Abstract
Objective:
To validate the Hopkins Symptom Checklist-25 (HSCL-25) for use as a depression screen amongst human immuno-deficiency virus (HIV) positive pregnant women.
Method:
Amongst 903 (mean age 24.8 years) HIV-positive pregnant women, a two-phased design included measures for health-related quality of life, perceived social support, and the HSCL-25 screen for depressive (HSCL-15 subscale) and anxiety symptoms. The Structured Clinical Interview for DSM-IV (SCID) was independently administered on a stratified random subsample.
Results:
Internal consistency of the HSCL-25 (alpha 0.93) and HSCL-15 (alpha 0.9) was adequate, with expected findings demonstrated in discriminant validity analysis. A depression-anxiety construct explained nearly 40% of the variance. Eight individual HSCL-25 items demonstrated an area under the curve (AUC) greater than 0.6 for DSM-IV major depression and the HSCL-25 and HSCL-revised had an optimal depression cut-off score of 1.06 and 1.03 for the HSCL-15.
Conclusion:
The HSCL-25 demonstrated utility as a screen for depression; its inability to gauge severity of symptoms in this cultural context is discussed.
Keywords: HSCL-25 validation, depression, pregnant women and HIV
Introduction
Human immuno-deficiency virus (HIV) infection is chiefly a heterosexually transmitted disease, with the greatest burden falling on sub-Saharan Africa, accounting for over 70% of individuals living with HIV/acquired immuno-deficiency syndrome (AIDS) globally (1). Its ramifications for mental health include substantial disability from depressive disorder, to which socio-economically disadvantaged groups such as women are particularly vulnerable (2, 3). Yet most studies on depression and HIV infection have been conducted in western countries (4–6), on samples of well educated and gainfully employed mostly white homosexual men. Studies incorporating the use of structured and operational diagnostic criteria are almost all carried out in the US (7–10), and very few have been conducted among HIV-positive women (11, 12).
Depression may influence manifestations of HIV infection, through interference with motivation to obtain good medical care (13) as well as its associated immune dysfunction (14–16). There are, however, conflicting data regarding the contribution of depression to the course of HIV infection (17, 18), and the very nature of the association between HIV and depression has been questioned (19). Studies carried out outside the west (20–22) or with minority groups (23–25) suggest stronger associations between HIV and depression. Being female may confer enhanced risk for more rapid progression of HIV infection irrespective of reproductive status (26, 27); survival among men is 14% longer than survival among women at the same stage of illness (28), and HIV-positive women experience more distress than men, even within a monogamous relationship (29). The limited information on depression amongst pregnant women in the sub-Saharan African context, reveals about 24% of psychiatric morbidity, largely because of depression (30), the rate being about 10% when one focuses on depression alone (31).
Before approaching the subjects of associations and prevalence of depression, we must examine the problem of diagnostic methods and the utility of screening instruments. There are indications that standardized instruments vary in their intrinsic performance both across different population groups and cultures. These variations may be in part because of cultural differences, for example, a greater tendency to report psychological distress in somatized form in primary care settings has been reported in both western and non-western settings (32–36). While teasing out physiological vs. psychosocial causes for symptoms can be particularly complex in HIV-positive populations (37–39), stronger associations of symptoms with depression have implications for the clinical management of persons with HIV infection (40, 41). Studies exploring how a given population understands mental illness and what indigenous expressions and classifications they use can complement epidemiological investigations (42, 43). Additionally, the validity of any psychiatric instrument will depend on calibration for the population under study (44). Cut-off points for ‘caseness’ without renorming can result in inaccurate estimates as scores that are numerically identical can have psychologically different meanings across cultures (45, 46). The premise of this study illustrated by these analyses was that a simple screening tool can be helpful in detecting depression in a setting where resources for training are scarce and the prevalence of disease is high. While access to healthcare for women in developing countries is often limited, their routine presentation for prenatal care allows for consistent contact in the Tanzanian setting, and hence this population was targeted. This article provides analysis of data to validate and calibrate the Hopkins Symptom Checklist-25 (HSCL-25), for use amongst HIV-positive pregnant women in the primary care setting in Tanzania.
Material and methods
The sample
Between April 1995 and July 1997, 1078 HIV-positive pregnant women attending antenatal clinics in Dar es Salaam (Muhimbili, Mwananyamala, Temeke, Ilala and Mwenge Hospitals) were enrolled in a randomized controlled trial examining the effect of vitamin supplementation on perinatal transmission and progression of HIV. Resident women, with less than 27 weeks gestation (from the last menstrual period) who intended to stay in Dar es Salaam, were eligible to participate in the study. Fawzi et al. (47) provide information on the study design and methods in greater detail. The data used for this analysis are derived from 903 women with completed initial psychosocial information prior to delivery. Post-delivery data were excluded from these analyses to avoid confounding because of the likelihood of higher symptoms of psychological distress during the postpartum period.
A stratified random sample was selected for participation in a validation substudy based on HSCL-25 scores 3 months after enrolment. The first 50 women who had scored at first psychosocial assessment above the cut-off score of 1.75 for ‘caseness’ (48) on the depression subscale were recruited for a structured clinical interview for the DSM-IV diagnosis (SCID). During the same time period of recruitment a random sample of 50 women who had scored on or below the cut-off score of 1.75 were also asked to complete the SCID for the validation study.
Instruments
Socio-demographic and other background information were collected at baseline and psychosocial information at 3 months after baseline, 2 months after delivery, and every 6 months thereafter.
The psychosocial instrument comprised three scales. The HSCL-25 is a widely used screening measure that includes symptoms of anxiety (10 items) and depression (15 items) derived from the 90-item Symptom Checklist (SCL-90, 48–50). The 25-item version (HSCL-25), is scored on a severity scale from ‘1’ (not at all) to ‘4’ (extremely), and has demonstrated its usefulness as a screening tool in various cross-cultural settings (51–53), primary care settings (54, 55), and in family planning clients (56). In refugee populations sensitivity and specificity for detection of DSM III major depression were estimated as 88 and 73%, based on a cut-off score of 1.75 for ‘caseness’ (51). The Medical Outcomes Study Short Form-36 (SF-36) measured health-related quality of life on eight dimensions and has been shown to predict health outcomes over a period of time for a number of different clinical conditions. The SF-36 has been widely used in different cultural settings and has demonstrated good validity and reliability in different languages (57,58). The Kiswahili version of the SF-36 used in Dar es Salaam, Tanzania, revealed good internal consistency (Cronbach’s α ranging from 0.7 to0.92; median 0.81, 59), and expected variations in mean scores on its scales by age, gender, education level, socio-economic status and perceived morbidity and disability (60).
A 10-item perceived social support scale was derived from a questionnaire, designed ‘to measure functional elements of social support of patients in a primary care setting’ (61). Items were selected to reflect emotional/affective support (I get/have: visits from friends and relatives; useful advice about important things in my life; chances to talk to someone about problems at work or with my housework; chances to talk to someone I trust about my personal and family problems; people who care what happens to me; and love and affection) and material/instrumental support (I get/have: help around the house; help with money in an emergency; help when I need transportation; and help when I am sick). Overall test–retest reliability for the original scale was reported as 0.66 (61). However, this calculation excluded the items ‘help with transportation’ and ‘help with money’. These two items were retained in this study given their importance in this context.
SCID is a semistructured interview schedule with modules that reflect DSM-IV defined disorders. It closely mirrors the clinical diagnostic process that is employed by trained clinicians (62) and has demonstrated its validity and reliability among English speaking populations (63). Symptoms are rated in a format that allows for rephrasing and asking additional clarifying questions, an aspect that affords helpful flexibility when its use is transferred to a cultural context that differs from its source. The SCID modules used to represent common mental disorders at primary care levels and include those for major depressive disorder, generalized anxiety disorder, mixed anxiety depressive disorder, and somatization disorder. The modules elicited reports on lifetime prevalence of DSM-IV disorders, as well as 1-year and 1-month prevalence; 1-month prevalence data are used in these analyses (64).
Instrument translation
The instruments were translated to Kiswahili and back translated to English by separate groups of translators and discrepancies between the various translations were subjected to a panel discussion of indigenous translators that included three psychiatrists with clinical experience in Dar es Salaam. Each item was examined to ensure face validity and a transfer of conceptual meaning in the Kiswahili versions. Final changes to the Kiswahili versions were made after piloting amongst antenatal clinic attendees prior to onset of the study to ensure that the idioms used would be understood by the study population.
Minor modifications of the physical functioning subscale of the SF-36 were made to accommodate the context of the study setting. For example, in the second item of the physical functioning scale reflecting moderate activities, the original version of the SF-36 that included ‘moving a table, pushing a vacuum cleaner, bowling, or playing golf’ was changed to include more contextual activities such as ‘drawing water, washing clothes, and carrying a baby.’ In addition, ‘climbing several flights of stairs’, was changed to ‘walking up a steep hill’ given the limited opportunities for stair climbing in Dar es Salaam.
Data collection procedures
Research assistants at the study sites collected the psychosocial information using face-to-face administration, as some of the study participants were illiterate. The SCID was administered within two weeks of administration of the HSCL-25 by two indigenous psychiatrists who were blind to the HSCL-25 scores.
Statistical analysis
A summary description of socio-demographic characteristics of the sample and subsample, means and standard deviations (SD) of endorsed items on the HSCL-25 is provided. Internal consistency reliability of items on the HSCL-25, as well as the depression and anxiety subscales, was estimated by calculating Cronbach’s α. In addition to ensuring careful transfer of items that measured the constructs of general psychological distress and depression, factor analysis of the HSCL-25 and HSCL-15 with varimax rotation was conducted to further assess construct validity. Initial discriminant validity was assessed by establishing Pearson’s correlations for single items with overall sum scores of the HSCL-25 and 15. Further an a priori assumption is made that high scorers on the HSCL-25 will report lower scores on quality of life indicators and perceived social support as measured by the SF-36 and the perceived social support scale, respectively. Criterion validity was determined using receiver operating characteristic (ROC) analysis. DSM IV criteria for probable depression is utilized as a ‘gold standard’ to estimate the area under the curve (AUC) for all possible cut-off points on individual items of the HSCL in order to generate symptoms that would be most predictive of major depressive disorder. Finally using ROC analysis, the specificity and sensitivity of the HSCL-25, the depression subscale (HSCL-15) and a modified version of the HSCL (HSCL-revised) that includes the most predictive items are estimated in order to calibrate the scales. The HSCL-revised subscale was developed through preliminary use of ROC analysis. The AUC was calculated for each individual symptom on the HSCL-25, using DSM-IV criteria for major depression as the ‘gold standard’. Items that yielded the highest AUCs were considered to be the most predictive of major depression and were included in a subscale of eight symptoms that reflected depression and anxiety.
Results
Socio-demographic information
The sample was comprised of relatively young women of mean age 24.8 years with minimal exposure to formal education, most having completed various stages of primary school education (7 years in Tanzania). The mean gestational age of the sample was 18 weeks, with an average household size of 3.6 persons and a per capita daily expenditure on food of less than a dollar (USD approx: 800 Tanzanian shillings). More than half of the women were married in monogamous partnerships and just over one in 10 were single, separated or divorced. The partners of married or cohabiting women had a relatively higher mean age(32.9 ± 4 years) and greater exposure to post-primary education(see Table 1).
Table 1.
Socio-demographic characteristics of 903 HIV-positive antenatal clinic attendees, Dar es Salaam, Tanzania
| Demographics | n or mean ± SD (n= 903) | % |
|---|---|---|
| Women’s age (range 19–40 years): | 24.8 ± 4.8 | |
| 15–24 | 471 | 52.2 |
| 25–29 | 279 | 30.9 |
| 30+ | 153 | 16.9 |
| Women’s education level | ||
| Primary school | 743 | 82.3 |
| Post-primary education | 88 | 9.7 |
| Nil or adult education | 72 | 8.0 |
| Mean number of household members | 3.6 ±2.0 | - |
| Mean daily per-capita expenditure on food (TShs)* | 529 ± 275.6 | - |
| Mean gestational age (range 8–26 weeks) | 18.0 ±3.2 | - |
| Marital status | ||
| Married monogamous | 533 | 59.0 |
| Cohabiting | 222 | 24.6 |
| Single/divorced/separated | 97 | 10.7 |
| Married polygamous | 51 | 5.6 |
| Mean number of years married/cohabiting (n = 814) | 3.5 ± 4.0 | - |
| Spouse/partner’s mean age (n= 815, range 19–56 years) | 32.9 ±6.6 | |
| Did not know age | 88 | 9.7 |
| Spouse/partner’s education level (n= 813) | ||
| Primary school | 519 | 57.5 |
| Post-primary education | 207 | 22.9 |
| Nil or adult education | 17 | 1.9 |
| Did not know | 70 | 7.8 |
USD = approximately 890 Tanzanian Shillings (TShs).
Psychometric properties of the HSCL-25
Endorsement of items on the HSCL-25 at any level of severity in the sample ranged from 2 to 26%. The most frequently endorsed items were low mood and loss of sexual interest or pleasure, reported by more than a fifth of the women followed by worrying too much about things, headaches, feeling trapped, and a series of physiological disturbance items as noted in Table 2.
Table 2.
Endorsement frequency and mean scores of the HSCL-25 and correlations between the HSCL sum scores its individual items in 903 HIV-positive antenatal clinic attendees, Dar es Salaam, Tanzania
| Scales | Frequency endorsed* (%) | Mean score and SD | Pearson’s correlations† |
|---|---|---|---|
| HSCL-25 items (Cronbach’s α 0.93)‡ | |||
| Feeling blue | 26.0 | 1.23 ± 0.59 | 0.77 (0.80) |
| Loss of sexual interest or pleasure | 23.0 | 1.41 ± 0.86 | 0.52 (0.56) |
| Headaches | 18.0 | 1.25 ± 0.59 | 0.47 (0.38) |
| Worrying too much about things | 18.0 | 1.28 ± 0.68 | 0.71 (0.75) |
| Feeling trapped or caught | 17.0 | 1.26 ± 0.65 | 0.66 (0.72) |
| Difficulty falling sleep or staying asleep | 16.0 | 1.21 ± 0.60 | 0.52 (0.52) |
| Feeling low in energy, slowed down | 15.0 | 1.20 ± 0.53 | 0.68 (0.68) |
| Blaming oneself for things | 14.0 | 1.20 ± 0.54 | 0.70 (0.70) |
| Poor appetite | 11.0 | 1.15 ± 0.49 | 0.46 (0.46) |
| Heart pounding or racing | 10.0 | 1.30 ± 0.65 | 0.57 (0.45) |
| Feeling everything is an effort | 10.0 | 1.14 ± 0.46 | 0.66 (0.66) |
| Feeling hopeless about the future | 10.0 | 1.15 ± 0.51 | 0.65 (0.68) |
| Feeling fearful | 10.0 | 1.13 ± 0.45 | 0.65 (0.51) |
| Crying easily | 10.0 | 1.14 ± 0.47 | 0.55 (0.55) |
| Spells of terror or panic | 9.0 | 1.12 ± 0.44 | 0.71 (0.61) |
| Feeling no interest in things | 9.0 | 1.12 ± 0.44 | 0.60 (0.63) |
| Faintness, dizziness, or weakness | 9.0 | 1.13 ± 0.46 | 0.54 (0.44) |
| Feeling lonely | 9.0 | 1.12 ± 0.44 | 0.67 (0.70) |
| Being suddenly scared for no reason | 8.0 | 1.11 ± 0.41 | 0.62 (0.49) |
| Feelings of worthlessness | 7.0 | 1.11 ± 0.46 | 0.67 (0.72) |
| Feeling restless, not being able to sit still | 6.0 | 1.08 ± 0.35 | 0.58 (0.52) |
| Thoughts of ending one’s life | 6.0 | 1.10 ± 0.40 | 0.57 (0.60) |
| Nervousness or shakiness inside | 6.0 | 1.19 ± 0.52 | 0.67 (0.57) |
| Feeling tense or keyed up | 5.0 | 1.10 ± 0.32 | 0.59 (0.50) |
| Trembling | 2.0 | 1.03 ± 0.24 | 0.40 (0.30) |
Higher HSCL scores indicate greater psychological morbidity.
Correlations between sum scores of the HSCL 25 and (HSCL-15) and individual HSCL-25 items, All correlation coefficients are significant at 0.01 level; 2-tailed.
Items are endorsed at any level of severity on the HSCL-25.
The internal consistency of the HSCL-25 was reasonable with an overall Cronbach’s α of 0.93 and 0.9 and 0.85 for the depression and anxiety subscales, respectively. The items of the HSCL-25 were subjected to a principal components analysis with varimax rotation, retaining factors with an eigenvalue greater than one. A factor loading on items with an absolute value of 0.4 or more was used as sufficient criteria for its inclusion in a scale on both methodological (65), and substantive grounds, given that the items with factor loadings between 0.4 and 0.5 reflected core physiological symptoms of depression for factors three and four (see Table 3). Thirty-nine percent of the variance in items on the HSCL-25 was explained by a depression-anxiety construct (first factor), while 25% of the variance is accounted for by the second factor and includes items that can be described as a predominantly anxiety construct. The third and fourth factors, which each explain 18% of the variance includes items that can best be described as psycho-physiological and physiological constructs, respectively.
Table 3.
Factor structure of the HSCL-25 amongst antenatal clinic attendees screening HIV positive in Dar es Salaam, Tanzania (n = 903)
| HSCL-25 Item | Loadings |
|---|---|
| Factor 1: Depression-anxiety; explained 39% of variance (13 items) | |
| Feelings of worthlessness | 0.77 |
| Feeling hopeless about the future | 0.75 |
| Feeling trapped or caught | 0.71 |
| Faintness, dizziness, or weakness | 0.70 |
| Feeling blue | 0.68 |
| Worrying too much about things | 0.66 |
| Thoughts of ending one’s life | 0.65 |
| Feeling lonely | 0.63 |
| Blaming oneself for things | 0.58 |
| Feeling everything is an effort | 0.55 |
| Feeling no interest in things | 0.52 |
| Spells of terror or panic | 0.40 |
| Crying easily | 0.40 |
| Factor 2: Anxiety-panic; explained 25% of variance (5 items) | |
| Feeling fearful | 0.79 |
| Being suddenly scared for no reason | 0.71 |
| Spells of terror or panic | 0.71 |
| Nervousness or shakiness inside | 0.70 |
| Feeling tense or keyed up | 0.59 |
| Factor 3: Psycho-physiological; explained 18% of variance(6 items) | |
| Heart pounding or racing | 0.58 |
| Headaches | 0.58 |
| Loss of sexual interest or pleasure | 0.57 |
| Feeling low in energy, slowed down | 0.51 |
| Poor appetite | 0.48 |
| Crying easily | 0.40 |
| Factor 4: Physiological; explained 18% of variance(5 items) | |
| Trembling | 0.75 |
| Faintness, dizziness, or weakness | 0.60 |
| Difficulty falling sleep or staying asleep | 0.56 |
| Feeling low in energy, slowed down | 0.48 |
| Poor appetite | 0.46 |
A similar principal components analysis with varimax rotation was performed on the HSCL-15 depression subscale (see Table 4) and demonstrated items that clustered into two factors. The first factor represented predominantly psychological distress (65% of variance explained) while the second more physiological aspects of depression (35% of variance explained).
Table 4.
Factor structure of the depression subscale (HSCL-15) amongst antenatal clinic attendees screening HIV positive in Dar es Salaam, Tanzania (n = 903)
| HSCL-15 Items | Loadings |
|---|---|
| Factor 1: Depression psychological, 65% of variance explained | |
| Feeling hopeless about the future | 0.76 |
| Feelings of worthlessness | 0.76 |
| Feeling blue | 0.71 |
| Thoughts of ending one’s life | 0.70 |
| Feeling trapped or caught | 0.69 |
| Blaming oneself for things | 0.68 |
| Feeling lonely | 0.68 |
| Worrying too much about things | 0.68 |
| Crying easily | 0.53 |
| Feeling everything is an effort | 0.52 |
| Feeling no interest in things | 0.49 |
| Factor 2: Depression psycho-physiological 35% of variance explained | |
| Poor appetite | 0.77 |
| Feeling low in energy, slowed down | 0.70 |
| Difficulty falling sleep or staying asleep | 0.62 |
| Loss of sexual interest or pleasure | 0.50 |
| Feeling everything is an effort | 0.46 |
| Feeling no interest in things | 0.43 |
Discriminant validity was initially assessed by examining the correlation between individual HSCL-25 and HSCL-15 items to the overall sum scores of these scales (Table 2). Significant correlations are demonstrated between individual HSCL-25 items and the sum scores of the main and subscale. The correlation coefficients for most of the depressive items were slightly higher for the overall HSCL-15 compared with the overall HSCL-25 scores. Correlations between the total HSCL-25 score and the social support and SF-36 dimension scores, summarized in Table 5, supported an a priori assumption that high scores on the HSCL-25 (more symptomatology) would correlate negatively with perceived health-related quality of life scores (lower perceived health-related quality of life) and positively with social support (lower perceived social support).
Table 5.
Endorsement frequency and/or mean scores of SF-36 dimensions and the Social Support Scale and their correlations with HSCL sum scores in 903 HIV-positive antenatal clinic attendees, Dar es Salaam, Tanzania
| Scales | Frequency endorsed (%) | Mean score* and SD | Pearson’s correlations |
|---|---|---|---|
| Perceived social support (Cronbach’s α 0.98)† | - | 1.37 ±0.60 | 0.27 (0.36) |
| Get love and affection | 85.0 | 1.41 ±0.77 | - |
| Get help when sick | 85.0 | 1.23 ±0.60 | - |
| Visits from relatives and friends | 83.0 | 1.25 ±0.59 | - |
| Have people who care | 83.0 | 1.43 ± 0.80 | - |
| Useful advice on important things | 77.0 | 1.37 ± 0.77 | - |
| Get help around the house | 74.0 | 1.45 ±0.84 | - |
| Get financial help in emergency | 74.0 | 1.24 ±0.62 | - |
| Chance to talk about problems | 73.0 | 1.46 ± 0.85 | - |
| Get help for transport | 73.0 | 1.29 ±0.70 | - |
| Have a confidant | 68.0 | 1.61 ±0.99 | - |
| SF-36 dimensions‡ | |||
| Mental health | 90.66 ±16.5 | −0.80 (−0.63) | |
| Vitality | 87.97 ± 18.5 | −0.64 (−0.59) | |
| Social functioning | 93.15 ± 15.5 | −0.60 (−0.51) | |
| General health | 79.84 ± 18.7 | −0.58 (−0.78) | |
| Role emotional functioning | 89.85 ± 26.9 | −0.51 (−0.57) | |
| Bodily pain | 85.33 ± 20.9 | −0.49 (−0.48) | |
| Role physical functioning | 86.85 ± 30.1 | −0.47 (−0.47) | |
| Physical functioning | 94.11 ± 11.16 | −0.40 (−0.39) |
Correlations between sum scores of the HSCL 25 and (HSCL-15) SF-36 dimension and perceived social support sum means; All correlation coefficients are significant at 0.01 level; 2-tailed.
Items endorsed ‘as much as I would have liked’ on perceived social support scale; Lower mean scores indicate higher perceived social support.
Higher mean scores indicate greater health-related quality of life.
Criterion validity
Using ROC analysis, and DSM IV criteria for probable and definite major depressive episode as a ‘gold standard’, AUC at all possible cut-off points is used to establish items on the HSCL-25 most predictive of a major depressive episode. Eleven women of ninety-nine who yielded diagnostic information from the SCID met definite criteria for major depressive episode (n =7.7% 1-month prevalence); mixed anxiety and depressive disorder (n= 3.3% one-month prevalence); and generalized anxiety disorder (n =1.1% 1-year prevalence). None met criteria for somatization disorder, and two subjects met criteria for probable depressive disorder. On a clinical basis, probable disorder might have been diagnosed as depressive disorder but both subjects did not satisfy the exclusion criteria B.10 on the SCID, related to ‘symptoms causing significant distress or impairment in social, occupational, or other important areas of functioning’. Substitution of roles and responsibilities when a person is ill in a setting where members of the extended family live-in and role definitions are based on age and gender divisions rather than individual responsibilities, might influence one’s perception of diminished/impaired functioning in this cultural context. Establishing impairment of functioning from collateral information was not possible in an antenatal clinic setting where relatives do not accompany women.
ROC analysis of individual HSCL-items revealed AUCs ranging from 0.495 to 0.797. Eight items generated AUC’s that were equal to or greater than 0.6, two being items from the anxiety subscale and six from the depressive subscale, substantiating clinical observations of an overlay of anxiety symptoms in individuals with depressive disorders in this cultural context. The symptoms included ‘feeling blue’ (AUC =0.80); ‘feeling trapped or caught’ (AUC =0.70); ‘difficulty falling or staying asleep’ (AUC= 0.70); ‘worrying too much about things’ (AUC= 0.68); ‘heart pounding or racing’ (AUC =0.65); ‘crying easily’ (AUC = 0.63); ‘feeling hopeless about the future’ (AUC = 0.63); and ‘faintness, dizziness or weakness’ (AUC 0.61). A modified depression sub-scale (HSCL-revised) was derived from these eight items for screening for depression in antenatal populations and further ROC analysis was conducted to establish cut-off points of the HSCL-25, HSCL-15 and HSCL-revised.
Calibration of the HSCL-25 for caseness in the Tanzanian antenatal primary care context
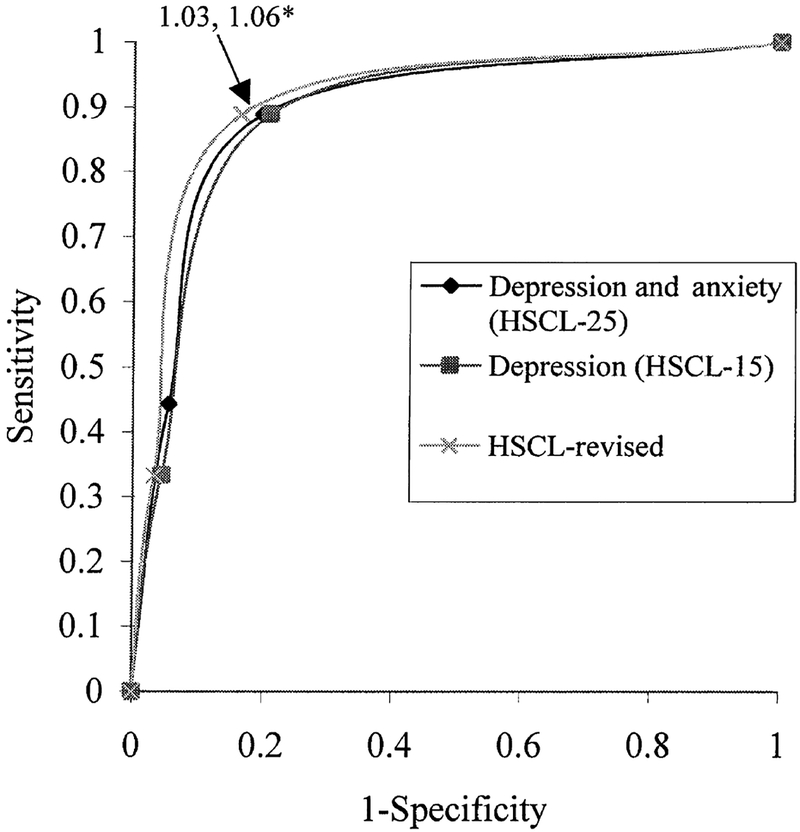
The ROC curves indicate that the total HSCL-25 and depression subscale scores are comparable with respect to their ability to detect major depressive disorder (Fig. 1). This is reflected in the similar estimates of the area under the ROC curve (AUC) as follows: for the total HSCL-25 score, the AUC was estimated as .86 [95% confidence interval (CI): 0.72–0.99], while that of the depression subscale was also 0.86 (95% CI: 0.73–0.99). The HSCL-revised demonstrated a slightly higher AUC estimated at 0.88 (95% CI: 0.75–1.0).
Fig. 1.
ROC curve analysis for the HSCL-25, HSCL-15 and HSCL-revised as screens for major depressive disorder. *Cut-off points for subscales are as follows: HSCL-25: 1.06; HSCL-15: 1.03; and HSCL-revised: 1.06.
The optimal cut-off points for detecting major depression using the HSCL-25, HSCL-15 and HSCL-revised subscales as screening tests were1.06, 1.03 and 1.06, respectively. Although the HSCL-25, HSCL-15, and HSCL-revised scales demonstrated the same sensitivity at 89%, the specificity is slightly better for the HSCL-revised (85%), compared with the HSCL-25 (80%) and the HSCL-15 (79%).
Given that this validation study was based on a two-phase design, where the validation subsample was drawn from a stratified random sample of the larger cohort, a weighted analysis was also performed in order to account for the different sampling fractions for each strata (66). This sensitivity analysis indicated similar findings, whereby the optimal cut-off points for the sub-scales remained at 1.03 and 1.06 for the HSCL-15 and the HSCL-revised, respectively. Although sensitivity and specificity were attenuated for the weighted analysis of the HSCL-15, 75 and 81%, respectively, results were comparable for the HSCL-revised, with a sensitivity of 88% and a specificity of 89%.
Discussion
In the context of this study, the more important implications of early recognition and hence management of depressive disorders is in improving quality of remaining life (67) and motivation to obtain good medical care. These aspects have important significance on adherence to treatment and for strategies to decrease transmission risks including maternal to child transmission of HIV. In general, depressive disorders in primary care settings are often missed (68, 69), recognition rates across 15 sites in a WHO collaborative study ranging from 19.3 to 70% (70). The situation in countries such as Tanzania with low human resources for mental health care, and high HIV sero-prevalence informs the need for valid screening instruments for recognition of depression that can be used by health workers with minimal mental health skills who work with HIV-positive women in antenatal settings.
Studies that aim at validating measures of psychological states are hampered by the lack of a ‘gold standard’ (5, 71) and although cross-cultural deficiencies in DSM diagnostic criteria have been reported (72), the SCID provided an appropriate degree of structure and flexibility to accommodate a systematic assessment of major psychiatric disorder. Principal components analysis was used to examine the construct validity; factorial invariance is best understood as an indicator of dimensional constancy across various discrete categories among variables of interest. In this instance, it is evident that a core depression-anxiety construct emerges empirically from the data. All but one (an anxiety and panic construct) of the four constructs emerging from principal components analysis of the HSCL-25, indicating a mixture of somatic and psychological items. This supports previous observations of the absence of a Cartesian mind–body dichotomy in the African cultural context (73).
A large proportion of this sample of HIV-positive women manifests with a predominantly psychological ‘core’ symptomatology of depression and anxiety, the most frequently endorsed symptoms being ‘feeling sad’ and ‘loss of sexual interest or pleasure’ and ‘worrying too much about things’. Scores for ‘loss of sexual interest or pleasure’ had lower correlations with sum scores on both the HSCL-25 and 15; and a relatively smaller AUC (0.57) on ROC analysis of individual HSCL-items, suggesting conditions other than depression may account for the high endorsement of this symptom. Need for future exploration of possible hypoactive sexual desire disorder, a condition that has been reported as prevalent (20%) amongst HIV-seropositive women elsewhere (13) is suggested.
The depression subscale demonstrated a comparable accuracy to the total HSCL-25 scale in the ROC analysis, suggesting its usefulness for the identification of ‘probable cases’ of clinically significant depression in the primary care settings of this study. However, the abbreviated HSCL-revised in this context provides for not only a more efficient but also a slightly more accurate method of assessment. The lower optimal cut-off score observed in all of the scales (compared with the more universally calibrated cut-off score of1.75), may reflect difficulty in establishing the conceptual equivalence of ‘scales’ across cultures, as the validation results suggest that any level of endorsement of depressive or anxiety symptoms may be clinically relevant in this population. This could suggest a cultural orientation towards not emphasizing that these symptoms are bothering them ‘quite a bit’ or ‘extremely.’ The HSCL-25 mean scores on endorsed items for cases is much lower than similar mean scores established elsewhere (50, 51, 74), also supporting a possible under-reporting of severity of psychological distress in this population. The findings further support the likelihood of cultural influences on the experience and expression of emotional states (75–77), and emphasize the importance of renorming adapted standardized screening instruments.
The inability of the HSCL in this setting to reflect well the severity of depressive symptomatology is a major limitation on its use. The validated cut-off points close to 1.0 (indicating no symptomatology) suggests need to expand upon this basic tool in the future to refine the identification of levels of psychosocial intervention that may be needed on an individual basis. It is likely that there are local idioms that are not part of the standard construct of depression and hence not included in the HSCL-25 that might further improve the sensitivity and specificity for detecting major depression in this population.
Another methodological limitation is in the conduction of this validation study among a HIV-positive cohort of pregnant women. It is important to note that all women in this sample had not progressed to AIDS at the time of the interview and the cohort was drawn from a larger group of women accessing general antenatal services at clinics in Dar es Salaam. While there is minimal information on the behaviour of conventional screening instruments in populations of pregnant women, there are suggestions that at least in the puerperium, equivalent rates for major depressive disorders with minimal overlap occurs with a variety of self-report symptom inventories (78). There is, however, sufficient evidence to argue for a need for further studies that replicate the reported properties of the HSCL 25 and its subscales in HIV negative pregnant women and primary care populations outside antenatal care.
In conclusion while the HSCL-25 is a useful screening tool for depression at primary care in Dar es Salaam, it is not informative for detecting severity of symptomatology. Additional in depth research utilizing qualitative methods of inquiry to gather information is needed to identify symptoms of major depression that may be specific to the Tanzanian context and other developing countries where HIV is highly prevalent. This will allow for the further adaptation of standardized instruments to improve accuracy in measurements of symptom severity in resource-poor settings.
Acknowledgements
The authors wish to acknowledge women who participated in the study and the research assistants who worked collaboratively with them to collect the data. We would also like to thank all of the coinvestigators and coworkers who contributed to this manuscript and the larger study. This research was made feasible through a grant from the National Institute of Mental Health, USA (R03 MH55451). The primary grant for this research study is from the National Institute of Child Health and Development (R01-HD32257).
References
- 1.Unaids. AIDS Epidemic Update: December 2000. UNAIDS/00.44E–HO/CDS/CSR/EDC/20009,2000.
- 2.Dennerstein L Psychosocial and mental health aspects of women’s health. World Health Statistics Q; 1993;46:234–236. [PubMed] [Google Scholar]
- 3.Patel V, Araya R, De Lima M, Ludermir A, Todd C. Women, poverty and common mental disorders in four restructuring societies. Social Sci Med 1999;49: 1461–1471. [DOI] [PubMed] [Google Scholar]
- 4.Ostrow DG, Monjan A, Joseph J et al. HIV-related symptoms and psychological functioning in a cohort of homosexual men. Am J Psychiatry 1989;146:737–742. [DOI] [PubMed] [Google Scholar]
- 5.Cochran SD, Mays VM. Depressive distress among homosexually active African American men and women. Am J Psychiatry 1994;151:524–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perkins DO, Stern RA, Golden RN, Murphy C, Naftolowitz D, Evans DL. Mood disorders in HIV infection. prevalence and risk factors in a non-epicenter of the AIDS epidemic. Am J Psychiatry 1994;151:233–236. [DOI] [PubMed] [Google Scholar]
- 7.Atkinson JH, Grant I, Kennedy C et al. Prevalence of psychiatric disorders among men infected with human immunodeficiency virus. Arch Gen Psychiatry 1988;45:859–886. [DOI] [PubMed] [Google Scholar]
- 8.Perry S, Jacobsberg LB, Fishman B et al. Psychiatric diagnosis before serological testing for the human immunodeficiency virus. Am J Psychiatry 1990;147:89–93. [DOI] [PubMed] [Google Scholar]
- 9.Williams JVW, Rabkin JG, Remien RH, Gorman JM, Ehrhardt AA. Multidisciplinary baseline assessment of homosexual men with and without human immunodeficiency virus infection, II. standardized clinical assessment of current and lifetime psychopathology. Arch Gen Psychiatry 1991;48:124–130. [DOI] [PubMed] [Google Scholar]
- 10.Rabkin JG, Ferrando SJ, Jacobsberg LB, Fishman B. Prevalence of axis I disorders in an AIDS cohort: a cross-sectional, controlled study. Comp Psychiatry 1997;38:146–154. [DOI] [PubMed] [Google Scholar]
- 11.Brown GR. Prospective study of psychiatric morbidity in HIV-seropositive women. Psychol Med 1989;51:246–247. [DOI] [PubMed] [Google Scholar]
- 12.Brown GR, Rundell JR. Prospective study of psychiatric morbidity in HIV-seropositive women without AIDS. Gen Hosp Psychiatry 1990;12:30–35. [DOI] [PubMed] [Google Scholar]
- 13.Katon W, Sullivan MD. Depression and chronic medical illness. J Clin Psychiatry 1990;51(Suppl. 6):3–11. [PubMed] [Google Scholar]
- 14.Evans DL, Leserman J, Pedersen CA et al. Immune correlates of stress and depression. Psychopharmacol Bull 1989;25:319–324. [PubMed] [Google Scholar]
- 15.Kessler RC, Foster C, Joseph J et al. Stressful life events and symptom onset in HIV infection. Am J Psychiatry 1991;148:733–738. [DOI] [PubMed] [Google Scholar]
- 16.Reichlin S Mechanisms of disease: neuroendocrineimmune interactions. N Engl J Med 1993;329:1246–1253. [DOI] [PubMed] [Google Scholar]
- 17.Burack JH, Barrett DC, Stall RD, Chesney MA, Ekstrand ML, Coates TJ. Depressive symptoms and CD4 lymphocyte decline among HIV-infected men. JAMA 1993;270:2568–2573. [PubMed] [Google Scholar]
- 18.Lyketsos CG, Hoover DR, Guccione M et al. Depressive symptoms over the course of HIV infection before AIDS. Soc Psychiatry Psychiatr Epidemiol 1996;31:212–219. [DOI] [PubMed] [Google Scholar]
- 19.Atkinson JH, Grant I. Mood disorder due to human immunodeficiency virus: yes, or maybe? Semin Clin Neuropsychiatry 1997;2:276–284. [DOI] [PubMed] [Google Scholar]
- 20.Sebit MB. Neuropsychiatric HIV-1 infection study. in Kenya and Zaire. Cross-sectional phase I and II. Central African J Med 1995;41:315–322. [PubMed] [Google Scholar]
- 21.Fukunishi I, Matsumoto T, Negishi M, Hayashi M, Hosaka T, Moriya H. Somatic complaints associated with depressive symptoms in HIV-positive patients. Psychother Psychosom 1997;66:248–251. [DOI] [PubMed] [Google Scholar]
- 22.Maj M, Janssen R, Starace F et al. WHO neuropsychiatric AIDS study, cross-sectional phase I. Arch Gen Psychiatry 1994;51:39–49. [DOI] [PubMed] [Google Scholar]
- 23.Belkin GS, Fleishman JA, Stein MD, Piette J, Mor V. Physical symptoms and depressive symptoms among individuals with HIV infection. Psychosomatics 1992;33: 416–427. [DOI] [PubMed] [Google Scholar]
- 24.Mcclure JB, Catz SL, Prejean J, Brantley PJ, Jones GN. Factors associated with depression in a heterogeneous HIV-infected sample. J Psychosom Res 1996;40:407–415. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan MS, Marks G, Mertens SB. Distress and coping among women with HIV infection: preliminary findings from a multiethnic sample. Am J Orthopsychiatry 1997;67:80–91. [DOI] [PubMed] [Google Scholar]
- 26.Koonin L, Ellerbrock T, Atrash H et al. Pregnancy-associated deaths due to AIDS in the United States. JAMA 1989;261:1306–1309. [PubMed] [Google Scholar]
- 27.Selwyn P, Schoenbaum E, Davenny K et al. Prospective study of human immunodeficiency virus infection and pregnancy outcomes in intravenous drug users. JAMA 1989;261:1289–1294. [PubMed] [Google Scholar]
- 28.Rothenberg R, Woelfel M, Stoneburner R et al. Survival with the acquired immunodeficiency syndrome. N Engl J Med 1987;317:1297–1302. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy CA, Skurnick JH, Foley M, Louria DB. Gender differences in HIV-related psychological distress in heterosexual couples. AIDS Care 1995;7(Suppl. 1): S33–S38. [DOI] [PubMed] [Google Scholar]
- 30.Assael M, Namboze JM, German GA, Bennett FJ. Psychiatric disturbances during pregnancy in a rural group of African women. Social Sci Med 1972;6:387–395. [DOI] [PubMed] [Google Scholar]
- 31.Cox JL. Psychiatric morbidity and pregnancy: a controlled study of 263 semi-rural Ugandan women. Br J Psychiatry 1979;134:401–405. [DOI] [PubMed] [Google Scholar]
- 32.Sen B An analysis of the nature of depressive phenomena in primary health care utilizing multivariate statistical techniques. Acta Psychiatric Scand 1987;76:28. [DOI] [PubMed] [Google Scholar]
- 33.Katon W, Walker E. Medically unexplained symptoms in primary care. J Clinicalpsychol 1998;59(Suppl. 20):15–21. [PubMed] [Google Scholar]
- 34.Penayo U, Kullgren C, Caldera T. Mental disorders among primary health care patients in Nicaragua. Acta Psychiatrica Scand 1990;82:82. [DOI] [PubMed] [Google Scholar]
- 35.Bhat A, Tomenson B, Benjamnin S. Transcultural patterns of somatization in primary care: a preliminary report. J Psyhcosom Res 1989;33:671–680. [DOI] [PubMed] [Google Scholar]
- 36.Cherian VI. Peltzer K, Cherian L. The factor-structure of the Self Reporting Questionnaire (SRQ-20) in South Africa. East African Med J 1998;75:654–656. [PubMed] [Google Scholar]
- 37.Bornstein RA, Pace P, Rosenberger P et al. Depression and neuropsychological performance in asymptomatic HIV infection. Am J Psychiatry 1993;150:922–927. [DOI] [PubMed] [Google Scholar]
- 38.Drebing CE, Van Gorp WG, Hinkin C et al. Confounding factors in the measurement of depression in HIV. J Pers Assess 1994;62:68–83. [DOI] [PubMed] [Google Scholar]
- 39.Kalichman SC, Sikkema KJ, Somlai A. Assessing persons with human immunodeficiency virus (HIV) infection using the Beck Depression Inventory: disease processes and other potential confounds. J Pers Assess 1995;64:86–100. [DOI] [PubMed] [Google Scholar]
- 40.Perkins DO, Leserman J, Stern RA et al. Somatic symptoms and HIV infection: relationship to depressive symptoms and indicators of HIV disease. Am J Psychiatry 1995;152:1776–1781. [DOI] [PubMed] [Google Scholar]
- 41.O’dell MW, Meighen M, Riggs RV. Correlates of fatigue in HIV infection prior to AIDS: a pilot study. Disabil Rehabil 1996;18:249–254. [DOI] [PubMed] [Google Scholar]
- 42.Depression Kleinman A., somatization, and the ‘new cross-cultural psychiatry.’ Social Sci Med 1977;11:3–9. [DOI] [PubMed] [Google Scholar]
- 43.Kirmayer LJ. Cultural variations in the response to psychiatric disorders and emotional distress. Social Sci Med 1989;29:327–339. [DOI] [PubMed] [Google Scholar]
- 44.Geisinger KF. Cross-cultural normative assessment. Translation and adaptation issues influencing the normative interpretation of assessment instruments. Psychol Assess 1994;6:304–312. [Google Scholar]
- 45.Van DE Vijver FJR, Poortinga YH. Testing across cultures In: Hambleton RK, Zaal JN, eds. Advances in educational and psychological testing. Boston: Kluwer Academic; 1991: 277–308. [Google Scholar]
- 46.Parry CDH. A review of psychiatric epidemiology in Africa: strategies for increasing validity when using instruments transculturally. Transcultural Psychiatr Res Rev 1996;33:173–188. [Google Scholar]
- 47.Fawzi WW, Msamanga GI, Spigelman D, Urassa EJ, Hunter DJ. Rationale and design of the Tanzania Vita-min and HIV infection trial. Control Clin Trials 1999;20:75–90. [DOI] [PubMed] [Google Scholar]
- 48.Parloff MB, Kelman HC, Frank JD. Comfort effectiveness and self-awareness as criteria for improvement in psychotherapy. Am J Psychiatry 1954;3:343–351. [DOI] [PubMed] [Google Scholar]
- 49.Derogratis LR, Lipman RS, Rickels EH, Uhlenhutheh, Covi L. SCL-90-R: an outpatient psychiatric rating scale. Psychopharmacol Bull 1973;9:13–28. [PubMed] [Google Scholar]
- 50.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist: a measure of primary symptom dimensions. Psychol measuxrements psychopharmacology. Mod Probl Pharmacopsychiat 1974;7:79–110. [DOI] [PubMed] [Google Scholar]
- 51.Hinton WLN, Chen YC, Tran CG, Newman TB, LU FG. Screening for major depression in Vietnamese refugees: a validation and comparison of two instruments in a health screening population. J General Intern Med 1994;9:202–206. [DOI] [PubMed] [Google Scholar]
- 52.Mollica RF, Wyshak G, DE Marneffe D, Khuon F, Lavelle J. Indochinese version of the Hopkins Symptom Checklist-25: a screening instrument for psychiatric care of refugees. Am J Psychiatry 1987;144:497–500. [DOI] [PubMed] [Google Scholar]
- 53.McKelvey RS, Webb JA. A prospective study of psychological distress related to refugee camp experience. Aust N Z J Psychiatry 1997;31:549–554. [DOI] [PubMed] [Google Scholar]
- 54.Hesbacher PT, Rickels K, Morris RJ, Newman H, Rosenfeld H. Psychiatric illness in family practice. J Clin Psychiatry 1980;41:6–10. [PubMed] [Google Scholar]
- 55.Hansson L, Nettelbladt P, Borgquist L, Nordstrom G. Screening for psychiatric illness in primary care: a cross-sectional study in a Swedish health district. Soc Psychiatry Psychiatr Epidemiol 1994;29:83–87. [DOI] [PubMed] [Google Scholar]
- 56.Winokur A, Winokur DF, Rickels K, Cox DS. Symptoms of emotional stress in family planning service: stability over a four-week period. Br J Psychiatry 1984;144:395–399. [DOI] [PubMed] [Google Scholar]
- 57.Sullivan M, Karlsson J, Ware J. The Swedish SF-36 Health Survey. I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Social Sci Med 1995;41:1349–1358. [DOI] [PubMed] [Google Scholar]
- 58.Bullinger M German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA Project. Social Sci Med 1995;41:1359–1366. [DOI] [PubMed] [Google Scholar]
- 59.Wagner AK, Wyss K, Gandek B, Kilima PM, Lorenz S, Whiting D. A Kiswahili version of the SF-36 Health Survey for use in Tanzania: translation and tests of scaling assumptions. Quality Life Res 1999;8:101–110. [DOI] [PubMed] [Google Scholar]
- 60.Wyss K, Wagner AK, Whiting D et al. Validation of the Kiswahili version of the SF-36 Health Survey in a representative sample of an urban population in Tanzania. Quality Life Res 1999;8:111–120. [DOI] [PubMed] [Google Scholar]
- 61.Broadhead WE, Gehlbach SH, Degruy FV, Kaplan BH. The Duke-UNC functional social support questionnaire. Med Care 1988;26:709–723. [DOI] [PubMed] [Google Scholar]
- 62.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID).I. History, rationale, and description. Arch Gen Psychiatry 1992;49:624–629. [DOI] [PubMed] [Google Scholar]
- 63.Riskind JH, Beck AT, Berchick RJ, Brown G, Steer RA. Reliability of DSM-III diagnoses for major depression and generalized anxiety disorder using the structured clinical interview for DSM-III. Arch Gen Psychiatry 1987;44:817–820. [DOI] [PubMed] [Google Scholar]
- 64.First MB, Gibbon M, Spitzer RL, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), Research, Version 2.0. (Draft). New York: NY State Psychiatric Institute; October 1995. [Google Scholar]
- 65.Bailey KD. Methods of Social Research, 2nd edn New York: The Free Press; 1982. [Google Scholar]
- 66.Dunn G, Pickles A, Tansella M, Vazquez-Barquero JL. Two-phase epidemiological surveys in psychiatric research. Br J Psychiatry 1999;174:95–100. [DOI] [PubMed] [Google Scholar]
- 67.Rabkin JG, Rabkin R, Wagner G. Effects of fluoxetine on mood and immune status of depressed patients with HIV illness. J Clin Psychiatry 1994;55:92–97. [PubMed] [Google Scholar]
- 68.Karlsson H, Joukamaa M, Lehtinen V. Differences between patients with identified and non identified psychiatric disorders in primary care. Acta Psychiatrica Scand 2000;102:354–358. [DOI] [PubMed] [Google Scholar]
- 69.Goldberg D, Gater R. Implications of the World Health Organization study of mental illness in general care for training primary health care staff. Br J Gen Psychiatry 1996;46:483–485. [PMC free article] [PubMed] [Google Scholar]
- 70.Ustun TB, Van Korff M. Primary mental health services: access and provision of care In: Ustun TB, Sartorius N, eds. Mental Illness in General Health Care: an International Study. New York: John Wiley and Sons; 1995;347–360. [Google Scholar]
- 71.Nunnally JC, Bernstein IH. Psychometric Theory: Series in Psychology. New York: McGraw-Hill Inc; 1995; 96–97. [Google Scholar]
- 72.Maser JD, Kaelber C, Weise RE. International use and attitudes towards DSM-III and DSM-III-R: growing consensus in psychiatric classification. J Abnorm Psychol 1991;100:271–279. [DOI] [PubMed] [Google Scholar]
- 73.Lambo TA. The village of Aro. Lancet 1964;2:513–514. [PubMed] [Google Scholar]
- 74.Mouanoutoua VL, Brown LG. Hopkins Symptom Checklist-25, Hmong version: a screening instrument for psychological distress. J Personality Assessment 1995;64: 376–383. [DOI] [PubMed] [Google Scholar]
- 75.Lutz C Depression and translation of emotional worlds In: Kleinman A, Good B, eds. Culture and Depression: Studies in the Anthropology and Cross-Cultural Psychiatry of Affect and Disorder. Berkley: University of California Press; 1985; 63–100. [Google Scholar]
- 76.Good BJ, Kleinman A, Epilogue. Culture and Depression In: Kleinman A, Good B, eds. Culture and Depression: Studies in the Anthropology and Cross-Cultural Psychiatry of Affect and Disorder. Berkley: University of California Press; 1985; 1–42. [Google Scholar]
- 77.Jenkins JH, Kleinman A, Good BJ. Cross-Cultural Studies of Depression In: Becker J, Kleinman A, Hillsdale NJ, eds. Advances in Mood Disorders. New York: Erlbaum; 1990. [Google Scholar]
- 78.Muzik M, Klier CM, Rosenblum KL, Holzinger A, Umek W, Ktsching H. Are commonly used self-report inventories suitable for screening post-partum depression and anxiety disorders? Acta Psychiatrica Scand 2000; 102:71–73. [DOI] [PubMed] [Google Scholar]