Abstract
Objective:
To test theorized patient-level mediators in the causal pathway between health literacy (HL) and 1-year mortality among adults with cardiovascular disease (CVD)
Patients and Methods:
3,000 adults treated at Vanderbilt University Hospital from October 11, 2011 to December 18, 2015 for acute coronary syndrome or acute decompensated heart failure (ADHF) participated in the Vanderbilt Inpatient Cohort Study. Participants completed a bed-side administered survey and consented to health record review and longitudinal follow-up. Multivariable mediation models examined the direct and indirect effects of HL (a latent variable with 4 indicators) with 1-year mortality post-discharge (dichotomous). Hypothesized mediators included social support, health competence, health behavior, comorbidity index, type of CVD diagnosis, and prior year hospitalizations.
Results:
Of the 2,977 patients discharged from the hospital (60% male, mean age 61 years, 83% non-Hispanic White, 37% admitted for ADHF), 17–23% had inadequate HL depending on measure, and 10% died within 1 year. The total effect of lower HL on 1-year mortality (AOR=1.31 [95% CI, 1.01, 1.69]) was decomposed into an indirect effect (AOR=1.50 [1.35, 1.67]) via the mediators and a nonsignificant direct effect (AOR=0.87 [CI, 0.66, 1.14]). Each standard deviation decrease in HL was associated with an absolute 3.2 percentage point increase in the probability of 1-year mortality via mediators admitted for ADHF, comorbidities, health behavior, health competence, and prior hospitalizations (by contribution to indirect effect).
Conclusion:
Patient-level factors drive the relationship between low HL and mortality. Health competence and health behavior are modifiable mediators that could be targeted by interventions.
Introduction
After hospitalization for cardiovascular disease (CVD), patients must understand and integrate new information to perform complicated self-care behaviors and manage new medications, lifestyle changes, and follow-up appointments.1 Success is influenced by their ability to read and understand text-based resources; locate and interpret reliable health information; use numbers for tasks such as adherence to medications; and listen effectively to instructions.2 Collectively, these abilities are conceptualized as health literacy (HL)3, 4 which is a multidimensional construct5 largely formed early in life alongside educational attainment.4 Previous cohort studies have demonstrated that low HL independently predicts mortality in community-dwelling elders6, 7 and adults with congestive heart failure (CHF),8, 9 and after hospitalization for CHF.10, 11 However, cohort studies have not explored the link between HL and mortality among adults with acute coronary syndromes (ACS).12
Despite emphasis on HL as an important determinant of mortality among adults with CVD,2 the mechanisms by which HL might lead to increased mortality are poorly understood. Research identifying modifiable targets linking low HL to poor outcomes is needed to inform interventions among adults with CVD.5, 9, 13, 14 Mediation analysis elucidates relationships between a predictor and outcome by examining variables (mediators) posited to lie in the causal pathway. Several hypothesized mediators link low HL to adverse health outcomes, including death.15 For instance, low HL has been linked to less ability to understand, be motivated towards,16 and perform successful self-management3 and having inadequate social support14 for maintaining health care follow-ups and self-management. Furthermore, low HL may affect post-discharge outcomes via associations with higher disease prevalence,10, 17, 18 increased comorbidities,8 and worse overall health3, 17 which in turn may lead to increased mortality.8
Few studies19–27 have explored mediators of the effects of HL on patient outcomes, and to our knowledge, none has explored mediators of the relationship between HL and mortality in any population. Therefore, we tested hypothesized13, 15 patient-level behavioral, social, and clinical mediators of effects of HL on 1-year mortality among adults hospitalized for CVD.
Methods
The Vanderbilt Inpatient Cohort Study (VICS) was a 5-year prospective study which enrolled 3,000 adult patients treated at Vanderbilt University Hospital October 11, 2011 through December 18, 2015. VICS was designed to examine how social determinants, in particular HL, affect care transitions and outcomes. Participants had a physician-confirmed diagnosis of ACS and/or acute decompensated heart failure (ADHF) for the index hospitalization. Patients were excluded if they had dementia or unstable psychiatric illness, were unable to communicate in English, or were in hospice care or too ill to complete an interview. The Vanderbilt University Institutional Review Board approved all study procedures. Mediators and covariates were specified a priori13 drawing on a conceptual causal model of the pathways by which HL may affect health outcomes.15 We focused on the patient-level mediators, excluding provider and health care system factors in the proposed model.15 Details of the study design have been published.13
Measures
Informed consent and interviews were completed at the patients’ bedside by a trained research assistant, generally within 24 hours of hospitalization. CVD diagnosis and comorbidities were determined from electronic health record data and mortality data were gathered from multiple sources.
Predictor: Health Literacy (HL).
We assessed Hl with the Brief Health Literacy Screen (BHLS),28, 29 the short form of the Test of Functional Health Literacy in Adults (S-TOFHLA),30, 31 a 3-item version of the Subjective Numeracy Scale (SNS-3),32–34 and years of education (self-report). The BHLS is a subjective measure, asking patients to report their level of confidence filling out medical forms, need for assistance in reading hospital materials, and understanding of written medical information. The S-TOFHLA is an objective test in which respondents choose words missing from text representing medical directions and information about health care. The SNS-3 asks patients to rate their own math skills and preferences for numerical information.
Covariates.
Potential confounders included as covariates were age, male gender, minority race/ethnicity, and socioeconomic status (SES). Race and ethnicity responses were combined to characterize participants as non-Hispanic White or minority. Participant-reported indicators of SES included employment status (3-level categorical variable: employed full- or part-time, disabled or, referent, able to work but not working), financial strain, household income, and insurance status (dichotomized: underinsured, including uninsured or public insurance only, versus adequately insured). Financial strain was assessed using a single question, “How difficult is it for you (and your family) to pay your monthly bills?,”35 analyzed as a continuous variable with higher scores reflecting greater difficulty. Household income was assessed with modified strata from the Behavioral Risk Factor Surveillance System questionnaire.36
Mediators.
Social/behavioral mediators included health competence, health behaviors, and social support. Clinical mediators included a comorbidity index, CVD diagnosis, and prior year hospitalizations.
Health competence was assessed with two items from the Perceived Health Competence Scale:37 “It is difficult for me to find effective solutions for health problems that come my way” (reverse scored) and “I am able to do things for my health as well as most other people.” Higher scores indicate a higher belief in one’s capacity to optimize his/her health outcomes.
Health behavior was assessed with a Health Behavior Index38 which reflects 6 health behaviors assessed with validated scales or items: medication adherence, resilient coping, smoking, alcohol consumption, diet, and exercise. The domain scores are summed to produce an index score, with higher scores indicating healthier behaviors.
Social support was assessed with the Enhancing Recovery in Coronary Heart Disease (ENRICHD) Social Support Inventory,39, 40 which includes 6 questions regarding emotional and instrumental support, and a categorical variable called home status (3-level variable: married/partnered, living alone and not married/partnered or, referent, not married/partnered but living with someone).
Comorbidities.
We used an index by van Walraven that provides a weighted summary score for the presence or absence of 30 conditions identified by Elixhauser.41 We did not include the weight for CHF in the index score because this diagnosis was a separate variable in the analyses.
CVD diagnosis was a 3-level categorical variable: ACS only (referent), ACS with CHF history, and ADHF at index hospitalization.
Prior year hospitalizations.
Participants reported how many hospitalizations they had experienced in the 12 months prior to the index hospitalization.
Outcome: 1-year mortality.
Mortality data were gathered using a combination of data from the Social Security Administration’s Death Master File (DMF),42 documentation in the electronic health record, family report, and obituaries. During this study, the DMF was downloaded monthly into the Vanderbilt Enterprise Data Warehouse and linked to patient records by social security number or, when that was not available, through a matching algorithm that utilizes other variables. The DMF is widely used in research43, 44 and provides accurate matches for death (> 90% among American-born individuals), but does omit some events. Supplementing and verifying DMF data with other sources provides a highly accurate ascertainment of vital status. We have complete follow-up on all participants for at least 1 year; for this analysis, we constructed a dichotomous variable reflecting all-cause death within 365 days of hospital discharge.
Note: Although HL measures were captured at the time of enrollment, we assume that HL remains reasonably constant over time and therefore precedes and is a potential cause of all mediating variables. Although the constancy of HL over the lifespan is debated,4, 45 there is little support that the proposed mediating variables cause or quickly change HL.
Analyses
Analyses were performed using Stata 14.2 or AMOS 24.0 with P<.05 considered statistically significant.
Latent variable analysis.
Often constructs of interest are not directly observable but rather merely estimated by observed indicators (measures), each of which have varying strengths, limitations, degree of error and/or measure different aspects of a multidimensional construct. Latent variable analysis obtains a robust representation of constructs by combining indicators using the variance/covariance matrix.46 HL, SES, and social support, are each multidimensional constructs. Therefore, we conducted latent variable analysis with multiple indicators for each construct using structural equation modeling (SEM) prior to mediation analysis. We developed latent variables for HL (indicator variables: S-TOFHLA, BHLS, SNS-3, education), SES (indicator variables: employed, disabled, financial strain, income, underinsured), and social support (indicator variables: ENRICHD and home status indicators married and living alone) following guidelines for measurement model development in SEM.46 Model fit was assessed using thresholds for multiple fit indices (the comparative fit index, CFI≥0.95; the root mean square error of approximation, RMSEA≤0.06 with confidence interval [CI] 0.00–0.08; and the standardized root mean square residual, SRMR<0.08).46 Good model fit indicates the variance/covariance matrix implied by the model does not differ significantly from that observed in the data.
Mediation analysis.
We used multiple imputation (m=10)47 to impute 1.05% missing data and latent variables. In mediation analysis (Figure 1), the total effect (also known as the c path; Figure 1A) is that of the predictor on the outcome in a model without mediators. The addition of mediators to the model (Figure 1B), decomposes the total effect into a direct effect (c’ path) and a total indirect effect (ab path). The direct effect represents the total effect further adjusted for the mediators. The total indirect effect represents the effect of the predictor on the outcome through its effects on the mediators. In this multiple mediator model, we further examine indirect effects for each mediator, adjusted for all other mediators in the model (depicted by curved arrows among mediators in Figure 1B). Indirect effects with bootstrapped 95% confidence intervals (CIs) that exclude zero are consistent with mediation.48
Figure 1. Mediation models examining the relationship between lower health literacy (HL) and 1-year mortality.
A) Base model (no mediators); total effect (c) of lower HL on 1-year mortality adjusted for covariates. B) Multiple mediator model; decomposes total effect into a direct (c’) and total indirect (ab) effect. Direct effect (c’) depicts effect of lower HL on 1-year mortality adjusted for all covariates and mediators; a paths depict effects of lower HL on each mediator adjusted for other mediators and covariates; b paths depict effects of mediators on 1-year mortality adjusted for all other mediators, covariates, and HL. The Karlson, Holm, & Breen method used for analyses adjusts for other mediators when calculated separate effects of each (depicted with curved arrows). Covariates were age, gender, minority status, and socioeconomic status (not shown).
To aid in interpretation of significant indirect effects (ab paths) in the multiple mediator models, we first regressed each mediator on HL adjusting for covariates and other mediators using linear and multinomial logistic regression models to capture the association of HL and each of the mediators (a paths). Next, using logistic regression, we regressed 1-year mortality (yes/no) on the mediators adjusting for HL and confounders to capture the independent effect of each mediator on 1-year mortality (b paths). We then used the Karlson, Holm, and Breen (KHB)49, 50 method (Stata package khb51) to examine indirect effects in a multiple mediator model.49, 50 The KHB method addresses key challenges associated with the present analyses: (a) it generates interpretable and meaningful coefficients using average partial effects (APEs) which provide the absolute difference, on average, in the probability of 1-year mortality for a standard deviation (SD) decrease in health literacy, and (b) it disentangles the contributions of multiple mediators into multiple indirect effects.52 To capture uncertainty in all effect estimates we used a non-parametric bootstrap with 5,000 replicates.48, 53 We also conducted a sensitivity analysis for the multiple mediator model with SEM using full information maximum likelihood to handle missing data and bootstrapping to ascertain if the same mediation effects were significant as those identified in the planned analysis. Findings were consistent with those presented here and are not shown.
Results
A total of 44,600 patient charts were screened, identifying 12,736 with a confirmed diagnosis of ACS and/or ADHF. Of these, nearly 30% (3,763) met all eligibility criteria. Eighty percent (3,000) of eligible patients enrolled. Twenty-three participants died during the index hospitalization and were excluded, resulting in a total sample of 2,977 participants. Table 1 shows participant characteristics, describing those who died within 1 year versus those who did not. Per the S-TOFHLA, 17% had inadequate HL; per the BHLS, 23% had low HL. Ten percent (n=304) of the sample died within a year of hospital discharge.
Table 1.
Participant characteristics stratified by 1-year mortality and total.
| Survived (n=2673) | Died (n=304) | Total (N=2,977) | ||
|---|---|---|---|---|
| COVARIATES | Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | Range [IQR] |
| Age, years | 60.1 (12.3) | 63.8 (13.4) | 60.5 (12.5) | 20 – 95 [53, 69] |
| Race/Ethnicity | ||||
| Non-Hispanic White | 83.2 % | 82.5 % | 83.1 % | |
| Non-Hispanic Black | 12.9 % | 13.8 % | 13.0 % | |
| Hispanic | 2.2 % | 1.0 % | 2.0 % | |
| Other race/ethnicity | 1.7 % | 2.6 % | 1.8 % | |
| Male | 59.9 % | 56.6 % | 59.6 % | |
| Socioeconomic Status | ||||
| Employment Status | ||||
| Employed | 37.1 % | 8.3 % | 41.1 % | |
| Disabled, unable to work | 23.1 % | 39.1 % | 34.1 % | |
| Able to work but not working | 39.8 % | 52.6 % | 24.8 % | |
| Financial Strain | ||||
| Somewhat/very difficult to pay bills | 44.9 % | 51.8 % | 45.6 % | |
| Income (USD) | ||||
| <$20,000 | 20.8 % | 30.8 % | 21.8 % | |
| $20,000 – $34,999 | 24.9 % | 28.7 % | 25.3 % | |
| $35,000 – $49,999 | 16.0 % | 20.1 % | 16.5 % | |
| $50,000 – $74,999 | 14.5 % | 11.1 % | 14.1 % | |
| ≥$75,000 | 23.8 % | 9.3 % | 22.3 % | |
| Insurance Status | ||||
| Uninsured | 7.2 % | 2.3 % | 6.7 % | |
| Public (Medicare, Medicaid) only | 53.6 % | 80.6 % | 56.3 % | |
| Private (Commercial, Other) | 39.2 % | 17.1 % | 37.0 % | |
| PREDICTOR | ||||
| Health Literacy | ||||
| Education, years | 13.7 (2.9) | 13.3 (3.1) | 13.6 (2.9) | 1 – 25 [12, 16] |
| S-TOFHLA | 29.7 (7.5) | 25.6 (9.5) | 29.4 (7.8) | 0 – 36 [26, 35] |
| BHLS | 11.8 (3.1) | 11.2 (3.3) | 11.8 (3.1) | 2 – 15 [10, 15] |
| SNS-3 | 4.5 (1.3) | 4.2 (1.4) | 4.4 (1.3) | 1 – 6 [3.7, 5.7] |
| MEDIATORS | ||||
| Health Competence (PHCS-2) | 7.8 (2.2) | 6.8 (2.2) | 7.7 (2.2) | 2 – 10 [6, 10] |
| Health Behavior (HBI) | 6.9 (1.4) | 6.5 (1.2) | 6.8 (1.4) | 2.0 – 10.6 [5.9, 7.8] |
| Social Support | ||||
| Home Status | ||||
| Married/partnered | 61.0 % | 52.2 % | 60.1 % | |
| Lives alone | 19.2 % | 24.7 % | 20.2 % | |
| Lives with someone (not spouse/partner) | 19.8 % | 23.1 % | 19.7 % | |
| ENRICHD Social Support Inventory | 25.9 (4.6) | 25.8 (4.8) | 25.9 (4.6) | 6 – 30 [24, 30] |
| Comorbidities (adjusted Elixhauser score) | 9.4 (9.0) | 17.2 (9.5) | 10.2 (9.3) | −11 – 60 [3, 16] |
| Prior Year Hospitalizations | 1.3 (2.0) | 2.5 (2.7) | 1.4 (2.1) | 0 – 24 [0, 2] |
| Cardiovascular Disease Diagnosis | ||||
| ACS only | 43.0 % | 6.6 % | 39.2 % | |
| ACS with CHF history | 24.3 % | 18.4 % | 23.7 % | |
| ADHF at index hospitalization | 32.7 % | 75.0 % | 37.1 % | |
Latent constructs bolded: Socioeconomic Status, Health Literacy, or Social Support, with indicator variables italicized. M (SD) = mean (standard deviation); IQR, interquartile range. ACS, acute coronary syndromes; ADHF, acute decompensated heart failure; BHLS, Brief Health Literacy Screen; CHF, congestive heart failure; ENRICHD, Enhancing Recovery in Coronary Heart Disease; HBI, health behavior index; PHCS-2, Perceived Health Competence Scale-2 item version; S-TOFHLA, Short Test of Functional Health Literacy in Adults; SNS-3, Subjective Numeracy Scale, 3 item.
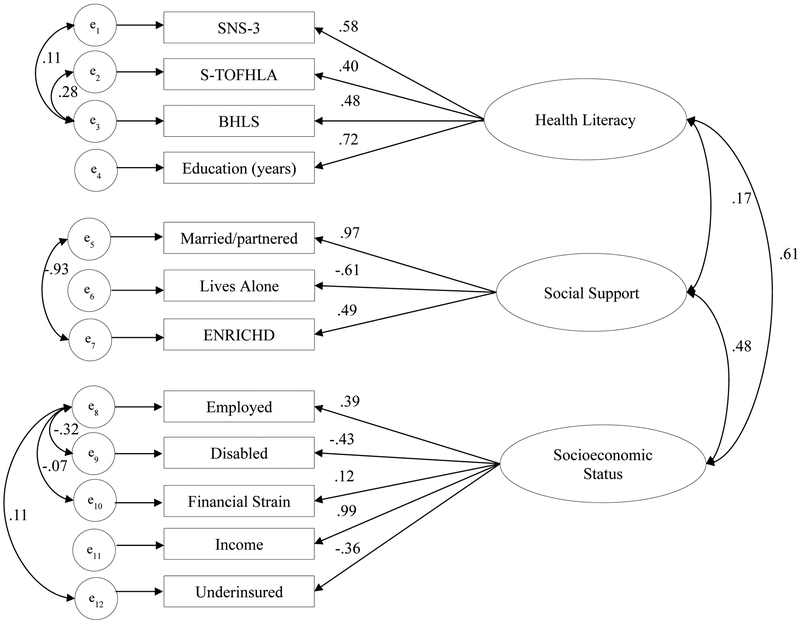
The final measurement model (Figure 2) had good fit (CFI=0.95; RMSEA=0.05, CI [0.05–0.06], SRMR=0.04). Adjusted HL to mediator (a) and mediator to 1-year mortality (b) paths (Table 2) inform interpretation of indirect effects identified in the multiple mediator model. Lower HL was independently associated with lower health competence, worse health behaviors, lower social support, more prior year hospitalizations, and greater likelihood of being admitted for ADHF. HL was not independently associated with comorbidities. Health competence, health behavior, comorbidities, prior year hospitalizations and CVD diagnosis (either ACS with CHF history or ADHF at index hospitalization) each independently predicted mortality in expected directions, but social support did not.
Figure 2. Final measurement model used for latent variables used in mediation analyses.
The three latent variables used in mediation analyses were Health Literacy, Social Support, and Socioeconomic Status. The numbers (right to left) depict: correlations between the latent variables; standardized coefficients for the factor loading of each indicator (measure); correlations between the residual measurement error (e) for some indicators. BHLS = Brief Health Literacy Screen; ENRICHD = Enhancing Recovery in Coronary Heart Disease Social Support Inventory; SNS-3 = Subjective Numeracy Scale-3; S-TOFHLA = Short form of the Test of Functional Health Literacy in Adults.
Table 2.
Adjusted regression models examining lower Health Literacy to Mediator (a paths) and Mediator to 1-year Mortality (b paths).
| a paths: Lower Health Literacy → Mediator | Unstandardized | Standardized | |||
|---|---|---|---|---|---|
| b | 95% Confidence Interval | P value | β | ||
| Health Competence | −0.718 | −0.833 | −0.602 | <.001 | −0.437 |
| Health Behavior | −0.431 | −0.516 | −0.347 | <.001 | −0.418 |
| Social Support | −0.261 | −0.377 | −0.145 | <.001 | −0.224 |
| Comorbidities | 0.681 | −0.226 | 1.588 | .13 | 0.100 |
| Prior Year Hospitalizations | 0.335 | 0.206 | 0.465 | <.001 | 0.216 |
| CVD Diagnosis (referent, ACS only) | LOR | 95% Confidence Interval | P value | RRR | |
| ACS with CHF history | 0.047 | −0.293 | 0.198 | .70 | 1.049 |
| ADHF at index hospitalization | 0.303 | 0.051 | 0.554 | .02 | 0.739 |
| b paths: Mediator → 1-year mortality | Unstandardized | Standardized | |||
|---|---|---|---|---|---|
| LOR | 95% Confidence Interval | P value | AOR for SD increase | ||
| Health Competence | −0.064 | −0.127 | 0.001 | .05 | 0.866 |
| Health Behavior | −0.126 | −0.240 | −0.124 | .03 | 0.837 |
| Social Support | 0.008 | −0.100 | 0.116 | .89 | 1.013 |
| Comorbidities | 0.041 | 0.027 | 0.055 | <.001 | 1.464 |
| Prior Year Hospitalizations | 0.102 | 0.051 | 0.152 | <.001 | 1.241 |
| CVD Diagnosis (ACS only, referent) | LOR | 95% Confidence Interval | P value | AOR | |
| ACS with CHF history | 1.146 | 0.612 | 1.680 | <.001 | 3.146 |
| ADHF at index hospitalization | 2.049 | 1.554 | 2.543 | <.001 | 7.760 |
All models adjusted for covariates: age, gender, minority status, and socioeconomic status; a paths show effect of lower health literacy on each mediator in separate models adjusted for all other mediators, b paths show effect of each mediator on 1-year mortality in single model adjusted for all mediators and health literacy. β, standardized regression coefficients, represent the standard deviation change in the outcome associated with each standard deviation decrease in health literacy; LOR, log odds ratio; AOR for SD increase, the adjusted odds ratio (AOR) for a one standard deviation (SD) increase in the predictor.
Table 3 shows results from the multiple mediator model (Figure 1B) including: AORs and 95% CIs for the total, direct, and indirect effects and covariates. For the indirect effects, AORs inform which effects are significantly different from zero but are not substantively meaningful; APEs are presented for substantive interpretation. Lower HL was associated with a higher probability of 1-year mortality in the base model (total effect AOR=1.31, CI [1.01, 1.69]). When mediators were included, there was no direct effect of HL on 1-year mortality (AOR=0.87, CI [0.66, 1.14]). Therefore the relationship between HL and 1-year mortality was driven by the mediators (total indirect effect AOR=1.50, CI [1.35, 1.67]); each SD decrease in HL was associated with a 3.2 percentage point increase (absolute difference) in the probability of death within 1 year through its association with the mediators. The mediators contributing most to the indirect effect were ADHF at index hospitalization (contributing an absolute 1.69 percentage points) and comorbidities (absolute 0.54 percentage points), but health behavior (0.44), health competence (0.42), and prior year hospitalizations (0.38) each contributed as well. Neither social support nor a history of CHF among those hospitalized for ACS mediated the effect of HL on mortality. Older age and lower SES independently predicted 1-year mortality.
Table 3.
Multiple mediator model of lower health literacy effects on 1-year mortality, with contributions of each mediator to the indirect effect, adjusted for covariates.
| AOR | 95% Confidence Interval | APE (%) | |
|---|---|---|---|
| Total Effect (c) | 1.31 | 1.01, 1.69 | 2.11 |
| Direct Effect (c’) | 0.87 | 0.66, 1.14 | −1.10 |
| Indirect Effect (ab) | 1.50 | 1.35, 1.67 | 3.20 |
| Decomposition of Indirect Effect | |||
| via Health Competence | 1.07 | 1.02, 1.13 | 0.42 |
| via Health Behavior | 1.06 | 1.01, 1.11 | 0.44 |
| via Social Support | 1.00 | 0.99, 1.01 | −0.01 |
| via Comorbidities | 1.06 | 1.04, 1.10 | 0.54 |
| via Prior Year Hospitalizations | 1.05 | 1.03, 1.08 | 0.38 |
| via CVD Diagnosis (ACS only, referent) | |||
| ACS with CHF history | 0.97 | 0.95, 1.00 | −0.26 |
| ADHF at index hospitalization | 1.27 | 1.18, 1.37 | 1.69 |
| Covariates | |||
| Age (10 years) | 1.30 | 1.18, 1.42 | na |
| Male | 1.13 | 0.86, 1.48 | na |
| Minority | 0.74 | 0.52, 1.05 | na |
| Socioeconomic Status (SD increase) | 0.81 | 0.68, 0.96 | na |
Results calculated using Karlson, Holm, and Breen method and 95% confidence intervals bias corrected with 5,000 bootstraps. AOR, adjusted odds ratio; APE, average partial effects interpreted as the absolute percentage point change in the outcome associated with a standard deviation decrease in health literacy; na, not available; SD, standard deviation.
Discussion
We examined hypothesized mediators of the effects of HL on 1-year mortality among adults hospitalized with CVD and extended research on the HL-mortality relationship among patients with CHF to include those with ACS. The mechanisms by which lower HL placed patients with CVD at greater risk for post-discharge mortality included greater likelihood of a CHF exacerbation, more comorbidities, more previous hospitalizations, lower perceived health competence, and worse health behaviors. The effect of HL via these mediators (the indirect effect) was sizable – each SD reduction in HL was associated with an average absolute increase of 3.2 percentage points in 1-year mortality. At extremes (±2 SDs from the mean), a patient with very low HL would be, on average, 12.8% more likely to die within 1 year of hospitalization for CVD than a patient with very high HL, after adjustment for age, gender, minority status, and SES. Although we expected social support to mitigate some of the risk associated with low HL, social support, as operationalized in this analysis, did not mediate the effect of HL on 1-year mortality. After adjustment for mediators, HL no longer predicted mortality (nonsignificant direct effect), but older age and lower SES remained significant predictors of 1-year mortality post-discharge.
In this study, the magnitude of the relationship between HL and mortality was similar to other published reports among community-dwelling adults (adjusted hazard ratios 1.526, 1.757) and among adults with CHF (adjusted hazard ratios 1.3410, 1.948, 1.919, 11). The relationship between lower HL and mortality in our sample of inpatients with CVD (where 39.2% had ACS only) was consistent with McNaughton et al.’s10 finding among inpatients with CHF (1.31 total and 1.50 indirect effects as compared to 1.34, respectively). Our examination is the most robust exploration of the HL and mortality relationship in terms of our measurement of HL and the social, behavioral and clinical determinants included. Our use of a latent variable to operationalize HL aligns with conceptual definitions3, 4 by including reading comprehension, self-rated ability to perform health care tasks, numeracy, and education. Other studies have used single measures assessing only reading ability6, 7, 11 or subjective self-report.8–10 Because measures of HL agree less than half the time in identifying those with low HL,54 use of single measures can substantively impact findings.
Strengths & Limitations
This study is the first to examine mediators of the relationship between HL and mortality to elucidate causal pathways and guide interventions. Strengths include use of a latent variable approach that overcomes bias and shortcomings associated with individual measures for a more robust estimation of important constructs such as HL, social support and SES. We also collected mortality data comprehensively by confirming all deaths using multiple sources. We used a previously hypothesized causal model13 to select mediators and covariates, although we acknowledge that different relationships could be posited. For instance, HL likely influences and is influenced by access to care (e.g., insurance status), health care utilization, and SES. Other limitations include the possibility of unmeasured confounders, use of self-report for health behaviors, single time-point assessments for social and behavioral mediators, and not examining causal paths between the mediators (e.g., social support could lead to improved health behavior which, in turn, could lead to lower mortality risk). Furthermore, we excluded patient-provider level variables that could mitigate effects of low HL on mortality, such as trust and communication quality. This study was performed at a single referral hospital in the southeast United States; however, participants resided in 20 states. Results should be replicated in samples with more racial/ethnic minorities.
Clinical Implications
Among adults with CVD, increasing perceived health competence and improving health behaviors may mitigate some of the risk associated with low HL, independent of clinical risk factors (i.e. comorbidities, CVD diagnosis, prior hospitalizations). Interventions such as health coaching55 and cardiac rehabilitation56 improve perceived health competence and health behaviors and may be particularly effective at reducing risk for post-discharge mortality when effectively delivered to patients with lower HL. These findings suggest patients screened to have low HL while hospitalized with CVD should further be assessed for perceived health competence and health behaviors to inform delivery of appropriate targeted interventions (e.g., health coaching for smoking cessation and dietary modifications; cardiac rehabilitation for individualized exercise programs; counseling for treatment of alcohol abuse) based on the patients’ specific health behaviors and requisites for management of their cardiovascular condition. Identification of adults with limited HL or low perceived health competence can be a first step to providing tailored interventions targeting these modifiable constructs to prevent poor outcomes, though future research studies with such interventions would be needed for confirmation. Additionally, low HL may exert its strongest effects on mortality risk via the development of worsening health over the life course, suggesting identification of limited HL early in life is critical, and future research should explore the causal mechanisms linking lower HL to development of CVD and other conditions.
Acknowledgments
Dr. Mayberry planned and executed the analyses and wrote the manuscript in collaboration with Drs. Schildcrout, Wallston, and Kripalani. Ms. Goggins together with Drs. Kripalani, Wallston, Schildcrout, Rothman, and Mixon participated in protocol development and data collection for the VICS study and participated in discussions about the analysis plan and results. Dr. Kripalani is the principal investigator for the VICS study and conceived of the research question for this analysis. All authors read and edited drafts of the manuscript, including the final draft. All authors have access to the data.
Financial support and conflict of interest disclosure: The VICS study was supported by grant R01 HL109388 from the National Heart, Lung, and Blood Institute and in part by grant 2 UL1 TR000445–06. Dr. Mayberry was supported by a career development award from the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK106306). Dr. Mixon was supported by Career Development Award 12–168 from the United States Department of Veterans Affairs Health Services Research and Development Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Department of Veterans Affairs. The funding agencies were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; nor preparation, review, or approval of the manuscript. Dr. Wallston and Dr. Rothman serve on the advisory board for EdLogics, a healthcare company that addresses health literacy in web-based health education. The authors disclose no other potential conflicts of interest.
Abbreviations:
- ACS
acute coronary syndromes
- ADHF
acute decompensated heart failure
- APE
average partial effects
- BHLS
Brief Health Literacy Screen
- CHF
congestive heart failure
- CVD
cardiovascular disease
- DMF
Death Master File
- ENRICHD
Enhancing Recovery in Coronary Heart Disease Social Support Inventory
- KHB
Karlson, Holm, and Breen method
- HL
health literacy
- SD
standard deviation
- SEM
structural equation modeling
- SES
socioeconomic status
- SNS-3
Subjective Numeracy Scale 3-item version
- S-TOFHLA
short form of the Test of Functional Health Literacy in Adults
- VICS
Vanderbilt Inpatient Cohort Study
Footnotes
Vanderbilt Inpatient Cohort Study:
Faculty:
Sunil Kripalani, MD, MSc, SHM (Principal Investigator); Justin Bachmann, MD, MPH; Susan P. Bell, MBBS, MSCI; Katharine M. Donato, PhD; Frank E. Harrell, PhD; Lindsay Mayberry, MS, PhD; Amanda S. Mixon, MD, MS, MSPH; Russell L. Rothman, MD, MPP; Jonathan S. Schildcrout, PhD; John F. Schnelle, PhD; Eduard E. Vasilevskis, MD, MPH; Kenneth A. Wallston, PhD
Senior staff:
Courtney Cawthon, MPH; Kathryn Goggins, MPH; Samuel K. Nwosu, MS
References
- 1.Riegel B, Moser DK, Anker SD, et al. State of the Science. Circulation. 2009;120(12):1141–1163. [DOI] [PubMed] [Google Scholar]
- 2.Evangelista LS, Rasmusson KD, Laramee AS, et al. Health literacy and the patient with heart failure—implications for patient care and research: a consensus statement of the Heart Failure Society of America. J Card Fail. 2010;16(1):9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155(2):97–107. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen-Bohlman L, Panzer A, Kindig D. Health literacy: a prescription to end confusion. Washington, DC: The National Academies Press, 2004. [PubMed] [Google Scholar]
- 5.Ventura HO, Piña IL. Health Literacy: An Important Clinical Tool in Heart Failure. Mayo Clin Proc 2017;93(1):1–3 [DOI] [PubMed] [Google Scholar]
- 6.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med 2007;167(14):1503–1509. [DOI] [PubMed] [Google Scholar]
- 7.Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med 2006;21(8):806–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabbri M, Yost K, Rutten LJF, et al. Health literacy and outcomes in patients with heart failure: a prospective community study. Mayo Clin Proc. 2018; 93(1):9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc 2015;4(5):e001799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21(8):612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Melo Ghisi GL, da Silva Chaves GS, Britto RR, Oh P. Health literacy and coronary artery disease: a systematic review. Patient Educ Couns 2018;101(2):177–184. [DOI] [PubMed] [Google Scholar]
- 13.Meyers AG, Salanitro A, Wallston KA, et al. Determinants of health after hospital discharge: rationale and design of the Vanderbilt Inpatient Cohort Study (VICS). BMC Health Serv Res 2014;14(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calvillo–King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med 2013;28(2):269–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav 2007;31(1):S19–S26. [DOI] [PubMed] [Google Scholar]
- 16.Dennison CR, McEntee ML, Samuel L, et al. Adequate health literacy is associated with higher heart failure knowledge and self care confidence in hospitalized patients. J Cardiovasc Nurs 2011;26(5):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. J Gen Intern Med 2004;19(12):1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray M, Tu W, Wu J, Morrow D, Smith F, Brater D. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther 2009;85(6):651–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns 2016;99(2):287–294. [DOI] [PubMed] [Google Scholar]
- 20.Brega AG, Ang A, Vega W, et al. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Educ Couns 2012;88(1):61–68. [DOI] [PubMed] [Google Scholar]
- 21.Lee EH, Lee YW, Moon SH. A structural equation model linking health literacy to self-efficacy, self-care activities, and health-related quality of life in patients with type 2 diabetes. Asian Nurs Res 2016;10(1):82–87. [DOI] [PubMed] [Google Scholar]
- 22.Osborn CY, Paasche-Orlow MK, Bailey SC, Wolf MS. The mechanisms linking health literacy to behavior and health status. Am J Health Behav 2011;35(1):118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun X, Shi Y, Zeng Q, et al. Determinants of health literacy and health behavior regarding infectious respiratory diseases: a pathway model. BMC public health. 2013;13(1):261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adams RJ, Piantadosi C, Ettridge K, et al. Functional health literacy mediates the relationship between socio-economic status, perceptions and lifestyle behaviors related to cancer risk in an Australian population. Patient Educ Couns 2013;91(2):206–212. [DOI] [PubMed] [Google Scholar]
- 25.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun 2010;15(S2):146–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med 2011;26(9):979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho YI, Lee S-YD, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med 2008;66(8):1809–1816. [DOI] [PubMed] [Google Scholar]
- 28.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;11:12. [PubMed] [Google Scholar]
- 29.Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med 2014;29(1):119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nurss J, Parker R, Williams M, Baker D. Directions for administration and scoring and technical data, short test of functional health literacy in adults (STOFHLA-English and STOFHLA-Spanish). Center for the Study of Adult Literacy. 1998. [Google Scholar]
- 31.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. J Gen Intern Med 1995;10(10):537–541. [DOI] [PubMed] [Google Scholar]
- 32.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. [DOI] [PubMed] [Google Scholar]
- 33.Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27(5):663–671. [DOI] [PubMed] [Google Scholar]
- 34.McNaughton CD, Cavanaugh KL, Kripalani S, Rothman RL, Wallston KA. Validation of a short, 3-item version of the Subjective Numeracy Scale. Med Decis Making. 2015;35(8):932–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osborn CY, Kripalani S, Goggins KM, Wallston KA. Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients. J Health Care Poor Underserved. 2017;28(1):499–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey questionnaire. Atlanta, GA; 2010. [Google Scholar]
- 37.Smith MS, Wallston KA, Smith CA. The development and validation of the Perceived Health Competence Scale. Health Educ Res 1995;10(1):51–64. [DOI] [PubMed] [Google Scholar]
- 38.Bachmann JM, Goggins KM, Nwosu SK, Schildcrout JS, Kripalani S, Wallston KA. Perceived health competence predicts health behavior and health-related quality of life in patients with cardiovascular disease. Patient Educ Couns 2016;99(12):2071–2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003. [DOI] [PubMed] [Google Scholar]
- 40.Mitchell PH, Powell L, Blumenthal J, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil 2003;23(6):398–403. [DOI] [PubMed] [Google Scholar]
- 41.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009:626–633. [DOI] [PubMed] [Google Scholar]
- 42.Research, Statistics, & Policy Analysis. ssa.gov. http://www.ssa.gov/policy/about/epidemiology.html. Accessed June 30, 2017.
- 43.Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med 2001;344(19):1443–1449. [DOI] [PubMed] [Google Scholar]
- 44.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297(10):1063–1072. [DOI] [PubMed] [Google Scholar]
- 45.Hernandez LM. Measures of health literacy: Workshop Summary. National Academies Press; 2009. [PubMed] [Google Scholar]
- 46.Kline RB. Principles and Practices of Structural Equation Modeling. 4th ed. New York, NY: The Guilford Press; 2016. [Google Scholar]
- 47.Little RJ, Rubin DB. Statistical analysis with missing data. John Wiley & Sons; 2014. [Google Scholar]
- 48.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication monogr 2009;76(4):408–420. [Google Scholar]
- 49.Karlson KB, Holm A. Decomposing primary and secondary effects: a new decomposition method. Res Soc Stratif Mobil 2011;29(2):221–237. [Google Scholar]
- 50.Karlson KB, Holm A, Breen R. Comparing regression coefficients between same-sample nested models using logit and probit: A new method. Sociological Methodol 2012;42(1):286–313. [Google Scholar]
- 51.Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models. Stata J. 2011;11(3):420–438. [Google Scholar]
- 52.Breen R, Karlson KB, Holm A. Total, direct, and indirect effects in logit and probit models. Sociol Methods Res 2013;42(2):164–191. [Google Scholar]
- 53.Chernick MR. Bootstrap methods: A practitioner’s guide. 2nd ed. New York: John Wiley & Sons; 2008. [Google Scholar]
- 54.Osborn CY, Weiss BD, Davis TC, et al. Measuring adult literacy in health care: performance of the newest vital sign. Am J Health Behav 2007;31(1):S36–S46. [DOI] [PubMed] [Google Scholar]
- 55.Coleman EA, Parry C, Chalmers S, Min S-j. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166(17):1822–1828. [DOI] [PubMed] [Google Scholar]
- 56.Rodgers WM, Murray TC, Selzler A-M, Norman P. Development and impact of exercise self-efficacy types during and after cardiac rehabilitation. Rehabil Psychol 2013;58(2):178. [DOI] [PubMed] [Google Scholar]