Abstract
Background and Aims:
Selection of an appropriate endotracheal tube (ETT) in paediatric patients is a challenging situation. The purpose of this study was to compare whether measurement of subglottic diameter with ultrasound or the age-old little finger width correlates better with the outer diameter (OD) of the ETT used for intubation.
Methods:
Following approval from the Institutional Ethics board and a written informed consent from parent or guardian, this prospective observational study was carried out on 60 American Society of Anesthesiologists physical status I and II patients aged 6 months–8 years, scheduled for elective surgery under general anaesthesia requiring oral endotracheal intubation. Preoperatively ultrasound-guided subglottic diameter (USGD) and little finger breadth (LFB) measurements were taken. On the day of surgery, intubation was done with an uncuffed ETT, whose OD was noted. The concordance and agreeability between two techniques for estimation of the OD of the ETT were measured by Lin's concordance correlation coefficient. Further, the bias and precision between the techniques and the inter-changeability of the techniques were assessed by using Bland and Altman and Mountain plotting, respectively.
Results:
Lin's concordance correlation coefficient between USGD and LFB with the OD of the ETT was found to be 0.29 (0.13–0.41) and 0.46 (0.29–0.6), respectively.
Conclusion:
Overall, neither USGD nor LFB can be used as a reliable tool to predict the OD of the ETT. Registered in Clinical Trial Registry of India. REF/2016/08/011955.
Key words: Endotracheal tube, little fingerbreadth, outer diameter, paediatrics, ultrasound-guided subglottic diameter
INTRODUCTION
Management of the paediatric airway is often stressful and challenging to the anaesthesia providers. Selection of an appropriate endotracheal tube (ETT) is a crucial step in paediatric airway management failure, which may lead to various complications. Bigger size tubes are difficult or impossible to pass through the airway. It may result in complications like airway damage (e.g., ulceration, local ischaemia or scar formation), increased incidence of post-operative sore throat, glottic oedema and subglottic stenosis. Similarly, smaller size tubes may result in accidental extubation, gas leaks thus resulting in inadequate delivery of tidal volume, increased theatre pollution and increased risk of aspiration.
Various simple methods are used to calculate the ETT size to be used for intubation which includes physical indices-based formulas,[1,2,3] little and index finger breadth.[4,5] Recent advances which aid us for the same are videobronchoscopy,[6,7] magnetic resonance imaging (MRI) and ultrasonography (USG).[6,7,8,9]
As it is the outer diameter (OD) of ETT which fits in the tracheal lumen, knowledge of the same is essential to get proper sized ETT. Many of the formulas predict the inner diameter (ID) of the ETT, whereas finger breadth and USG both predict the OD of the tube. Hence, comparison between little finger breadth (LFB) and ultrasound-guided subglottic diameter (USGD) looks more logical as both give the idea of the same parameter, that is, the OD of the ETT. As the narrowest part of paediatric upper airway is subglottis at the cricoid level, an appropriately sized uncuffed tube provides a proper and an adequate seal in children younger than 8 years of age.[10] Hence, we have used only uncuffed tubes in our study and upper age limit of the participants was taken as 8 years. In the present study, USGD was measured and little fingerbreadth was measured at the level of distal inter-phalangeal crease and it was observed whether and which of these measurements were in better correlation with the OD of the ETT clinically used for intubation. The hypothesis for this study: null hypothesis states that there is no difference between the two techniques for correlation with the OD of the ETT clinically used and alternative hypothesis states that one technique is not equal to the other technique for correlation with the OD of the ETT clinically used.
METHODS
Following approval from the Institutional Ethics Board, registration with CTRI (REF 2016/08/011955) and a written informed consent from parent or guardian, this prospective observational study was carried out on 60 ASA I and II (American Society of Anesthesiologists physical status classification system) patients aged 6 months–8 years, of either sex, scheduled for elective surgery under general anaesthesia (GA) requiring oral endotracheal intubation. This study adheres to the STROBE guidelines. Exclusion criteria included patients with ASA III and above, patients suffering from any respiratory disease that might cause airway narrowing, pre-existing laryngeal or tracheal pathology, any lesion that could cause airway deformity due to fibrosis and anticipated difficult airway. All the patients under the study had undergone pre-anaesthetic check-up and USG of the neck the day before surgery. USG (My Lab™ Seven EsaoteeHD Technology, Esaote S.p.A, Italy) was performed by a single experienced radiologist for every case. Patient was kept in supine position with head in slight extension. There was a possibility of respiratory-induced changes in airway dimensions. To avoid that, older and cooperative children were asked to take a slow inspiration when radiologist was taking the measurements. USG was done with linear probe (frequency 7–15 MHz) and measurements were taken in B-mode. The probe was placed on the midline of the anterior neck. At first, true vocal folds were located and identified as paired hyper-echoic linear structures moving with respiration and swallowing. Later, cricoid arch was identified by moving the probe caudally. Cricoid arch appears as a round hypo-echoic structure with hyper-echoic edges. The air column appears hyper-echoic. The subglottic diameter was measured by the transverse measurement of the air column obtained in cephalad half of cricoid arch [Figure 1].
Figure 1.
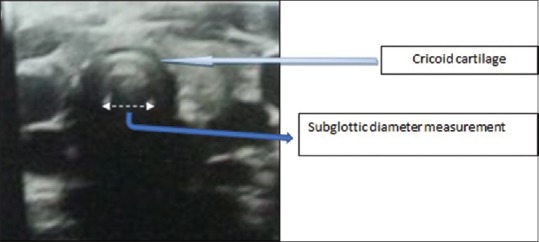
Ultrasonogram showing measurement of SGD. SGD = Subglottic diameter
Little finger measurement: Preoperatively, breadth of distal phalanx of little finger at the level of distal inter-phalangeal groove of all the patients was measured with the help of vernier calliper.
On the day of surgery, patient was wheeled into the operation theatre and monitors connected according to ASA guidelines. After giving premedication, all the patients were induced and administered muscle relaxant as per the institutional protocol. The intubating anaesthesiologist was blinded to the results of the ultrasound examination and little finger measurements. The size of uncuffed ETT for intubation for that particular patient was selected and intubation procedure was performed by an experienced anaesthesiologist. If some resistance was felt at the time of introduction of ETT, a tube smaller by 0.5 mm was chosen. On the other hand, a larger tube by 0.5 mm was chosen, if there was air leak at 20 cmH2O of peak inspiratory pressure and low expired tidal volume of less than 7 ml/kg. In order to avoid manufacturer-related discrepancies in OD measurements of ETT, we have used ETTs from a single manufacturer (Portex tracheal tube; Smiths Medical International Ltd., Kent, UK) for all the patients included in the study. Study was concluded at this point. The recorded data include the OD and ID of the finally selected and placed ETT, USGD and LFB. The primary objective of our study was correlation of USGD with the clinically selected OD of ETT used and secondary objectives include correlation of LFB with clinically used ETT and correlation of USGD with LFB.
There were no studies in the literature where three techniques of ETT estimation were compared. A pilot study was carried out on 12 patients. PASS 13 statistical software was used for calculating the power and sample size. Taking the mean difference of 0.1 between the two, a sample size was estimated to be around 60 with 80% power using a two-sided hypothesis test with a significance level of 0.05.
Statistical analysis was compiled with NCSS version 9 and MedCalc trial version 14.8.1.0 software. The results of the data were displayed as mean with standard deviation. Normality of the data was assessed by the Shapiro–Wilk test. A difference of ≤0.3 mm between the tested methods (USG, LFB) and the OD of the correct ETT size was considered as an acceptable difference.[11] Inter-changeability of techniques was assessed by plotting values obtained by each of the techniques against values of the actual OD of the ETT used. The concordance and agreeability between two techniques for estimation of ETT size were measured by Lin's concordance correlation coefficient. Values of ±1 denote perfect concordance and discordance; a value of zero denotes its complete absence. Bias and precision between the techniques were assessed by using Bland and Altman plotting.[12] Further, to assess the inter-changeability of the techniques, mountain plot tool was used as a complementary to Bland and Altman plotting. A P value of <0.05 was considered significant.
The study was registered in Clinical Trial Registry of India. REF/2016/08/011955
RESULTS
A total of 60 children (30 boys and 30 girls), who underwent elective surgeries under GA requiring oral endotracheal intubation, were included in the study. No patients were excluded. All the 60 patients underwent USG without any major technical issues except for inability of maintaining shallow respiration during the procedure in children less than 5 years of age (a total of 35 children). Average time taken for each patient to undergo the procedure was not more than 3 min. The demographic data displayed mean ± SD values of age, weight, height and body mass index (BMI) of 54.7 ± 47 months, 14.4 ± 5.9 kg, 0.9 ± 0.2 m and 18.21 ± 1.9 kg/m2, respectively. The data were found to be normally distributed (Shapiro–Wilk) with respect to BMI (P = 0.85) and age (P = 0.44). But height (P = 0.007) and weight (P = 0.006) were not normally distributed. As this is a growing age population, height and weight were expected to display abnormal distribution with imbalance in variance.
Lin's concordance correlation coefficient for comparison of USGD and LFB measurements with OD of the correct ETT between different methods is depicted in Figures 2 and 3. Out of 60 children, acceptable difference (≤0. 3 mm) between OD of correct sized ETT and USG was observed in 23% cases (CI 6.5–29.4%), and with LFB, it was 18.33% (CI 7.4–28.5%).
Figure 2.
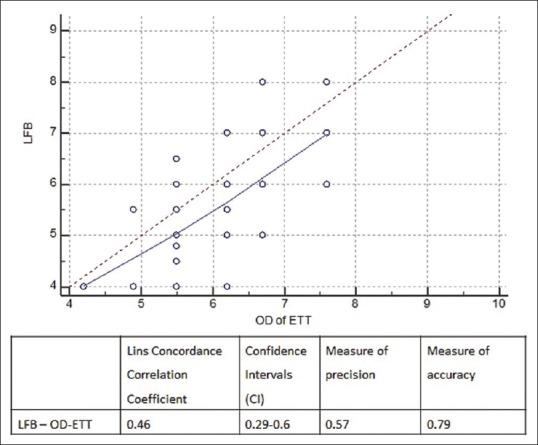
Graph showing Lin's concordance correlation coefficient between LFB with OD of ETT used. LFB = Little finger breadth; OD = Outer diameter; ETT = Endotracheal tube
Figure 3.
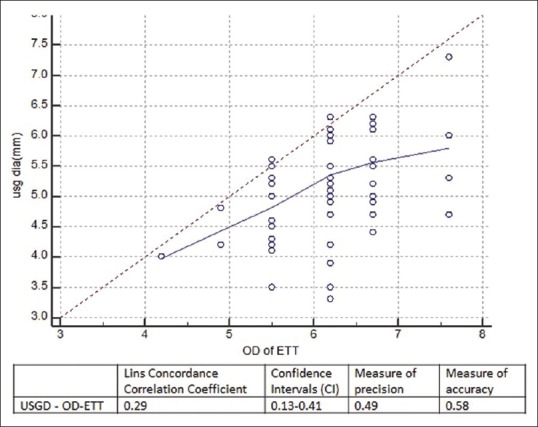
Graph showing Lin's concordance correlation coefficient between USGD with OD of ETT used. USGD = Ultrasound-guided subglottic diameter; OD = Outer diameter; ETT = Endotracheal tube
Bland and Altman analysis plot of LFB and OD of actual ETT used shows a mean difference of 0.44 mm (CI 0.1898–0.6935) [Figure 4]. The upper and lower limits of agreement (2 SD) were +2.35 and −1.47, respectively (P value = 0.0009). This displayed distribution of values mostly within the limits of agreement, but this was not the same with USG. Similarly, the plot of USG measured OD and OD of actual ETT showed a mean difference of 0.95 mm (CI 0.74–0.15) [Figure 5]. The upper and lower limits of agreement (2 SD) were +2.5 and −0.6, respectively. This too was statistically significant (P value of <0.0001). Values of LFB and USG appear to be distributed in almost a similar range of distribution (±1.96 for LFB and ± 1.6 for USG).
Figure 4.
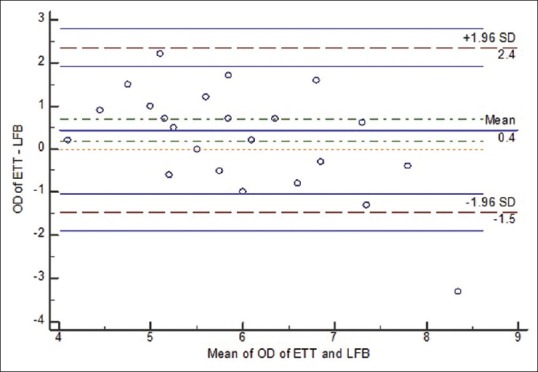
Bland–Altman plot for LFB and Od of ETT. LFB = Little finger breadth; OD = Outer diameter; ETT = Endotracheal tube
Figure 5.
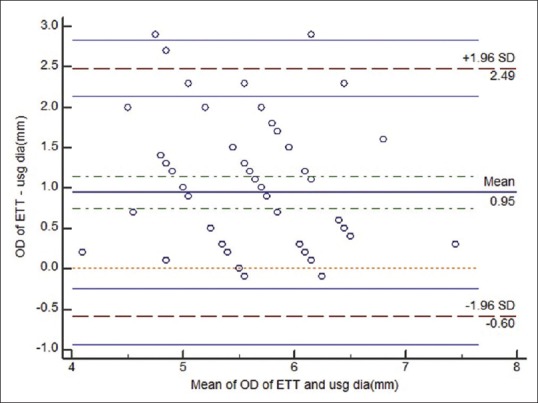
Bland–Altman plot for USG and OD of ETT. USGD = Ultrasound-guided subglottic diameter; OD = Outer diameter; ETT = Endotracheal tube; SD-standard deviation
Mountain plot gives a visual correlation of agreement and inter-changeability between techniques. Observations were made based on the comparison of shape of one mountain with the other. The median between actual OD-ETT and LFB-OD and USG-OD as assessed by mountain plots was 0.5 and 0.8, respectively [Figure 6]. The methods of measurement would be classified in the decreasing order of accuracy as follows: actual OD-ETT > LFB-OD > USG-OD. Absence of inter-changeability, which occurred with the techniques, was seen as either the base or the apex of the mountain not aligning exactly with each other.
Figure 6.
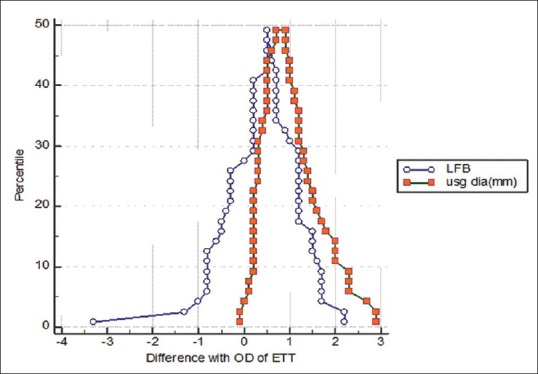
Mountain plot showing curves for USGD, LFB and OD of ETT values. USGD = Ultrasound-guided subglottic diameter; LFB = Little finger breadth; OD = outer diameter; ETT = Endotracheal tube; SD-Standard deviation
DISCUSSION
The primary objective of this study was to check for the reliability and usefulness of USGD and LFB in selecting an appropriate ETT for tracheal intubation. In our study, it was observed that ultrasound was consistently underestimating the OD of the ETT. The correlation coefficient was also very poor. Even the LFB values were not comparable to OD of ETT used. Though the correlation for LFB with OD of ETT was not good, it was better than that of USGD as depicted in the mountain plot. Most of the recent studies emphasised that the ultrasound was a reliable tool in measuring subglottic diameter, thereby predicting the OD of ETT.
In 2012, Gupta et al.[13] conducted a prospective clinical study in India for assessment of the subglottic region by USG for estimation of an appropriate size ETT. The relationship between calculated external diameters of the ETT from physical indices of age-based formulas, one that was predetermined by ultrasound and the third one, clinically used ETT for intubation during GA was observed. By the Bland–Altman analysis, the rate of agreement between clinically optimal and ultrasound-guided ETT was 98% (P < 0.001). USG was found to be a better tool for the assessment of the subglottic diameter of trachea in children to estimate the appropriate size ETT for intubation. In this study, they recruited 112 patients aged between 3 and 18 years, out of which only 18 patients were under 5 years of age, 35 patients were between 6 and 10 years and 59 patients were above the age of 10 years. So, we can observe that more than 50% of the patients are above 10 years. As already discussed in the literature, the airway stabilises to the adult form after 8 years of age.[14] Inclusion of diversified age groups can be considered as a limitation to this study. On the other hand, in our study, we have included patients aged 6 months–8 years where the airway is in the active growing phase. In our study, patient's comprehension was important to a certain extent as he was asked to take slow inspiration during the period of measurement of SGD in order to avoid respiratory-induced changes in airway dimensions. Comprehensive abilities increase with age. On most of the occasions, we could not achieve this task as participants in our study were much younger to those in study by Gupta et al. which could have led to inaccurate results in our study. Moreover, growth changes are more rapid during first 10 years of life after which the growth curve becomes more sustained. So, in patients above 10 years of age, there is a possibility for ultrasound to give consistent results which was reflected in the respective study.
The results of another study conducted by Schramm et al.[11] which was claimed to be the first European study to examine the role of ultrasound for prediction of correct uncuffed tube sizes. The comparator was age-related formulas for uncuffed endotracheal intubation in a paediatric population. The findings stated that the rate of irrelevant differences between the correctly sized ETT and the two different age-based formulas ID [mm] = 4.0 + (age [years]/4) (formula ‘4.0’) and ID [mm] = 4.5 +(age [years]/4) (formula ‘4.5’) with a maximum allowed deviation of ≤0.3 mm was 24% (95% CI, 13.0–38.2%) and 40% (95% CI, 26.4–54.9%), whereas ultrasound measurement of minimal transverse diameter of the subglottic airway (MTDSA) correctly predicted ETT in 48% (95% CI, 33.6–62.6%) of the cases. The results showed that ultrasound-guided MTDSA measurement facilitated selection of an appropriate ETT in paediatric patients. This study differed from our study in the timing of performing USG. In this study, USG was performed on the day of surgery during mask ventilation after inducing the patient, whereas in our study, USG was performed preoperatively the day before surgery when patient was fully awake and on spontaneous respiration. As both the methods were different, comparability of their results is questionable.
Lakhal et al.[15] compared the transverse diameter of the cricoid lumen assessed by USG and MRI and found a strong correlation between the two techniques (r = 0.99, P < 0.05). However, the participants were all adults in contrast to our study which included only paediatric age group.
A novel study was conducted in Korea where the investigators have developed an equation based on USG measurement of subglottic diameter to predict appropriate ETT.[16] The efficacy of the new equation was evaluated by comparing it with the conventional age-based formula (4 + age/4) in another 100 patients. The USG method allowed the correct tube size to be selected in 60% of cases, whereas the age-based method enabled this in 31% of cases (P < 0.001). The authors attributed the inefficiency of USG in 40% of cases to the following reasons: first, USG measures only the transverse diameter of the trachea at one level. Second, the external diameter of tracheal tubes varies according to the manufacturer, and thus, the tracheal tube size used must be assessed on an individual basis, and finally, diameter measurements are subject to variation and are also time consuming. In contrast to the above said studies, Husein et al.[7] have come up with conflicting results. In their study, they have compared ultrasound and a new video bronchoscopic technique to measure the subglottic diameter in paediatric population. They have concluded that video bronchoscopy was superior to USG in measuring subglottic diameter. They have also observed that USG always underestimated the size of the lumen and inferred that USG may be a poor method for absolute measurement. Results of this study were in agreement with our findings.
Most of the results from studies involving LFB measurements to predict the ETT size were in agreement with the observations in our present study. Study by van den Berg et al.[4] in 1997 has shown that the diameter of the terminal phalanx of little or index finger was a poor predictor of the external diameter of ETT that provided the best fit. King Br et al. have also made similar conclusions that neither fifth finger breadth nor fifth finger diameter accurately predicts proper ETT size in most children. Their study suggested that a more accurate estimation can be made using the age-based formula. However, breadth of the fifth finger nail can be of help when the child's age is unknown or when calculation is awkward or impossible.[5]
In our study, mountain plot figure displayed a better correlation of actual OD ETT with LFB compared to USG in our study. Hence, LFB may be useful as it is cost effective, especially in patients where age is unknown.
Our study has some limitations. First, children were unable to maintain slow respiration of the patients during USG measurements to avoid respiratory-induced changes in airway dimensions; this might have led to inaccurate measurements. USG in the intraoperative period after induction also carries some error for calculation. Hence, this error could not be avoided in paediatric group patients. Second, antero-posterior measurement of the subglottis could not be measured using USG. And finally, minute variations in probe placements might have led to significant differences in the measurements. Others include use of uncuffed tubes in place of cuffed tubes and external diameter measurement instead of internal diameter for ETT size assessment. This was done intentionally for study purpose to avoid the bias of two different designs.
CONCLUSION
Neither USG nor LFB methods for measurement of ETT can be used as a reliable tool to predict the OD of ETT.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Senior Professors R. Gopinath, Dilip Kulkarni and other departmental staff for guiding us and helping us in completion of this study.
REFERENCES
- 1.Cole F. Pediatric formulas for the anesthesiologist. AMA J Dis Child. 1957;94:672–3. doi: 10.1001/archpedi.1957.04030070084009. [DOI] [PubMed] [Google Scholar]
- 2.Salgo B, Schmitz A, Henze G, Stutz K, Dullenkopf A, Neff S, et al. Evaluation of a new recommendation for improved cuffed tracheal tube size selection in infants and small children. Acta Anaesthesiol Scand. 2006;50:557–61. doi: 10.1111/j.1399-6576.2006.01003.x. [DOI] [PubMed] [Google Scholar]
- 3.Luten RC, Wears RL, Broselow J, Zaritsky A, Barnett TM, Lee T, et al. Length-based endotracheal tube and emergency equipment in pediatrics. Ann Emerg Med. 1992;21:900–4. doi: 10.1016/s0196-0644(05)82924-5. [DOI] [PubMed] [Google Scholar]
- 4.van den Berg AA, Mphanza T. Choice of tracheal tube size for children: Finger size or age-related formula? Anaesthesia. 1997;52:701–3. doi: 10.1111/j.1365-2044.1997.az0130c.x. [DOI] [PubMed] [Google Scholar]
- 5.King BR, Baker MD, Braitman LE, Seidl-Friedman J, Schreiner MS. Endotracheal tube selection in children: A comparison of four methods. Ann Emerg Med. 1993;22:530–4. doi: 10.1016/s0196-0644(05)81937-7. [DOI] [PubMed] [Google Scholar]
- 6.Giguere CM, Manoukian JJ, Patenaude Y, Platt R. Ultrasound and a new videobronchoscopic technique to measure the subglottic diameter. J Otolaryngol. 2000;29:290–8. [PubMed] [Google Scholar]
- 7.Husein M, Manoukian JJ, Platt R, Patenaude Y, Drouin S, Giguere C. Ultrasonography and videobronchoscopy to assess the subglottic diameter in the paediatric population: A first look. J Otolaryngol. 2002;31:220–6. doi: 10.2310/7070.2002.21697. [DOI] [PubMed] [Google Scholar]
- 8.Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113:819–24. doi: 10.1097/ALN.0b013e3181ef6757. [DOI] [PubMed] [Google Scholar]
- 9.Kim EJ, Kim SY, Kim WO, Kim H, Kil HK. Ultrasound measurement of subglottic diameter and an empirical formula for proper endotracheal tube fitting in children. Acta Anaesthesiol Scand. 2013;57:1124–30. doi: 10.1111/aas.12167. [DOI] [PubMed] [Google Scholar]
- 10.Cravero JP, Kain ZN. Clinical Anesthesia by Paul G Barash. 6 ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009. pediatric anesthesia; p. 1207. [Google Scholar]
- 11.Schramm C, Knop J, Jensen K, Plaschke K. Role of ultrasound compared to age-related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth. 2012;22:781–6. doi: 10.1111/j.1460-9592.2012.03889.x. [DOI] [PubMed] [Google Scholar]
- 12.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 13.Gupta K, Gupta P, Jain M, Krishan A, Rastogi B, Garg G. Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res. 2012;6:157–60. doi: 10.4103/0259-1162.108298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eckenhoff JE. Some anatomic considerations of the infant larynx influencing endotracheal anesthesia. Anesthesiology. 1951;12:401–10. doi: 10.1097/00000542-195107000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Lakhal K, Delplace X, Cottier JP, Tranquart F, Sauvagnac X, Mercier C, et al. The feasibility of ultrasound to assess subglottic diameter. Anesth Analg. 2007;104:611–4. doi: 10.1213/01.ane.0000260136.53694.fe. [DOI] [PubMed] [Google Scholar]
- 16.Bae JY, Byon HJ, Han SS, Kim HS, Kim JT. Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for paediatric patients. Anaesthesia. 2011;66:994–8. doi: 10.1111/j.1365-2044.2011.06900.x. [DOI] [PubMed] [Google Scholar]


