Abstract
The aim of this study was to investigate the relationship between Type D personality and health behaviors of coronary artery disease patients and to determine the mediating effect of illness perception on this relationship. The participants were 142 coronary artery disease patients who underwent percutaneous coronary intervention in a university hospital in Korea. Type D personality, illness perception, and health behaviors were surveyed using structured questionnaires. The collected data were analyzed by a series of hierarchical multiple regressions. A total of 28.9 percent patients had Type D personality. Type D Patients were observed to have low illness perception and low health behaviors. There was a positive correlation between illness perception and health behaviors. The direct effect of Type D personality on health behaviors was significant (β = –.209, p = .013). However, the indirect effect of Type D personality on health behaviors via illness perception became low and non-significant (β = .007, p = .934). Based on the above results, it can be concluded that illness perception has a complete mediating effect on the relationship between Type D personality and health behaviors. The development of interventions that can improve illness perception is needed to improve health behaviors of Type D coronary artery disease patients.
Keywords: disease, health behaviors, perception, percutaneous coronary intervention, Type D personality
Introduction
The incidence and mortality rates of patients with coronary artery disease (CAD) are steadily increasing due to stress, sedentary lifestyle, and eating habits (Statistics Korea, 2013). Percutaneous coronary intervention (PCI) is considered to be the mainstay therapy for CAD because it accompanies less physical, mental, and economic burden than surgery and has a higher success rate of revascularization (Puymirat et al., 2017). However, even after successful PCI, several complications can occur. In particular, coronary artery restenosis is likely to occur within 6 months after the procedure (Piraino et al., 2017). Because PCI does not eliminate the cause of CAD, it should perform lifelong health behaviors such as hospital follow-ups, medication, dietary management, exercise, weight control, and stress management to prevent recurrence and complications (Throndson and Sawatzky, 2009).
There are various psychological factors such as depression, anxiety, stress, and social support that have been reported to affect health behaviors of patients with CAD (Steca et al., 2017). Among these, there is an increasing interest in the effect of Type D personality, which has been gradually formed with human growth and has not changed easily, on health behaviors and health outcomes of CAD patients (Mols et al., 2010; Williams et al., 2011b). The prevalence of Type D personality among patients with CAD is 20 to 33 percent, which is higher than that among the general population (Mols et al., 2010; Williams et al., 2011b). Type D personality is characterized by negative affectivity and social inhibition. Negative affectivity is a tendency to experience negative feelings regardless of time or situation. Social inhibition is the tendency to experience limitations in behavioral interactions and emotional expressions in interactions (Denollet, 2005).
People with Type D personality have been reported to have low performance of health behaviors such as smoking cessation, increase in physical activity, and dietary control (Pedersen and Denollet, 2003; Williams et al., 2008). According to a German study (Nefs et al., 2015), diabetic patients with Type D personality did not observe the prescribed healthy diets and tended to avoid counseling with health care professionals. Their odds ratio for inadequate health behaviors was three to four times higher than that of non-Type D patients. In a study of health behaviors of 386 CAD patients (Ginting et al., 2016), Type D personality was associated with lower health behaviors while controlling for anxiety and depression.
People with Type D personality tend to have negative illness perception. They feel that their illness will last for a long time and cause serious consequences, and that they cannot control the illness. In addition, they experience pain in the disease more intensely than those with non-Type D personality and experience also emotional problems such as depression and anxiety caused by the pain (Williams et al., 2011a). Mols and Denollet (2012) reported that people with Type D personality negatively perceived their illness and experienced more physical symptoms and emotional reactions due to illness in a survey of 3977 cancer patients. Illness perception is a concept derived from the self-regulation theory. Self-regulation theory defines humans as active problem solvers and explains how individuals behave through recognition, coping, and appraisal steps to reduce the perceived gap between the current and ideal health status (Leventhal and Carmeron, 1987). Illness perception is a self-reported belief in health, and health behaviors can vary according to illness perception; hence, changes in this illness perception can be the target of interventions (Broadbent et al., 2009; Petrie et al., 2002; Williams et al., 2011a). In previous studies (Park, 2014; Seong and Lee, 2011), the more positive the illness perception was, the higher the self-care ability was. Positive illness perception was correlated health behaviors such as cardiac rehabilitation participation, diet, exercise, and smoking (Broadbent et al., 2009; French et al., 2006).
In summary, Type D personality affects health behaviors and illness perceptions, and illness perception is also an influential factor of health behaviors. Type D personality is a relatively stabilized personality characteristic; it is difficult to change this and promote health behaviors. Conversely, illness perception is a variable that can be changed through intervention. Therefore, this study aims to provide the theoretical basis for the development of interventions that can improve the health behaviors by understanding the mediating effects of illness perception in the relationship between Type D personality and health behaviors among CAD patients who underwent PCI. The specific objectives of this study were to (1) assess Type D personality, illness perception, and health behaviors of study participants; (2) examine the differences in health behaviors according to participant characteristics; (3) examine the relationships between Type D personality, illness perception, and health behaviors; and (4) identify the mediating effects of illness perception on the relationship between Type D personality and health behaviors.
Methods
Design
This study used a cross-sectional survey to investigate the mediating effects of illness perception on the relationship between Type D personality and health behaviors in CAD patients who underwent PCI.
Sampling and data collection
The participants were adults over 18 years of age and met the following criteria:
Those who had been diagnosed with CAD such as angina pectoris and myocardial infarction in a university hospital located in the city of Changwon in South Korea;
Those who had undergone PCI;
Those who were in stable physical condition without complications at the time of data collection;
Those who had no problems in cognitive function.
For the sample size, the minimum number of samples required for multiple regression analysis was calculated using the G-power 3.1.9 program. A total of 131 participants were required when the effect size was .15 (Williams et al., 2011a), the power was .80, and the number of independent variables was set at 13. We collected data of 150 CAD patients considering the dropout rate of about 10 percent, and 142 of them, except the unreliable or missing respondents, were the final participants of this study.
We received approval from the S-University Hospital Internal Review Board for the content and procedures of the study prior to data collection (approval no. 15-SCMC-033-00). The data collection period was for about 2 months from 15 July 2015 to 31 August 2015. CAD patients who visited the cardiovascular outpatient clinic of the hospital were recruited. When the patient indicated the intention to participate, one of the researchers confirmed that he or she met the selection criteria. The questionnaires were administered to the participants after they signed an informed consent sheet. Questionnaires were self-report, but if the patient wanted it, the researcher read it verbally and wrote the answer of the patient. The average time spent in completing the questionnaire was 15 minutes.
Characteristics of study participants
A total of 142 CAD patients who underwent PCI participated in the study, with an average age of 65.21 ± 10.42 years and 76.8 percent of them being male. Among them, 79.6 percent were living with family and 51.4 percent followed a religion. About a half of the participants were educated at high school or higher. At the time of the survey, 46.5 percent of the participants had a job. As for the economic status, 66.2 percent answered “middle.”
ST-segment elevation myocardial infarction was the most frequent diagnosis (40.8%). Most participants had comorbidities, among which hypertension was the most common (35.8%), followed by diabetes (25.0%) and hyperlipidemia (24.1%). The family history of heart disease was reported by 23.2 percent participants. The mean duration of illness was 3.61 ± 2.36 years (Table 1).
Table 1.
Participants’ characteristics and health behaviors (N = 142).
| Characteristics | Categories | n | % | M ± SD | t/F | p |
|---|---|---|---|---|---|---|
| Gender | Male | 109 | 76.8 | 47.95 ± 9.20 | .47 | .639 |
| Female | 33 | 23.2 | 48.81 ± 9.40 | |||
| Age (years) | <50 | 10 | 7.0 | 47.60 ± 9.32 | .261 | .854 |
| 50–59 | 27 | 19.0 | 49.22 ± 10.52 | |||
| 60–69 | 51 | 35.9 | 48.47 ± 9.69 | |||
| ⩾70 | 54 | 38.0 | 47.42 ± 8.20 | |||
| M ± SD | 65.21 ± 10.42 | |||||
| Family living together | Yes | 113 | 79.6 | 48.07 ± 8.91 | .214 | .831 |
| No | 29 | 20.4 | 48.48 ± 10.50 | |||
| Religion | Yes | 73 | 51.4 | 49.76 ± 9.12 | 2.17 | .032 |
| No | 69 | 48.6 | 46.44 ± 9.08 | |||
| Education | None | 12 | 8.5 | 44.16 ± 8.51 | 1.24 | .291 |
| Elementary–middle | 69 | 48.6 | 48.65 ± 8.76 | |||
| ⩾High school | 61 | 43.0 | 48.37 ± 9.79 | |||
| Perceived economic status | High | 9 | 6.3 | 53.44 ± 9.34 | 2.69 | .071 |
| Middle | 94 | 66.2 | 48.54 ± 9.40 | |||
| Low | 39 | 27.5 | 46.00 ± 8.30 | |||
| Occupation | Yes | 66 | 46.5 | 48.74 ± 9.60 | .70 | .484 |
| No | 76 | 53.5 | 47.64 ± 8.87 | |||
| Diagnosis | Unstable angina | 45 | 31.7 | 48.66 ± 9.12 | .25 | .782 |
| NSTEMI | 39 | 27.5 | 48.53 ± 9.48 | |||
| STEMI | 58 | 40.8 | 47.50 ± 9.24 | |||
| Comorbidity | Yes | 122 | 85.9 | 48.56 ± 9.15 | 1.31 | .191 |
| No | 20 | 14.1 | 45.65 ± 9.46 | |||
| Type of comorbiditya | Hypertension | 76 | 35.8 | |||
| Dyslipidemia | 51 | 24.1 | ||||
| Diabetes | 53 | 25.0 | ||||
| Heart failure | 12 | 5.7 | ||||
| Renal failure | 5 | 1.4 | ||||
| Others | 17 | 8.0 | ||||
| Familial history of heart disease | Yes | 33 | 23.2 | 47.93 ± 9.44 | .15 | .881 |
| No | 109 | 76.8 | 48.22 ± 9.19 | |||
| Duration of illness (years) | <1 | 38 | 26.8 | 48.34 ± 9.96 | .14 | .986 |
| 1–5 | 74 | 52.1 | 48.13 ± 8.49 | |||
| >5 | 30 | 21.1 | 47.96 ± 10.26 | |||
| M ± SD | 3.61 ± 2.36 | |||||
NSTEMI: non-ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction; SD: standard deviation.
Multiple answers allowed.
Measurements
Type D personality
Type D personality was measured using the Korean version of Type D scale-14 (the Korean DS14) originally developed by Denollet (2005) and translated and validated by Lim et al. (2011). This scale consists of 2 domains, “negative affectivity” and “social inhibition,” and a total of 14 items, each with 7 items per domain. Each item is answered with a five-point Likert-type scale ranging from 0 to 4 points. If the respondent’s score is more than 10 points in both areas, he or she is classified as having Type D personality (Denollet, 2005). The reliability of the scale reported in the previous study (Lim et al., 2011) was Cronbach’s α = .86 for negative affectivity and Cronbach’s α = .80 for social inhibition. The reliability of the scale measured in this study was Cronbach’s α = .76 for negative affectivity and Cronbach’s α = .82 for social inhibition.
Illness perception
Illness perception was measured using the Brief Illness Perception Questionnaire (Brief-IPQ) developed by Broadbent et al. (2006). For this study, the questionnaire was translated and reverse translated into Korean with the authors’ permission, and the content validity of the scale was verified by five nursing professors and two cardiovascular nurses with master’s degrees. The content validity index (CVI) of all the items was more than .80, so the items of the original tool were maintained and the Korean expressions of the two items were modified to be easy to understand. The questionnaire consists of a total of eight items including the consequences, timeline, personal control, treatment control, identity, concern, understanding, and emotional response. Response to each item ranges from 0 to 10 points, and the total score ranges from 0 to 80. The higher the score, the more positive the illness perception. During its development, the reliability of the questionnaire was Cronbach’s α = .73 (Broadbent et al., 2006), and in this study it was Cronbach’s α = .70.
Health behaviors
Health behaviors were measured using the health behavior questionnaire of the CAD patients developed by Choi (2013). A total of 30 items were used, except 1 item (visiting outpatient clinic to check complication or recurrence even after PCI) that was not relevant to the situation of the current participants, with the permission of the original author. The final questionnaire consisted of eight sub-domains: two items for treatment compliance, three for disease management, five for diet, four for exercise, five for daily life style, two for sleep, six for stress, and three for emergency situation. Each question is answered with a four-point Likert-type scale ranging from 0 to 3. The possible range of scores is from 30 to 90. The higher the score, the better the health behavior. During its development, the reliability of the questionnaire was Cronbach’s α = .87 (Choi, 2013), and in this study it was Cronbach’s α = .78.
Statistical analysis
The collected data were analyzed using the SPSS/WIN 23.0 program (IBM Corp., Armonk, NY) as follows:
General characteristics and disease-related characteristics of the participants were presented as frequency, percentage, mean, and standard deviation;
The differences in health behaviors according to the characteristics of the participants were tested using t-test and ANOVA. Scheffe’s test was used for post hoc test;
The relationships between Type D personality, illness perception, and health behaviors were analyzed using t-test and Pearson’s correlation coefficient;
To test the mediating effect of illness perception, a series of hierarchical multiple regressions were performed according to Baron and Kenny’s (1986) procedures;
Sobel test (Preacher and Hayes, 2008) was conducted to verify the significance of the mediating effect of illness perception on the relationship between Type D personality and health behaviors.
Results
Type D personality, illness perception, and health behaviors of the study participants
If the participant’s Type D scale-14 score was more than 10 points in both domains, he or she was classified as a D-type personality according to the criteria proposed by Denollet (2005). A total of 28.9 percent participants were classified as having Type D personality. Their mean score on negative affectivity was 13.34 ± 2.38 and that on social inhibition was 13.80 ± 2.60. The mean score of the non-Type D participants was 4.63 ± 3.59 for negative affectivity and 5.81 ± 5.25 for social inhibition (Table 2).
Table 2.
Type D personality among study participants (N = 142).
| Personality | n (%) | Negative affectivity, M ± SD | Social inhibition, M ± SD |
|---|---|---|---|
| Type D | 41 (28.9) | 13.34 ± 2.38 | 13.80 ± 2.60 |
| Non-Type D | 101 (71.1) | 4.63 ± 3.59 | 5.81 ± 5.25 |
| Total | 142 (100.0) | 7.14 ± 5.14 | 8.11 ± 5.89 |
SD: standard deviation.
The mean of the total score of illness perception was 41.64 ± 13.22. Among the eight items, the score for the timeline item (how long do you think your illness will continue?) was the lowest at 1.18 ± 2.23, and for the treatment control item (how much do you think your treatment can help your illness?) was the highest at 7.16 ± 2.67. The mean of the total score of the participants’ health behaviors was 48.15 ± 9.22. Among the sub-domains, the score on “treatment compliance” was the highest at 5.14 ± .92 and “disease management” was the lowest at 2.88 ± 1.75.
Differences in health behaviors according to participant characteristics
Results of analyzing the difference in health behaviors according to participant characteristics revealed a significant difference according to religion. The health behaviors of the participants following a religion were significantly higher than the behaviors of those not following one (t = 2.17, p = .032). Conversely, there was no significant difference in health behaviors according to age, family living together, education level, economic status, present occupation, comorbidity, family history, diagnosis, and duration of illness (Table 1).
Relationship between Type D personality, illness perception, and health behaviors
In the process of examining the relationship between the variables, we analyzed the differences in the two variables according to Type D personality, because Type D personality was the categorical variable. The mean score of illness perception of Type D participants was significantly lower than that of non-Type D participants (t = 7.40, p < .001). In addition, the mean score of health behaviors of Type D participants was significantly lower than that of non-Type D participants (t = 3.21, p = .002; Table 3).
Table 3.
Illness perception and health behaviors according to Type D personality (N = 142).
| Variables | Type D (n = 41) | Non-Type D (n = 101) | t | p |
|---|---|---|---|---|
| M ± SD | M ± SD | |||
| Illness perception | 31.58 ± 9.33 | 45.72 ± 12.30 | 7.40 | <.001 |
| Health behaviors | 44.80 ± 7.07 | 49.51 ± 9.66 | 3.21 | .002 |
SD: standard deviation.
Pearson’s correlation analysis was used to examine the relationship between illness perception and health behaviors. There was a statistically significant correlation between illness perception and health behaviors (r = .43, p < .001). In other words, the more positive the participants’ perception of disease, the higher their performance of health behaviors.
The mediating effect of illness perception on the relationship between Type D personality and health behaviors
The tolerance limits of data were higher than the reference value of .1 and all variation inflation factor values were much smaller than the reference value of 10. Since there was no problem of multicollinearity, the assumption for regression analysis was satisfied. Univariate analysis showed that there was a difference in the health behaviors according to the religions of the participants. We adjusted the effect of religion by entering it as a control variable in a series of regression analyses. The mediating effect of illness perception was analyzed according to the three steps of Baron and Kenny (1986). In a series of multiple hierarchical regression analysis, religion did not have a significant effect.
As a result of step 1 analysis, the independent variable, Type D personality, had a significant effect on the dependent variable, health behaviors (β = –.209, p = .013). In step 2 analysis, the influence of Type D personality on the mediating variable, illness perception, was also significant (β = –.486, p < .001). Finally, in step 3 analysis, the combined effect of Type D personality and illness perception on health behaviors was also significant (β = .415, p < .001). At this step, the standardized coefficient (β), which was the influence of Type D personality on health behaviors, was smaller than that in step 1 and was not statistically significant (β = –.007, p = .934). On controlling illness perception, the absolute regression coefficient of Type D personality decreased, and the correlation between Type D personality and health behaviors changed to being non-significant. Therefore, illness perception between these two variables can be interpreted as having a complete mediating effect (Table 4 and Figure 1). Sobel test showed that the direct effect of Type D personality on health behaviors was not significant and the mediating effect of illness perception was significant (Z = –4.29, p < .001).
Table 4.
Results of hierarchical regressions for mediating effects (N = 142).
| Paths | SE | β | t | p |
|---|---|---|---|---|
| Type D personality → health behaviors | 1.62 | −.209 | −2.53 | .013 |
| Type D personality → illness perception | 2.18 | −.486 | −6.47 | <.001 |
| Type D personality → health behaviors | 1.77 | −.007 | −.08 | .934 |
| Illness perception → health behaviors | .06 | .415 | 4.79 | <.001 |
SE: standard error.
Figure 1.
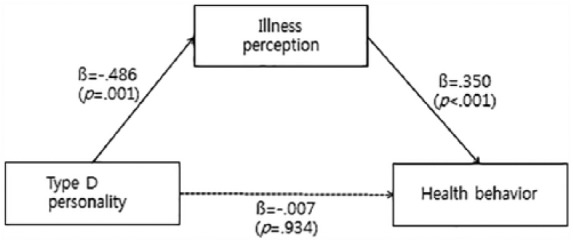
A model for the mediating effect of illness perception.
Discussion
In this study, we observed that illness perception completely mediates the effects of Type D personality on health behaviors of CAD patients who underwent PCI. Type D personality is characterized by negative affectivity and social inhibition (Denollet, 2005). Type D patients have negative thoughts on their illness (Williams et al., 2011a), and patients’ illness perception strongly affects their health behaviors and outcomes (Juergens et al., 2009). The results of this study suggest the importance of illness perception as a mechanism to explain the link between Type D personality and unhealthy behavior in CAD patients.
In this study, the illness perception of Type D patients was lower than that of non-Type D patients. These results can be interpreted as the influence of negative affectivities, which are the personality traits of Type D patients, on the formation of illness perception. Similar to our results, Williams et al. (2011a) studied the relationship between Type D personality and illness perception in patients with myocardial infarction and reported that illness perception was lower in Type D patients. In a study by Li et al. (2017) on peritoneal dialysis patients, patients with Type D personality had more negative beliefs about their illness. In general, Type D patients are more worried about their illness, less understanding, and emotionally depressed (Nefs et al., 2015).
The association between illness perception and health behaviors can be explained by the self-regulation systems theory of health. According to the self-regulatory model (Leventhal and Carmeron, 1987), individuals first form cognitive and emotional representations when faced with illness or health threats. Next, they adopt their behaviors to cope with it, and finally they appraise the efficacy of their own health behaviors. In this continuous and cyclical self-regulatory process of behavior, the illness representations play an important role. Patients form their own emotional representation such as fear, anger, and distress as well as cognitive representations including identity, consequences, cause, timeline, and control of their illness (Broadbent et al., 2006). These representations guide subsequent coping strategies and health behaviors such as compliance to health recommendations (Leventhal and Carmeron, 1987). The important role of illness perception and coping in health conditions has been confirmed in a recent meta-analysis (Dempster et al., 2015).
As a result of this study, it was revealed that illness perception has a complete mediating effect on the relationship between Type D personality and health behaviors. In other words, illness perception is a significant variable for enhancing health behaviors in relation to Type D personality and health behaviors, and Type D personality indirectly affects health behaviors through illness perception. At first glance, this result may seem to contradict the results of several previous studies suggesting a simple association between Type D personality and health behaviors (Ginting et al., 2016; Nefs et al., 2015; Williams et al., 2011b). In addition, Williams et al. (2011a) reported that Type D personality in myocardial infarction patients had a significant correlation with illness perception and could lead to negative health outcomes. A study of patients with rectal cancer (Mols and Denollet, 2012) and a study on peritoneal dialysis patients (Li et al., 2017) reported that Type D personality correlated with negative illness perception. All of the above-mentioned studies used univariate analyses such as mean comparison or correlation coefficient between Type D personality, illness perception, and health behaviors. On the other hand, in this study, we have presented the relationship between Type D personality, illness perception, and health behaviors in more detail by testing a mediating effect of illness perception using the multivariate regression model.
Cao et al. (2016) presented a systematic review of four intervention studies for cardiovascular patients with Type D personality. Although the interventions improved the outcomes of Type D patients, they were more effective for non-Type D patients. The authors suggested that it was necessary to improve the illness perception in order to increase the efficiency of intervention for Type D patients. Several previous studies have developed and applied intervention programs to raise illness perception. Broadbent et al. (2009) developed an intervention program to improve illness perception in patients with myocardial infarction. This program allowed patients to assess, plan, intervention, recover, and evaluate health behaviors and to plan healthy recovery after discharge. Petrie et al.’s program for patients with myocardial infarction was designed to seek changes in health behaviors and recovery of function beginning with the perspective of the individual patient’s illness and gradually expanding interventions (Petrie et al., 2002). In this way, the intervention program to raise illness perception not only includes mere education or rehabilitation training but also positively promotes awareness of the individual’s illness, ultimately enhancing the health behaviors for positive prognosis of the disease. Those interventions in Cao et al.’s (2016) review added socio-psychological counseling or meditation to basic cardiac rehabilitation program, but were not specifically designed for Type D patients. Interventions for Type D patients need to be individualized strategies and may focus on improving mood and health status, health-related behaviors, and interpersonal functioning (Pelle et al., 2012). Despite the high prevalence of Type D personality in CAD patients, interventions designed for Type D CAD patients are limited. Therefore, it is recommended that individualized interventions in the context of Type D personality be developed.
This study is meaningful in that it provided directions for nursing intervention by verifying the mediating effect of illness perception on the relationship between Type D personality, which is relatively difficult to change, and health behaviors of CAD patients. However, since a cross-sectional design was adopted in this study, it is difficult to discuss the causal relationship between the variables clearly. In other words, the mediating effect observed here is not a causal relationship according to time difference but a regressive relationship between the measured variables. Therefore, it is appropriate to look at it provisionally, and it is necessary to confirm the mediating effect of illness perception through longitudinal studies. Based on the results of this study, it is necessary to confirm the effects of illness perception intervention program to increase the health behaviors of Type D patients with CAD.
Conclusion
This study analyzed the mediating effects of illness perception on the relationship between Type D personality and health behaviors in CAD patients after undergoing PCI. Of the total 142 CAD patients, 28.9 percent had Type D personality. The presence of Type D personality in CAD patients was observed to predict health behaviors and illness perception significantly. However, Type D personality was observed to only indirectly affect health behaviors. In other words, illness perception can completely mediate the relationship between the two variables. Therefore, the development and application of interventions to improve illness perception of patients with CAD may improve their health behaviors and, ultimately, prevent recurrence and improve quality of life. We propose a rigorous analysis of the causal relationship between these variables through longitudinal or experimental studies.
Acknowledgments
We would like to thank all of the patients for participating in this study. M.K. and J.K. conceived and designed the research. M.K. collected and analyzed the data. J.K. wrote the paper.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Baron RM, Kenny DA. (1986) The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology 51(6): 1173–1182. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Ellis CJ, Thomas J, et al. (2009) Further development of an illness perception intervention for myocardial infarction patients: A randomized controlled trial. Journal of Psychosomatic Research 67(1): 17–23. [DOI] [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, et al. (2006) The Brief Illness Perception Questionnaire. Journal of Psychosomatic Research 60(6): 631–637. [DOI] [PubMed] [Google Scholar]
- Cao X, Wong EM, Chow Choi K, et al. (2016) Interventions for cardiovascular patients with Type D personality: A systematic review. Worldviews Evidence-Based Nursing 13(4): 314–323. [DOI] [PubMed] [Google Scholar]
- Choi YO. (2013) A comparison of factors influencing health behavior compliance by Type D personality in the patients with coronary artery disease. Master’s Thesis, Chonnam National University, Gwangju, South Korea. [Google Scholar]
- Dempster M, Howell D, McCorry NK. (2015) Illness perceptions and coping in physical health conditions: A meta-analysis. Journal of Psychosomatic Research 79(6): 506–513. [DOI] [PubMed] [Google Scholar]
- Denollet J. (2005) DS14: Standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosomatic Medicine 67(1): 89–97. [DOI] [PubMed] [Google Scholar]
- French DP, Cooper A, Weinman J. (2006) Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: A systematic review with meta-analysis. Journal of Psychosomatic Research 61(6): 757–767. [DOI] [PubMed] [Google Scholar]
- Juergens MC, Seekatz B, Moosdorf RG, et al. (2009) Illness beliefs before cardiac surgery predict disability, quality of life, and depression 3 months later. Journal of Psychosomatic Research 68(6): 553–560. [DOI] [PubMed] [Google Scholar]
- Ginting H, Van de Ven M, Becker ES, et al. (2016) Type D personality is associated with health behaviors and perceived social support in individuals with coronary heart disease. Journal of Health Psychology 21(5): 727–737. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Carmeron L. (1987) Behavioral theories and the problem of compliance. Patient Education and Counseling 10(2): 117–138. [Google Scholar]
- Li J, Wu X, Lin J, et al. (2017) Type D personality, illness perception, social support and quality of life in continuous ambulatory peritoneal dialysis patients. Psychology, Health & Medicine 22(2): 196–204. [DOI] [PubMed] [Google Scholar]
- Lim HE, Lee MS, Ko YH, et al. (2011) Assessment of the Type D personality construct in the Korean population: A validation study of the Korean DS14. Journal of Korean Medical Science 26(1): 116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mols F, Denollet J. (2012) The association between Type D personality and illness perceptions in colorectal cancer survivors: A study from the population-based PROFILES registry. Journal of Psychosomatic Research 73(3): 232–239. [DOI] [PubMed] [Google Scholar]
- Mols F, Martens EJ, Denollet J. (2010) Type D personality and depressive symptoms are independent predictors of impaired health status following acute myocardial infarction. Heart 27(1): 52–58. [DOI] [PubMed] [Google Scholar]
- Nefs G, Speight J, Pouwer F, et al. (2015) Type D personality, suboptimal health behaviors and emotional distress in adults with diabetes: Results from diabetes MILES–The Netherlands. Diabetes Research and Clinical Practice 108(1): 94–105. [DOI] [PubMed] [Google Scholar]
- Park SY. (2014) The correlation among anxiety, illness perception and self-care agency in elderly with heart disease. Master’s Thesis, Catholic University of Pusan, Busan, South Korea. [Google Scholar]
- Pedersen SS, Denollet J. (2003) Type D personality, cardiac events, quality and impaired of life: A review. Journal of Cardiovascular Prevention and Rehabilitation 10: 241–248. [DOI] [PubMed] [Google Scholar]
- Pelle AJ, Van den Broek KC, Denollet J. (2012) Interventions in the context of the distressed (Type D) personality. In: Dornelas EA. (ed.) Stress Proof the Heart: Behavioural Interventions for Cardiac Patients. New York: Springer, pp. 167–198. [Google Scholar]
- Petrie KJ, Cameron LD, Ellis CJ, et al. (2002) Changing illness perception after myocardial infarction: An early intervention randomized controlled trail. Psychosomatic Medicine 64(4): 580–586. [DOI] [PubMed] [Google Scholar]
- Piraino D, Cimino G, Buccheri D, et al. (2017) Recurrent in-stent restenosis, certainty of its origin, uncertainty about treatment. International Journal of Cardiology 230(1): 91–96. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40: 879–891. [DOI] [PubMed] [Google Scholar]
- Puymirat E, Simon T, Cayla G, et al. (2017) Acute myocardial infarction: Changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation 136(20): 1908–1919. [DOI] [PubMed] [Google Scholar]
- Seong YS, Lee YW. (2011) Relationship of illness perception, self-efficacy, and self-care among pulmonary tuberculosis patients. Korean Journal of Adult Nursing 23(1): 31–39. [Google Scholar]
- Statistics Korea (2013) 2013 Statistics of mortality cause. Available at: http://kosis.kr/wnsearch/totalSearch.jsp (accessed 10 October 2017).
- Steca P, Monzani D, Greco A, et al. (2017) Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS ONE 12(8): e0183905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Throndson K, Sawatzky JAV. (2009) Angina following percutaneous coronary intervention: In-stent restenosis. Canadian Journal of Cardiovascular Nursing 19(3): 16–23. [PubMed] [Google Scholar]
- Williams L, O’Connor RC, Grubb N, et al. (2011. a) Type D personality and illness perception in myocardial infarction patients. Journal of Psychosomatic Research 70(2): 141–144. [DOI] [PubMed] [Google Scholar]
- Williams L, O’Connor RC, Grubb N, et al. (2011. b) Type D personality predicts poor medication adherence in myocardial infarction patients. Psychology & Health 26: 703–712. [DOI] [PubMed] [Google Scholar]
- Williams L, O’Connor RC, Howard S, et al. (2008) Personality mechanisms of effect: The role of health related behavior and social support. Journal of Psychosomatic Research 64(1): 63–69. [DOI] [PubMed] [Google Scholar]


