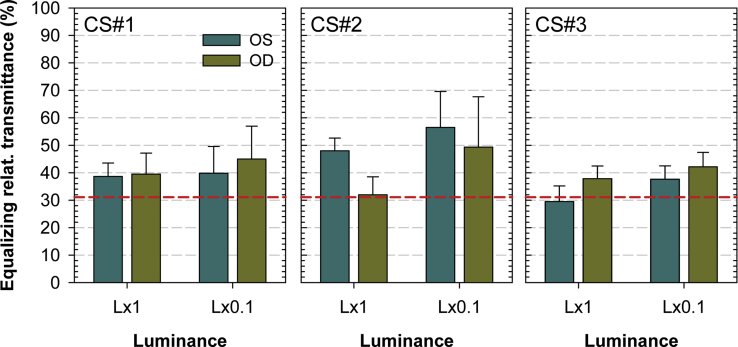
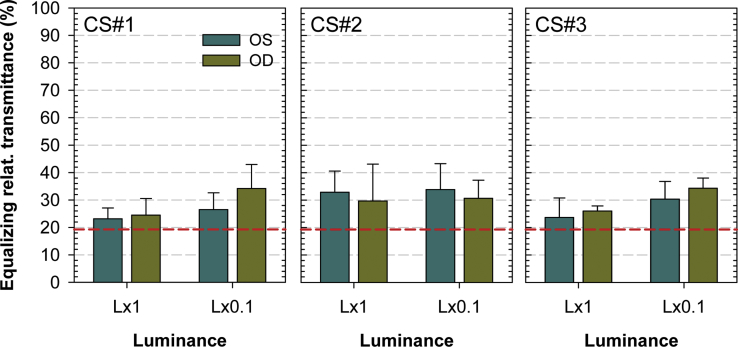
The same experiment testing the control subjects yielded ERT values as shown in Figure 4 (3.0-mm pupil case) and Figure 5 (4.0-mm pupil). For each subject (CS#1-3) the larger pupil was set either on the left (OS in the figure) or on the right (OD) eye and the small aperture was placed on the fellow eye. The performance of both eyes was very similar, the difference being not statistically significant (P > .05) except for 2 cases: Subjects SC#2 and SC#3 at maximum luminance and 3.0-mm pupil.
Figure 4.
Equalizing relative transmittance measured for an alternating 3.0-mm pupil on the control subjects (CS#1-3) for the 2 luminance conditions, maximum (L×1) and 10 times lower (L×0.1). Alternatively, both eyes were simulated with the small-aperture inlay and the alternating aperture of 3.0 mm was tested on the fellow eye (OS, OD). The red dashed line shows the theoretically expected value.
Figure 5.
Equalizing relative transmittance (ERT) measured for an alternating 4.0-mm pupil on the control subjects (CS#1-3) for the 2 luminance conditions, maximum (L×1) and 10 times lower (L×0.1). Alternatively, both eyes were simulated with the small-aperture inlay and the alternating aperture of 4.0 mm was tested on the fellow eye (OS, OD). The red dashed line shows the theoretically expected value.
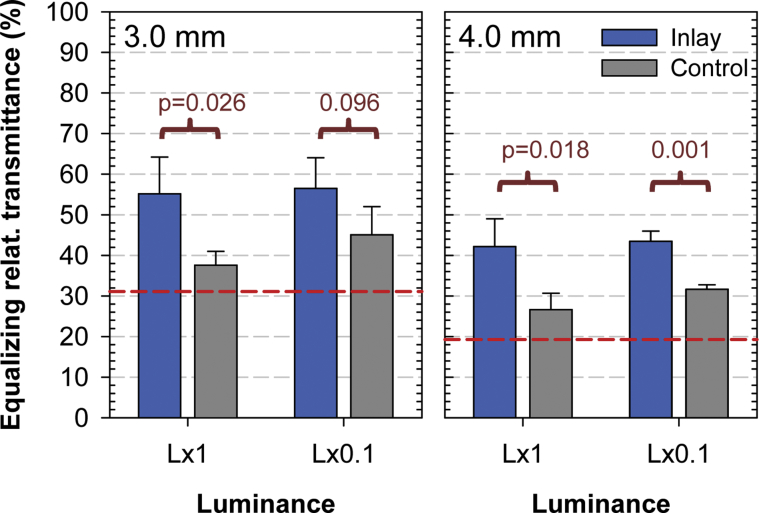
The similar performance between eyes allows us to take the mean as the relevant value in this group of subjects to compare with the results obtained from the subjects implanted with the inlay. This comparison is shown in Figure 6, where the average ERT for all subjects in each group is graphed. In all the studied conditions the mean ERT measured was always bigger for the subjects with the inlay. It was bigger by a factor ranging from ×1.25 in the case of the 3.0-mm pupil and diminished luminance to a maximum ×1.59 factor in the case of maximum luminance and 4.0-mm pupil. The mean factor across the different conditions was ×1.42. The difference was statistically significant (P < .05) for all the experimental conditions except in the case where diminished luminance at 3.0-mm aperture was used (P = .096).
Figure 6.
Average through subjects equalizing relative transmittance measured in the group of subject implanted with the inlay and compared with that of the control subjects. The corresponding P value for each difference is also shown. The comparison was carried out for the tested pupils of 3.0 mm and 4.0 mm and the 2 luminance conditions, maximum (L×1) and 10 times lower (L×0.1). The red dashed line signals the theoretically expected value.
Discussion
In this paper, we have described an experiment aimed at estimating the different brightness perception between eyes in subjects implanted monocularly with a small-aperture corneal inlay. Using a dedicated experimental instrument, we limited the effective pupil size on the nontreated eye and asked for the subject to change the transmittance throughout this pupil to match the luminance perceived by the eye implanted with the inlay. To achieve this, pupils on both eyes were alternating in such a way that only 1 of them was opened at any time, the subject's task consisting of finding the nonflicker condition. In all luminance conditions and pupil sizes tested, subjects provided ERT values clearly above the theoretically expected values considering the pupil areas and the SC effect.
To validate these results, 2 additional tests were carried out: Firstly, we validated the instrument to ensure that, in an objective manner, it was able to accurately provide the expected ERT values, discarding any malfunctioning or lack of precision that may have affected the measurements on subjects. Secondly, to validate the methodology, the measurements performed in the group of subjects implanted with the inlay were repeated in a group of control subjects with no inlay, with a simulated small aperture. The average ERT provided by the subjects in this group was always smaller than that measured in the subjects with the inlay, showing an enhanced brightness perception of the eye with the smaller pupil in the latter group of subjects.
Potential objections might be raised to this comparison between the 2 groups of subjects regarding, for instance, the difference in age or sex. However, the experiment is basically measuring the difference in brightness perception between eyes in the same subject, with both eyes being obviously equally affected by the factors mentioned above. In addition, the similar brightness perception between eyes found in the control subjects shows that a priori significant differences should not be expected and hence the different performance between eyes in the subjects with the inlay is expected to be caused by the small aperture itself and not by intrinsic factors such as a previous interocular brightness perception difference.
Whether the degree of satisfaction of the group of patients implanted with the inlay participating in the study might have affected the results should be also discussed. The 4 patients tested did not report any special dissatisfaction with the inlay. Other patients may report complaints related to the outcome of the surgical procedure, such as inlay decentration or dry eye. We were interested to know the possible adaptation to brightness in the common patient not reporting complaints. But, effectively after measuring 4 subjects, it is not possible to discard the existence of patients not showing this adaptation to the diminished retinal irradiance, and in the future it would be interesting to test some of the patients with continued complaints in situations of low luminance.
According to the specifications of the inlay, the tolerance in size of the inner diameter is 0.1 mm. This means that the largest diameter in the tested patients would be 1.7 mm. Let us ssume that the inner diameter of the inlay on those subjects implanted is 1.7 mm instead of 1.6 mm. In that case, the ERT values should be compared with expected values that take into account the real diameter of the smaller pupil. From equation 2, this new value is 32% instead of 28% for the 3-mm pupil. These values should be compared with the corresponding experimental values, approximately 55% (Figure 3), which are still significantly greater. In consequence, it happens that if the inner dimension of the inlay was greater than 1.6 mm then we would have been overestimating the adaptation effect, but still for a 1.7 mm (the maximum value) this effect is clearly measurable.
There are some perceptual effects that may influence the subjective brightness perception of a flickering visual stimulus. The Brücke-Bartley effect16, 17 describes an enhancement in the brightness perception of a flickering stimulus in comparison with the steady counterpart. In our experiment, because of the alternation between the smaller and the bigger pupils on both eyes, subjects perceive a flickering stimulus in the initial steps of the measurement when the transmittance in the larger pupil is far from the nonflicker condition. At this point it is possible that the Brücke-Bartley effect may influence the subject's brightness perception. However, when subjects complete their task, finding the nonflicker state, this perceptual effect no longer applies. It could be objected that it still applies monocularly on each eye but the parameters that determine the magnitude of the Brücke-Bartley effect, such as luminance and flickering frequency, are the same for both eyes and, in consequence, if there is an effect, it is canceled out and is not affecting perception.
To the best of our knowledge and considering all the above, there are neither instrumental nor visual explanations to the observed discrepancy with the expected values. This leads us to suggest a potential low-luminance adaptation phenomenon in the eye with the small aperture. Indeed, the adaptability of the human visual system to the changing luminous conditions is a well-known phenomenon. Light-adaptation18, 19 is commonly used to refer to the ability of the visual system to adapt to the changing overall illumination conditions. The higher the luminance of a background test stimulus the higher the threshold needed to detect a change in luminance. The mechanism underlying this process acts as an automatic gain, which adjusts the visual sensitivity depending on the luminance of the scene. A related phenomenon, dark adaptation,20, 21, 22 is commonly used to denote the improvement in sensitivity experienced after a reduction in light level, but it also specifically refers to the recovery process of the sensitivity after a high-intensity light exposure that bleaches a big proportion of the photopigments present in the retina. The study of this process has provided important insight into the underlying mechanisms that permit the adaptability of the visual system. These mechanisms23 basically fall into 5 categories that can be summarized into 2: the “photochemical,” which takes into account the density of photopigment; and the “neural,” which encompasses all the processes able to change the efficiency of the visual response at the level of the retina. But high-level neural mechanisms that could involve both eyes have not been described. Indeed, it was known from the nineteenth century that it was possible to bleach the photopigment in 1 eye without affecting the sensitivity in the fellow eye.22 All these findings are compatible with our hypothesis of a monocular low-luminance adaptation in those subjects implanted with the small-aperture corneal inlay.
In summary, we demonstrated that patients implanted with the small-aperture corneal inlay exhibited an enhanced brightness perception in the eye implanted in comparison with their untreated fellow eye. The amount of this increase was much larger than what could be expected owing to the Stiles-Crawford effect and was probably attributable to a neural adaptation process. This phenomenon could explain a reported equalization of brightness between eyes in patients implanted with unilateral inlays.
Acknowledgments
Funding/Support: This study was supported by the following grants: European Research Council Advanced Grant (SEECAT, #ERC-2013-AdG-339228); Secretaría de Estado de Investigación, Desarrollo e Innovación (SEIDI; #FIS2016-76163-R); Fundación Séneca - Agencia de Ciencia y Tecnología de la Región de Murcia (#19897/GERM/15); European Regional Development Fund (#EU-FEDER). Financial Disclosures: Kyle Webb is an employee of Acufocus and Pablo Artal is a consultant to Acufocus. The following author has no financial disclosures: Silvestre Manzanera. All authors attest that they meet the current ICMJE criteria for authorship.
References
- 1.Milder B., Rubin M.L. Progressive power lenses. Surv Ophthalmol. 1987;32(3):189–198. doi: 10.1016/0039-6257(87)90094-4. [DOI] [PubMed] [Google Scholar]
- 2.Atchison D.A. Optical performance of progressive power lenses. Clin Exp Optom. 1987;70(5):149–155. [Google Scholar]
- 3.Villegas E.A., Artal P. Spatially resolved wavefront aberrations of ophthalmic progressive-power lenses in normal viewing conditions. Optom Vis Sci. 2003;80(2):106–114. doi: 10.1097/00006324-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 4.De Vries N.E., Nuijts R.M.M.A. Multifocal intraocular lenses in cataract surgery: literature review of benefits and side effects. J Cataract Refract Surg. 2013;39(2):268–278. doi: 10.1016/j.jcrs.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Charman W.N. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34(4):397–426. doi: 10.1111/opo.12129. [DOI] [PubMed] [Google Scholar]
- 6.Sheppard A.L., Bashir A., Wolffsohn J.S., Davies L.N. Accommodating intraocular lenses: a review of design concepts, usage and assessment methods. Clin Exp Optom. 2010;93(6):441–452. doi: 10.1111/j.1444-0938.2010.00532.x. [DOI] [PubMed] [Google Scholar]
- 7.Marcos S., Ortiz S., Pérez-Merino P., Birkenfeld J., Durán S., Jiménez-Alfaro I. Three-dimensional evaluation of accommodating intraocular lens shift and alignment in vivo. Ophthalmology. 2014;121(1):45–55. doi: 10.1016/j.ophtha.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 8.Yilmaz O.F., Bayraktar S., Agca A., Yilmaz B., McDonald M.B., van de Pol C. Intracorneal inlay for the surgical correction of presbyopia. J Cataract Refract Surg. 2008;34(11):1921–1927. doi: 10.1016/j.jcrs.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Tabernero J., Artal P. Optical modeling of a corneal inlay in real eyes to increase depth of focus: optimum centration and residual defocus. J Cataract Refract Surg. 2012;38(2):270–277. doi: 10.1016/j.jcrs.2011.07.040. [DOI] [PubMed] [Google Scholar]
- 10.Seyeddain O., Riha W., Hohensinn M., Nix G., Dexl A.K., Grabner G. Refractive surgical correction of presbyopia with the AcuFocus small aperture corneal inlay: two-year follow-up. J Refract Surg. 2010;26(10):707–715. doi: 10.3928/1081597X-20100408-01. [DOI] [PubMed] [Google Scholar]
- 11.Plainis S., Petratou D., Giannakopoulou T., Radhakrishnan H., Pallikaris I.G., Charman W.N. Interocular differences in visual latency induced by reduced-aperture monovision. Ophthalmic Physiol Opt. 2013;33(2):123–129. doi: 10.1111/opo.12018. [DOI] [PubMed] [Google Scholar]
- 12.Artal P., Manzanera S. Perceived brightness with small apertures. J Cataract Refract Surg. 2018;44(6):734–737. doi: 10.1016/j.jcrs.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 13.Stiles W.S. The luminous efficiency of rays entering the eye pupil at different points. Proc R Soc B Biol Sci. 1933;112:428–450. [Google Scholar]
- 14.Schwarz C., Prieto P.M., Fernandez E.J., Artal P. Binocular adaptive optics vision analyzer with full control over the complex pupil functions. Opt Lett. 2011;36(24):4779–4781. doi: 10.1364/OL.36.004779. [DOI] [PubMed] [Google Scholar]
- 15.Manzanera S., Artal P. Minimum change in spherical aberration that can be perceived. Biomed Opt Express. 2016;7(9):3471–3477. doi: 10.1364/BOE.7.003471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brücke E. Über den Nutzeffect intermittierender Netzhautreizungen. Sitzungsber k Akad Wissensch Math-naturw Cl, Wien. 1864;49:128–153. [Google Scholar]
- 17.Bartley S.H. Subjective brightness in relation to flash rate and the light-dark ratio. J Exp Psychol. 1938;23(3):313–319. [Google Scholar]
- 18.Crawford B.H. Visual adaptation in relation to brief conditioning stimuli. Proc R Soc B Biol Sci. 1947;134(875):283–302. doi: 10.1098/rspb.1947.0015. [DOI] [PubMed] [Google Scholar]
- 19.Lamb T.D. The role of photoreceptors in light-adaptation and dark-adaptation of the visual system. In: Blakemore C., editor. Vision: Coding and Efficiency. Cambridge University Press; Cambridge: 1990. pp. 161–168. [Google Scholar]
- 20.Aubert H. E. Morgenstern; 1865. Physiologie Der Netzhaut. Breslau. [Google Scholar]
- 21.Hecht S., Haig C., Chase A.M. The influence of light adaptation on subsequent dark adaptation of the eye. J Gen Physiol. 1937;20(6):831–850. doi: 10.1085/jgp.20.6.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reuter T. Fifty years of dark adaptation 1961-2011. Vision Res. 2011;51(21-22):2243–2262. doi: 10.1016/j.visres.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 23.Bouman M.A., Ten Doesschate J. The mechanism of dark adaptation. Vision Res. 1962;1(5-6):386–403. [Google Scholar]