Abstract
Background: Ultrasonography is a cost-effective, noninvasive, and expedient imaging modality with numerous clinical applications. Conventional ultrasound uses transducers with frequencies that range from 5 to 12 MHz. However, ultrahigh frequency ultrasound (UHFUS) is capable of producing frequencies up to 70 MHz, which can achieve tissue resolution up to 30 μm. The purpose of our study is to present the capabilities of a novel technology and to describe its possible clinical applications for hand surgery. Methods: The Vevo 2100 (VisualSonics, Toronto, Canada) system was used to perform all ultrasound exams. Four unique linear array transducers were employed. All studies were performed by the authors, who have no formal training in ultrasound techniques, on 5 healthy resident volunteers and 1 clinical patient under institutional review board approval. Results: A series of 10 static images per participant and dynamic, real-time videos were obtained at various locations within the hand and wrist. UHFUS is capable of quickly and reliably imaging larger structures such as foreign bodies, soft tissue masses, and the flexor tendons, and diagnosing an array of pathologies within these structures. In addition, UHFUS can identify much finer structures such as the intimal layer of the arteries in the hand and individual fascicles within the digital nerves to provide data about vessel quality and vascular and neural pathologies. Conclusions: UHFUS is a novel technology that shows multiple advantages over conventional ultrasound for imaging the fine superficial structures of the hand and wrist, and can be deployed by the surgeon at the point of care.
Keywords: ultrasound, hand surgery, imaging, hand, wrist, high-frequency ultrasound
Introduction
Ultrasonography is a cost-effective, noninvasive, and expedient imaging modality with wide clinical applications. Recent technological advances in ultrasound have augmented our ability to image superficial soft tissue structures with high resolution. Conventional ultrasound uses transducers with frequencies that range from 5 to 12 MHz. These relatively low frequencies allow for penetration deep into the body to visualize target internal structures. However, ultrahigh frequency ultrasound (UHFUS) is capable of producing frequencies up to 70 MHz, which provides superior imaging of superficial anatomical structures. This imaging technology can achieve tissue resolution up to 30 μm, which is 3 to 4 times smaller than the average diameter of a volar digital nerve.6
Ultrasound is a well-established imaging modality for both diagnostic and therapeutic uses in hand surgery, including needle guidance for injections and the evaluation of soft tissue masses, foreign bodies, tendon injuries, compressive neuropathies, and rheumatologic joint disease.10,13,14 Our investigation focuses on the superior imaging capabilities of UHFUS, and its ability to improve and expand the clinical scope of ultrasound for imaging the hand and wrist. In addition, most studies can be performed by the hand surgeon at the bedside without formal training in ultrasound techniques. The purpose of our study is to present the capabilities of a novel technology, and to describe its possible clinical applications for hand surgery.
Materials and Methods
The Vevo 2100 (VisualSonics, Toronto, Canada) imaging system was used to perform all ultrasound exams. Four unique linear array transducers were employed, using both B mode and color Doppler. They include the following: MS250 at 13 to 24 MHz, MS400 at 18 to 38 MHz, MS550S at 32 to 56 MHz, and MS550D at 22 to 55 MHz. All of the studies were performed by the authors (S.L.V. and L.K.C.), who have no formal training in ultrasound techniques, on 5 healthy resident volunteers and 1 clinical patient. Institutional review board approval was obtained prior to the initiation of this study. Informed consent was obtained from all individual participants included in this study.
Results
A series of 10 static images per participant were obtained at dedicated locations within the hand and wrist. Dynamic, real-time videos of the flexor tendons were also obtained in zone II of middle finger in each participant. The findings are reported below and categorized by tissue type.
Masses and Foreign Bodies
Previous studies have demonstrated the use of conventional ultrasound for imaging common soft tissue masses of the hand.3 Simple and complex ganglia can be reliably diagnosed with conventional ultrasound, preventing the need for costly magnetic resonance imaging (MRI) studies.16 Moreover, Bray et al demonstrated that conventional ultrasound with a linear array transducer at 10 MHz can achieve sensitivity of 94% and specificity of 99% for detecting foreign bodies within the hand.2
The high-resolution imaging at superficial depths of UHFUS is particularly effective in the subcutaneous tissues of the finger where the vital structures are within 1 cm of the skin surface. We present a clinical case below that demonstrates how UHFUS imaging can easily identify and quantify pathological findings within the fingers and hand with extremely high resolution.
A clinical case
A 49-year-old male presented complaining of right index finger pain. The patient reported that he injured his hand on a piece of wood approximately 2 months prior to presentation. He attributed the pain to a retained “splinter.” Plain film radiographs of the hand were negative for any radiopaque foreign bodies. The finger was imaged by the author (S.L.V.) using a 32-MHz transducer. Multiple views were obtained, which clearly identify a hyperechogenic linear foreign body with a surrounding hypoechogenic granuloma in the right index finger. The body was found within the subcutaneous tissues between the dermis and the flexor tendons, 4.5 mm below the skin. Images were taken both in the long axis (Figure 1a) and short axis (Figure 1b) of the body to accurately measure its dimensions. Color Doppler mode was also used to measure the distance between the foreign body and the digital artery (Figure 1c). This case demonstrates that the surgeon can precisely pinpoint the location of a lesion and measure its relationship to nearby small, but crucial, neurovascular structures without formal training in advanced ultrasound techniques.
Figure 1.
(a) Linear hyperechoic foreign body within volar soft tissue of the finger, (b) foreign body and surrounding granuloma seen directly overlying the flexor tendon sheath, and (c) proximity of the foreign body to the nearby digital artery is measured with color Doppler mode.
Tendon
Tendons in the hand and wrist are particularly well suited to ultrasound examination due to their relatively superficial location. The tendons can be visualized as a hyperechoic structure with a fibrillar internal structure in the longitudinal plane. However, the tendons can exhibit variable echogenicity depending on the orientation relative to the probe. The tendon substance is hyperechoic when the tendon is oriented at 90° to the probe but becomes hypoechoic as the angle veers away from the perpendicular plane. This phenomenon is called anisotropy, and it is particularly important in the fingers.7 The pulley system of the flexor tendon sheath keeps the tendon in close approximation to the underlying phalanges, which causes the tendon to course in a curvilinear along the skeletal structures of the finger. As a result, the tendon will exhibit differential areas of hyperechogenicity and hypoechogenicity.
The tendons can be easily identified and tracked from the wrist to their insertions. In the dorsum of the hand, the extensors are easily found beneath the dermis overlying the bright hyperechoic rim of the metacarpals and the dorsal interosseous muscles (Figure 2). In the fingers, flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) can be clearly visualized from the level of the metacarpophalangeal (MP) joint, through Camper chiasm, and to their individual insertions (Figure 3). At the level of the proximal interphalangeal (PIP) joint, the FDP tendon is seen superficial to the FDS tendon. With UHFUS, the volar plate is clearly visualized as a hyperechoic structure spanning between the FDS tendon and the hypoechoic joint space (Figure 4).
Figure 2.

Cross-sectional view of the dorsum of the hand over the third metacarpal showing the dorsal veins, extensor tendon, and dorsal interosseous muscles.
Figure 3.

Axial view of the distal interphalangeal joint of the finger showing the FDP tendon crossing the joint and inserting onto the base of the distal phalanx.
Note. FDP = flexor digitorum profundus.
Figure 4.
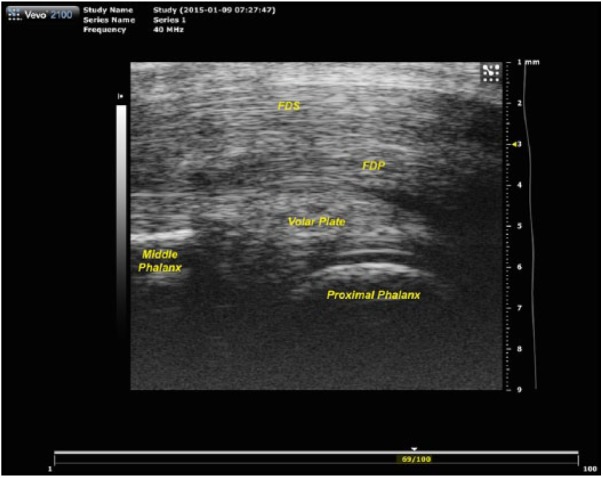
Axial view of the proximal interphalangeal joint of the finger clearly identifying the flexor tendons and the underlying volar plate.
Note. FDS = flexor digitorum superficialis; FDP = flexor digitorum profundus.
A unique advantage of ultrasound compared with other imaging modalities is the ability to obtain dynamic, real-time imaging of the motion and mechanics of the hand. When a participant ranges the finger, the tendons are recognized gliding within the tendon sheath and exerting pull on the phalanges to range the joints. With UHFUS, additional information is gained on the mechanics of the flexor mechanism with this type of dynamic imaging. For example, we discovered when the finger is actively flexed and the probe is placed within zone II of the flexor tendons, the 2 slips of FDS are seen moving from volar to FDP to dorsal to FDP (Online Video 1).
Nerve
Conventional ultrasound has been used for decades to evaluate the median nerve for carpal tunnel syndrome. Wong et al demonstrated in 2002 that a cross-sectional area (CSA) of the median nerve at carpal tunnel inlet greater than 0.098 cm2 is both sensitive (88%) and specific (83%) for the diagnosis of carpal tunnel syndrome.17 More recent studies have shown that the cross-sectional area of the nerve correlates significantly with the severity of nerve impairment seen on nerve conduction studies.4
With UHFUS, the median nerve in the distal forearm and carpal tunnel can be quickly and simply visualized to measure the CSA of the nerve. In cross section, the nerve appears as an elliptical structure with a honeycomb fascicular architecture. Each fascicle is round and hypoechoic surrounded by a hyperechoic rim (Figure 5). The motor group can be seen as a smaller fascicular group on the radial side of the nerve, separate from the larger sensory group. At this level, the small recurrent motor branch can be tracked from its take-off to a point distal to the transverse carpal ligament, allowing the surgeon to identify which course the nerve takes relative to the ligament.
Figure 5.
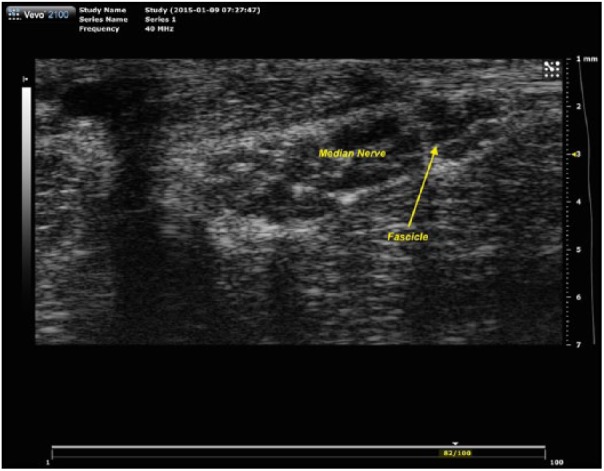
Cross-sectional view of the median nerve just proximal to the carpal tunnel, showing a hyperechoic ring surrounding each fascicle and the motor fascicular group at the right side of the nerve.
In the finger, UHFUS has the resolution to visualize individual fascicles in the proper digital nerves (Figure 6). Such high resolution provides the surgeon the capability to definitively determine the exact level and type of digital nerve injury. Similarly, UHFUS has the capacity to detect small neuromas within the fingers or at an amputation stump. In the only other published report of using UHFUS to image sensory nerves in the hand, Stokvis et al describe imaging structures as small as cutaneous branches in the hand and fingers in cadavers using an 82.5-MHz probe.15
Figure 6.
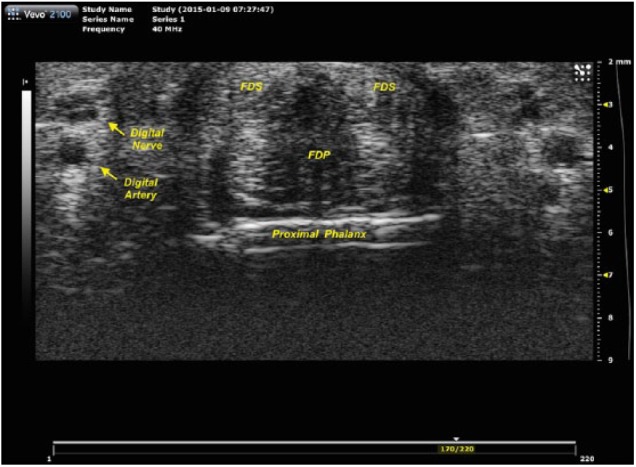
Cross-sectional view of the proximal segment of the finger showing the flexor tendons, digital arteries, and digital nerves.
Note. FDS = flexor digitorum superficialis; FDP = flexor digitorum profundus.
Blood Vessels
The imaging power of UHFUS is particularly advantageous when imaging vascular structures. Color Doppler ultrasound provides both quantitative and qualitative information about vessel flow, which is critically important when evaluating for vessel thrombosis or injury. Conditions such as hypothenar hammer syndrome can be diagnosed at the point of care without the need for more expensive or invasive modes of angiography.5 But more importantly, the UHFUS technology also provides information about the quality of the vessel wall itself by measurements of intimal thickness. Ultrahigh frequency probes clearly delineate the individual layers of the vessel walls, with the intimal layer appearing as a bright hyperechoic layer between the vessel lumen and the hypoechoic medial layer (Figures 7a and 7b).
Figure 7.
(a) Axial view of the radial artery along its long access demonstrating the intima as a bright hyperechoic layer between the lumen and the hypoechoic media layer and (b) cross-sectional view of the radial artery and its venae comitantes (VC).
Discussion
Few human studies have tested the use of UHFUS, and even fewer have used the technology in the hand and wrist. As described above, UHFUS has been used to accurately identify small cutaneous sensory nerves in the hand, which demonstrates the technology’s high tissue resolution for superficial structures.15 Another study used UHFUS to image the complex, but small, anatomy of the nail unit. The authors obtained detailed images of the nail fold, matrix, root, and plate along with their vascular supply. They continued to assert that the technology is promising for other dermatologic applications such as imaging the layers of the skin and hair follicles.1
Others have investigated the clinical implications the high-resolution images obtained of the peripheral vascular system provided by UHFUS. A study by Myredal et al used UHFUS with a 55-MHz probe to measure the intimal thickness of the radial artery in individuals with hypertension and prehypertension compared with a matched group without hypertension. They found that the intimal layer averaged 12% to 14% thicker in the hypertension and prehypertension cohorts.8 Intimal thickness has long been considered a marker for atherosclerosis and is an independent predictor of severe cardiovascular events.18 Schneeberger et al described the use of UHFUS measurement of the intima-media thickness of the radial and ulnar arteries at 1 year following hand allotransplantation to monitor for chronic graft rejection.11 By using the intimal thickness as a marker for atherosclerosis, the hand surgeon can gain valuable information that can guide decision making when considering procedures such as replantation or flap-based reconstructions that strongly depend on vessel quality.
Moreover, diagnostic ultrasound is relatively inexpensive when compared with other musculoskeletal imaging modalities. In a study by Sistrom and McKay, the average operating costs and charges of computed tomography (CT), ultrasound and radiography, nuclear medicine, and MRI were compared across hospitals in the state of Florida. The average charge per procedure for ultrasound and radiography was $410 compared with $1565 and $2048 for CT and MRI, respectively.12 A recent review of musculoskeletal imaging costs and cost-effectiveness demonstrates that musculoskeletal ultrasound could be substituted for MRI for 45.4% of all musculoskeletal diagnoses without significant reduction in diagnostic sensitivity. For the hand and wrist, that figure increases to 77.2%. In addition, the authors report a potential cost savings of more than $6.9 billion over the period of 2006 to 2020 if ultrasound were substituted for MRI when possible.9
The purpose of our study is to outline the capabilities of a novel technology and to describe feasible clinical applications for hand surgery. It is the authors’ opinion that the Vevo ultrahigh frequency imaging system is a powerful tool that can be deployed by the hand surgeon in bedside or “point of care” setting. With a small early investment into the basics of ultrasound imaging techniques, hand surgeons will be able to combine their extensive knowledge of hand anatomy with the abilities of the UHFUS to obtain valuable clinical images and data. Moreover, such examinations may often obviate the need for otherwise expensive, time-consuming, or invasive modes of imaging. As smaller, more streamlined machines come into production, UHFUS will become as easy to deploy as other commonly used bedside ultrasound devices.
Nevertheless, collaboration with formally trained ultrasound technicians will maximize the clinical capability of UHFUS. The limitations of ultrasound examination have been well described. In contrast to other imaging modalities, diagnostic accuracy is highly dependent on the experience and skill of the operator. For this reason, the authors recommend formal ultrasound evaluation for any injury or pathology that the hand surgeon is not comfortable or confident imaging at the point of care.
Our study demonstrates the feasibility and diagnostic potential of UHFUS. The technology can accurately and reliably identify the clinically important structures in the hand and wrist. UHFUS can be employed to diagnose the presence and location of foreign bodies, soft tissue masses, fluid collections, tendon rupture and tendonopathies, neuromas and nerve injuries, vascular lesions, atherosclerosis, and vessel thrombosis. While this study is limited by its shortage of clinical data, it illustrates the clinical value of the technology and the need for additional human prospective studies to expand and define the role of UHFUS in hand surgery.
Conclusion
UHFUS is an inexpensive, noninvasive, novel technology that shows multiple advantages over conventional ultrasound for imaging the fine superficial structures of the hand and wrist. The technology can be deployed at the point of care by the surgeon or by trained radiology technicians to diagnose a wide array of subcutaneous tissue, tendon, nerve, and vascular pathologies in the hand and wrist. In addition, UHFUS can obviate the need for more expensive, invasive, and time-consuming imaging modalities such as CT, MRI, and angiography.
Supplementary Material
Acknowledgments
The authors acknowledge and thank FUJIFILM VisualSonics Inc (Toronto, Ontario, Canada) for the use of the Vevo 2100 imaging system.
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Berritto D, Iacobellis F, Rossi C, et al. Ultra high-frequency ultrasound: new capabilities for nail anatomy exploration. J Dermatol. 2016;44(1):43-46. [DOI] [PubMed] [Google Scholar]
- 2. Bray PW, Mahoney JL, Campbell JP. Sensitivity and specificity of ultrasound in the diagnosis of foreign bodies in the hand. J Hand Surg Am. 1995;20(4):661-666. [DOI] [PubMed] [Google Scholar]
- 3. Guerini H, Morvan G, Vuillemin V, et al. Ultrasound of wrist and hand masses. Diagn Interv Imaging. 2015;96(12):1247-1260. [DOI] [PubMed] [Google Scholar]
- 4. Karadag YS, Karadag O, Cicekli E, et al. Severity of carpal tunnel syndrome assessed with high frequency ultrasonography. Rheumatol Int. 2010;30(6):761-765. [DOI] [PubMed] [Google Scholar]
- 5. Ken J, Khangura D, Stickles SP. Point-of-care ultrasound to identify distal ulnar artery thrombosis: case of hypothenar hammer syndrome. West J Emerg Med. 2015;16(4):565-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kessler JM, de la Lama M, Umans HR, et al. High-frequency sonography of the volar digital nerves of the hand. Muscle Nerve. 2012;45(2):222-226. [DOI] [PubMed] [Google Scholar]
- 7. Middleton WD, Teefey SA, Boyer MI. Hand and wrist sonography. Ultrasound Q. 2001;17(1):21-36. [DOI] [PubMed] [Google Scholar]
- 8. Myredal A, Gan LM, Osika W, et al. Increased intima thickness of the radial artery in individuals with prehypertension and hypertension. Atherosclerosis. 2010;209(1):147-151. [DOI] [PubMed] [Google Scholar]
- 9. Parker L, Nazarian LN, Carrino JA, et al. Musculoskeletal imaging: Medicare use, costs, and potential for cost substitution. J Am Coll Radiol. 2008;5(3):182-188. [DOI] [PubMed] [Google Scholar]
- 10. Read JW, Conolly WB, Lanzetta M, et al. Diagnostic ultrasound of the hand and wrist. J Hand Surg Am. 1996;21(6):1004-1010. [DOI] [PubMed] [Google Scholar]
- 11. Schneeberger S, Gorantla VS, Brandacher G, et al. Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Ann Surg. 2013;257(2):345-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sistrom CL, McKay NL. Costs, charges, and revenues for hospital diagnostic imaging procedures: differences by modality and hospital characteristics. J Am Coll Radiol. 2005;2(6):511-519. [DOI] [PubMed] [Google Scholar]
- 13. Sofka CM. Ultrasound of the hand and wrist. Ultrasound Q. 2014;30(3):184-192. [DOI] [PubMed] [Google Scholar]
- 14. Starr HM, Jr, Sedgley MD, Murphy MS. Ultrasound in hand surgery. J Hand Surg Am. 2014;39(12):2522-2524. [DOI] [PubMed] [Google Scholar]
- 15. Stokvis A, Van Neck JW, Van Dijke CF, et al. High-resolution ultrasonography of the cutaneous nerve branches in the hand and wrist. J Hand Surg Eur Vol. 2009;34(6):766-771. [DOI] [PubMed] [Google Scholar]
- 16. Teefey SA, Dahiya N, Middleton WD, et al. Ganglia of the hand and wrist: a sonographic analysis. AJR Am J Roentgenol. 2008;191(3):716-720. [DOI] [PubMed] [Google Scholar]
- 17. Wong SM, Griffith JF, Hui AC, et al. Discriminatory sonographic criteria for the diagnosis of carpal tunnel syndrome. Arthritis Rheum. 2002;46(7):1914-1921. [DOI] [PubMed] [Google Scholar]
- 18. Zielinski T, Dzielinska Z, Januszewicz A, et al. Carotid intima-media thickness as a marker of cardiovascular risk in hypertensive patients with coronary artery disease. Am J Hypertens. 2007;20(10):1058-1064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.




