Abstract
Background: Lack of a universally accepted location and normal value limits the utility of measuring scapholunate diastasis. The primary purpose of this study was to define the optimal location to measure the scapholunate gap throughout sequential ligament transections. Secondary purposes were to compare plain radiographs with fluoroscopy and to evaluate interrater reliability in measuring scapholunate diastasis. Methods: Five cadaver forearms were imaged with intact carpal ligaments and after sequentially transecting the scapholunate, radioscaphocapitate, and scaphotrapezium-trapezoid ligaments. Plain radiographs and static fluoroscopic images were obtained with wrists in neutral and 30° ulnar deviation for each stage. Multiple reviewers performed measurements of the scapholunate interval at 3 separate locations. Mean distances were calculated and pairwise comparisons between groups were made. Intraclass correlation was calculated to determine interrater reliability. Results: Overall, measurements made in the middle of the scapholunate joint had the smallest margins of error for all imaging modalities, ligament disruptions, and wrist positions. For normal wrists, the mean scapholunate measurements were all less than 2.0 mm at the middle of the joint, regardless of imaging modality or wrist position. Fluoroscopy detected significance between more stages of instability than plain radiographs at the middle of the joint. Conclusions: Measurements in the middle of the scapholunate joint in neutral and 30° of ulnar deviation under fluoroscopic imaging best capture all stages of ligamentous disruptions. Measurements less than 2.0 mm at the middle of the scapholunate interval may be considered within normal range.
Keywords: scapholunate, scaphotrapezium-trapezoid, radioscaphocapitate, dorsal radiocarpal, dorsal intercarpal, carpal instability
Introduction
Disruption of scapholunate ligament is the most common cause of carpal instability, yet the optimal method to diagnose scapholunate dissociation remains controversial.5 One particular challenge is identifying the location to measure diastasis across the scapholunate joint. Proposed values range from 2 to 5 mm or simply wider than the uninjured wrist.2,4,7,10,12 Some authors recommend measuring from the proximal ulnar-most border of scaphoid to proximal radial-most border of lunate while others recommend using the middle of the joint.2,4,7,10,12 These discrepancies may be attributed to the retrospective nature of previous studies, variation in measurement techniques, lack of a control group to account for anatomic variations, and inadvertent disruption of secondary stabilizers of the scapholunate joint.
Screening radiographs may miss dynamic scapholunate instability if the secondary stabilizers remain intact. Studies of cadaveric wrists under cyclical loading have demonstrated attenuation of these secondary stabilizers over time.13-15 Missed injuries often become apparent on static radiographs months later only after these structures fail.
Several radiographic parameters have been proposed to detect static and dynamic instability on initial imaging to treat injuries expeditiously. Diastasis of the scapholunate joint is one commonly used parameter and has been shown to be an excellent indicator of scapholunate instability with high sensitivity.7,10 However, lack of a universally accepted measuring location or threshold value limit its utility. In addition, clinicians may prefer either plain radiographs or fluoroscopic imaging to screen for diastasis. Both modalities have high specificity and are quick, inexpensive, and convenient in many office settings before proceeding to more expensive and time-consuming imaging.6,10,16
Few studies have directly compared imaging methods. One recent cadaver study evaluated stress radiographs in detecting dynamic scapholunate instability. No more than 30° of ulnar deviation on plain radiographs and fluoroscopic imaging maximized the scapholunate diastasis.6 Diastasis throughout stages of instability was not evaluated, and only the middle of the scapholunate joint was used for measurements. Previous reports have shown that the primary stabilizer of the scapholunate joint is the scapholunate interosseous ligament (SLIL) and the most important secondary stabilizers are the radioscaphocapitate (RSC) and scaphotrapezium-trapezoid (ST) ligaments.13-15 The dorsal wrist ligaments also contribute to wrist kinematics and may have been violated in previous studies. Building on these works, the primary aim of this study was to define the optimal location to measure the scapholunate interval in normal wrists and throughout stages of static and dynamic instability. Secondary purposes were to compare plain radiographs with fluoroscopy and to describe interrater reliability in measuring scapholunate diastasis.
Material and Methods
Specimens
Five fresh-frozen cadaver distal forearms were screened for preexisting deformities using fluoroscopy and gross examination. All significant soft tissue around the wrist and bony anatomy remained intact prior to dissection. Each specimen was thawed to room temperature prior to any imaging and kept moist. Dissections were completed within 24 hours for each specimen.
Dissections
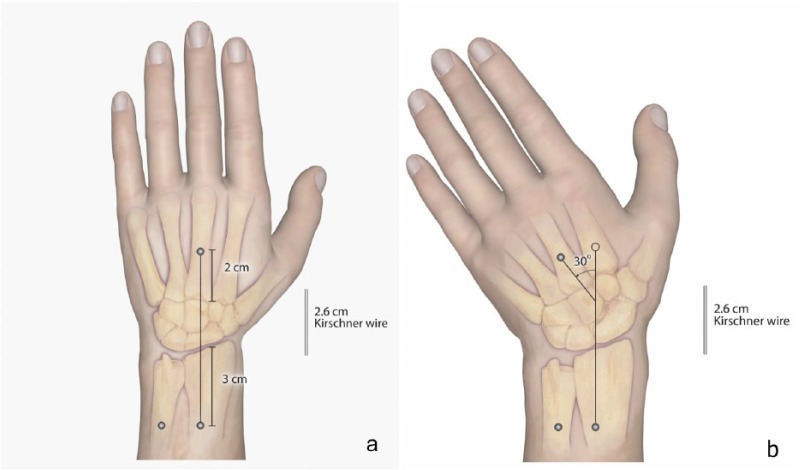
Each specimen was fixed to a flat wooden base using three 1/8 × 3-in headless pins (Stryker, Mahwah, New Jersey). Each specimen was positioned in the same fashion. One pin was placed into the midline of the radius 3 cm proximal to the radiocarpal joint. Another pin was placed parallel to the first into the middle of the ulna. A third pin was placed into the third metacarpal 2 cm distal to the carpometacarpal joint. Two 0.062 Kirschner wires, fixed at 30° to each other and the radial shaft, were placed on the wooden base adjacent to the specimens. To alternate between neutral and 30° ulnar wrist deviation, the third metacarpal pin was moved between 2 points (Figure 1). One hole was made with the third metacarpal parallel with the radial shaft and the other with the metacarpal 30° to the radial shaft using the Kirschner wires for reference. Angular measurements were calculated with a protractor and confirmed by digital calipers in a Picture Archiving Communication System (PACS; Philips Medical System, Eindhoven, The Netherlands). In addition, a 0.062 Kirschner wire 2.6 cm in length was placed within the imaging field of every image to calibrate measurements thereby minimizing magnification error.
Figure 1.
Illustrations of cadaver positioning.
Note. (a) Each specimen was fixed to a wooden base using headless pins in the radius, ulna, and third metacarpal as shown. (b) Ulnar deviation was achieved by translating the third metacarpal pin to a position in the base set at 30° to the radius shaft. A 2.6-cm Kirschner wire was placed within the field to calibrate digital measurements between all images.
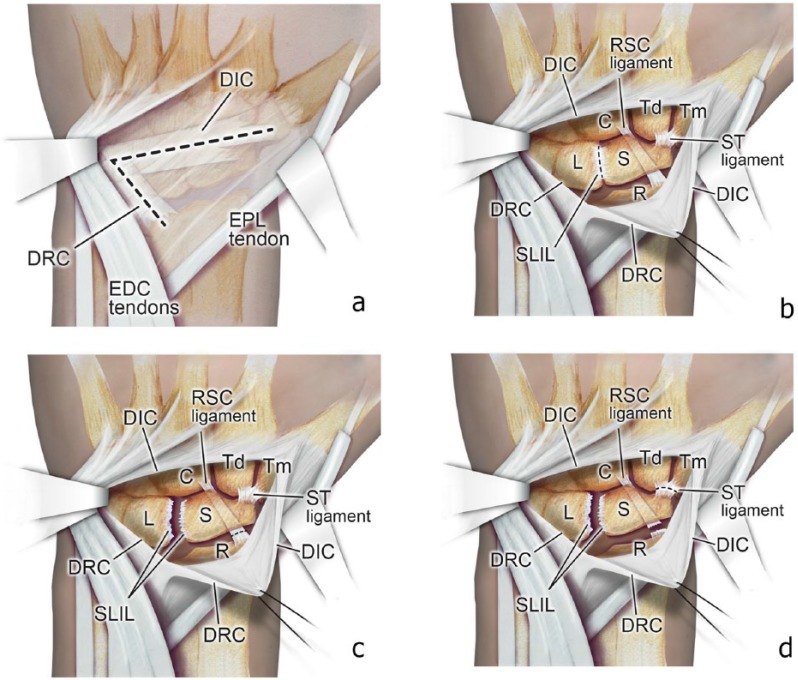
A standard dorsal longitudinal approach to the wrist was utilized, parallel with the third metacarpal and just ulnar to Lister tubercle. The fourth extensor compartment was retracted ulnarly, and third extensor compartment was released and retracted. A dorsal-ligament sparing capsulotomy using palpable landmarks described by Berger was performed (Figure 2).1 The studies by Short et al validated that this approach preserves carpal mechanics.13-15 Next, the capsular flap was elevated, preserving the intrinsic ligaments. Plain radiograph and fluoroscopic images were obtained before ligament dissection and after each ligament was transected. The SLIL was identified first and completely transected sharply using a No. 11 blade by palpation and direct visualization. The radioscapholunate ligament, which contributes little to carpal kinematics, was also transected.5 Next, the RSC ligament was identified and sharply transected between the scaphoid and radius in a similar fashion as previous described.13-15 Finally, the ST ligament was identified and transected sharply off the distal scaphoid.
Figure 2.
Illustrations of cadaver dissections.
Note. (a) The standard dorsal approach to the wrist is performed with retraction of the extensor digitorum comminus (EDC) and extensor pollicis longus (EPL) tendons. A ligament-preserving dorsal capsulotomy is shown by the dashed lines,1,2 (b) elevation of the capsular flap and transection of the scapholunate interosseous ligament (SLIL) is performed, (c) the radioscaphocapitate (RSC) ligament was transected between the radius and scaphoid, and (d) finally, the scaphotrapezium-trapezoid (ST) ligament was transected. DIC = dorsal intercarpal ligament; C = capitate; Td = trapezoid; Tm = trapezium; L = lunate; S = scaphoid; DRC = dorsal radiocarpal ligament; R = radius.
Imaging
All specimens were imaged in the same manner, alternating between the neutral and the 30° ulnar deviation positions. The specimens were transfixed to the wooden base in neutral flexion-extension during all imaging for consistent positioning. The X-ray beam was centered over the SLIL on each specimen to minimize parallax error. Standard posteroanterior (PA) wrist plain radiographs and static fluoroscopic images using a mini C-arm (OrthoScan, Scottsdale, Arizona) were taken under a single attempt with specimens in neutral wrist position with all ligaments intact. The specimens were then placed in the 30° ulnar deviation position by moving the third metacarpal parallel to the 30° Kirschner wire as described above. Plain radiographs and fluoroscopic imaging were taken again. The imaging sequence was repeated between interval sectioning of the SLIL, RSC, and ST ligaments. All images were stored in a PACS for review.
Analysis
Reviewers included 2 fellowship-trained musculoskeletal radiologists, 1 fellowship-trained senior orthopedic surgeon, and 1 senior orthopedic surgery resident. Radiographic images were transferred to ImageJ computer software (National Institutes of Health, Bethesda, Maryland).11 Using this software, magnification differences were accounted for by calibrating the image sizes with a 2.6-cm Kirschner wire placed in all radiographs. Images were cropped to reveal only the scapholunate interval. Reviewers then performed scapholunate measurements at the most distal joint space, middle joint space, and proximal ulnar-most border of scaphoid to proximal radial-most border of lunate described by Cautilli and Wehbe (Figure 3).2 Intraclass correlation (ICC) was calculated to determine interrater reliability. To do so, 10 identical images were randomly inserted into the blinded set of images each reviewer measured. The average measure ICC was then calculated between observers using a 2-way mixed model. Analysis of variance (ANOVA) tests were used to compare transection types at each of the 3 locations, followed by Tukey post hoc tests to identify differing pairs. Paired t tests were performed to compare plain radiographs and cineradiographs in neutral and ulnar deviation. All tests were performed using SPSS (version 21; SAS Institute, Cary, North Carolina) with significance set for values of P < .05.
Figure 3.
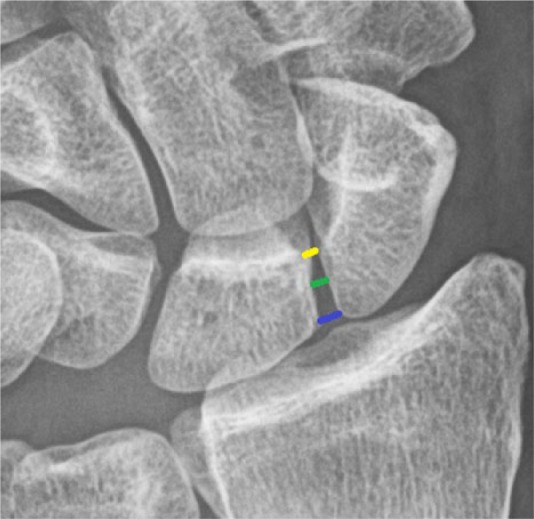
Plain radiograph demonstrating example locations for proximal (blue), middle (green), and distal (yellow) measurements in an intact scapholunate joint in neutral wrist position.
Results
The ICC showed that the overall interrater reliability was 92.0%. The mean measurements at each of the 3 locations are shown in Table 1. The means were calculated for both imaging modalities at both wrist position and at each stage of instability. ANOVA comparisons revealed significant differences between mean measurements. Pairwise comparisons between stages of instability were performed. Measurements at the middle of the joint had the most comparisons with significant differences and distal measurements had the least. Comparing wrist position, neutral imaging provided the most comparisons with significant differences but did not have significance when comparing normal and SLIL-disrupted wrists. Only ulnar deviation wrist positioning detected a significant difference between normal and SLIL-disrupted wrists. Disruption of the RSC was necessary for widening on neutral imaging. A paired t test was performed for plain radiographs and fluoroscopic images in neutral and ulnar deviation to compare imaging modalities. The differences between plain radiographs and fluoroscopic imaging were statistically significant for measurements in the middle of the joint. Specifically, fluoroscopic imaging detected significance between more stages of instability after accounting for radiographic magnification. In addition, mean measurements on fluoroscopic imaging were all larger than on plain radiographs.
Table 1.
Mean Scapholunate Measurements for Each Ligament Transection and Imaging Method.
| X-ray |
Cineradiography |
|||
|---|---|---|---|---|
| Neutral |
Ulnar deviation |
Neutral |
Ulnar deviation |
|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Normal | ||||
| Proximal | 1.90 ± 0.55 | 1.70 ± 1.00 | 2.33 ± 0.68 | 2.26 ± 0.88 |
| Middle | 0.77 ± 0.35 | 0.99 ± 0.54 | 1.21 ± 0.41 | 1.41 ± 0.73 |
| Distal | 0.40 ± 0.48 | 0.59 ± 0.57 | 0.95 ± 0.56 | 1.01 ± 0.66 |
| Scapholunate (SL) | ||||
| Proximal | 2.09 ± 0.99 | 2.47 ± 0.77 | 2.58 ± 1.09 | 2.80 ± 0.79 |
| Middle | 1.10 ± 0.74 | 1.64 ± 0.47 | 1.36 ± 0.72 | 2.30 ± 0.80 |
| Distal | 0.66 ± 0.77 | 1.13 ± 0.68 | 1.04 ± 0.77 | 1.69 ± 0.82 |
| Radioscaphocapitate (RSC) | ||||
| Proximal | 3.26 ± 0.62 | 3.03 ± 1.22 | 3.47 ± 0.74 | 3.22 ± 1.29 |
| Middle | 1.84 ± 0.54 | 1.79 ± 0.68 | 2.21 ± 0.46 | 2.22 ± 0.89 |
| Distal | 1.14 ± 0.89 | 1.10 ± 0.76 | 1.62 ± 0.70 | 1.66 ± 1.10 |
| Scaphotrapezium (ST) | ||||
| Proximal | 3.17 ± 1.07 | 2.78 ± 1.16 | 4.57 ± 0.83 | 3.64 ± 0.69 |
| Middle | 1.71 ± 0.74 | 2.14 ± 0.85 | 3.00 ± 0.88 | 2.91 ± 0.65 |
| Distal | 1.224 ± 0.94 | 1.42 ± 0.79 | 2.26 ± 1.12 | 2.28 ± 0.71 |
| P value | ||||
| Proximal | .000 (B, C, D, E) | .001 (B, C) | .000 (B, C, D, E, F) | .000 (B, C, E) |
| Middle | .000 (B, C, D, E) | .000 (A, B, C) | .000 (B, C, D, E, F) | .000 (A, B, C, F) |
| Distal | .003 (C, B) | .004 (C) | .000 (C, E) | .000 (C) |
Note. P values are for ANOVA comparisons of measurements at each location, between transections, and within each imaging type. Pairwise comparisons were made using Tukey tests. A = normal vs SL; B = normal vs RSC; C = normal vs ST; D = SL vs RSC; E = SL vs ST; F = RSC vs ST. ANOVA = analysis of variance.
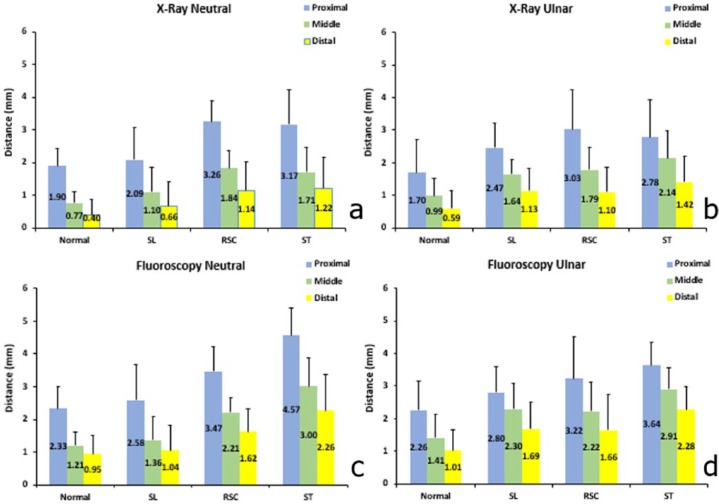
For normal wrists, the mean scapholunate measurements were all less than 2.0 mm at the middle of the joint, regardless of imaging modality or wrist position (Figure 4). Measurements at the middle of the joint also had the smallest margins of error across all imaging modalities, ligament disruptions, and wrist positions. Mean measurements made at the distal joint were always smallest, and proximal measurements were always largest in each group. Thirty degrees of ulnar deviation detected differences between normal and SLIL disrupted wrists, whereas neutral-position imaging could not (Figure 4).
Figure 4.
(a-d) Graphs depicting mean measurements ± standard deviation for neutral and ulnar deviation radiographs and for neutral and ulnar deviation fluoroscopy.
Note. Changes in measurements at each of the 3 locations are shown against each ligament dissection. SL = scapholunate interosseous ligament; RSC = radioscaphocapitate ligament; ST = scaphotrapezium-trapezoid ligament.
Discussion
Scapholunate diastasis provides a useful screening parameter for scapholunate dissociation, but there is no universally accepted normal value or location to measure it. Values reported in the literature range from 2 to 5 mm.2,4,7,10 The retrospective nature of these studies, variation in measurement techniques, lack of a control group to address anatomic variations, and inadvertent disruption of the secondary stabilizers of the scapholunate joint contribute to these discrepancies.2,4,7,10
In this study, measurements in the middle of the scapholunate interval captured the most stages of ligament disruptions. For normal wrists, the mean scapholunate measurements were all less than 2.0 mm at the middle of the joint, regardless of imaging modality or wrist position. The mean measurements at the middle of the joint did not exceed 2.5 mm for isolated scapholunate ligament disruption regardless of position or imaging modality. These findings are consistent with previous studies. Schimmerl-Metz et al evaluated normal scapholunate intervals on magnetic resonance imaging (MRI) and described 3 scapholunate morphologies: parallel congruent (78%), inverted Y (15%), and point-like (8%).12 The least variable location of measurement in that study was found to be in the middle of the joint, which coincides with the results in the current study. The variable morphology also explains variation in gapping seen in normal wrists.
Fluoroscopy had consistently larger measurements than plain radiographs after accounting for radiographic magnification. One possible explanation for the advantage of neutral fluoroscopic images over neutral plain radiographs is disambiguation of the measuring points for reviewers. Irregular joint surfaces combined with 2-dimensional imaging of 3-dimensional structures create variability in reference points. Scaphoid and lunate flexion or extension further complicate reproducible measuring points. With fluoroscopic imaging, the resolution may provide a more reproducible surface for measurements, obscuring point-like morphology described by Schimmerl-Metz et al. Nonetheless, this finding may not be clinically relevant.
This study builds on previous work of scapholunate stabilizers. Short et al published a series of biomechanical cadaver studies concluding that the RSC and ST ligaments are the most important secondary stabilizers.13-15 The dorsal wrist ligaments’ contribution to scapholunate stability has conflicting reports in the literature. Whereas Short et al attribute secondary influence of the dorsal radiocarpal (DRC) and dorsal intercarpal (DIC) ligaments on scapholunate stability, others have reported a more important role.3,8 It is possible that the dorsal ligaments have similar roles as the RSC and STT in that large changes are visibly only after dividing either of these secondary stabilizers as Werner et al have concluded.17 The discrepancy in the DRC and DIC contribution to stability may only be detectable with highly sensitive tracking devices used in the Short et al studies. Regardless, radiographic evidence of scapholunate diastasis should raise concern for a multiply injured wrist, and the conclusions in this study support measuring that diastasis in the middle of the joint.3
Fluoroscopic imaging is of particular use in assessing dynamic instability as the wrist can be taken through full radial to ulnar deviation in real time. However, the full range of motion under imaging may not be necessary in assessing scapholunate diastasis. In a cadaver study, Lee et al evaluated multiple stress imaging techniques on the size of the scapholunate interval.6 Ulnar deviation up to 30° with clenched-fist provided maximum diastasis of the scapholunate interval. The pencil-grip stress view provided 30° of ulnar deviation with a comparison view of the contralateral side as well. In clinical practice, the disadvantage of grip is that with wrist flexion or extension during grip stress views will profile the volar or dorsal aspects of the interval. As the volar and dorsal aspects are wider than the cartilage surface viewed on neutral PA views of wrists, flexion or extension views can show a falsely wide interval.12 To accommodate this change in profile in the current study would mean to compromise the positioning of the wrist between views. For these reasons, static neutral wrist views and 30° ulnar deviation views were chosen for this study.
This study has several limitations. The study uses a small cohort of cadavers. The irregular scapholunate joint surface contributed to variations in measurements between observers. Moneim originally described a method to better visualize the scapholunate space with 20° ulnar elevation.9 However, imaging specimens on a flat surface provided more reproducible wrist positioning and carpal alignment and emulates common clinical practice. For similar reasons, this study did not examine intercarpal angles. In practice, their clinical utility is limited by high variability among examiners and the need for perfect lateral positioning. For screening purposes, the scapholunate diastasis is more convenient.
Conclusion
Overall, the study adds to the literature regarding the optimum location to screen for scapholunate diastasis. The findings suggest that measurements in the middle of the scapholunate joint in neutral and 30° of ulnar deviation with fluoroscopy best capture all stages of ligamentous disruptions. Neutral imaging was necessary but not sufficient to detect all scapholunate diastasis. Adding 30° of ulnar deviation captures dynamic instability. Disruption of the RSC ligament was necessary for static instability. Measurements less than 2.0 mm at the middle of the scapholunate interval may be considered within normal range.
Acknowledgments
The authors thank Kathleen Gebhart, Director of Media Services, State University of New York at Stony Brook for illustrations.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statements of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: No informed consent was required for this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(1):54-59. [DOI] [PubMed] [Google Scholar]
- 2. Cautilli GP, Wehbe MA. Scapho-lunate distance and cortical ring sign. J Hand Surg Am. 1991;16(3):501-503. [DOI] [PubMed] [Google Scholar]
- 3. Elsaidi GA, Ruch DS, Kuzma GR, et al. Dorsal wrist ligament insertions stabilize the scapholunate interval: cadaver study. Clin Orthop Relat Res. 2004;(425):152-157. [DOI] [PubMed] [Google Scholar]
- 4. Kindynis P, Resnick D, Kang H, et al. Demonstration of the scapholunate space with radiography. Radiology. 1990;175(1):278-280. [DOI] [PubMed] [Google Scholar]
- 5. Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2008;33(6):998-1013. [DOI] [PubMed] [Google Scholar]
- 6. Lee S, Desai H, Silver B, et al. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg Am. 2011;36(7):1149-1157. [DOI] [PubMed] [Google Scholar]
- 7. Megerle K, Pohlmann S, Kloeters O, et al. The significance of conventional radiographic parameters in the diagnosis of scapholunate ligament lesions. Eur Radiol. 2011;21(1):176-181. [DOI] [PubMed] [Google Scholar]
- 8. Mitsuyasu H, Patterson RM, Shah MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg Am. 2004;29(2):279-288. [DOI] [PubMed] [Google Scholar]
- 9. Moneim MS. The tangential posteroanterior radiograph to demonstrate scapholunate dissociation. J Bone Joint Surg Am. 1981;63(8):1324-1326. [PubMed] [Google Scholar]
- 10. Pliefke J, Stengel D, Rademacher G, et al. Diagnostic accuracy of plain radiographs and cineradiography in diagnosing traumatic scapholunate dissociation. Skeletal Radiol. 2008;37(2):139-145. [DOI] [PubMed] [Google Scholar]
- 11. Rasband WS. ImageJ. Bethesda, MD: US National Institutes of Health; 1997-2015. http://imagej.nih.gov/ij/. Accessed August 12, 2017. [Google Scholar]
- 12. Schimmerl-Metz S, Metz V, Totterman S, et al. Radiologic measurement of the scapholunate joint: implications of biologic variation in scapholunate joint morphology. J Hand Surg Am. 1999;24(6):1237-1244. [DOI] [PubMed] [Google Scholar]
- 13. Short W, Werner F, Fortino MD, et al. A dynamic biomechanical study of scapholunate ligament sectioning. J Hand Surg Am. 1995;20(6):986-999. [DOI] [PubMed] [Google Scholar]
- 14. Short W, Werner F, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate. J Hand Surg Am. 2002;27(6):991-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Short W, Werner F, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part III. J Hand Surg Am. 2007;32(3):297-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sulkers G, Schep N, Maas M, et al. Intraobserver and interobserver variability in diagnosing scapholunate dissociation by cineradiography. J Hand Surg Am. 2014;39(6):1050-1054. [DOI] [PubMed] [Google Scholar]
- 17. Werner FW, Sutton LG, Allison MA, et al. Scaphoid and lunate translation in the intact wrist and following ligament resection: a cadaver study. J Hand Surg Am. 2011;36(2):291-298. [DOI] [PMC free article] [PubMed] [Google Scholar]