Abstract
HIV-status disclosure may improve psychosocial health and adherence to antiretroviral therapy (ART), but existing insights suffer from methodological limitations. We explored disclosure over time during pregnancy and postpartum among 1347 HIV-positive women in Cape Town. Among 995 women diagnosed HIV-positive before the pregnancy and entering antenatal care (median age: 30 years), 95% had disclosed to ≥1 individual. In Mokken scale analysis, we observed two separate dimensions of disclosure: disclosure to a male partner, and disclosure to family/community members. Among 352 women diagnosed during the pregnancy and initiating ART (median age: 27 years), 61% disclosed to a male partner and 71% to a family/community member by 12 months after diagnosis. Relationship status modified the impact of pregnancy intentions and poverty on disclosure to a male partner. These unique data provide important insights into dimensions of disclosure during pregnancy and postpartum, and suggest that women’s social and economic circumstances are central determinants of disclosure.
Keywords: Disclosure, HIV, pregnancy, Mokken scale analysis, South Africa
Introduction
HIV-status disclosure may have beneficial effects on both psychosocial health and adherence to antiretroviral therapy (ART) among HIV-positive individuals. As a means of accessing social support from family and community networks, disclosure may improve psychological well-being [1] and facilitate the development of effective coping strategies [2]. Non-disclosure has been identified as a barrier to antiretroviral adherence in studies of adults living with HIV [3] and specifically among women in prevention of mother-to-child transmission (PMTCT) programmes [4–6]. This association may be explained by attempts to hide antiretroviral usage so as not to inadvertently disclose, as well as individuals not receiving support for adherence. Given the potential benefits, disclosure is widely encouraged in counselling services for people living with HIV. Despite widespread fears around disclosing [7–9], documented reactions to disclosure are generally positive, with some evidence linking disclosure to sexual risk reduction in sexual partnerships and the ability to seek care openly, although some individuals do experience negative reactions such as anger or rejection [10,11]. Most HIV-positive individuals typically report having disclosed to at least one person [7,12–14], although selective disclosure appears to be the norm, with levels of disclosure to different individuals differing markedly [12].
Disclosure has been described as a process of revealing one’s HIV status to an increasing number of individuals over time [12]. This process includes a feedback loop where the individual’s positive or negative response to the disclosure event results in greater openness and additional future disclosure events or greater concealment, respectively [1]. Inherent in this model is the effect that one disclosure event can have on subsequent disclosure trajectories. A limitation of much disclosure research to date is the reliance on cross-sectional data to evaluate what is inherently a process that occurs over time [1]. A further limitation is the commonly used approach of operationalising disclosure as any versus no disclosure, or using sum scores to indicate the total number of persons to whom an individual has disclosed [15]. These approaches treat disclosure to different individuals as interchangeable events. Rather, it has been argued that disclosure should be conceptualised as a multi-dimensional process consisting of clusters of disclosure events to different individuals, given that disclosure events are neither interchangeable nor independent [15,16]. Based on this idea, two recent studies have sought to extend the methodology of disclosure research using psychometric data reduction techniques in general adult HIV-positive populations [15,16].
Less attention has been paid to the methodology of disclosure research among HIV-positive pregnant and postpartum women. In terms of disclosure, HIV-positive pregnant women differ from non-pregnant adults in important ways: in South Africa and other high-burden settings, women typically test HIV-positive in the context of antenatal care when they may feel healthy, rather than through voluntary counselling and testing or provider-initiated testing in other contexts. In many low- and middle-income country settings, women may be economically dependent on their male partner, with their economic vulnerability heightened by pregnancy and having implications for disclosure to their male partner [17]. Further, they may be at heightened risk of mental health problems such as depression, particularly in low- and middle-income country settings [18,19], and may consequently require a greater degree of support. Among HIV-positive pregnant women, levels of disclosure to male partners may be particularly low [20–23], especially among women diagnosed in the context of antenatal care [12,13,24,25]. A widely reported predictor of disclosure to a male partner is stable relationship status [7,20,23,26], but there are few considerations of how factors such as relationship status may modify other determinants of disclosure.
Given methodological limitations in operationalising disclosure and the dearth of longitudinal data, high-quality evidence is lacking, and interventions and counselling messaging are based on data with substantial limitations. To address this gap, we explored patterns and predictors of HIV-status disclosure among HIV-positive pregnant women in Cape Town, South Africa. Our objectives were to explore patterns and predictors of disclosure among three analytic populations, each using different analyses: (i) women diagnosed HIV-positive before the pregnancy and entering antenatal care, using cross-sectional analyses and incorporating psychometric data reduction techniques previously used in a study of HIV-positive adults [15], with (ii) descriptive longitudinal analyses in a subset who were followed through pregnancy and postpartum; and (iii) women diagnosed HIV-positive during the pregnancy and followed through pregnancy and postpartum, using longitudinal analyses.
Methods
Study design
These secondary analyses draw on the MCH-ART study, a multi-phase implementation science study evaluating strategies for providing HIV care and treatment services in Cape Town (ClinicalTrials.gov NCT01933477). The design and methods of the study have been previously described [27]. The study was conducted at one antenatal care clinic in the former township of Gugulethu, where an antenatal HIV prevalence of ~30% has been documented [28]. In this setting, ART eligibility was determined based on CD4 cell count or clinical disease staging until June 2013; from July 2013 onward, all HIV-positive pregnant women were eligible to initiate lifelong ART under Option B+ guidelines [29].
Participants
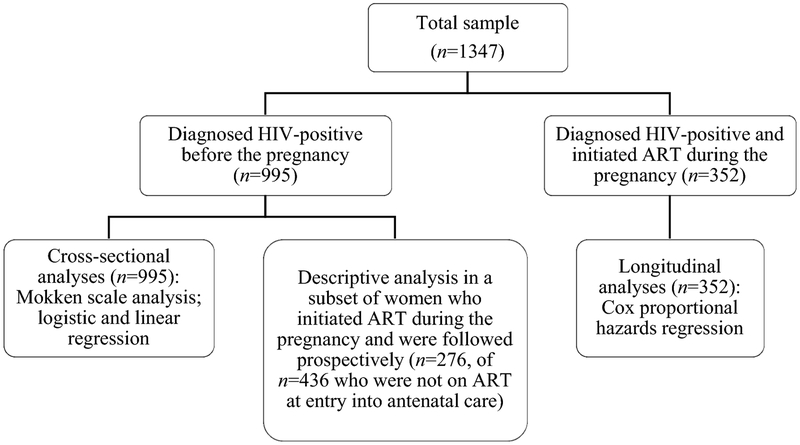
For the broader MCH-ART study, consecutive HIV-positive women who were 18 years or older and were entering antenatal care were recruited and enrolled in a cross-sectional evaluation; women who were initiating ART were followed until their first postpartum clinic visit at up to 3 study visits, with follow-up at up to 6 additional study visits through 12 months postpartum among women who chose to breastfeed [27]. For the purposes of the current analyses, we used different analytic methods across three analytic populations: (i) a cross-sectional analysis of disclosure reported at entry into antenatal care among all women who were known HIV-positive before the pregnancy; (ii) a descriptive analysis of longitudinal data through 12 months postpartum among women who were known HIV-positive and who were initiating ART and followed as part of the broader study; and (iii) an analysis of longitudinal data through 12 months postpartum among women who were diagnosed HIV-positive during the pregnancy and who were initiating ART and followed as part of the broader study (see Figure 1 for an overview of the analytic populations and methods used). All women provided written informed consent prior to enrolment, and the study was approved by the University of Cape Town’s Faculty of Health Sciences Human Research Ethics Committee and by Columbia University Medical Center’s Institutional Review Board in New York.
Figure 1.
Analytic populations and methods used1
1 ART: antiretroviral therapy.
Study measures
Study measures were administered in isiXhosa, the predominant local language, by trained interviewers at study visits separate from routine HIV or antenatal/postpartum care. All measures were translated from English into isiXhosa and were back-translated to ensure accuracy using standard procedures for translation and back-translation [30]. Basic sociodemographic characteristics were assessed, and included age, educational attainment and relationship status. Pregnancy intentions were assessed by asking women whether or not they were trying to have a baby when they found out that they were pregnant. A composite poverty score was calculated based on current employment, housing type and access to household assets in order to categorise participants according to relative levels of disadvantage, as previously described [31]. Women self-reported their date of HIV diagnosis, and this was used to calculate the time between diagnosis and entry into antenatal care and to categorise women according to the timing of diagnosis (before versus during the pregnancy). Gestation was assessed using ultrasound.
Although HIV-status disclosure may be involuntary, for example if someone else reveals the individual’s HIV-status without his/her permission, only voluntary disclosure was assessed in the broader study, thus we use the term “disclosure” in the present article to refer only to voluntary disclosure. At entry into antenatal care, disclosure was assessed by asking women whether or not they had told anyone that they are HIV-positive, and then by asking whether or not they had disclosed to each of 18 possible categories: male partner; mother; father; sister; brother; daughter; son; uncle; aunt; male cousin; female cousin; other male family member; other female family member; other sexual partner; friend; spiritual leader; current or former employer; and the broader public/community. This list was developed for the purposes of this study, and disclosure to each category was assessed using response options of ‘Yes’, ‘No’, or ‘Not Applicable’. At each subsequent visit, women were asked whether they had disclosed to anyone new since their last visit, with disclosure to the same 18 possible categories assessed. Given the exploratory nature of these analyses, we combined the response options ‘No’ and ‘Not Applicable’ in analyses, and excluded disclosure to certain categories given that disclosure to these categories was infrequently reported: daughter (reported by 9% of women who were diagnosed HIV-positive before the pregnancy), son (6%), employer (4%), other sexual partner (3%) and the public/community (1%).
Data analysis
Data were analysed using Stata 12 (StataCorp Inc, College Station, Texas, USA) and R (R Foundation for Statistical Computing, Austria). Baseline characteristics were summarised using frequencies and percentages for categorical variables and medians and inter-quartile ranges [IQR] for non-normally distributed variables.
Cross-sectional analyses
Among women diagnosed before the pregnancy, we examined the dimensionality of disclosure using Mokken scale analysis, a form of non-parametric item response theory, based on the approach used by Dima et al. [15] The Mokken scale model implies an ordinal scale for observable scores (here, the number of categories of individuals disclosed to), allowing an ordering of HIV-positive individuals in terms of the number of categories to whom they report having disclosed [32,33]. A special case of the model is the double monotonicity model which additionally allows for an ordering of items that have invariant item ordering [33]. Here, this would imply that the order in which individuals disclose to different categories does not differ across individuals [34].
Using the mokken package in R and the approach recommended by Sijtsma & van der Ark [33], we ran an automated item selection procedure (aisp) algorithm 12 times consecutively at increasing values of c (c=0 to c=0.55), where c is a chosen positive coefficient representing the threshold of homogeneity above which an item is included in the scale. We calculated item (Hj, representing how well each item discriminates between individuals’ overall disclosure) and total scale (H, representing the accuracy with which items within the total scale are able to order individuals with respect to overall disclosure) scalability coefficients and standard errors; checked scale assumptions; and examined the possibility of invariant item ordering to assess whether or not women disclosed to different categories in the same order. Following this exploratory analysis and based on these results, we examined factors independently associated with disclosure to a male partner and to the sum of family/community categories (which we refer to as the family/community subscale) in logistic and linear regression models, respectively. As we did not assess the exact number of family/community members to whom women have disclosed (as women may have disclosed to, for example, more than one friend), we used the sum of categories as a proxy for overall disclosure. Finally, we explored factors independently associated with report of any versus no disclosure in logistic regression models in order to serve as a comparison against these more nuanced disclosure analyses. Throughout, we adjusted for sociodemographic characteristics, ART use and time since HIV diagnosis.
Longitudinal analyses
Using longitudinal data, we explored the time to first report of disclosure to a male partner and to family/community categories. Where participants reported a new disclosure event at a study visit, we used the midpoint between that and the previous study visit as a proxy for the date of disclosure. Using these data, we then explored the time to first disclosure among previously-diagnosed women who had not disclosed at entry into antenatal care and who initiated ART and were followed prospectively. Similarly, we explored the time to first disclosure among women who were diagnosed during the pregnancy and who initiated ART and were followed prospectively, and used product-limit methods and Cox proportional hazards models to explore variables associated with disclosure to a male partner and to one or more family/community categories. We examined how relationship status may modify the predictors of disclosure to a male partner in stratified analyses by comparing (i) women who were married and/or cohabiting and (ii) women who were neither married nor cohabiting. This latter group included a small number of women who reported that they were not in a relationship.
Results
Sociodemographic and clinical characteristics
These analyses include data from 1347 HIV-positive pregnant women. A total of 995 pregnant women who were known HIV-positive at entry into antenatal care (median age: 30.5 years) were included in the cross-sectional component, with 276 women who initiated ART during pregnancy and who were followed prospectively included in longitudinal analyses. Longitudinal analyses were also conducted among 352 women who were diagnosed HIV-positive during the pregnancy and initiated ART (median age: 26.9 years). All participants were enrolled between March 2013 and June 2014, and characteristics measured at enrolment are described in Table 1. Low levels of educational attainment, employment, and married and/or cohabiting relationship status and high levels of unintended pregnancy were observed in both groups. Among women diagnosed before pregnancy, the median time since HIV diagnosis was 4.2 years.
Table 1.
Participant characteristics at entry into antenatal care by timing of HIV diagnosis
| Variable | Diagnosed before pregnancy – total sample; n (%) |
Diagnosed before pregnancy – on ART; n (%)1 |
Diagnosed before pregnancy – not on ART; n (%) |
Diagnosed during pregnancy – n (%) |
|---|---|---|---|---|
| Number of women | 995 | 559 | 436 | 352 |
| Median [IQR] maternal age | 30.5 [26.9, 34.2] | 31.5 [27.9, 34.9] | 29.4 [26.0, 32.9] | 26.9 [23.5, 31.6] |
| Completed secondary/any tertiary education | 233 (23) | 125 (22) | 108 (25) | 109 (31) |
| Currently employed | 353 (35) | 212 (38) | 141 (32) | 146 (41) |
| Poverty categories | ||||
| Least disadvantaged | 299 (30) | 164 (29) | 135 (31) | 112 (32) |
| Moderate disadvantage | 329 (33) | 191 (34) | 138 (32) | 116 (33) |
| Most disadvantaged | 367 (37) | 204 (36) | 163 (37) | 124 (35) |
| Married and/or cohabiting | 478 (48) | 271 (48) | 207 (47) | 130 (37) |
| First pregnancy | 88 (9) | 58 (10) | 30 (7) | 95 (27) |
| Pregnancy unintended | 603 (61) | 313 (56) | 290 (67) | 245 (70) |
| Median [IQR] gestation in weeks | 20 [14, 27] | 19 [14, 26] | 20 [14, 26] | 21 [16, 27] |
| Median [IQR] years since diagnosis | 4.2 [2.3, 6.8] | 4.6 [2.9, 7.4] | 3.7 [1.9, 5.9] | - |
| On ART | 559 (56) | 559 (100) | 0 (0) | 0 (0) |
ART: antiretroviral therapy
Reported disclosure at entry into antenatal care among women diagnosed before pregnancy
Among women diagnosed before the pregnancy (n=995, with n=559 on ART at entry into antenatal care), 95% had disclosed to at least one individual, with disclosure to one or more individuals (versus disclosure to none) significantly associated with being on ART at entry into antenatal care (p<0.001) and longer time since HIV diagnosis (p=0.001). No other factors were associated with disclosure to one or more versus no individuals. Disclosure to different categories ranged from 77% of women having disclosed to their male partner, to 9% having disclosed to a spiritual leader; across all categories, disclosure was significantly more common among women who were already on ART when entering antenatal care (Table 2).
Table 2.
Proportion of women reporting having disclosed to different individuals at entry into antenatal care and scalability coefficients (Hj) with standard errors (SE) for the family/community subscale from Mokken scale analysis among 995 women diagnosed HIV-positive before pregnancy
| Proportion of women reporting having disclosed |
||||
|---|---|---|---|---|
| Total sample; n (%) | On ART; n (%)1 | Not on ART; n (%) | Hj (SE) | |
| Male partner | 771 (77) | 476 (85) | 295 (68) | - |
| Sister | 605 (61) | 399 (71) | 206 (47) | 0.44 (0.03) |
| Friend | 518 (52) | 359 (64) | 159 (36) | 0.39 (0.03) |
| Mother | 471 (47) | 303 (54) | 168 (39) | 0.39 (0.03) |
| Female cousin | 373 (37) | 256 (46) | 117 (27) | 0.54 (0.02) |
| Brother | 372 (37) | 266 (48) | 106 (24) | 0.46 (0.02) |
| Other female family member | 271 (27) | 199 (36) | 72 (17) | 0.57 (0.02) |
| Male cousin | 230 (23) | 170 (30) | 60 (14) | 0.61 (0.02) |
| Aunt | 221 (22) | 154 (28) | 67 (15) | 0.54 (0.02) |
| Uncle | 175 (18) | 131 (23) | 44 (10) | 0.59 (0.02) |
| Father | 164 (16) | 114 (20) | 50 (11) | 0.38 (0.03) |
| Other male family member | 159 (16) | 125 (22) | 34 (8) | 0.62 (0.02) |
| Spiritual leader | 89 (9) | 63 (11) | 26 (6) | 0.45 (0.04) |
ART: antiretroviral therapy
Using Mokken scale analysis, we found that disclosure to a male partner formed a separate single-item dimension, while all 12 remaining categories formed one scale. This suggests that the decision to disclose to a male partner in this sample is independent of decisions to disclose to family/community members, with disclosure to family/community categories occurring as related events. Scalability coefficients and standard errors for the 12-item family/community subscale are presented in Table 2. For this subscale, H=0.5 (standard error: 0.02), suggesting that these items form a medium-strong scale [35]. The items father, female cousin and other female family member showed signs of violating invariant item ordering, suggesting that these categories are not disclosed to at the same point in the typical order of disclosure events by all women. After exclusion of these categories, the remaining 9 items met criteria for invariant item ordering, suggesting that in this sample women tended to disclose to particular categories in the following order: a sister, friend, mother, brother, male cousin, aunt, uncle, other male family member and, lastly, a spiritual leader. This implies that women who had disclosed to, for example, their brother were likely to have also disclosed to their mother, friend and sister. This smaller scale showed medium accuracy in terms of invariant item ordering (HT=0.42) and high reliability (Molenaar-Sijtsma coefficient=0.82) [35,36].
Factors associated with disclosure at entry into antenatal care among women diagnosed before pregnancy
Table 3 presents factors associated with disclosure to a male partner, as well as factors associated with the number of categories in the family/community subscale to whom women had disclosed at entry into antenatal care among women diagnosed before the pregnancy. After adjustment for age and time since diagnosis, disclosure to a male partner was strongly associated with being in a married and/or cohabiting relationship [adjusted odds ratio (aOR): 2.51; 95% confidence interval (CI): 1.81, 3.48] and with being on ART at entry into antenatal care (aOR: 2.98; 95% CI: 2.15, 4.11), and was more common among women who had completed secondary or any tertiary education (aOR: 1.59; 95% CI: 1.08, 2.34); no association was observed between length of time since HIV diagnosis and disclosure to a male partner.
Table 3.
Factors associated with disclosure to a male partner and with the number of family/community categories to whom women report having disclosed at entry into antenatal care among 995 women diagnosed HIV-positive before pregnancy
| Disclosure to a male partner | Number of family/community categories | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Unadjusted OR [95% CI]1 |
P-value | Adjusted OR [95% CI]2 |
P-value | Unadjusted β [95% CI]3 |
P-value | Adjusted β [95% CI]2 |
P-value |
| Maternal age | 1.00 [0.97, 1.03] | 0.791 | 0.97 [0.94, 1.00] | 0.079 | 0.06 [0.02, 0.10] | 0.003 | 0.01 [−0.04, 0.05] | 0.793 |
| Education | ||||||||
| Primary/some secondary | Reference | Reference | Reference | |||||
| Secondary/tertiary | 1.38 [0.95, 1.99] | 0.091 | 1.59 [1.08, 2.34] | 0.018 | −0.28 [−0.75, 0.18] | 0.236 | ||
| Employment | ||||||||
| Unemployed | Reference | Reference | Reference | |||||
| Employed | 1.12 [0.82, 1.53] | 0.478 | −0.45 [−0.87, −0.03] | 0.031 | −0.65 [−1.03, −0.27] | 0.001 | ||
| Poverty categories | ||||||||
| Least disadvantaged | Reference | Reference | ||||||
| Moderate disadvantage | 0.83 [0.57, 1.21] | 0.340 | −0.21 [−0.71, 0.29] | 0.404 | ||||
| Most disadvantaged | 0.99 [0.68, 1.44] | 0.970 | −0.14 [−0.63, 0.34] | 0.562 | ||||
| Relationship status | ||||||||
| Neither married nor cohabiting | Reference | Reference | Reference | Reference | ||||
| Married and/or cohabiting | 2.29 [1.67, 3.13] | <0.001 | 2.51 [1.81, 3.48] | <0.001 | −0.89 [−1.28, −0.50] | <0.001 | −0.95 [−1.31, −0.59] | <0.001 |
| Previous pregnancies | ||||||||
| First pregnancy | Reference | Reference | Reference | |||||
| One or more previous pregnancies | 0.81 [0.47, 1.41] | 0.453 | −0.74 [−1.43, −0.05] | 0.037 | −0.76 [−1.43, −0.09] | 0.027 | ||
| Antiretroviral therapy (ART) use | ||||||||
| Not on ART | Reference | Reference | Reference | Reference | ||||
| On ART | 2.74 [2.02, 3.73] | <0.001 | 2.98 [2.15, 4.11] | <0.001 | 2.00 [1.62, 3.48] | <0.001 | 1.75 [1.38, 2.12] | <0.001 |
| Years since diagnosis | 1.03 [0.98, 1.07] | 0.249 | 1.01 [0.96, 1.07] | 0.585 | 0.27 [0.21, 0.32] | <0.001 | 0.24 [0.18, 0.30] | <0.001 |
OR: odds ratio; 95% CI: 95% confidence interval;
Adjusted models are adjusted for covariates shown;
β: regression coefficient
As disclosure to family/community categories meets the criteria for a Mokken scale in this sample, sum scores represent a meaningful indicator of disclosure to family/community categories, and allow an ordering of individual women with regard to the number of family/community categories to whom they had disclosed. Women had disclosed to a median of 3 categories (IQR: 1–5) in this subscale. In a multivariable model adjusted for age, the number of categories to whom women had disclosed was lower among women who were in a married and/or cohabiting relationship [regression coefficient (β): −0.95; 95% CI: −1.31, −0.59]. This finding did not differ according to whether or not women had disclosed to their male partner. Other determinants of disclosure to a higher number of family/community categories were being on ART at entry into antenatal care (β: 1.75; 95% CI: 1.38, 2.12) and a longer time since HIV diagnosis (β for a one-year increase in time since diagnosis: 0.24; 95% CI: 0.18, 0.30). Women who were employed or who reported one or more previous pregnancies had disclosed to fewer family/community categories (β: −0.65; 95% CI: −1.03, −0.27; and β: −0.76; 95% CI: −1.43, −0.09, respectively).
Disclosure over time among women diagnosed before pregnancy
In a subset of 276 women who were diagnosed before the pregnancy but initiated ART during the pregnancy and were followed prospectively, new disclosure events appeared uncommon. Of the 98 women who had not disclosed to their male partner at entry into antenatal care and were followed prospectively, only 25% had disclosed by 12 months after enrolment into the study. Similarly, new disclosure events to family/community categories ranged from 2% of women who had not disclosed at entry into antenatal care disclosing to their father by 12 months after enrolment, to 20% disclosing to a friend.
Disclosure over time among women diagnosed during pregnancy
The group of 352 women who were diagnosed during the pregnancy and initiated ART were followed for a median of 14.4 months (IQR: 6.1–16.5) from diagnosis. By 12 months after diagnosis, 86% had disclosed to at least one individual. During this time, 61% disclosed to a male partner, and 71% to one or more categories in the family/community subscale, with the frequency of disclosure to each family/community category similar to that observed among women diagnosed before pregnancy. Time to first disclosure events was short: 50% and 53% of women disclosed to their male partner and to a family/community member within 30 days of diagnosis, respectively; with women disclosing to a median of 1 (IQR: 0–2) family/community category over follow-up.
Predictors of disclosure over time among women diagnosed during pregnancy
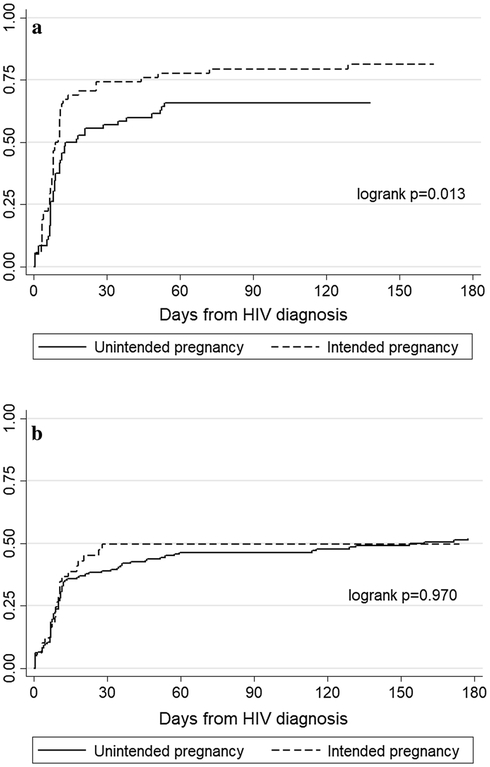
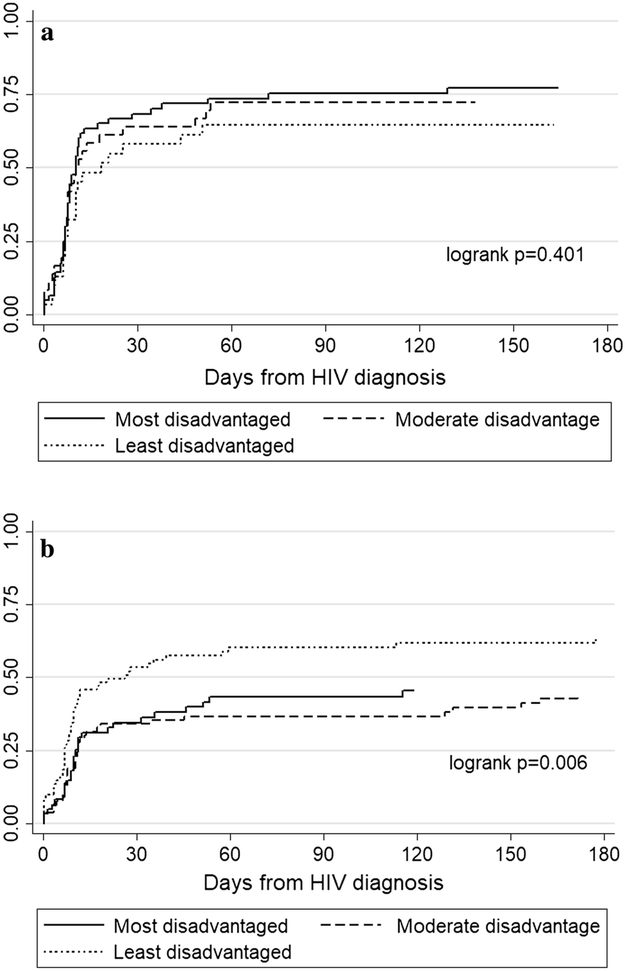
In unadjusted analyses, disclosure to a male partner was strongly associated with married and/or cohabiting relationship status [hazard ratio (HR): 1.80; 95% CI: 1.37, 2.36] and was more common among women who reported that their pregnancy was intended (HR: 1.45; 95% CI: 1.10, 1.93). In a multivariable Cox proportional hazards model adjusted for poverty, these associations persisted, and disclosing to a male partner was less likely with increasing age [adjusted hazard ratio (aHR) for a one-year increase in age: 0.97; 95% CI: 0.95, 1.00]. Marked differences in the predictors of disclosure to a male partner were observed when stratified by relationship status: among women in married and/or cohabiting relationships, intended pregnancy remained significantly associated with disclosure (aHR: 1.61; 95% CI: 1.07–2.42) after adjustment for age, education, poverty and number of previous pregnancies, but this association was not observed among women who were neither married nor cohabiting (Figures 2a and 2b; Table 4). Among this latter group, disclosure to a male partner was less common among those reporting higher levels of poverty (aHR for moderate disadvantage and most disadvantaged, compared to least disadvantaged: 0.57; 95% CI: 0.37, 0.88; and 0.60; 95% CI: 0.38, 0.97, respectively), independent of age, educational attainment, pregnancy intention and number of previous pregnancies (Figures 3a and 3b; Table 4).
Figure 2a.
Impact of pregnancy intention on occurrence of disclosure to a male partner among women diagnosed HIV-positive during pregnancy and married and/or cohabiting
2b Impact of pregnancy intention on occurrence of disclosure to a male partner among women diagnosed HIV-positive during pregnancy and neither married nor cohabiting
Table 4.
Impact of relationship status on the predictors of disclosure to a male partner among 352 women diagnosed HIV-positive during pregnancy
| Married and/or cohabiting | Neither married nor cohabiting | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Unadjusted HR [95% CI]1 |
P-value | Adjusted HR [95% CI]2 |
P-value | Unadjusted HR [95% CI] |
P-value | Adjusted HR [95% CI]2 |
P-value |
| Maternal age | 0.99 [0.95, 1.03] | 0.590 | 1.00 [0.96, 1.05] | 0.835 | 0.97 [0.93, 1.00] | 0.048 | 0.95 [0.91, 0.99] | 0.024 |
| Education | ||||||||
| Primary/some secondary | Reference | Reference | Reference | Reference | ||||
| Secondary/tertiary | 0.93 [0.59, 1.47] | 0.766 | 0.94 [0.58, 1.52] | 0.802 | 1.52 [1.05, 2.19] | 0.028 | 1.44 [0.98, 2.12] | 0.062 |
| Employment | ||||||||
| Unemployed | Reference | Reference | ||||||
| Employed | 0.71 [0.46, 1.09] | 0.118 | 1.03 [0.71, 1.48] | 0.886 | ||||
| Poverty categories | ||||||||
| Least disadvantaged | Reference | Reference | Reference | Reference | ||||
| Moderate disadvantage | 1.36 [0.77, 2.42] | 0.290 | 1.54 [0.85, 2.80] | 0.156 | 0.55 [0.36, 0.84] | 0.006 | 0.57 [0.37, 0.88] | 0.011 |
| Most disadvantaged | 1.41 [0.83, 2.37] | 0.200 | 1.46 [0.83, 2.56] | 0.189 | 0.57 [0.36, 0.90] | 0.016 | 0.60 [0.38, 0.97] | 0.035 |
| Pregnancy intention | ||||||||
| Unintended | Reference | Reference | Reference | Reference | ||||
| Intended | 1.64 [1.10, 2.45] | 0.016 | 1.61 [1.07, 2.42] | 0.022 | 1.01 [0.65, 1.57] | 0.970 | 1.02 [0.65, 1.60] | 0.946 |
| Previous pregnancies | ||||||||
| First pregnancy | Reference | Reference | Reference | Reference | ||||
| One or more previous pregnancies | 0.52 [0.31, 0.86] | 0.012 | 0.51 [0.29, 0.90] | 0.020 | 0.89 [0.61, 1.30] | 0.531 | 1.29 [0.81, 2.05] | 0.276 |
HR: hazard ratio; 95% CI: 95% confidence interval;
Adjusted models are adjusted for covariates shown
Figure 3a.
Impact of poverty on occurrence of disclosure to a male partner among women diagnosed HIV-positive during pregnancy and married and/or cohabiting
3b Impact of poverty on occurrence of disclosure to a male partner among women diagnosed HIV-positive during pregnancy and neither married nor cohabiting
Compared to women who were neither married nor cohabiting, women who were married and/or cohabiting were less likely to disclose to a family/community member over time (HR: 0.62; 95% CI: 0.47, 0.82). This association persisted after adjustment for age and poverty (aHR: 0.62; 95% CI: 0.47, 0.83); no other predictors of disclosure to family/community categories were observed.
Discussion
This research explored patterns and predictors of disclosure among HIV-positive pregnant women in South Africa. In the group of women diagnosed before the pregnancy, which included both women on ART and women initiating ART during the pregnancy, disclosure appeared to consist of two separate dimensions: disclosure to a male partner, and disclosure to family/community members, with disclosure to family/community categories tending to occur in a particular order. Among women diagnosed during the pregnancy and initiating ART, initial disclosure occurred rapidly but women appeared to favour selective rather than widespread disclosure. Across both groups of women, relationship status was observed to be a central determinant of disclosure, with women who were married and/or cohabiting more likely to disclose to a male partner but less likely to disclose to family/community categories. In addition, relationship status modified the predictors of disclosure to a male partner among women diagnosed during the pregnancy.
Extensions to the literature
This study design and measurements allowed for both cross-sectional and longitudinal insights into a process that inherently occurs over time. Most disclosure research to date has relied solely on cross-sectional data [1], and our longitudinal work notably extends the existing literature. Among women diagnosed before the pregnancy, we showed that time since diagnosis was associated with disclosure to more family/community categories, but not with disclosure to a male partner. This suggests that women who disclose to their male partner do so quickly, and is consistent with results among newly-diagnosed women: in this group, initial disclosure to male partners and to family/community categories occurred rapidly, as has been observed in a general adult population in South Africa [20].
A further advance introduced by this study is that most research to date operationalises disclosure as any versus no disclosure. Here, we demonstrated in the group of women diagnosed before the pregnancy that operationalising disclosure in this way blurs the predictors of disclosure. Using a novel analytic technique, we showed that disclosure is not a unidimensional process in this sample. Consistent with Dima et al.’s findings [15], we observed that disclosure to a spouse/partner occurs as an independent event. In contrast to their finding of additional disclosure dimensions consisting separately of (i) close family members and (ii) other relatives and the larger community among HIV-positive adults in Tanzania [15], we observed that all family and community categories assessed formed one disclosure subscale. In the present study, we assessed disclosure to individual relatives rather than a single category of ‘other relatives’, which may have contributed to the differences observed. The single observed scale of disclosure events to family and community categories in the present study may also be due to isiXhosa culture, in which distant or extended family members are often seen to be as close as immediate family members, and nuclear families are relatively uncommon [37]. The order in which women tended to disclose to family/community categories in this sample may reflect the availability of different individuals to provide support, or may be reflective of social distance, again noting that the closeness of family members according to familial relationship may differ in this setting compared to Western settings.
Importance of social and economic circumstances
The finding that married and/or cohabiting relationship status is a central determinant of disclosure to a male partner is well documented [7,20,23,26]. Here, we additionally observed that married and/or cohabiting relationship status is associated with less disclosure to family/community members. We hypothesise that women in married and/or cohabiting relationships may receive a greater degree of support from their male partner, and consequently may experience less need to disclose to other individuals, or that partners may restrict a woman’s choice to disclose to family/community members. This finding has important implications for counselling: disclosure is highly dependent on women’s social circumstances, and these circumstances need to be taken into account in counselling messages. Conversations about disclosure need to consider the specific life experiences of individual women, as well as individual women’s experiences of disclosure.
Further, we observed relationship status to be a modifier of the predictors of male partner disclosure among newly-diagnosed women, again highlighting the importance of context. Compared to women who were married and/or cohabiting, women who were neither married nor cohabiting were significantly less likely to disclose to their male partner, and the intendedness of the pregnancy did not change the likelihood of disclosure in this group. We hypothesise that an unintended pregnancy, which is typically associated with negative outcomes, may have no impact on disclosure when a relationship is already relatively unstable. Previous research in South Africa has suggested that pregnant women’s disclosure to their male partner may be subordinated to concerns over maintaining the relationship and receiving continued support [17]. Here, we found that higher levels of poverty were associated with a lower likelihood of disclosure to a male partner among women who were neither married nor cohabiting, suggesting that women who are in less stable relationships and may be economically dependent on their male partner face heightened vulnerability and may be less likely to disclose. Along these lines, qualitative research in Uganda has highlighted the fear of loss of material and financial support as a key barrier to disclosure to male partners among women who test HIV-positive during antenatal care [38]. Among previously-diagnosed women, the finding that women who had attained higher levels of education were more likely to disclose to their male partner may similarly be explained by higher levels of dependence on their partner among women with lower educational attainment.
Disclosure during pregnancy and postpartum
These data are among the first to explore prospective reports of disclosure among pregnant and postpartum women, a highly vulnerable population. Among women diagnosed during pregnancy, we observed rapid disclosure to both male partners and family/community members, with levels of disclosure broadly similar by 12 months postpartum to levels among women diagnosed before the pregnancy. Although diagnosed during routine HIV testing in the context of antenatal care and clearly influenced by economic and social vulnerabilities, levels of disclosure among newly-diagnosed women were high. However, a better understanding of the differences in disclosure between pregnant and non-pregnant populations is needed, and these findings should be generalised to non-pregnant populations with caution. Further, these findings should be contextualised as arising during a particular period in the HIV epidemic: with dramatically increasing numbers of pregnant women initiating ART, it is possible that HIV and ART have become more normalized over time in this setting, with implications for disclosure. Finally, further study of the impact of disclosure during pregnancy and postpartum is warranted, and longitudinal data are needed to provide high-quality evidence.
Strengths and limitations
A strength of the present study is the inclusion of both cross-sectional and longitudinal data, given the inherent nature of disclosure and the dearth of similar data in the literature, as well as the use of a novel analytic technique to advance understandings of disclosure. In addition, the inclusion of a large sample of HIV-positive women attending primary care increases the generalizability of these findings to other communities of pregnant and postpartum women in the region. A limitation of this analysis is the self-reported nature of these data, given concerns around recall and social desirability bias, although this is common to all disclosure research. Further, we used the first report of disclosure to family/community members in longitudinal analyses, and did not assess the exact number of individuals to whom women have disclosed within categories, thus sum scores in the family/community subscale are only proxies for the total number of disclosure events. Finally, we did not explore the impact of disclosure on HIV or health-related outcomes or on mental health in these analyses.
Conclusion
Despite some limitations, these results provide important insights into disclosure in this population. Our findings suggest that disclosure occurs rapidly after diagnosis but that levels of disclosure to different individuals differ widely, and that disclosure to male partners and family/community members form separate dimensions of disclosure events. Although we ultimately used sum scores as indicators of disclosure to family/community categories, we argue that researchers should first investigate the dimensionality of disclosure events in their data before proceeding with analyses rather than assuming that a rank ordering of individuals is meaningful [32]. Further high-quality evidence of the impact of disclosure on HIV and health-related outcomes is needed in order to inform counselling messaging and intervention efforts, and we argue that basing these on the current evidence base has limitations. Finally, we note here that women’s social and economic circumstances are central determinants of disclosure to both male partners and to family/community members, reflecting women’s vulnerability in this context. This suggests that counselling about disclosure needs to consider and be tailored to the broader social and economic circumstances of women’s lives, particularly in the case of pregnancy, and that counselling messaging must take into account this vulnerability.
Acknowledgements
The authors would like to thank the women who participated in this study, as well as the study staff for their support of this research. This research was supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the National Institute of Child Health and Human Development (NICHD), grant number 1R01HD074558. Additional funding comes from the Elizabeth Glaser Pediatric AIDS Foundation. Ms. Brittain is supported by the South African Medical Research Council under the National Health Scholars Programme. Drs. Mellins and Remien are supported by a grant from NIMH to the HIV Center for Clinical and Behavioral Studies (P30-MH45320).
Funding: This study was funded by NICHD under grant 1R01HD074558.
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical approval: This study was conducted in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments, and was approved by and conducted in accordance with the standards of the Faculty of Health Sciences Human Research Ethics Committee of the University of Cape Town as well as the Institutional Review Board of the Columbia University Medical Centre. Written informed consent was obtained from all individual participants included in the study.
References
- 1.Chaudoir SR, Fisher JD, Simoni JM. Understanding HIV disclosure: a review and application of the Disclosure Processes Model. Soc Sci Med. 2011; 72:1618–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medley AM, Kennedy CE, Lunyolo S, Sweat MD. Disclosure outcomes, coping strategies, and life changes among women living with HIV in Uganda. Qual Health Res. 2009; 19(12):1744–54. [DOI] [PubMed] [Google Scholar]
- 3.Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012; 26:2059–67. [DOI] [PubMed] [Google Scholar]
- 4.Gourlay A, Birdthistle I, Mburu G, Iorpenda K, Wringe A. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013; 16:18588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hodgson I, Plummer ML, Konopka SN, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One. 2014; 9(11):e111421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Hiarlaithe M, Grede N, de Pee S, Bloem M. Economic and social factors are some of the most common barriers preventing women from accessing maternal and newborn child health (MNCH) and prevention of mother-to-child transmission (PMTCT) services: a literature review. AIDS Behav. 2014; 18:S516–30. [DOI] [PubMed] [Google Scholar]
- 7.Makin JD, Forsyth DWC, Visser MJ, Sikkema KJ, Neufeld S, Jeffery B. Factors affecting disclosure in South African HIV-positive pregnant women. AIDS Patient Care STDS. 2008; 22(11):907–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007; 83:29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, Eisele TP. Disclosure of HIV status to sex partners among HIV-infected men and women in Cape Town, South Africa. AIDS Behav. 2012; 16:132–38. [DOI] [PubMed] [Google Scholar]
- 10.King R, Katuntu D, Lifshay J, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS Behav. 2008; 12:232–43. [DOI] [PubMed] [Google Scholar]
- 11.Atuyambe LM, Ssegujja E, Ssali S, et al. HIV/AIDS status disclosure increases support, behavioural change and, HIV prevention in the long term: a case for an urban clinic, Kampala, Uganda. BMC Health Serv Res. 2014; 14:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. 2011; 101(6):1011–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardon A, Vernooij E, Bongololo-Mbera G. Women’s views on consent, counselling and confidentiality in PMTCT: a mixed-methods study in four African countries. BMC Public Health. 2012; 12:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yonah G, Fredrick F, Leyna G. HIV serostatus disclosure among people living with HIV/AIDS in Mwanza, Tanzania. AIDS Res Ther. 2014; 11:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dima AL, Stutterheim SE, Lyimo R, de Bruin M. Advancing methodology in the study of HIV status disclosure: the importance of considering disclosure target and intent. Soc Sci Med. 2014; 108:166–74. [DOI] [PubMed] [Google Scholar]
- 16.Préau M, Beaulieu-Prévost D, Henry E, Bernier A, Veillette-Bourbeau L, Otis J. HIV serostatus disclosure: development and validation of indicators considering target and modality. Results from a community-based research in 5 countries. Soc Sci Med. 2015; 146:137–46. [DOI] [PubMed] [Google Scholar]
- 17.Crankshaw TL, Voce A, King RL, Giddy J, Sheon NM, Butler LM. Double disclosure bind: complexities of communicating an HIV diagnosis in the context of unintended pregnancy in Durban, South Africa. AIDS Behav. 2014; 18(Suppl 1):S53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker SP, Wachs TD, Meeks Gardner J, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007; 369(9556):145–57. [DOI] [PubMed] [Google Scholar]
- 19.Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011; 378(9799):1325–38. [DOI] [PubMed] [Google Scholar]
- 20.Abdool Karim Q, Dellar RC, Bearnot B, et al. HIV-positive status disclosure in patients in care in rural South Africa: implications for scaling up treatment and prevention interventions. AIDS Behav. 2015; 19:322–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Genet M, Sebsibie G, Gultie T. Disclosure of HIV seropositive status to sexual partners and its associated factors among patients attending antiretroviral treatment clinic follow up at Mekelle Hospital, Ethiopia: a cross sectional study. BMC Res Notes. 2015; 8:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hardon A, Gomez GB, Vernooij E, et al. Do support group members disclose less to their partners? The dynamics of HIV disclosure in four African countries. BMC Public Health. 2013; 13:589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Obiri-Yeboah D, Amoako-Sakyi D, Baidoo I, Adu-Oppong A, Rheinländer T. The ‘fears’ of disclosing HIV status to sexual partners: a mixed methods study in a counseling setting in Ghana. AIDS Behav. 2016; 20(1):126–36. [DOI] [PubMed] [Google Scholar]
- 24.Brou H, Djohan G, Becquet R, et al. When do HIV-infected women disclose their HIV status to their male partner and why? A study in a PMTCT programme, Abidjan. PLoS Med. 2007; 4(12):e342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. 2013; 13:433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel R, Ratner J, Gore-Felton C, Kadzirange G, Woelk G, Katzenstein D. HIV disclosure patterns, predictors, and psychosocial correlates among HIV positive women in Zimbabwe. AIDS Care. 2012; 24(3):358–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer L, Phillips TK, Zerbe A, et al. Optimizing antiretroviral therapy (ART) for maternal and child health (MCH): rationale and design of the MCH-ART study. J Acquir Immune Defic Syndr. 2016; 72:S189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myer L, Phillips TK, Hsiao N-Y, et al. Plasma viraemia in HIV-positive pregnant women entering antenatal care in South Africa. Journal Int AIDS Soc. 2015; 18:20045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Western Cape Government, 2013. PMTCT Clinical Guidelines Update, Cape Town, South Africa. Available at: https://www.westerncape.gov.za/assets/departments/health/wcp_2013_pmtct_clinical_guidelines_update_final_replacement_2.pdf. Accessed June 29, 2016.
- 30.Preciago J, Henry M. Linguistic barriers in health education and services In: Garcia JG, Zea MC, eds. Psychological interventions and research with Latino populations. Boston: Allyn and Bacon; 1997. [Google Scholar]
- 31.Brittain K, Mellins CA, Phillips T, et al. Social support, stigma and antenatal depression among HIV-infected pregnant women in South Africa. AIDS Behav. 2017; 21:274–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meijer RR, Baneke JJ. Analyzing psychopathology items: a case for nonparametric item response theory modeling. Psychol Methods. 2004; 9(3):354–68. [DOI] [PubMed] [Google Scholar]
- 33.Sijtsma K, van der Ark LA. A tutorial on how to do a Mokken scale analysis on your test and questionnaire data. Br J Math Stat Psychol. 2017; 70:137–58. [DOI] [PubMed] [Google Scholar]
- 34.Van Schuur WH. Mokken scale analysis: between the Guttman scale and parametric item response theory. Political Anal. 2003; 11:139–63. [Google Scholar]
- 35.Stochl J, Jones PB, Croudace TJ. Mokken scale analysis of mental health and well-being questionnaire item responses: a non-parametric IRT method in empirical research for applied health researchers. BMC Med Res Methodol. 2012; 12:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van der Ark LA. New developments in Mokken scale analysis in R. J Stat Softw. 2012; 48(5):1–27. [Google Scholar]
- 37.Department of Social Development, 2012. White paper on families in South Africa. Pretoria: Department of Social Development. Available from: http://www.dsd.gov.za/index.php?option=com_docman&task=cat_view&gid=33&Itemid=39. Accessed December 22, 2017.
- 38.Rujumba J, Neema S, Byamugisha R, Tylleskär T, Tumwine JK, Heggenhougen HK. “Telling my husband I have HIV is too heavy to come out of my mouth”: pregnant women’s disclosure experiences and support needs following antenatal HIV testing in eastern Uganda. J Int AIDS Soc. 2012; 15:17429. [DOI] [PMC free article] [PubMed] [Google Scholar]