Abstract
Background Appropriate management of attention-deficit/hyperactivity disorder (ADHD) involves parents, clinicians, and teachers. Fragmentation of interventions between different settings can lead to suboptimal care and outcomes. Electronic systems can bridge gaps across settings. Our institution developed an email-based software to collect ADHD information from parents and teachers, which delivered data directly to the clinician within the electronic health record (EHR).
Objective We sought to adapt our institution's existing EHR-linked system for ADHD symptom monitoring to support communication between parents and teachers and then to assess child characteristics associated with sharing of ADHD information.
Methods We updated our software to support automated sharing of ADHD information between parents and teachers. Sharing was optional for parents but obligatory for teachers. We conducted a retrospective cohort study involving 590 patients at 31 primary care sites to evaluate a system for sharing of ADHD-specific health information between parents and teachers. We used multivariable logistic regression to estimate associations between child characteristics and parental sharing. We further investigated the association between child characteristics and viewing of survey results delivered through the electronic communication system.
Results Most parents (64%) elected to share survey results with teachers at the first opportunity and the vast majority (80%) elected to share all possible information. Parents who elected to share usually continue sharing at subsequent opportunities (89%). Younger child age and performance impairments were associated with increased likelihood of sharing. However, parents viewed only 16% of teacher submitted surveys and teachers only viewed 30% of surveys shared by parents.
Conclusion This study demonstrates that electronic systems to capture ADHD information from parents and teachers can be adapted to support communication between them, and that parents are amenable to sharing ADHD information with teachers. However, strategies are needed to encourage viewing of shared information.
Keywords: attention-deficit/hyperactivity disorder, information dissemination, surveys and questionnaires, communications, other clinical informatics applications
Background and Significance
Attention-deficit/hyperactivity disorder (ADHD) is the most common inheritable chronic childhood neurobehavioral disorder, affecting approximately 6.5% of school-aged children. 1 2 3 The effects of ADHD manifest in multiple environments, but most commonly lead to issues at both home and school. 2 As a result, effective management of children with ADHD involves collaboration between parents, clinicians, and teachers. ADHD rating scales (e.g., Vanderbilt scales) are the standard method for clinicians to collect data and monitor disease severity during evaluation and treatment of ADHD. 2 4 In clinical practice, rating scales represent a one-way, parallel communication from parent and teacher to clinician; there is a missed opportunity to foster communication between parents and teachers, key members of a child's ADHD management team.
Recognizing the need for collaboration, the 2011 American Academy of Pediatrics Guidelines for the care of children with ADHD stress the need for shared decision making (SDM). 2 SDM involves the identification of possible treatment options, sharing of preferences and goals for intervention, and implementation of the preferred treatment plan. 5 Although research has begun to demonstrate benefits of SDM in ADHD care, 6 7 communication challenges between families, clinicians, and schools remain. Standard use of data collection instruments does not support SDM as parents and teachers do not have access to data collected by clinicians. The role of technology in facilitating this information sharing is under investigation. 8
Despite the need for teamwork across settings, fragmentation of interventions between schools and the health care system often undermines ADHD care and limits SDM. 9 10 11 12 Parents and teachers may wish to collaboratively set behavior and education goals informed by areas of concern identified during ADHD evaluations. In addition, through sharing parents may become aware of issues that present exclusively at school that should be addressed in treatment plans. When families experience difficulty communicating their preferences and goals for treatment to providers and educators involved in their child's care, the quality and adherence to treatment plans may be adversely impacted. 13 Despite ubiquitous mobile devices transforming interpersonal communication, 14 sharing of ADHD information between interested parties continues to be inconsistent. 15 16 Multiple barriers, including school policies, can lead to decreased communication between parents, teachers, and clinicians. 17 18 19 20 While validated rating scales have helped clinicians diagnose and monitor ADHD, 4 21 22 less work has been done to address barriers to communication and fragmentation of care, which can result in suboptimal outcomes. 15 16 17 In addition, poor communication and coordination may result in duplication of services and inadequate monitoring and tailoring of treatment to align with a child's needs and his or her family's preferences and goals. 23 24 Quality of care and uptake of evidence-based therapies have been reported to be low in poorly integrated systems. 9 20 25 Informatics-based interventions that can facilitate cross-systems collaboration and support ongoing communication are urgently needed. 16
Building on prior success in using an internally developed tool for ADHD monitoring by clinicians, 26 27 28 29 30 we sought to develop a system to improve communication between parents and teachers to decrease fragmentation of care. We targeted communication between parents and teachers due to recognition that this data exchange channel was unsupported by our electronic health record (EHR), and hypothesized that our current clinical decision support (CDS) could be modified to support this information sharing. During this study, we evaluated patient characteristics that may have influenced parents and teachers to use this system to share and view patient ADHD information. Recently, it has been demonstrated that Web-based portals help improve coordination among parents and providers for the management of pediatric chronic medical conditions. 31 32 Web-based interventions have been developed for ADHD as well, and have been shown to improve rating scale completion and patient satisfaction and patient outcomes. 26 33 34 35 36 37 Although portals have been developed for pediatricians to collect ADHD information from parents and teachers and can support communication, no previous interventions support automated sharing of ADHD survey responses between parents and teachers. Based on studies of children with other chronic medical conditions, 31 32 we hypothesized that parents of more severely affected children would be more likely to share information with teachers.
Objective
We sought to adapt our institution's EHR-linked system for ADHD symptom monitoring to support communication between parents and teachers. Upon completion, we then evaluated child characteristics associated with sharing of ADHD information to determine the relationship between socioeconomic and other clinical factors on willingness to share information.
Methods
Study Setting and Population
We conducted this study within the Children's Hospital of Philadelphia (CHOP) ambulatory care network. We undertook a retrospective cohort study to evaluate the use of a system, the ADHD Care Assistant, to facilitate sharing of information on ADHD symptoms, performance impairments, medication side effects, comorbid symptoms, and treatment goals between parents and teachers. The original software was made available on November 1, 2014. The study period began on January 25, 2017 when the updates to the software were implemented to allow for sharing between parents and teachers and ended on June 16, 2017 to align with the end of the school year. In our analysis, we included all patients whose parent/guardian used the ADHD Care Assistant at least once during the study period ( N = 590). A study flow diagram ( Fig. 1 ) demonstrates how the study sample was derived. The ADHD Care Assistant was displayed to clinicians for all patients with a diagnosis of ADHD or a chief complaint of “ behavior problem ” within the reason for visit select box. Use of this system was optional and offering it to families was solely at the discretion of the primary clinician. The institutional review board at CHOP approved this project and granted a waiver of consent.
Fig. 1.
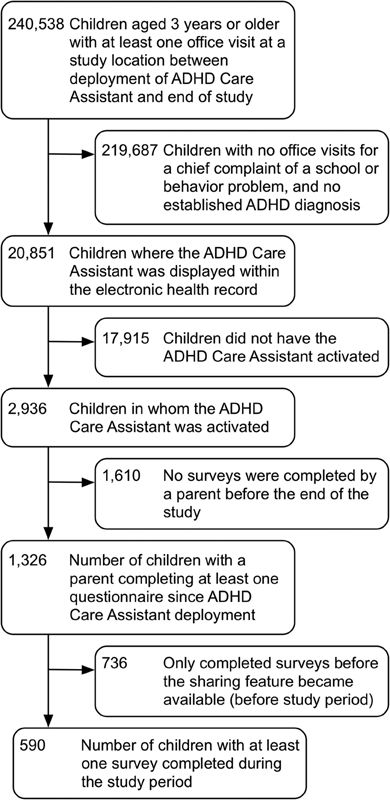
Study flow diagram. Approximately 8.7% of patients seen since the introduction of the attention-deficit/hyperactivity disorder (ADHD) Care Assistant have ADHD or had a concern raised for ADHD. Of these, 14% were registered by clinicians to use the intervention. Nearly half (45%) of parents who registered to use the intervention completed at least one survey. Of parents who used the system, 44% completed at least one survey during the study period.
The ADHD Care Assistant
The ADHD Care Assistant ( Fig. 2 ) is an internally developed CDS module used across the CHOP's network of 31 primary care sites to improve data collection from parents and teachers of school-aged children with ADHD. 26 Through the ADHD Care Assistant, a clinician can register a parent and teacher to receive scheduled ADHD symptom surveys, which are delivered directly to the parent's personal email address. A form given to the teacher provides instructions on how to register and receive surveys, which are then delivered directly to the teacher's email address. Parents and teachers completed surveys by clicking the survey-specific link and assessing information on symptoms, performance impairments, comorbid symptoms, and medication side effects based on the Vanderbilt ADHD Rating Scales. 4 21 In addition, parents provided information on their ADHD treatment preferences and goals using the ADHD Preference and Goal Instrument (PGI). 6 38 Both the Vanderbilt and PGI are validated survey instruments for children with ADHD. The initial parent survey instrument contained 104 questions while the initial teacher survey and follow-up survey instruments each contained approximately 45 questions. Prior to initializing emailed surveys, a clinician obtains a Health Insurance Portability and Accountability Act (HIPAA) release in the office and gave the parent a Family Educational Rights and Privacy Act (FERPA) release form so that the school could document parental permission for the teacher to use the system.
Fig. 2.
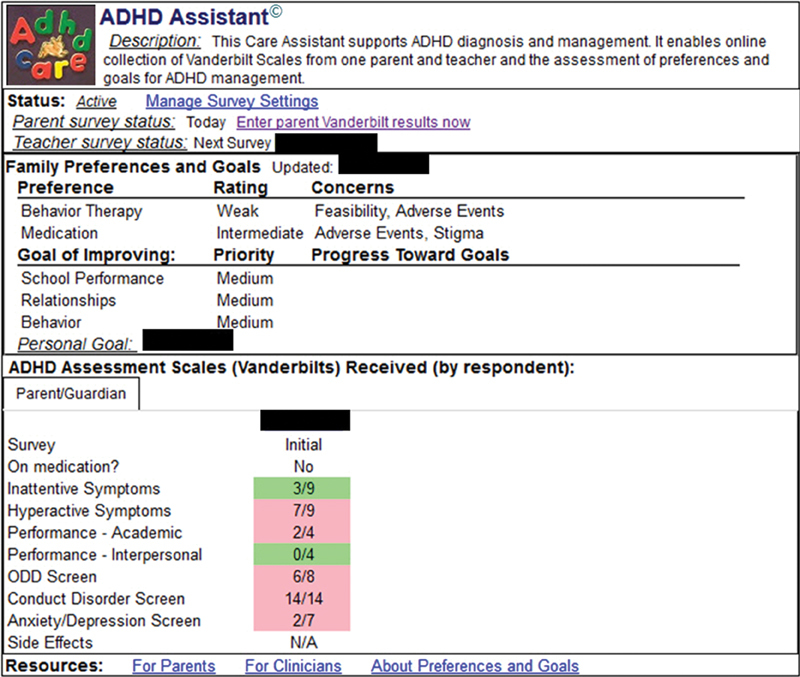
The Attention-Deficit/Hyperactivity Disorder (ADHD) Care Assistant . The ADHD Care Assistant has these functions: (1) email-based support for gathering information from parents and teachers including ADHD symptoms, performance impairments, and treatment preferences and goals, (2) automatic delivery of information to clinicians through the electronic health record (EHR), and (3) links to educational materials.
Our institution uses this system for children with behavior concerns as a screening tool and to track symptom severity, performance, treatment goals, and, when applicable, medication side effects for patients diagnosed with ADHD. No particular script was provided to help clinicians introduce the system. Use of the system was voluntary and activation of the system required a primary care clinical encounter. In this system, parents annually updated their child's teacher. Consistent with standard practice, we initially developed this system with a unidirectional data flow from parents and teachers directly into the EHR for clinician review and did not facilitate parent–teacher communication. To inform development of the system to support parent–teacher communication, we solicited input from 8 parents, 11 pediatricians, and 8 educators in a series of stakeholder meetings between September 2015 and September 2016. Based on stakeholder input, we enhanced the system to support parents selectively sharing portions from each submitted survey with a teacher, a key feature not present in similar software systems, and one that had yet to be studied. Secure viewing of submitted surveys was achieved using Cisco Registered Envelope Service (Cisco System, Inc., San Jose, California, United States), which requires users to register prior to accessing secured messages. 39 The teacher–parent information sharing functionality is shown in Fig. 3 .
Fig. 3.
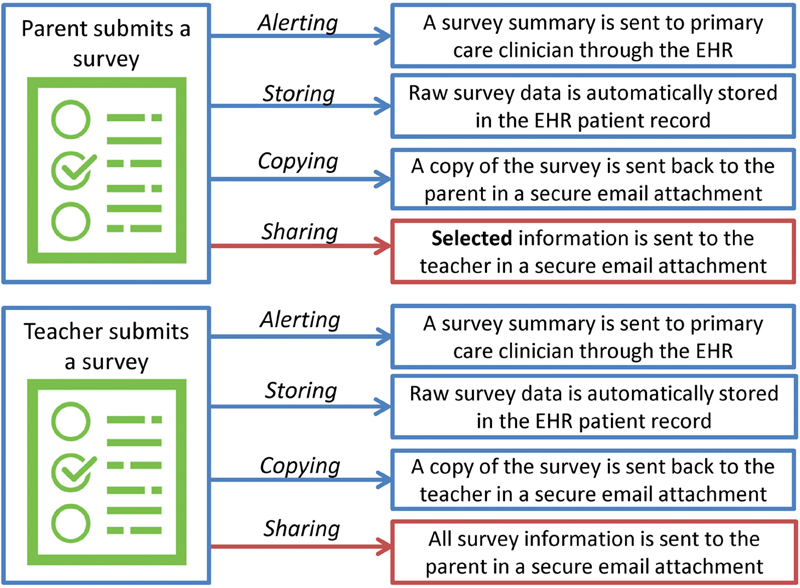
Messages handling upon survey completion. Upon survey submission, the clinician is alerted, the raw data are stored in the electronic health record (EHR), and a copy is sent to the survey submitter. Parent survey data can be selectively shared with teachers and teacher survey data are automatically shared with parents.
Endpoints
We selected as the primary study endpoint parent/guardian sharing of any component of the parent ADHD survey at first opportunity during the study period. When sharing occurred, we further analyzed the type of information shared (symptoms, performance, goals, and/or medication side effects). For patients with multiple opportunities to share, we conducted a secondary analysis to assess patterns in sharing over the study period. For this secondary analysis, we restricted the sample to children whose parent/guardian shared at the first opportunity and completed at least two surveys during the study period. Finally, we investigated the frequency with which teachers and parents viewed shared information. For this analysis, we included all surveys completed during the study period for our study population.
Child Characteristics Associated with Parent Sharing
We assessed child characteristics that were potential drivers of parent/guardian sharing. Characteristics included ADHD symptom and performance scores calculated using standard Vanderbilt Rating Scale scoring practices. 4 Specific characteristics used in the analysis included: (1) ADHD symptoms (categorized as no symptoms, inattentiveness only, hyperactivity only, or combined symptoms), (2) performance impairment (categorized as no impairments, academic impairment only, interpersonal impairment only, or both), (3) symptoms of comorbidities (none, any, and symptoms for oppositional defiance disorder, conduct disorder, or anxiety/depression), (4) prior diagnosis or problem list entry of ADHD, (5) medication side effects (categorized as none, mild, or moderate/severe side effects), (6) survey type (initial or follow-up), and (7) completion of a teacher survey during the study period. In our primary analysis, we included each family's first survey during the study period. That first survey could be either an initial or follow-up ADHD rating scale survey depending on whether it was the parent's first time using the ADHD Care Assistant rating scale collection system (initial survey) or whether they were already using the system at the start of the study (follow-up survey). While the initial and follow-up survey both have sections addressing symptom and performance impairment, it is important to note that only the initial survey contained the treatment goal section and only the follow-up survey contained the medication side effect section. Parent, clinician, and teacher demographics were not obtained as part of this study as we relied on data collected during the provision of routine medical care.
Covariates
Covariates included patient age (3–12 vs. 13–18 years), sex, race (white, African American, or other race), Hispanic/Latino ethnicity, insurance status (Medicaid vs. private), practice setting (urban vs. suburban), ADHD medication orders, and parent report of ADHD medication use. We selected these age ranges to evaluate differences in sharing in primary school versus high school. Ten parents of preschool-aged children used the system to submit ADHD information from parents and preschool educators. We performed a subgroup analysis on the 9- to 12-year-old cohort to assess if this population was significantly different from the younger primary school group. If either a parent reported ADHD medication use on the survey or the EHR contained an order for ADHD medications, this patient was classified as a medication user.
Statistical Analysis
We examined the distribution of ADHD characteristics and patient demographics in the study population. For our primary analysis, we examined bivariate associations between these characteristics and whether parents decided to share information at the first opportunity using chi-squared tests. After identifying patient ADHD characteristics associated with sharing (at the p < 0.1 level), we used multivariable logistic regression to estimate associations of these characteristics with sharing at the first opportunity. Characteristics examined in the full model included ADHD symptoms, performance impairments, survey type, and teacher survey completion. We controlled for patient covariates that were associated with sharing in bivariate analyses, including age, race, insurance status, and ADHD medication use based on documentation in either the EHR or parent report through the ADHD Care Assistant.
We then examined viewing patterns of survey results by parents and teachers. We calculated the proportions of shared parent surveys that were viewed by the teacher and teacher surveys that were viewed by the parent (all teacher surveys are shared automatically). We looked for associations between patient characteristics and teacher viewing of surveys. Finally, we examined patterns of sharing over time. We calculated the proportion of children whose parent/guardian shared at least two surveys, and examined the distribution of total number of surveys shared by each parent. We examined whether there were differences in parent and teacher viewing of survey results between parents who chose to share a subsequent survey and those who did not.
Results
Study Population
Between January 25, 2017 and June 16, 2017, 590 parents/guardians completed at least one survey using the ADHD Care Assistant for their child; 232 of these children had a teacher survey completed during the study period (39.3%). A total of 1,006 parent surveys and 493 teacher surveys were completed overall (range: 1–10 parent surveys per child and 0–10 teacher surveys per child).
Table 1 presents the distribution of demographic characteristics of the study population. Most children (88%) in the study had a diagnosis of ADHD either before or during the study period. Overall, 85.9% of patients were aged 3 to 12 years, 70.2% were male. Note that 48.3% were white, 40.0% were African American, and 5.1% were Hispanic/Latino. A total of 63.6% were privately insured, and 61.5% were from suburban practices. ADHD medication use was documented and/or reported for 87% of children.
Table 1. Demographic and clinical characteristics of study population and bivariate associations with whether parents chose to share ADHD survey information with teachers on the first survey in the study period.
| Demographic characteristic | N (%) with characteristic (column %) | Shared at first opportunity a – N (row %) | p -Value c |
|---|---|---|---|
| Total, N | 590 | 380 (64.4) | |
| Age (y) | < 0.001 | ||
| 3–12 | 507 (85.9) | 345 (68.1) | |
| 13–18 | 83 (14.1) | 35 (42.2) | |
| Sex | 0.8 | ||
| Male | 414 (70.2) | 268 (64.7) | |
| Female | 176 (29.8) | 112 (63.6) | |
| Race | 0.03 | ||
| White | 285 (48.3) | 169 (59.3) | |
| African American | 236 (40.0) | 160 (67.8) | |
| Other race | 69 (11.7) | 51 (73.9) | |
| Ethnicity | 0.3 | ||
| Hispanic/Latino | 30 (5.1) | 22 (73.3) | |
| Not Hispanic/Latino | 560 (94.9) | 358 (63.9) | |
| Insurance status | 0.06 | ||
| Medicaid | 215 (36.4) | 149 (69.3) | |
| Private | 375 (63.6) | 231 (61.6) | |
| Primary care practice type | 0.1 | ||
| Urban | 227 (38.5) | 155 (68.3) | |
| Suburban | 363 (61.5) | 225 (62.0) | |
| ADHD medication use b | < 0.001 | ||
| Yes | 513 (86.9) | 314 (61.2) | |
| No | 77 (13.1) | 66 (85.7) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; EHR, electronic health record.
Parent and teacher surveys were administered at regular intervals set by the child's primary care clinician. In our primary analysis, we included each family's first survey during the study period and determined whether the parent chose to share any component of the survey with their child's teacher.
Based on EHR documentation and parent report. Of children with medications listed on medication recorded in the EHR, 92.0% were on a stimulant only, 4.7% were on a stimulant and either an α agonist or atomoxetine, 1% were on an α agonist only, and < 1% were on other combinations.
p -Values calculated using chi-squared tests to compare the proportion of parents in each category that chose to share information with teachers at the first opportunity.
Value of Sharing to Parent and Teacher Stakeholders
During the preimplementation stakeholder meetings, parents and teachers both indicated desire for access to the information they personally submitted and to the information that was submitted by their counterparts. Stakeholder parents expressed concern that some parents may wish to control which information was shared with the teacher, using examples from the Vanderbilt Rating Scale of answers to particular questions that people may not like to share (e.g., #32: Has stolen things that have value). 21 To address this acceptability concern, we developed our system to allow selective sharing at the section level. The shareable sections were ADHD symptoms, performance impairments, treatment goals (initial survey only), and medication side effects (follow-up surveys only).
Parents and teachers both requested to see “what the clinician sees” in terms of presentation of results. To support this function, we provided both a longitudinal view and raw data within the reports sent to parents and teachers. We used the same color-coding of results that was provided to clinicians—green for good, yellow for borderline, and red for areas of concern. We did not provide scores or cutoffs for diagnosis, as this was felt to be beyond the reach of the CDS application and would not facilitate communication between parents and teachers.
Parent and teacher stakeholders reviewed prototype reports and provided feedback during the iterative development process. The stakeholders indicated that the layout and content of the result reports in their final form would be beneficial in supporting SDM surrounding ADHD diagnosis and management ( Fig. 4 ). Overall, stakeholders valued the possibility of an electronic tool to address known difficulties in communication of ADHD information.
Fig. 4.
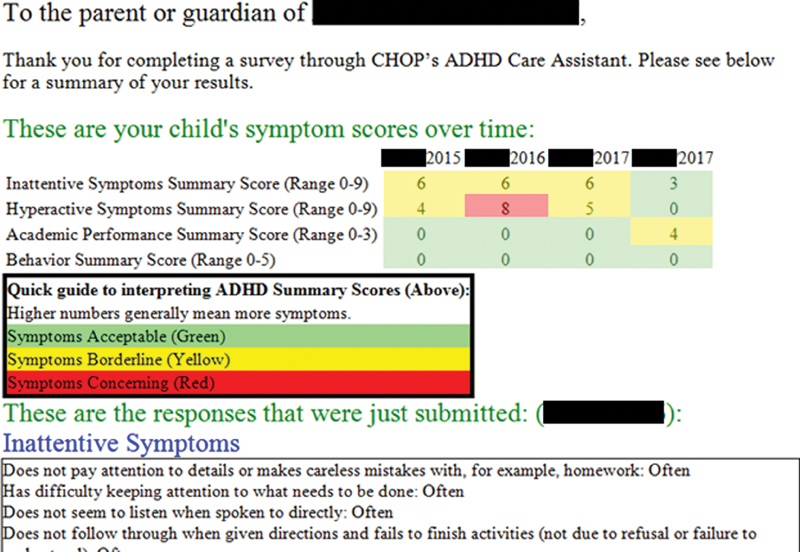
Example of emailed report sheet. This example of a patient-directed report sheet generated by the Attention-Deficit/Hyperactivity Disorder (ADHD) Care Assistant includes longitudinal data summarizing all scores submitted since the patient was registered and includes the questions/answers submitted on the most recent ADHD survey response. Parent and teachers reports are formatted the same.
Sharing at the First Opportunity
Out of 590 patients whose parent completed a survey during the study period, 380 parents chose to share results with their child's teacher at the first opportunity (64.4%, Table 1 ). Most parents (304, 80.0%) shared all sharable survey components with their child's teacher. In bivariate analysis, parents of children aged 3 to 12 and of children who were publically insured were more likely to share than parents of adolescents or parents of privately insured children ( Table 1 ). In a subgroup analysis, we noted no difference between the youngest (3–8 years) and middle aged (9–12 years) patient groups. Parents of white children were less likely to share, as were parents of children using medication for ADHD. Practice location (urban vs. suburban) did not affect the likelihood of decision to share.
In bivariate analyses ( Table 2 ), parents were more likely to share an initial compared with a follow-up survey ( p < 0.001). In addition, parents whose child was manifesting elevations in ADHD symptoms, performance impairments, or symptoms of any comorbidity (scoring as per Vanderbilt Rating Scale instructions) were significantly more likely to share information with teachers ( p < 0.05 for all comparisons). Having no prior diagnosis of ADHD was associated with an increased likelihood of a parent selecting to share the results with the teacher. Medication side effects were not associated with sharing. Parents of children whose teacher completed a survey during the follow-up period were also more likely to share information with teachers ( p = 0.001). In a secondary analysis, we looked at the relationship between parental preferences and goals and information sharing. We found that these were not associated ( p ≥ 0.05 for all preference and goal categories).
Table 2. Bivariate associations of ADHD characteristics with parents' decision to share information with teachers at the first opportunity.
| ADHD characteristics: Parent surveys a | N (%) with characteristic (column %) | Shared at first opportunity – N (row %) |
p -Value c |
|---|---|---|---|
| Total, N | 590 | 380 (64.4) | |
| Survey type | < 0.001 | ||
| Initial | 180 (30.5) | 141 (78.3) | |
| Follow-up | 410 (69.5) | 239 (58.3) | |
| Teacher completed survey during study | 0.001 | ||
| Yes | 232 (39.3) | 168 (72.4) | |
| No | 358 (60.7) | 212 (59.2) | |
| ADHD diagnosis or problem list entry | < 0.001 | ||
| Yes | 520 (88.1) | 325 (62.5) | |
| No | 70 (11.9) | 55 (78.6) | |
| ADHD symptoms reported b | 0.02 | ||
| No ADHD symptom criteria met | 302 (51.2) | 176 (58.3) | |
| Inattentive symptom criteria met | 124 (21.0) | 89 (71.8) | |
| Hyperactive symptom criteria met | 31 (5.3) | 21 (67.7) | |
| Both inattentive and hyperactive symptom criteria met | 133 (22.5) | 94 (70.7) | |
| Performance impairments b | < 0.001 | ||
| No impairment criteria met | 184 (31.2) | 95 (51.6) | |
| Academic only | 163 (27.6) | 115 (70.6) | |
| Interpersonal only | 69 (11.7) | 47 (68.1) | |
| Both academic and interpersonal | 174 (29.5) | 123 (70.7) | |
| Symptoms of comorbidities d ( N = 180) | 0.03 | ||
| No criteria for comorbidities met b | 102 (56.7) | 74 (72.6) | |
| Criteria met for 1 or more comorbidity | 78 (43.3) | 67 (85.9) | |
| Criteria met for specific comorbidities | |||
| Oppositional defiance | 66 (36.7) | 55 (83.3) | 0.2 |
| Conduct disorder | 12 (6.7) | 10 (83.3) | 0.7 |
| Anxiety or depression | 37 (20.6) | 34 (91.9) | 0.03 |
| Medication side effects ( N = 410) | 0.8 | ||
| No side effects | 46 (11.2) | 25 (54.4) | |
| Mild side effects | 119 (29.0) | 69 (58.0) | |
| Moderate/severe side effects | 245 (59.8) | 145 (59.2) |
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
ADHD symptoms and performance items were asked on both initial and follow-up surveys ( N = 590 parent surveys and 232 teacher surveys). Comorbidities were only assessed on initial surveys ( N = 180 parent surveys and 104 teacher surveys), while side effects were only assessed on follow-up surveys ( N = 410 parent surveys and 128 teacher surveys).
Scoring performed according to instructions provided in the Vanderbilt survey handout. No symptoms/evidence in each category indicates that a parent or teacher did not indicate a positive in any subsection of the scale. Inattentive and hyperactive symptoms require 6/9 positive responses. Other sections of the Vanderbilt had varying criterion for positives.
p -Values calculated using chi-squared tests to compare the proportion of parents in each category that chose to share information with teachers at the first opportunity.
This reflects symptoms of comorbidities reported by parent at time of survey completion—not diagnosed comorbidities. The comparator for each comorbidity group was no comorbidity. Many children screened positive for more than one comorbidity.
In multivariable models controlling for patient age, race, insurance status, and ADHD medication use, parents of children experiencing ADHD-related performance impairments in academics, interpersonal relationships, or both were significantly more likely to share relative to those with no impairments (odds ratios [ORs] of 1.95 [95% confidence interval [CI]: 1.21, 3.15], 2.03 [1.09, 3.76], and 2.09 [1.26, 3.44], respectively, Table 3 ). In addition, parents of children whose teacher had completed a survey during the study period had 1.5 times greater odds of sharing (OR, 1.52 [95% CI: 1.03, 2.23]. Finally, parents tended to be more likely to share an initial compared with a follow-up survey (OR, 1.61 [95% CI: 0.97, 2.66], p = 0.06). In these models, prior diagnosis of ADHD and ADHD symptom scores were not associated with information sharing.
Table 3. Multivariable associations of ADHD characteristics with parents' decision to share ADHD survey information with teachers at the first opportunity.
| Child's ADHD characteristics | Parent shared with teacher at first opportunity, odds ratio (95% CI) a |
|---|---|
| Survey type – Initial (vs. follow-up) | 1.61 (0.97, 2.66) |
| Teacher completed a survey during study (vs. not) | 1.52 (1.03, 2.23) |
| ADHD diagnosis or problem list entry | 0.79 (0.40, 1.59) |
| ADHD symptoms at time of survey completion | |
| No symptoms | Reference |
| Inattentiveness only | 1.12 (0.67, 1.88) |
| Hyperactivity only | 0.92 (0.40, 2.14) |
| Combined symptoms | 0.88 (0.52, 1.50) |
| ADHD-related performance impairments | |
| None | Reference |
| Academic impairment only | 1.95 (1.21, 3.15) |
| Interpersonal impairment only | 2.03 (1.09, 3.76) |
| Both academic and interpersonal impairments | 2.09 (1.26, 3.44) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; CI, confidence interval; EHR, electronic health record; OR, odds ratio.
Results are from multivariable logistic regression of the characteristics above and sharing at the first opportunity. ADHD characteristics that were included were bivariately associated with sharing ( p < 0.1 as cutoff). Models additionally adjusted for patient demographic and clinical characteristics that were bivariately associated with sharing, including child age, race, insurance payer, and ADHD medication use (documented in the EHR or based on parent report).
Viewing of Surveys
Of the 667 shared parent surveys, 107 (16.0%) were viewed by the child's teacher, whereas 149 of the 493 teacher surveys were viewed by parents (30.2%). Parents and teachers viewed their own survey results at similar rates: 71 out of 1,006 total parent surveys (7.1%) and 38 out of 493 total teacher surveys (7.7%) (chi-square, p = 0.2). Parents and teachers were both more likely to view information provided by the other rather than viewing their own results. There was no relationship between ADHD diagnosis and either parent or teacher viewing email results. Teachers of children in the suburban setting and of children with private insurance were significantly more likely to view shared surveys (8.8% vs. 20.3% [ p < 0.001] and 19.6% vs. 19.9% [ p = 0.001], respectively).
Subsequent Sharing
A total of 152 parents/guardians shared survey results with teachers on the first opportunity and completed at least two surveys during the study period (25.8% of the total sample). Among those with the opportunity to share again, 135 (88.8%) shared results with teachers on a second occasion. There was no difference in the percent of parents viewing teacher surveys between those who did and did not share a later survey (17.0% vs. 17.7%). In addition, 22 (30.9%) parents/guardians who elected not to share at the first opportunity did choose to share at a subsequent opportunity.
Discussion
Fragmentation of services may lead to care inefficiencies and suboptimal care. 15 Technology can help promote SDM and decrease fragmentation but has not been widely integrated in ADHD management. 40 SDM in ADHD depends upon information exchange among parents, clinicians, and teachers, yet multiple barriers to this process remain. Our results indicate that the majority of families were willing to share relevant health information with teachers using a technology-assisted approach, which can promote SDM. Performance impairments (OR, 2.09) were the strongest patient characteristic associated with sharing, with younger patient age also noted to be an important predictor, consistent with other literature on ADHD help-seeking adolescents. 41 42 Younger patient age was also noted to be an important predictor which may be reflective of a trend for parents to become less involved in their children's schooling when they become adolescents. 43 44 This is consistent with other studies addressing barriers to ADHD treatment. 20 Despite a large quantity of sharing, only a minority of shared surveys were viewed; parents and teachers viewed 16 and 30% of shared surveys, respectively.
Our results indicate that the majority of families are willing to share health information with teachers when that shared information is essential to effective treatment. Despite good reasons for having privacy laws (HIPAA for health care and FERPA for scholastic areas), these regulatory burdens can impair the sharing of information, even when all stakeholders agree that sharing is desirable. Our ADHD information sharing system, which adhered to all regulatory constraints, demonstrated that a technological approach to sharing is acceptable to families. Despite needing to opt in for sharing, most parents (64.4%) decided to share at least part of their survey responses with their child's teacher and 80% who elected to share, shared everything. We also found that parents who started using the system after the sharing features were activated (i.e., families completing initial Vanderbilt surveys with the new system) tended to share more than established users of the system (i.e., parents completing follow-up surveys when sharing features became available). This could reflect that the novelty of the system was a driving force for sharing. 45 46 Sharing rates for initial surveys may also be higher for other reasons, including potentially the ability to share the treatment goal section, which is unique to the initial survey. Those parents who elected to share on the initial survey were very likely to share subsequent surveys suggesting a perceived benefit for parents from sharing, given the need to opt in at each opportunity. 47 Other factors that could have influenced sharing include parental trust in the medical system and the influence of the primary care physician on the parent decision-making process, even outside of the office visit.
We hypothesized that increased ADHD severity would be associated with increased sharing. Interestingly, we found performance impairments were associated with sharing after controlling for confounding, but simply having symptoms was not. This finding likely reflects the perceived importance of performance (e.g., academic problems) as opposed to symptoms in seeking to enlist a teacher's help by sharing information. 41 42 48 49 Parents also could be more interested in sharing if they believed that there was something that needed to be fixed. 31 32 41 42 Our results suggest the need to especially encourage system use among families who most need support to address these impairments, as they are those most likely to utilize the tools.
Although sharing was common, our results indicate a need for developing improved strategies to support viewing of shared results. Despite only 16% of parents and 30% of teachers cross-reviewing submitted surveys, we were encouraged by these rates of viewing given numerous barriers to accessing messages through the secure messaging software. 39 These findings suggest that some families and teachers see more value in reviewing the information than others. There is known variation in patient engagement and adherence to recommendations in families of children with ADHD. 20 We could potentially improve sharing and viewing by highlighting these features during patient registration, providing support for clinicians, onboarding families, and facilitating teacher enrollment.
Within our system, viewing surveys required parents and teachers to access information through a secure email delivery service, which required its own logon and password. This process was thought to be more difficult than simply electing to share via a survey question. Simplifying access to this system using our institution's personal health record, providing logon support, the creation of a mobile-friendly portal, and/or allowing teachers restricted access to a patient's EHR portal could improve viewing of shared information. Evidence-based strategies could also be employed to encourage the viewing of shared information including sending electronic reminders or the use of incentives. 50 51 Teachers of children in suburban practices and on private insurance were more likely to view information, potentially indicating that socioeconomic status of the child or resources of the school system play a role in teachers viewing information. From stakeholders, we learned that urban teachers may be responsible for large numbers of students, with diverse educational needs, and time constraints alone may have limited viewing. Additional supports may be needed to help teachers in the urban setting and/or who provide education for children with public insurance in accessing and viewing the shared surveys. Finally, the emails only provided the data and data trends without guidance for parents or teachers on what to do next. Parents and teachers may have been less likely to open emails if they did not have a clear action to take based on the information provided. Future revisions to the tool may best support families if suggested actions are highlighted. It is also possible that the parents elected to share information with teachers without informing the teachers. In these circumstances, it would be entirely likely that a teacher would not view the email.
Many children with ADHD are managed by external providers, and clinicians caring for these patients would be unlikely to utilize the ADHD Care Assistant for these families, which helps to explain why only 14% of identified patients were registered for the system. In addition, certain clinicians and practices had existing established workflows for ADHD and were reluctant to change their processes by using the electronic system. This study had several limitations. The patients in this study represented a limited subset of all patients seen in our practices with ADHD and for whom screening for ADHD was triggered by the EHR. It may be difficult to draw generalizations to the larger population, especially those with ADHD managed outside of primary care or whose parents are less comfortable using technology to manage health concerns. The focus of the evaluation was selection of sharing for parents who already opted in to use the system. Parents who elected to use this system may be different from parents who opted not to use this system and why parents and teachers elected to complete or not complete a survey was beyond the scope of this study. An evaluation of the factors that influence use of this type of system will require future study. From a design standpoint, the use of observational data limits our ability to establish causation, and therefore it is difficult to identify precisely those factors that can improve sharing. We had limited control over when and why clinicians chose to use the system, resulting in activation of the system for children less than 5 years old. Given the small number of preschoolers included, it would be difficult to draw conclusions from this study for this population. We also lacked information regarding clinician, parent, and teacher demographics so we cannot draw conclusions related to nonpatient demographics. In addition, our reliance on technology may limit the generalizability of the approaches we used in health systems with older or more constrained EHRs, which are common in many practice settings. Nonetheless, Web services like Health Level-7's Fast Healthcare Interoperability Resources and our own Care Assistant framework are increasingly common with many EHR vendors and are likely to increasingly support the implementation of novel informatics approach to care, such as the partnership between families and teachers described in this article. As with many CDS interventions, sustainability and dissemination are concerns. We have transitioned ownership of this project from a research team to our operational team and hope to generate lessons learned about this process and to support dissemination beyond our organizational walls. Future studies involving this intervention will address how sharing of information impacts ADHD-related outcomes (i.e., symptoms, performance impairment, and medication use), the value of sharing ADHD scores between parents and teachers, whether we can decrease barriers to sharing of information, and whether this approach can be applied to other disorders affecting health and school performance.
Conclusion
Electronic tools to support communication can decrease fragmentation of care and support SDM for children with ADHD. Most parents were willing to share ADHD-related information with teachers, and those with more severely affected children were most likely to share information. Despite barriers to accessing information, parents and teachers successfully viewed the shared surveys at modest rates. System enhancements to facilitate the viewing of shared surveys are technologically feasible and should be explored in future studies. Future work is needed to determine if sharing information impacts patient care outcomes relevant to ADHD.
Clinical Relevance Statement
Treatment for children with ADHD is often fragmented leading to suboptimal care. Electronic tools may foster communication but have not yet been applied for improving communication among parents, teachers, and clinicians during the provision of ADHD management. We demonstrate the potential of using electronic systems provided by the medical home to promote parental sharing of information about their child's ADHD with teachers.
Multiple Choice Questions
-
Sharing of results and viewing of results were the two new functions developed and evaluated as part of the update to this intervention. Which of the following correctly match a clinical or patient characteristic with increased utilization of the new function?
Survey Type AND Sharing of Surveys by Parents.
Survey Type AND Viewing of Surveys by Teachers.
Suburban Office Setting AND Sharing of Surveys by Parents.
Suburban Office Setting AND Viewing of Surveys by Teachers.
Performance Impairments AND Sharing of Survey by Teachers.
Correct Answer: The correct answer is option d. This question addresses the evaluation of results presented using bivariate and covariate analysis. In bivariate analyses, potential relationships between patient characteristics may appear significant, but upon a covariate analysis, after controlling for patient demographics, these relationships may be found to no longer be significant. Answer a is only an association identified during the bivariate analyses. When controlling for patient characteristics, it was not found to be significant. Additionally, the question asks for a clinical or patient characteristic and this is an ADHD survey characteristic. Answer b is incorrect as viewing of surveys by teachers was not investigated for different survey types (insufficient power to perform this analysis). Answer c is incorrect as suburban office setting was found to be unrelated to sharing in the bivariate analysis. Answer d reports a correct association of a patient characteristic and a significant finding. Answer e is incorrect because it is sharing by parents and not sharing by teachers that was investigated.
-
Multiple potential barriers were identified to parent and teacher viewing of survey results. Which follow-up study could be performed to evaluate a potential solution to a technologic barrier of viewing emailed surveys?
Repeating the study with an increase in sample size to overcome barriers to viewing.
Randomizing parents to receive secure versus nonsecure emails with ADHD survey results.
Switching from an email-based system to a Web portal-based system for accessing records.
Compensating families and teachers each time they viewed a new survey result.
Allowing multiple teachers to have access to the system to increase the likelihood of a tech-savvy participant.
Correct Answer: The correct answer is option b. This question addresses different ways future studies could be performed to address technical limitations of this study. Answer b directly addresses the proposed technical limitation that SEND SECURE messages deter people from opening for results. Answer a would not address the technical barrier, but could be useful in determining if patient characteristics are related to viewing by increasing the study power. Answer c would potentially increase views but would not directly target the technical barrier of needing to have a login and password to obtain the results. Compensating families (answer d) might improve rates but would not address the technical barriers. Answer e would also potentially increase views but would not address the technical barriers.
Acknowledgments
We thank the network of primary care physicians and their patients and families for their contributions to clinical research through the CHOP ambulatory care network including involvement in the stakeholder workgroups which informed the updates to the ADHD Care Assistant. We wish to acknowledge Jeritt Thayer and Dean Karavite for their contributions to development and deployment of the ADHD Care Assistant.
Funding Statement
Funding This work was funded through the Patient Centered Outcomes Research Institute (CDR-1408–20669).
Conflict of Interest Dr. Michel, Dr. Grundmeier, and Mr. Miller are the primary authors of the ADHD Care Assistant, which was used to implement portions of the intervention evaluated in this article. No patent or licensing agreement exists for this technology and the invention has generated no revenue. The remaining authors have no conflicts of interest relevant to this article to disclose.
Drs. Grundmeier and Fiks are coinventors of the Care Assistant framework, which was used to implement portions of the intervention evaluated in this article. No patent or licensing agreement exists for this technology and the invention has generated no revenue. The remaining authors have no financial relationships relevant to this article to disclose. Though he personally took no salary support, Dr. Fiks's research team received grant support from Pfizer for an independent research project to improve ADHD care.
Protection of Human and Animal Subjects
This study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by the CHOP's Institutional Review Board.
References
- 1.Sharma A, Couture J. A review of the pathophysiology, etiology, and treatment of attention-deficit hyperactivity disorder (ADHD) Ann Pharmacother. 2014;48(02):209–225. doi: 10.1177/1060028013510699. [DOI] [PubMed] [Google Scholar]
- 2.Wolraich M, Brown L, Brown R T et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(05):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polanczyk G V, Willcutt E G, Salum G A, Kieling C, Rohde L A. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43(02):434–442. doi: 10.1093/ije/dyt261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolraich M L, Feurer I D, Hannah J N, Baumgaertel A, Pinnock T Y. Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. J Abnorm Child Psychol. 1998;26(02):141–152. doi: 10.1023/a:1022673906401. [DOI] [PubMed] [Google Scholar]
- 5.Murray E, Charles C, Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Educ Couns. 2006;62(02):205–211. doi: 10.1016/j.pec.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Fiks A G, Mayne S, Debartolo E, Power T J, Guevara J P. Parental preferences and goals regarding ADHD treatment. Pediatrics. 2013;132(04):692–702. doi: 10.1542/peds.2013-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brinkman W B, Hartl Majcher J, Poling L M et al. Shared decision-making to improve attention-deficit hyperactivity disorder care. Patient Educ Couns. 2013;93(01):95–101. doi: 10.1016/j.pec.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyon A R, Whitaker K, French W P, Richardson L P, Wasse J K, McCauley E.Collaborative care in schools: enhancing integration and impact in youth mental health Adv Sch Ment Health Promot 20169(3-4):148–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoagwood K, Kelleher K J, Feil M, Comer D M. Treatment services for children with ADHD: a national perspective. J Am Acad Child Adolesc Psychiatry. 2000;39(02):198–206. doi: 10.1097/00004583-200002000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Zwi M, Jones H, Thorgaard C, York A, Dennis J A. Parent training interventions for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev. 2011;(12):CD003018. doi: 10.1002/14651858.CD003018.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DuPaul G J, Gormley M J, Laracy S D. School-based interventions for elementary school students with ADHD. Child Adolesc Psychiatr Clin N Am. 2014;23(04):687–697. doi: 10.1016/j.chc.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Lange A M, Daley D, Frydenberg M, Rask C U, Sonuga-Barke E, Thomsen P H. The effectiveness of parent training as a treatment for preschool attention-deficit/hyperactivity disorder: study protocol for a randomized controlled, multicenter trial of the New Forest Parenting Program in Everyday Clinical Practice. JMIR Res Protoc. 2016;5(02):e51. doi: 10.2196/resprot.5319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wagner E H.The role of patient care teams in chronic disease management BMJ 2000320(7234):569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bilgrami Z, McLaughlin L, Milanaik R, Adesman A. Health implications of new-age technologies: a systematic review. Minerva Pediatr. 2017;69(04):348–367. doi: 10.23736/S0026-4946.17.04937-4. [DOI] [PubMed] [Google Scholar]
- 15.Guevara J P, Feudtner C, Romer D et al. Fragmented care for inner-city minority children with attention-deficit/hyperactivity disorder. Pediatrics. 2005;116(04):e512–e517. doi: 10.1542/peds.2005-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolraich M L, Bickman L, Lambert E W, Simmons T, Doffing M A. Intervening to improve communication between parents, teachers, and primary care providers of children with ADHD or at high risk for ADHD. J Atten Disord. 2005;9(01):354–368. doi: 10.1177/1087054705278834. [DOI] [PubMed] [Google Scholar]
- 17.Power T J, Blum N J, Guevara J P, Jones H A, Leslie L K. Coordinating mental health care across primary care and schools: ADHD as a case example. Adv Sch Ment Health Promot. 2013;6(01):68–80. doi: 10.1080/1754730X.2013.749089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinke W M, Stormont M, Herman K C, Puri R, Goel N. Supporting children's mental health in schools: teacher perceptions of needs, roles, and barriers. Sch Psychol Q. 2011;26(01):1–13. [Google Scholar]
- 19.Heuer B, Williams S. Collaboration between PNPs and school nurses: meeting the complex medical and academic needs of the child with ADHD. J Pediatr Health Care. 2016;30(01):88–93. doi: 10.1016/j.pedhc.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Corkum P, Bessey M, McGonnell M, Dorbeck A. Barriers to evidence-based treatment for children with attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord. 2015;7(01):49–74. doi: 10.1007/s12402-014-0152-z. [DOI] [PubMed] [Google Scholar]
- 21.Wolraich M L, Lambert W, Doffing M A, Bickman L, Simmons T, Worley K. Psychometric properties of the Vanderbilt ADHD diagnostic parent rating scale in a referred population. J Pediatr Psychol. 2003;28(08):559–567. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]
- 22.Chang L Y, Wang M Y, Tsai P S. Diagnostic accuracy of rating scales for attention-deficit/hyperactivity disorder: a meta-analysis. Pediatrics. 2016;137(03):e20152749. doi: 10.1542/peds.2015-2749. [DOI] [PubMed] [Google Scholar]
- 23.Brinkman W B, Epstein J N. Promoting productive interactions between parents and physicians in the treatment of children with attention-deficit/hyperactivity disorder. Expert Rev Neurother. 2011;11(04):579–588. doi: 10.1586/ern.10.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hart C N, Kelleher K J, Drotar D, Scholle S H. Parent-provider communication and parental satisfaction with care of children with psychosocial problems. Patient Educ Couns. 2007;68(02):179–185. doi: 10.1016/j.pec.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel A, Medhekar R, Ochoa-Perez M et al. Care provision and prescribing practices of physicians treating children and adolescents with ADHD. Psychiatr Serv. 2017;68(07):681–688. doi: 10.1176/appi.ps.201600130. [DOI] [PubMed] [Google Scholar]
- 26.Power T J, Michel J, Mayne Set al. Coordinating systems of care using health information technology: development of the ADHD care assistant Adv Sch Ment Health Promot 20169(3-4):201–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fiks A G, Grundmeier R W, Biggs L M, Localio A R, Alessandrini E A. Impact of clinical alerts within an electronic health record on routine childhood immunization in an urban pediatric population. Pediatrics. 2007;120(04):707–714. doi: 10.1542/peds.2007-0257. [DOI] [PubMed] [Google Scholar]
- 28.Fiks A G, Zhang P, Localio A R et al. Adoption of electronic medical record-based decision support for otitis media in children. Health Serv Res. 2015;50(02):489–513. doi: 10.1111/1475-6773.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tham E, Swietlik M, Deakyne S et al. Clinical decision support for a multicenter trial of pediatric head trauma: development, implementation, and lessons learned. Appl Clin Inform. 2016;7(02):534–542. doi: 10.4338/ACI-2015-10-CR-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Michel J, Utidjian L H, Karavite D et al. Rapid adjustment of clinical decision support in response to updated recommendations for palivizumab eligibility. Appl Clin Inform. 2017;8(02):581–592. [Google Scholar]
- 31.Fiks A G, Mayne S, Karavite D J, DeBartolo E, Grundmeier R W. A shared e-decision support portal for pediatric asthma. J Ambul Care Manage. 2014;37(02):120–126. doi: 10.1097/JAC.0000000000000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fiks A G, Mayne S L, Karavite D J et al. Parent-reported outcomes of a shared decision-making portal in asthma: a practice-based RCT. Pediatrics. 2015;135(04):e965–e973. doi: 10.1542/peds.2014-3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Epstein J N, Langberg J M, Lichtenstein P K, Kolb R, Simon J O. The myADHDportal.com Improvement Program: an innovative quality improvement intervention for improving the quality of ADHD care among community-based pediatricians. Clin Pract Pediatr Psychol. 2013;1(01):55–67. doi: 10.1037/cpp0000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Epstein J N, Langberg J M, Lichtenstein P K, Kolb R, Altaye M, Simon J O. Use of an Internet portal to improve community-based pediatric ADHD care: a cluster randomized trial. Pediatrics. 2011;128(05):e1201–e1208. doi: 10.1542/peds.2011-0872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epstein J N, Kelleher K J, Baum R et al. Impact of a web-portal intervention on community ADHD care and outcomes. Pediatrics. 2016;138(02):e20154240. doi: 10.1542/peds.2015-4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baum R A, Epstein J N, Kelleher K. Healthcare reform, quality, and technology: ADHD as a case study. Curr Psychiatry Rep. 2013;15(07):369. doi: 10.1007/s11920-013-0369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fiks A G, Mayne S L, Michel J J et al. Distance-learning, ADHD quality improvement in primary care: a cluster-randomized trial. J Dev Behav Pediatr. 2017;38(08):573–583. doi: 10.1097/DBP.0000000000000490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiks A G, Mayne S, Hughes C C et al. Development of an instrument to measure parents' preferences and goals for the treatment of attention deficit-hyperactivity disorder. Acad Pediatr. 2012;12(05):445–455. doi: 10.1016/j.acap.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cisco Registered Envelope Service.San Jose, CA: Cisco Systems, INC.2017 [Google Scholar]
- 40.Schatz N K, Fabiano G A, Cunningham C E et al. Systematic review of patients' and parents' preferences for ADHD treatment options and processes of care. Patient. 2015;8(06):483–497. doi: 10.1007/s40271-015-0112-5. [DOI] [PubMed] [Google Scholar]
- 41.Eiraldi R B, Mazzuca L B, Clarke A T, Power T J. Service utilization among ethnic minority children with ADHD: a model of help-seeking behavior. Adm Policy Ment Health. 2006;33(05):607–622. doi: 10.1007/s10488-006-0063-1. [DOI] [PubMed] [Google Scholar]
- 42.Bussing R, Zima B T, Gary F A, Garvan C W. Barriers to detection, help-seeking, and service use for children with ADHD symptoms. J Behav Health Serv Res. 2003;30(02):176–189. doi: 10.1007/BF02289806. [DOI] [PubMed] [Google Scholar]
- 43.Child Trends. Parental involvement in schools; 2013. Available at:https://www.childtrends.org/?indicators=parental-involvement-in-schools. Accessed November 29, 2018
- 44.Hill N, Taylor L. Parental school involvement and children's academic achievement: pragmatics and issues. Curr Dir Psychol Sci. 2004;13(04):161–164. [Google Scholar]
- 45.Gardner B, Phillips L A, Judah G. Habitual instigation and habitual execution: definition, measurement, and effects on behaviour frequency. Br J Health Psychol. 2016;21(03):613–630. doi: 10.1111/bjhp.12189. [DOI] [PubMed] [Google Scholar]
- 46.Schomaker J, Meeter M. Short- and long-lasting consequences of novelty, deviance and surprise on brain and cognition. Neurosci Biobehav Rev. 2015;55:268–279. doi: 10.1016/j.neubiorev.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 47.Kwahk K-Y, Ahn H, Ryu Y U. Understanding mandatory IS use behavior: how outcome expectations affect conative IS use. Int J Inf Manage. 2018;38(01):64–76. [Google Scholar]
- 48.Gulliver A, Griffiths K M, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10(01):113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rickwood D J, Deane F P, Wilson C J.When and how do young people seek professional help for mental health problems? Med J Aust 2007187(7, Suppl):S35–S39. [DOI] [PubMed] [Google Scholar]
- 50.Tao D, Xie L, Wang T, Wang T. A meta-analysis of the use of electronic reminders for patient adherence to medication in chronic disease care. J Telemed Telecare. 2015;21(01):3–13. doi: 10.1177/1357633X14541041. [DOI] [PubMed] [Google Scholar]
- 51.Coleman M T, Pasternak R H. Effective strategies for behavior change. Prim Care. 2012;39(02):281–305. doi: 10.1016/j.pop.2012.03.004. [DOI] [PubMed] [Google Scholar]


