Abstract
Introduction:
Early recognition of prediabetes may prevent progression to diabetes, yet not all adults are aware of their prediabetes risk. To reach all adults unaware of their risk, additional risk assessment strategies are warranted.
Objectives:
The objective of this study was to evaluate the potential scope of benefit from prediabetes risk assessment in the dental care setting and to identify characteristics of dental patients likely to unknowingly have prediabetes or diabetes.
Methods:
Data from 10,472 adults in the National Health and Nutrition Examination Survey from 2013 to 2014 and 2015 to 2016 were analyzed for associations among prediabetes/diabetes risk factors, health care use, and hemoglobin A1C levels according to chi-square tests and multivariate logistic regression.
Results:
A total of 7.73% of US adults had seen a dentist but not a medical provider in the past 12 mo. The composition of this subpopulation was significantly different from that who saw a medical provider, in ways that might affect their diabetes risk. In addition, 31.27% of this subpopulation would be identified as being at high risk for prediabetes according to the CDC Prediabetes Screening Test (Centers for Disease Control and Prevention), and 15.83% had hemoglobin A1C levels indicative of undiagnosed prediabetes or diabetes. Screening in a dental setting would have the highest odds of identifying someone unaware of his or her diabetes risk among those who were non-White, obese, or ≥45 y old.
Conclusion:
Extrapolation from this analysis indicates that screening for prediabetes at dental visits has the potential to alert an estimated 22.36 million adults of their risk for prediabetes or diabetes. Incorporating prediabetes or diabetes risk assessment into routine dental visits may enable 1) those with prediabetes to take action to decrease their risk of developing diabetes and 2) those with diabetes to engage in treatment to decrease their risk of diabetes-related complications.
Knowledge Transfer Statement:
Screening for prediabetes and diabetes during dental visits has the potential to raise patients’ awareness of diabetes risk and prevent prediabetes from progressing to diabetes. For some patients, the dental visit may be the only point of contact with the health care system, which heightens the importance of including diabetes risk assessment for patient well-being.
Keywords: glycated hemoglobin A, nutrition surveys, hyperglycemia, asymptomatic diseases, chronic disease, dentistry
Introduction
Prediabetes is a reversible condition in which plasma glucose levels are higher than normal but below levels diagnostic of type 2 diabetes (American Medical Association and Centers for Disease Control and Prevention [CDC] 2015). Prediabetes is associated with an increased risk of cardiovascular disease, coronary heart disease, stroke, and all-cause mortality (Huang et al. 2016). If prediabetes is left untreated, 15% to 30% of people with it progress to type 2 diabetes within 5 y (American Medical Association and CDC 2015). Type 2 diabetes is a major contributor to morbidity, mortality, and health care costs (CDC 2017b). It is the leading cause of kidney failure, lower limb amputations, and adult-onset blindness, and it significantly increases the risk of heart attack and stroke (CDC 2016a). The costs associated with diabetes in 2017 were an estimated $327 billion per year, accounting for >1 in 4 health care dollars spent in the United States (American Diabetes Association 2018d). Diabetes is also relevant to oral health. Periodontal disease and diabetes are common conditions, and the American Diabetes Association (2018b) reports greater periodontal disease severity and prevalence among people with diabetes. The association between the diseases appears to include bidirectional exacerbation (Chapple et al. 2013).
Diabetes frequently remains unrecognized and undiagnosed until complications appear. In the United States as of 2015, 88.4% of people with prediabetes and 23.8% of people with diabetes are unaware of their increased risk of diabetes and diabetes-related complications (CDC 2017b). Prediabetes risk assessment, commonly referred to as screening, is one strategy to address this. Screening evaluates people with no overt symptoms of diabetes for factors that increase their risk of developing diabetes, such as age, family history of diabetes, and physical inactivity. For those with prediabetes, awareness of diabetes risk enables them to engage in activities to reduce their risk of developing diabetes; there are robust data demonstrating that behavioral intervention alone or the combination of behavioral and pharmacologic intervention can prevent or delay the development of diabetes (Knowler et al. 2002; Herman et al. 2005; Aroda et al. 2017). For individuals with diabetes, screening is a first step toward obtaining a diagnosis of diabetes, which is requisite to engaging in treatment that can postpone or even prevent diabetes-associated micro- and macrovascular complications. An estimated 75% of people with diabetes receive a “late diagnosis,” meaning that within 6 mo of diagnosis, they have at least 1 diabetes-related comorbidity or complication (Roche and Wang 2014). Increased participation in screening has the potential to result in earlier detection, thus preventing or delaying progression of diabetes and its complications (Herman, Ye, et al. 2015; Feldman et al. 2017).
The American Diabetes Association (2018a) and the American Medical Association and the CDC (2015) recommended screening adults for prediabetes and type 2 diabetes with a short risk factor assessment. The CDC suggested that the dental office may be a useful setting in which to identify individuals with undiagnosed prediabetes or diabetes (CDC 2014), and the American Diabetes Association (2017) indicated that further research was needed demonstrating the feasibility of screening in a dental care setting. When surveyed, dentists (Greenberg et al. 2010), dental hygienists (Greenberg et al. 2017), physicians (Greenberg et al. 2015), and dental patients (Greenberg et al. 2012) agreed that screening was acceptable in a dental setting. This study was conducted to estimate the size and demographics of the population that might be identified if prediabetes or diabetes risk factor assessment was routine in the dental care setting.
Methods
The National Health and Nutrition Examination Survey (NHANES) is a stratified multistage probability sample of the civilian noninstitutionalized population of the United States. During the survey period, participants were interviewed at home and then received a standardized physical examination of objective measures in a mobile center (US Department of Health and Human Services 2018). For the present data analysis, we used the most recently available public use data files (2013 to 2014 and 2015 to 2016). We restricted the sample to those ≥20 y whose hemoglobin A1C was measured. Pregnant participants were excluded due to universal screening for gestational diabetes and because pregnancy affects glucose measurements.
Self-reported survey data included age, sex, race, ethnicity, and frequency and type of health care encounters. The race/ethnicity categories were non-Hispanic White, non-Hispanic Black, Mexican American, other Hispanic, non-Hispanic Asian, and other race. Bivariate analyses of Mexican American and other Hispanic groups were conducted with all independent and dependent variables in this analysis. These groups were statistically similar in every comparison except the proportion who had seen a health care worker in the last year but did not have a dental visit (48.5% for Mexican Americans vs. 38.1% for other Hispanics, chi-square P < 0.0001). Therefore, Mexican Americans and other Hispanics were combined to form a single group termed “Hispanics,” allowing for sufficient numbers to calculate reliable variance estimates. Health care utilization patterns were based on any self-report of dental or health care use in the last 12 mo. Individuals who reported having been told by a doctor or health professional that they had prediabetes or diabetes were categorized as having had a diagnosis of prediabetes or diabetes, respectively. Those who reported doing no moderate or vigorous physical activity during a typical week were categorized as getting little to no exercise in a typical day. Adults were classified as meeting the US Department of Health and Human Services’ (2008) physical activity guidelines if they reported participating in at least 150 min of moderate/vigorous-intensity or 75 min of vigorous-intensity physical activity per week at work and leisure.
The clinical examination data included height, weight, and hemoglobin A1C. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. BMI was interpreted with the standard categories of normal (18.5 to 24.9), overweight (25 to 29.9), and obese (≥30.0; CDC 2017a). The American Diabetes Association’s (2017) criteria were used for prediabetes (hemoglobin A1C, 5.7% to 6.4% [39 to 46 mmol/mol]) and diabetes (hemoglobin A1C ≥6.5% [48 mmol/mol]). Those who did not report having been diagnosed with prediabetes or diabetes but who had elevated A1C levels were considered to have unknown prediabetes or unknown potential diabetes.
Survey and examination data were used to calculate a risk score for each individual in the sample, on the basis of the CDC Prediabetes Screening Test (CDC 2016b), which has 74% sensitivity and 54% specificity for undiagnosed prediabetes and diabetes (Poltavskiy et al. 2016). The CDC Prediabetes Screening Test consists of 7 questions, answered as yes or no. Points are assigned for each yes answer, then totaled for a score ranging from 0 to 18. Those taking the test are assigned 9 points for being ≥65 y old, 5 points for being 45 to 64 y old, and 5 points for <65 y old and getting little to no exercise on a typical day. Five points are assigned for those with BMI >27. One point each is assigned to having had a baby weighing >9 lb at birth, having a sibling with diabetes, or having a parent with diabetes. Scoring ≥9 signifies high risk for prediabetes. Although the NHANES data set contained information on age, BMI, and physical activity, responses to questions about family history of diabetes or baby weight were available only for individuals who had indicated that they felt as though they were at risk for diabetes (n = 2,659, 25.4%). Since the missing data could add at most a maximum of 3 points to a respondent’s score, missing information on baby weight or family history of diabetes did not affect whether a respondent was classified as above or below the prediabetes risk threshold.
All statistical analyses were conducted in SAS 9.4 (SAS Institute), with NHANES examination subsample weights for 4-year nationally representative estimates. Taylor series linearization to estimate variance and Rao-Scott chi-square tests to determine whether there was a significant relationship among categorical variables were used to adjust for the complex survey design. Single and multivariate logistic regression models calculated the odds of unknown prediabetes or potential diabetes among dental patients. All variables in the bivariate analyses were initially included in the models; independent variables that were nonsignificant in crude models were not included in the final regression models.
Results
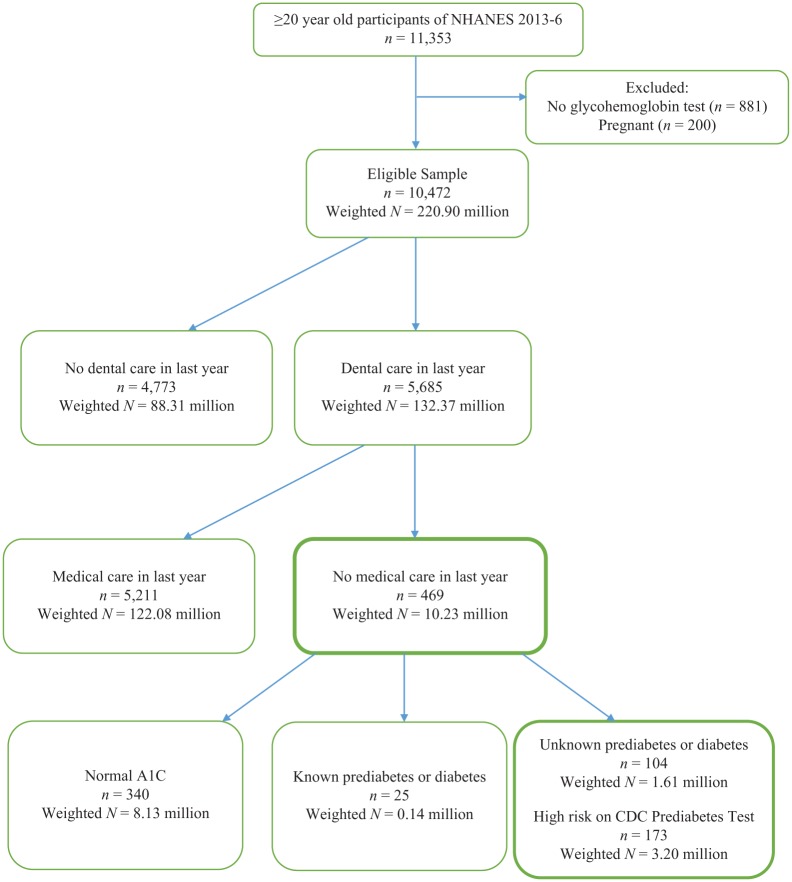
The NHANES cycles from 2013 to 2014 and 2015 to 2016 included 11,553 adults aged ≥20 y. The 200 pregnant participants and 881 participants without hemoglobin A1C test results were excluded (Fig.). The group without hemoglobin A1C test results had a significantly smaller proportion of male respondents (48.1% missing A1C results vs 48.7% not missing, P = 0.03), older adults (54.2% aged 20 to 44 y without A1C vs. 44.0% with A1C, P = 0.001), and non-Hispanic Whites (51.1% without A1C vs. 65.5% with A1C, P < 0.0001). The remaining 10,472 participants served as the study population, and their demographics and diabetes-related characteristics are described in Table 1. Based on A1C results, the prevalences of undiagnosed prediabetes and diabetes were, respectively, 17.31% and 1.64% of the sample. Those with undiagnosed prediabetes or diabetes included significantly higher proportions of older adults, overweight or obese adults, and non-White adults, as compared with those having normal A1C levels. The majority of adults in the survey (78.17%) did not meet the physical activity guidelines for moderate and vigorous activity per week. Among those with unrecognized prediabetes or diabetes, the proportion of individuals not meeting levels of physical activity sufficient for moderate or vigorous activity (82.23%) was significantly higher than that among those having normal A1C levels (76.22%; P = 0.0004). As predicted, significantly more of those with unrecognized prediabetes and diabetes (73.45% and 82.40%, respectively) scored as being at risk for prediabetes on the CDC Prediabetes Screening Test as compared with those having normal A1C levels (42.32%; P < 0.0001).
Figure.
Sample selection and health care use flowchart: National Health and Nutrition Examination Survey (NHANES) 2013 to 2016. CDC, Centers for Disease Control and Prevention.
Table 1.
Sample Characteristics: NHANES 2013 to 2016 (N = 10,472).
| Entire Sample | Undiagnosed Potential Diabetes | Undiagnosed Prediabetes | |||||
|---|---|---|---|---|---|---|---|
| Unweighted, n | Prevalence(95% CI) | Unweighted, n | Prevalence(95% CI) | Unweighted, n | Prevalence(95% CI) | P Value | |
| Total population | 10,472 | 240 | 1.6(1.3 to 2.0) | 2,090 | 17.3(16.4 to 18.3) | ||
| Sex | 0.1 | ||||||
| Male | 5,067 | 48.7(47.8 to 49.6) | 113 | 51.0(42.2 to 59.8) | 1,001 | 46.3(44.3 to 48.3) | |
| Female | 5,405 | 51.3(50.5 to 52.2) | 127 | 49.0(40.2 to 57.8) | 1,089 | 53.7(51.7 to 55.7) | |
| Age, y | <0.0001 | ||||||
| 20 to 44 | 4,382 | 44.0(42.1 to 46.0) | 47 | 22.5(14.7 to 30.4) | 522 | 24.7(22.1 to 27.3) | |
| 45 to 64 | 3,797 | 37.7(35.1 to 39.2) | 119 | 52.2(42.6 to 61.7) | 920 | 45.5(42.1 to 48.9) | |
| ≥65 | 2,293 | 18.3(16.8 to 19.8) | 74 | 25.3(18.4 to 32.2) | 648 | 29.8(26.7 to 32.8) | |
| Race/ethnicity | <0.0001 | ||||||
| Non-Hispanic White | 4,028 | 65.5(60.4 to 70.6) | 58 | 47.1(35.3 to 59.0) | 665 | 57.8(51.8 to 63.9) | |
| Non-Hispanic Black | 2,112 | 10.9(8.2 to 13.7) | 64 | 18.6(12.6 to 24.6) | 558 | 16.6(12.5 to 20.7) | |
| Hispanic | 2,786 | 15.0(11.3 to 18.6) | 75 | 20.7(12.4 to 29.0) | 580 | 16.6(12.2 to 21.0) | |
| Non-Hispanic Asian | 1,209 | 5.5(4.1 to 6.9) | 39 | 11.1(6.8 to 15.4) | 234 | 6.0(4.4 to 7.5) | |
| Other race/ethnicity | 337 | 3.2(2.5 to 3.8) | 4 | 2.5(0 to 5.7) | 53 | 3.0(1.9 to 4.1) | |
| Body mass index | <0.0001 | ||||||
| Normal weight | 2,795 | 27.6(25.8 to 29.3) | 23 | 7.8(3.9 to 11.6) | 425 | 19.4(17.0 to 21.8) | |
| Overweight | 3,339 | 32.9(31.9 to 33.9) | 64 | 20.5(14.0 to 27.0) | 706 | 33.5(30.7 to 36.4) | |
| Obese | 4,069 | 39.5(37.7 to 41.3) | 148 | 71.8(64.5 to 79.1) | 916 | 47.0(44.3 to 49.8) | |
| Care utilization | |||||||
| Health care last year, no dental visit | 3,713 | 34.2(31.6 to 36.8) | 88 | 43.7(34.5 to 52.9) | 754 | 37.1(34.3 to 39.9) | <0.0001 |
| Dental care last year, no health visit | 469 | 4.6(4.2 to 5.1) | 12 | 3.8(1.8 to 5.8) | 92 | 4.0(3.1 to 4.9) | 0.005 |
| Physical activity | 0.0003 | ||||||
| Met CDC guidelines | 1,892 | 21.9(20.1 to 23.7) | 25 | 14.1(7.9 to 20.3) | 329 | 18.1(15.1 to 21.2) | |
| Did not meet CDC guidelines | 8,580 | 78.1(76.3 to 79.9) | 215 | 85.9(79.7 to 92.1) | 1,761 | 81.9(78.8 to 84.9) | |
| Health insurance or health care plan | 0.6 | ||||||
| Yes | 8,434 | 84.4(82.5 to 86.2) | 191 | 83.2(79.0 to 87 to 43) | 1,684 | 84.0(81.0 to 86.9) | |
| No | 2,024 | 15.6(13.8 to 17.5) | 49 | 16.8(12.6 to 21.0) | 400 | 16.1(13.1 to 19.0) | |
| Screening test | 82.4(75.8 to 89.0) | 73.5(70.9 to 76.0) | <0.0001 | ||||
| <9 | 6,110 | 45.4(43.6 to 47.3) | 202 | 17.6(11.0 to 24.2) | 1,546 | 26.6(24.0 to 29.1) | |
| ≥9 | 10,472 | 54.6(52.7 to 56.4) | 240 | 82.4(75.8 to 89.0) | 2,090 | 73.5(70.9 to 76.0) | |
CDC, Centers for Disease Control and Prevention; NHANES, National Health and Nutrition Examination Survey.
From 2013 to 2016, 59.98% of participants saw a dentist in the past 12 mo. An estimated 7.73% of these people did not see or talk to any other doctor or health care professional in that time (Fig.). This subpopulation of patients differed significantly from those who had both a medical visit and a dental visit (Table 2). It was composed of a higher proportion of men and non-Hispanic Black, Hispanic, or non-Hispanic Asian adults; it was also comparatively younger. The subpopulation of adults who saw a dentist but not another medical provider in the last 12 mo had a significantly lower proportion of overweight or obese adults (64.97% vs. 71.35%, P < 0.0001) and a higher proportion that met the CDC’s guidelines for moderate or intense physical activity per week (26.62% vs. 23.73%, P < 0.0001). People who saw a health or dental professional in the last year were more likely to have some kind of health insurance or health care plan than those who did not (93.36% vs. 50.40%, P < 0.0001).
Table 2.
Characteristics by Recent Health Care Utilization Pattern: NHANES 2013 to 2016 (N = 10,472).
| Health Visit, No Dental Visit | Dental Visit, No Health Visit | Both Health and Dental Care in Past 12 mo | No Health or Dental Care in Past 12 mo | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Unweighted, n | Prevalence(95% CI) | Unweighted, n | Prevalence(95% CI) | Unweighted, n | Prevalence(95% CI) | Unweighted, n | Prevalence(95% CI) | P Value | |
| Total population | 3,713 | 31.1(28.9 to 33.4) | 469 | 4.6(4.2 to 5.1) | 5,211 | 55.4(52.7 to 58.0) | 1,052 | 8.9(8.1 to 9.7) | |
| Sex | <0.0001 | ||||||||
| Male | 1,794 | 47.1(45.0 to 49.1) | 302 | 68.9(64.3 to 73.5) | 2,247 | 44.4(42.5 to 46.2) | 714 | 71.0(67.4 to 74.7) | |
| Female | 1,919 | 52.9(50.9 to 55.0) | 167 | 31.1(26.5 to 35.7) | 2,964 | 55.7(53.8 to 57.5) | 338 | 29.0(25.3 to 32.6) | |
| Age group, y | <0.0001 | ||||||||
| 20 to 44 | 1,476 | 45.8(42.9 to 48.7) | 306 | 65.9(60.1 to 71.6) | 1,941 | 37.8(35.2 to 40.3) | 647 | 65.4(62.3 to 68.5) | |
| 45 to 64 | 1,289 | 35.0(32.8 to 37.1) | 147 | 32.4(26.1 to 38.6) | 2,010 | 40.8(38.6 to 43.0) | 346 | 30.6(27.6 to 33.6) | |
| ≥65 | 948 | 19.2(17.0 to 21.5) | 16 | 1.8(0.7 to 2.9) | 1,260 | 21.4(19.5 to 23.3) | 59 | 4.0(2.5 to 5.6) | |
| Race/ethnicity | <0.0001 | ||||||||
| Non-Hispanic White | 1,374 | 60.6(54.8 to 66.5) | 152 | 60.0(51.9 to 68.1) | 2,203 | 71.6(67.0 to 76.3) | 294 | 47.9(41.0 to 54.9) | |
| Non-Hispanic Black | 867 | 13.9(10.2 to 17.5) | 69 | 8.4(5.2 to 11.6) | 993 | 9.4(7.1 to 11.6) | 178 | 11.2(8.5 to 13.9) | |
| Hispanic | 1,030 | 17.2(12.9 to 21.5) | 134 | 19.0(13.8 to 24.2) | 1,177 | 10.5(7.6 to 13.4) | 431 | 32.1(25.4 to 38.8) | |
| Non-Hispanic Asian | 326 | 4.8(3.7 to 5.9) | 102 | 10.2(7.6 to 12.9) | 661 | 5.4(3.7 to 7.2) | 118 | 5.9(3.8 to 8.0) | |
| Other race/ethnicity | 116 | 3.5(2.3 to 4.7) | 12 | 2.4(0.7 to 4.1) | 177 | 3.1(2.4 to 3.8) | 31 | 2.8(1.9 to 3.8) | |
| Body mass index | <0.0001 | ||||||||
| Normal weight | 902 | 24.3(22.1 to 26.5) | 163 | 35.0(27.3 to 42.7) | 1,430 | 28.7(26.7 to 30.6) | 296 | 28.4(24.5 to 32.2) | |
| Overweight | 1,097 | 28.9(27.3 to 30.7) | 157 | 35.1(28.4 to 41.9) | 1,717 | 34.7(32.2 to 36.3) | 357 | 34.2(30.0 to 38.5) | |
| Obese | 1,600 | 46.8(44.2 to 49.3) | 140 | 29.8(24.0 to 35.7) | 1,938 | 36.6(34.4 to 38.8) | 380 | 37.4(33.5 to 41.3) | |
| Physical activity | <0.0001 | ||||||||
| Met CDC guidelines | 579 | 17.8(15.9 to 19.7) | 109 | 26.6(22.5 to 30.7) | 998 | 23.7(21.2 to 26.3) | 204 | 22.5(19.1 to 25.8) | |
| Did not meet CDC guidelines | 3,134 | 82.2(80.3 to 84.1) | 360 | 73.4(69.3 to 77.5) | 4,213 | 76.3(73.7 to 78.9) | 848 | 77.5(74.2 to 80.9) | |
| Health insurance or health care plan | <0.0001 | ||||||||
| Yes | 2,876 | 79.4(77.3 to 81.5) | 324 | 75.6(71.6 to 79.6) | 4,750 | 93.4(92.0 to 94.7) | 464 | 50.4(44.7 to 56.2) | |
| No | 831 | 20.6(18.5 to 22.7) | 145 | 24.4(20.4 to 28.4) | 455 | 6.6(5.3 to 8.0) | 595 | 49.6(43.9 to 55.4) | |
| CDC prediabetes screen score | <0.0001 | ||||||||
| <9 | 1,414 | 43.3(40.4 to 46.2) | 296 | 68.7(62.6 to 74.8) | 2,048 | 42.2(40.1 to 44.3) | 595 | 61.0(58.1 to 63.9) | |
| ≥9 | 2,299 | 56.7(53.8 to 59.6) | 173 | 31.3(25.2 to 37.4) | 3,163 | 57.8(55.7 to 59.9) | 457 | 39.0(36.1 to 41.9) | |
| Undiagnosed | |||||||||
| Prediabetes | 754 | 19.3(17.5 to 21.1) | 92 | 14.5(10.9 to 18.1) | 999 | 17.1(16.0 to 18.3) | 237 | 20.3(17.3 to 23.2) | 0.009 |
| Potential diabetes | 88 | 2.1(1.5 to 2.6) | 12 | 1.3(0.6 to 2.0) | 98 | 1.3(0.9 to 1.8) | 41 | 3.0(1.9 to 4.0) | 0.0005 |
CDC, Centers for Disease Control and Prevention; NHANES, National Health and Nutrition Examination Survey.
Although those seeing a dentist were comparatively younger and less likely to be overweight than those who had seen a medical professional in the last year, they were not free from risk factors for diabetes. Based on the information available from NHANES, 55.73% of adults who had seen a dentist in the previous year had a score on the CDC Prediabetes Screening Test sufficient to warrant referral to a medical provider for a definitive diagnosis of diabetes.
Based on the hemoglobin A1C results in NHANES for all those who had seen a dentist in the previous year (as an estimate of their glycemic status from 2013 to 2016), an estimated 18.24% would have been defined as having unknown prediabetes and diabetes. For the smaller group for whom a dental provider was the only point of contact with the health care system, 31.27% would have had a score on the CDC Prediabetes Screening Test indicative of prediabetes (Table 2). Based on hemoglobin A1C, 15.83% of this subset had undiagnosed prediabetes or diabetes.
Table 3 displays the crude and adjusted odds ratios (ORs) of the characteristics for those who had a dental visit but were unaware of their elevated A1C. The factors known to be associated with an increased risk of diabetes in the general population were also associated with an increased risk of undiagnosed prediabetes or diabetes in this subpopulation. Thus, after adjusting for sex, race/ethnicity, BMI, and physical activity level, increasing age was associated with significantly increased odds of unrecognized prediabetes or diabetes (Table 3). As compared with those aged 20 to 44 y, those aged 45 to 64 y had significantly greater odds (adjusted OR: 3.37, 95% CI: 1.91 to 5.93) of potentially having diabetes but being unaware of it, and those aged ≥65 y had even higher odds (adjusted OR: 4.26, 95% CI: 2.59 to 7.00). Similarly, elevated BMI was associated with significantly increased odds of potentially having diabetes, with overweight adults having 2.28 the odds (95% CI: 1.24 to 4.20) and obese adults 8.44 the odds (95% CI: 4.96 to 14.36) as compared with those having normal BMI. When compared with non-Hispanic White adults, non-Hispanic Black, Hispanic, and non-Hispanic Asian adults and those of other races and ethnicities had higher odds of potentially unrecognized prediabetes or diabetes. Insufficient weekly physical activity was associated with significantly higher odds of undiagnosed prediabetes (OR: 1.33, 95% CI: 1.07 to 1.67) and undiagnosed diabetes (OR: 1.77, 95% CI: 1.03 to 3.04), but the odds reduced to statistical nonsignificance after adjusting for sex, age group, race/ethnicity, and BMI.
Table 3.
Odds of Undiagnosed Prediabetes or Diabetes for Those Visiting a Dentist in Last Year (n = 5,685).
| Odds of Undiagnosed Diabetes (95% CI) [P Value] | Odds of Undiagnosed Prediabetes (95% CI) [P Value] | |||
|---|---|---|---|---|
| Crude | Adjusteda | Crude | Adjusteda | |
| Sex | ||||
| Female | Reference | Reference | Reference | Reference |
| Male | 1.13(0.77 to 1.65) [0.5] | 1.32(0.88 to 1.97) [0.2] | 0.87(0.79 to 0.96) [0.008] | 0.92(0.82 to 1.04) [0.2] |
| Age, y | ||||
| 20 to 44 | Reference | Reference | Reference | Reference |
| 45 to 64 | 3.00(1.78 to 5.06) [0.0002] | 3.37(1.91 to 5.93) [0.0001] | 2.69(2.28 to 3.16) [<0.0001] | 2.84(2.40 to 3.37) [<0.0001] |
| ≥65 | 3.15(2.02 to 4.90) [<0.0001] | 4.26(2.59 to 7.00) [<0.0001] | 4.40(3.59 to 5.41) [<0.0001] | 5.14(4.13 to 6.40) [<0.0001] |
| Race/ethnicity | ||||
| Non-Hispanic White | Reference | Reference | Reference | Reference |
| Non-Hispanic Black | 2.49(1.65 to 3.76) [<0.0001] | 2.63(1.71 to 4.04) [<0.0001] | 2.08(1.84 to 2.36) [<0.0001] | 2.59(2.29 to 2.94) [<0.0001] |
| Hispanic | 1.99(1.23 to 3.21) [0.006] | 2.28(1.36 to 3.83) [0.003] | 1.31(1.11 to 1.53) [0.002] | 1.74(1.47 to 2.07) [<0.0001] |
| Non-Hispanic Asian | 2.90(1.75 to 4.81) [0.0002] | 6.36(3.75 to 10.79) [<0.0001] | 1.29(1.09 to 1.54) [0.005] | 2.00(1.67 to 2.38) [<0.0001] |
| Other race/ethnicity | 1.13(0.28 to 4.47) [0.9] | 1.25(0.29 to 5.30) [0.8] | 1.09(0.75 to 1.57) [0.6] | 1.34(0.93 to 1.92) [0.1] |
| Body mass index | ||||
| Normal weight | Reference | Reference | Reference | Reference |
| Overweight | 2.30(1.27 to 4.16) [0.007] | 2.28(1.24 to 4.20) [0.01] | 1.62(1.34 to 1.95) [<0.0001] | 1.48(1.20 to 1.83) [0.0006] |
| Obese | 7.39(4.41 to 12.40) [<0.0001] | 8.44(4.96 to 14.36) [<0.0001] | 2.05(1.72 to 2.44) [<0.0001] | 1.93(1.61 to 2.32) [<0.0001] |
| Physical activity | ||||
| Met CDC guidelines | Reference | Reference | Reference | Reference |
| Did not meet CDC guidelines | 1.77(1.03 to 3.04) [0.04] | 1.42(0.82 to 2.43) [0.2] | 1.33(1.07 to 1.67) [0.01] | 1.07(0.86 to 1.33) [0.5] |
CDC, Centers for Disease Control and Prevention; NHANES, National Health and Nutrition Examination Survey.
Models adjusted for all other variables in table.
Discussion
Using the data from this analysis to extrapolate to the US population, we estimate that among the 10.23 million individuals who had a routine dental visit but no medical visit in the last year, 1.61 million adults were unaware that they were at risk for prediabetes or diabetes. For these individuals, given the absence of a medical provider visit, their routine dental visit represents a unique health care encounter during which to screen for prediabetes or diabetes risk. Our results are consistent with those reported for a similar analysis conducted with data from the New York City Community Health Survey (Myers-Wright et al. 2018) or previous NHANES cycles (Borrell et al. 2007).
In addition, these results indicate that 20.75 million individuals nationwide had both a dental visit and a medical visit in the last year and were unaware of their prediabetes or diabetes risk. Although for these people the dental visit was not the only opportunity to raise awareness about their risk, the dental visit does represent an opportunity to 1) reinforce a message that they had failed to hear or 2) raise their awareness about something not discussed during their medical visit. In both circumstances, screening for prediabetes or diabetes risk in the dental care setting has the potential to increase individual awareness about diabetes risk. Doing so can better enable engagement in the lifestyle change to reduce the likelihood of developing periodontal disease, diabetes, or other conditions (Feldman et al. 2017).
Patients complete or update their medical history forms while waiting to be seen by dental health professionals. Prediabetes or diabetes risk screening could be added with a printed or online version of the current 7-item assessment, available through organizations such as the American Diabetes Association, CDC, and the American Medical Association. Such screening tools are designed to be simple and noninvasive, and they can be self-administered by patients (Poltavskiy et al. 2016). Similar prediabetes risk assessments were successfully conducted in dental settings (Lalla et al. 2011; Herman, Taylor, et al. 2015).
There are alternative methods to identify those at high risk of prediabetes or diabetes. A recent study conducted in the setting of a Federally Qualified Health Center, with a fully integrated dental and medical electronic health record database, presented a model for predicting dysglycemia that incorporated data on patient demographics, clinical examination, and dental examination and correctly identified 70% of the dental patients with undiagnosed prediabetes or diabetes (Acharya et al. 2018). Although this is promising, the majority of current dental practices do not have access to patient medical electronic health records. Until such time that they do, having patients complete a short risk assessment screening test has the potential to increase patients’ awareness of their potential prediabetes risk.
Based on this analysis, for every 10 patients aged ≥20 y who had their risk assessed in a dental setting in the United States, 2 might have had prediabetes or diabetes that had not yet been diagnosed. For patients scoring in the high-risk range of prediabetes or diabetes on a risk assessment screening test, dental personnel can 1) recommend that they seek out testing and care from a physician and 2) provide them with materials about prediabetes and diabetes from reliable sources, such as the American Diabetes Association (2018c) and CDC (2016c). The value of alerting dental patients about their prediabetes or diabetes risk is that it leads to physician follow-up (Genco et al. 2014), positive lifestyle changes, and reduction in A1C (Lalla et al. 2015).
This analysis is subject to limitations. NHANES is collected at a single point in time, which limits its ability to prove temporal relationships or causality. The classification of prediabetes or diabetes diagnosis and health care utilization was based on survey data, which are subject to social desirability and recall bias. Furthermore, a single measure of A1C was used to identify potential undiagnosed diabetes, which may have misclassified the glycemic status of some participants in the NHANES data set. The American Diabetes Association (2018a) recommended either clinical symptoms or a second confirmatory blood-based test for diagnosis confirmation.
This analysis does, however, demonstrate the potential benefit of incorporating prediabetes screening into the dental care visit to identify individuals at high risk of prediabetes or diabetes and refer them to medical care. This does not represent a circumstance where dentists would make medical diagnoses or provide treatment for diabetes but rather refer at-risk individuals for follow-up with medical providers for diagnosis and care.
Conclusion
This analysis supports that not all adults are aware of their risk of prediabetes or diabetes. Screening for prediabetes or diabetes risk factors during dental visits has the potential to raise patients’ awareness of their risk. In addition, for some dental patients, the dental visit may be their only point of contact with the health care system. For all patients whom a dentist sees, there is an opportunity to raise awareness about an important health risk and contribute to their overall well-being.
Author Contributions
C.G. Estrich, contributed to conception, design, data analysis, and interpretation, drafted and critically revised manuscript; M.W.B. Araujo, contributed to conception, design, and data interpretation, drafted and critically revised manuscript; R.D. Lipman, contributed to conception, design, and data interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Footnotes
The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
ORCID iDs: C.G. Estrich  https://orcid.org/0000-0001-6156-5177
https://orcid.org/0000-0001-6156-5177
R.D. Lipman  https://orcid.org/0000-0001-8632-3895
https://orcid.org/0000-0001-8632-3895
References
- Acharya A, Cheng B, Koralkar R, Olson B, Lamster IB, Kunzel C, Lalla E. 2018. Screening for diabetes risk using integrated dental and medical electronic health record data. JDR Clin Trans Res. 3(2):188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. 2017. Standards of medical care in diabetes—2017. Diabetes Care. 40 Suppl 1:S11–S24. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. 2018. a. Classification and diagnosis of diabetes. Diabetes Care. 41 Suppl 1:S13–S27. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. 2018. b. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes—2018. Diabetes Care. 41 Suppl 1:S28–S37. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. 2018. c. Diabetes basics. Arlington (VA): American Diabetes Association; [accessed 6 Jul 2018]. http://www.diabetes.org/diabetes-basics. [Google Scholar]
- American Diabetes Association. 2018. d. Economic costs of diabetes in the US in 2017. Diabetes Care. 41(5):917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Medical Association, Centers for Disease Control and Prevention. 2015. Preventing type 2 diabetes. Atlanta (GA): Centers for Disease Control and Prevention; [accessed 18 Apr 2018]. https://www.cdc.gov/diabetes/prevention/pdf/stat_toolkit.pdf. [Google Scholar]
- Aroda VR, Knowler WC, Crandall JP, Perreault L, Edelstein SL, Jeffries SL, Molitch ME, Pi-Sunyer X, Darwin C, Heckman-Stoddard BM, et al. 2017. Metformin for diabetes prevention: insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia. 60(9):1601–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Kunzel C, Lamster I, Lalla E. 2007. Diabetes in the dental office: using NHANES III to estimate the probability of undiagnosed disease. J Periodontal Res. 42(6):559–565. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2014. Working together to manage diabetes: a guide for pharmacy, podiatry, optometry, and dentistry. Atlanta (GA): Centers for Disease Control and Prevention; [accessed December 27, 2017]. https://www.cdc.gov/diabetes/ndep/toolkits/ppod.html. [Google Scholar]
- Centers for Disease Control and Prevention. 2016. a. At a glance 2016: diabetes—working to reverse the US epidemic. Atlanta (GA): Centers for Disease Control and Prevention; [accessed December 21, 2017]. https://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/2016/diabetes-aag.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. 2016. b. CDC Prediabetes Screening Test. Atlanta (GA): Centers for Disease Control and Prevention; [accessed 2018]. https://www.cdc.gov/diabetes/prevention/pdf/prediabetestest.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. 2016. c. National Diabetes Prevention Program: materials to engage patients. Atlanta: GA: Centers for Disease Control and Prevention; [accessed 17 Apr 2018]. https://www.cdc.gov/diabetes/prevention/lifestyle-program/deliverers/screening-referral.html. [Google Scholar]
- Centers for Disease Control and Prevention. 2017. a. About adult BMI. Atlanta (GA): Centers for Disease Control and Prevention; [accessed 17 Apr 2018]. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. [Google Scholar]
- Centers for Disease Control and Prevention. 2017. b. National diabetes statistics report, 2017. Atlanta (GA): Centers for Disease Control and Prevention; [accessed 27 Dec 2017]. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. [Google Scholar]
- Chapple IL, Genco R. Working Group 2 of the Joint EFP/AAP Workshop. 2013. Diabetes and periodontal diseases: consensus report of the joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol. 84(4):S106–S112. [DOI] [PubMed] [Google Scholar]
- Feldman AL, Griffin SJ, Fharm E, Norberg M, Wennberg P, Weinehall L, Rolandsson O. 2017. Screening for type 2 diabetes: do screen-detected cases fare better? Diabetologia. 60(11):2200–2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genco RJ, Schifferle RE, Dunford RG, Falkner KL, Hsu WC, Balukjian J. 2014. Screening for diabetes mellitus in dental practices: a field trial. J Am Dent Assoc. 145(1):57–64. [DOI] [PubMed] [Google Scholar]
- Greenberg BL, Glick M, Frantsve-Hawley J, Kantor ML. 2010. Dentists’ attitudes toward chairside screening for medical conditions. J Am Dent Assoc. 141(1):52–62. [DOI] [PubMed] [Google Scholar]
- Greenberg BL, Kantor ML, Bednarsh H. 2017. American dental hygienists’ attitudes towards chairside medical screening in a dental setting. Int J Dent Hyg. 15(4):e61–e68. [DOI] [PubMed] [Google Scholar]
- Greenberg BL, Kantor ML, Jiang SS, Glick M. 2012. Patients’ attitudes toward screening for medical conditions in a dental setting. J Public Health Dent. 72(1):28–35. [DOI] [PubMed] [Google Scholar]
- Greenberg BL, Thomas PA, Glick M, Kantor ML. 2015. Physicians’ attitudes toward medical screening in a dental setting. J Public Health Dent. 75(3):225–233. [DOI] [PubMed] [Google Scholar]
- Herman WH, Hoerger TJ, Brandle M, Hicks K, Sorensen S, Zhang P, Hamman RF, Ackermann RT, Engelgau MM, Ratner RE, et al. 2005. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med. 142(5):323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman WH, Taylor GW, Jacobson JJ, Burke R, Brown MB. 2015. Screening for prediabetes and type 2 diabetes in dental offices. J Public Health Dent. 75(3):175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman WH, Ye W, Griffin SJ, Simmons RK, Davies MJ, Khunti K, Rutten GE, Sandbaek A, Lauritzen T, Borch-Johnsen K, et al. 2015. Early detection and treatment of type 2 diabetes reduce cardiovascular morbidity and mortality: a simulation of the results of the Anglo-Danish-Dutch Study of Intensive Treatment in People with Screen-Detected Diabetes in Primary Care (ADDITION-Europe). Diabetes Care. 38(8):1449–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Cai X, Mai W, Li M, Hu Y. 2016. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 355:i5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM; Diabetes Prevention Program Research Group. 2002. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalla E, Cheng B, Kunzel C, Burkett S, Ferraro A, Lamster IB. 2015. Six-month outcomes in dental patients identified with hyperglycaemia: a randomized clinical trial. J Clin Periodontol. 42(3):228–235. [DOI] [PubMed] [Google Scholar]
- Lalla E, Kunzel C, Burkett S, Cheng B, Lamster IB. 2011. Identification of unrecognized diabetes and pre-diabetes in a dental setting. J Dent Res. 90(7):855–860. [DOI] [PubMed] [Google Scholar]
- Myers-Wright N, Lamster IB, Jasek JP, Chamany S. 2018. Evaluation of medical and dental visits in new york city: opportunities to identify persons with and at risk for diabetes mellitus in dental settings. Community Dent Oral Epidemiol. 46(1):102–108. [DOI] [PubMed] [Google Scholar]
- Poltavskiy E, Kim DJ, Bang H. 2016. Comparison of screening scores for diabetes and prediabetes. Diabetes Res Clin Pract. 118:146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche MM, Wang PP. 2014. Factors associated with a diabetes diagnosis and late diabetes diagnosis for males and females. J Clin Transl Endocrinol. 1(3):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. 2008. 2008 physical activity guidelines for Americans. Rockville (MD): US Department of Health and Human Services; [accessed 2018]. https://health.gov/paguidelines/pdf/paguide.pdf. [Google Scholar]
- US Department of Health and Human Services. 2018. National Health and Nutrition Examination Survey: estimation procedures, 2011–2014. Vital Health Stat 2 (177):1–26. [PubMed] [Google Scholar]