Abstract
Purpose
To monitor the outcomes of surgical correction of esotropia in order to improve preoperative counselling for patients and their families.
Methods
A retrospective review audit of the medical charts at King Fahad Medical City. All patients treated surgically to correct esotropia, from January 2007 to December 2013. All operated cases were included regardless of age and esotropia etiology. The study used a goal-determined metric to assess the outcomes of strabismus surgery > 6 months post-operatively, and on last follow-up. The risk factors for poor surgical outcomes were identified using a Pareto chart.
Results
A total of 99 cases with sufficient documentation to determine the surgical goal were included in the analysis. The goal was to improve eye contact (cosmetic correction) in 77.8% cases, to establish binocularity in 15.2% cases, to resolve diplopia for 4% cases, and to improve anomalous head posture for 3%. The overall outcome was excellent for 70.7% at the first follow-up and for 57.6% at the final visit. Simultaneous vertical muscle surgery and/or superior oblique muscle palsy were risk factors for poor outcome (odds ratio 3.15, 95% CI 1.11–8.99).
Conclusions
Excellent outcome of esotropia surgery in this study is comparable to outcomes reported internationally using the goal determined metrics. Quality improvement processes like the Pareto chart are simple to use and helpful for determining the risk factors associated with poor surgical outcomes after esotropia correction from different etiology.
Keywords: Esotropia surgery, Strabismus outcome, Surgery goal, Audit
Introduction
Surgical correction of esotropia (ET) was pioneered at the end of the 18th century by Dieffenbach, who performed myotomy of the medial rectus.1 Subsequently, the surgical correction of ET evolved to include other procedures aimed at weakening the medial rectus and/or tightening the lateral rectus. In recent years, and as a part of the patient safety process, quality improvement initiatives have begun to include detailed preoperative discussions with patients and their family members that include the expected outcomes of the procedure, and long term stability of outcome. Surgical correction of ET has not been reported uniformly in the literature, which has made counselling prior to surgery an extremely complicated process due to the variability of ET etiology and patient age at the time of surgery.
Surgeries to correct ET are reported to have successful outcomes in 48.5–89.7% of cases globally.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 The large variability in success rates is due to differences in the post-operative angle from orthophoria used to assess outcome, the etiology of ET, the type of procedure, the length of post-operative follow-up, and other associated risk factors.
Surgical correction of ET is the most common strabismus surgery in the Kingdom of Saudi Arabia (KSA), comprising 3375 out of 4886 strabismus surgeries performed in a 14-year period at a single ophthalmology tertiary care institute in Riyadh.14 The outcomes of these surgeries were not reported. Indeed, the scarcity of published reports in the KSA makes it difficult to monitor surgical outcomes for strabismus surgery to aid in pre-operative counselling. One published study, from KSA, that reviewed all strabismus surgeries in adults performed between 2000 and 2007 at a single center found a success rate of 80% based on achieving a post-operative angle <20 prisms from orthophoria.15 Monitoring the outcome of health care delivery improves the decision making process for physicians, and patients who choose surgical correction, and it is important so that patients and their families can provide fully informed consent prior to a surgical procedure. Due to the unclear unified metrics used to audit the outcomes of strabismus surgery, consent is incomplete. There are currently just a few studies that can be used to inform patients’ about surgical outcome, but none from KSA.10, 12
This study reviewed the 6-month and long-term outcomes of ET surgery correction performed at a single center in the KSA and assessed the potential risk factors associated with poor outcome following the goal-determined metrics tool published in 2014.10
Patients and methods
A retrospective chart review was conducted in 2016 of ET cases operated on at “XXX” from January 2007 until December 2013. We reviewed both the primary outcome at the first post-operative visit, 6-month follow-up, and the final outcome at the last recorded visit. The inclusion criteria were all-etiology ET plus a minimum post-surgery follow-up of 6 months. Patients were included regardless of age. Patients with insufficient documentation to determine the goal of surgery or who had <6 months of post-operative follow-up were excluded from the study.
The study protocol followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board at XXX prior to the start of the chart review. A data collection sheet was created to record the information from the patients’ charts based on a form created in the goal-determined metrics study.10 The data sheet was modified to make it easier to fill in. The name of the surgeon was not included as a variable in this study, and no patient questionnaires were used in the audit. The data were entered into an Excel spreadsheet for analysis. We recorded patient demographic data at the initial assessment, ophthalmic findings at the last preoperative assessment, at the first post-operative assessment, and at the final follow-up assessment.
The data form was created to document the results of the sensorimotor examination (if this examination was performed) and the factors that seemed the most likely to influence the success of the surgery, based on the study by Ehrenberg.10 The goals of strabismus surgery include the following: (1) improve eye contact (cosmetic correction); (2) establish binocularity; (3) resolve diplopia in the primary position and the reading position; and (4) improve anomalous head posture (AHP). If the goal for surgery was not clearly stated in the patient notes, ‘cosmetic’ was used as the goal by the researchers if there was no diplopia and if AHP was not mentioned in the patient’s chart. If the surgery was performed when the patient was 3 years old or younger, binocular potential was used as a goal if no goal was recorded.
Age at surgery was included as a factor that might influence the success of the outcome. It was used as a continuous variable and also as a categorized variable by dichotomizing it to ≤60 months vs. >60 months. Other factors that were included were previous strabismus surgery, amblyopia, sex, and refraction status by calculating the spherical equivalent in diopters. The presenting ET angle was used as a continuous variable and was also dichotomized to ≥50 vs. <50 prism diopters (P.D.) as measured by the simultaneous prism and cover test or by the Krimsky test. A cerebral palsy (CP) diagnosis, delays in milestones, seizure disorders, having undergone surgery for brain tumor, or having central nervous system disease (CNSD) was combined as a risk factor called CP/CNSD. Premature birth and Down’s syndrome (if recorded in the chart) were combined as a single risk factor; similarly, 6th nerve palsy and Duane’s syndrome were combined as a risk factor as were superior oblique (SO) palsy and simultaneous vertical muscle surgery. Other diagnoses, like Brown syndrome, midface deformity, and syndromatic features, were combined together as one risk factor.
The goal-determined success criteria are shown in Table 1 as were proposed in the study by Ehrenberg et al.10 Patients who developed post-operative vertical deviation that was not present preoperatively were considered to have a poor outcome. Consecutive vertical deviation was added as an extra metric to assess the outcome of the surgery in our audit.
Table 1.
Goal determined outcomes criteria of esotropia surgery.10
| Goal | Outcome | Definition |
|---|---|---|
| Binocular potential | Excellent | Distance ET1 ≤ 10P.D.2 or XT3 ≤ 5P.D. Near No XT, any ET |
| Good | Distance ET ≤ 15P.D. or XT ≤ 10P.D. Near X(T) ≤10P.D. any ET |
|
| Poor | Distance ET > 15P.D. or XT > 10P.D. Unplanned reoperation (horizontal) or Developed post-operative vertical deviation |
|
| Cosmetic | Excellent | ≤10P.D. ET or ≤ 10P.D. XT |
| Good | ≤15P.D. ET or ≤ 15P.D. XT | |
| Poor | Unplanned reoperation (horizontal) Developed post-operative Vertical deviation |
|
| Torticollis | Excellent | Torticollis ≤ 8P.D. |
| Good | Torticollis > 8 to ≤ 12P.D. | |
| Poor | Planned reoperation for diplopia or torticollis or > 12 degrees Developed post-operative vertical deviation |
|
| Diplopia | Excellent | No diplopia in the primary position |
| Good | Diplopia controlled with prism ≤ 10P.D. in the primary position | |
| Poor | Unplanned reoperation for diplopia or diplopia not controlled with prism correction Developed post-operative vertical deviation |
|
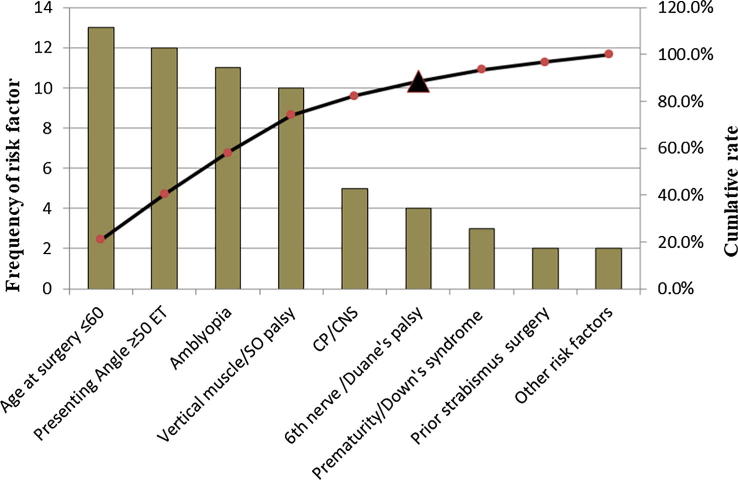
Since the study was performed as a clinical audit, the Pareto principle or the 80:20 principle (which states that 20% of the variables are responsible for 80% of the defects) was applied by creating a Pareto chart that identified the risk factors responsible for 80% of the poor surgical outcomes.16
Statistical analysis
Descriptive analyses of the demographic characteristics of the study cases were reported using medians with interquartile ranges (IQs) for continuous variables and proportions for categorical variables. Univariate analysis of risk factors was performed using a dichotomous outcome variable, poor vs. successful, with successful defined as either an excellent or good outcome. Differences in medians were analyzed using the Mann-Whitney U test for continuous variables and the chi-square test or Fisher’s exact test, as appropriate, for categorical variables. A logistic regression model was created that included risk factors for poor outcome that were identified in the Pareto chart. All analyses were performed using the StatsDirect software program, and the significance level was set as P ≤ 0.05.
Results
During the study period from January 2007 to December 2013, a total of 329 strabismus surgeries were performed at KFMC. Of these, 143 (43%) cases were performed to correct ET, and 111 cases (78%) had enough data in their electronic files to be included in the study. The final analysis included 99 cases, with 12/111 (10.8%) cases excluded because there was no post-surgical follow-up as the patients did not attend any appointments.
Out of the 99 cases included in our study, 77 (77.8%) were operated on to improve the cosmetic appearance; 15 (15.2%) to establish binocularity; 4 (4%) to resolve diplopia; and 3 (3%) to improve AHP. One or more risk factor was identified In 78 (78.8%) cases, with angle ≥ 50P.D. being the most common risk factor, recorded in 25 (25.3%) cases. The demographic data of the study cases and the outcomes according to the goal of surgery are shown in Table 2.
Table 2.
Characteristics of the study cohort according to the goal of surgery, and surgery outcome.
| Variable | Overall | Cosmetic | Binocular Potential | Diplopia | AHPa |
|---|---|---|---|---|---|
| N = 99 | N = 77 | N = 15 | N = 4 | N = 3 | |
| Age at presentation in years, median (IQR)b | 4 (1, 7) | 5 (2, 7) | 1 (<1, 1) | 14.5 (11, 24) | 6 (1, 18) |
| Age at the time of surgery in months, median (IQR) | 71 (46, 114) | 79 (55, 114) | 24 (18, 32) | 187.5 (146,303.5) | 83 (22, 226) |
| Length of follow-up post-surgery in months, median (IQR) | 39 (20, 61) | 40 (26, 61) | 39 (16, 65) | 12.5 (9.5,17.5) | 13 (11, 73) |
| Length of follow-up prior to surgery in months, median (IQR) | 12 (5, 24) | 14 (5, 29) | 12 (6, 12) | 7.5 (4, 11) | 1 (0, 1) |
| Spherical equivalent REc, median (IQR) | + 2.00 (+0.75, +3.25) | +2.00 (+1.00, +3.50) | +2.75 (+2.25, +3.50) | −0.75 (−8.50, +0.25) | −0.25 (−1.25, +1.00) |
| Angle of deviation in P.Dd., median (IQR) | 35 (25, 50) | 35 (25, 50) | 35 (30, 40) | 28 (23, 38) | 25 (20, 30) |
| Male sex, N (%) | 50 (50.5%) | 42 (54.6%) | 5 (33.3%) | 1 (25%) | 2 (66.7%) |
| Any risk factor, N (%) | 78 (78.8%) | 60 (77.9%) | 11 (73.3%) | 4 (100%) | 3 (100%) |
| Excellent outcome, N (%) | 59 (59.6%) | 45 (58.4%) | 11 (73.3%) | 3 (75%) | 0 (0%) |
| Good outcome, N (%) | 8 (8.1%) | 7 (9.1%) | 0% | 0% | 1 (33.3%) |
| Poor outcome, N (%) | 32 (32.3%) | 25 (32.5%) | 4 (26.7%) | 1 (25%) | 2 (66.7%) |
AHP = anomalous head poster.
IQR = interquartile range.
RE = right eye.
P.D. = prisms diopter.
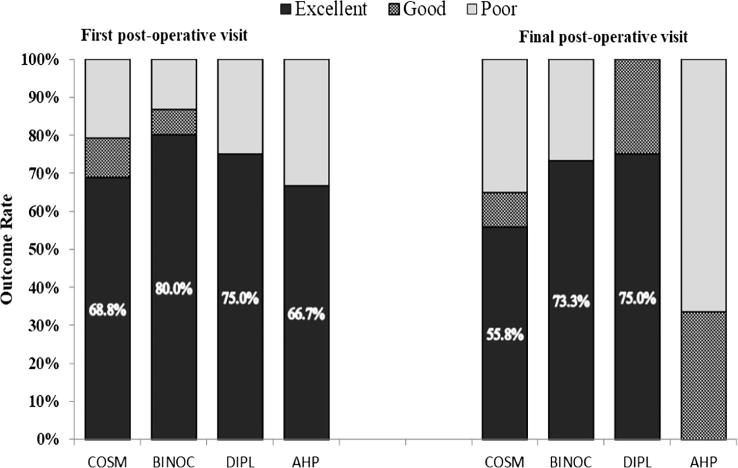
An overall excellent outcome was achieved in 70 (70.7%) cases at the first follow-up and in 57 (7.6%) cases at the final visit. Fig. 1 shows the distribution of outcomes according to the different surgery goals at the first postoperative visit and at the final visit. Reoperation was performed in 10 (10.1%) cases: 6 cases in the cosmetic group, 1 in the binocular potential group, 1 in the diplopia group, and 2 in the AHP group. The second surgery was performed to correct residual ET in 5 cases, consecutive XT in 3 cases, and consecutive vertical deviation in 2 cases. The choice to undergo surgery and the degree of correction was not studied in this audit, but the most common procedure was bimedial rectus recession (BMR) in 55 of 99 cases (55.6%), followed by BMR with simultaneous inferior oblique surgery in 12 of 99 cases (12.1%).
Fig. 1.
Outcomes of surgical correction of esotropia according to the goal of surgery, at the first and final post-operative visits. AHP, improve anomalous head posture; BINOC, binocular potential goal; COSM, cosmetic goal; DIPL = resolve diplopia goal.
For the dichotomized outcome variable, 33 of 99 cases (33.3%) had poor outcomes and 66 of 99 cases (66.7%) had successful outcomes at the final post-operative visit. We found that 78 of 99 cases (78.8%) had at least one risk factor, including 26 cases with a poor outcome and 52 with a successful outcome; there was no significant difference between the two groups in terms of the rate of any of the risk factors (P > 0.9999).
The Mann-Whitney U test showed that the median age at presentation at the ophthalmology clinic was similar in both groups 65 months in the poor outcome group vs. 45 months in the successful outcome group (two-sided P = 0.61). The median age at surgery was similar for both groups, 79 months in the poor outcome group vs. 69 months in the successful outcome group (two-sided P = 0.84). The spherical equivalent (SE) in both eyes was similar: SE in the right eye was + 2.00 diopters (IQR + 0.75, +3.25), and SE in the left eye was + 2.50 (IQR + 0.75, +3.50) (two-sided P = 0.47). Using the right eye SE for the univariate analysis of refractive status as a risk factor showed similar medians in the poor outcome group (+1.25) vs. the successful outcome group (+2.00) (two-sided P = 0.41). There was no difference in the median preoperative angle in the poor vs. successful outcome groups (40 vs. 35P.D.; two-sided P = 0.15).
Table 3 shows the categorized risk factors according to surgery goal, and Table 4 shows the univariate analysis in which the chi-square test was used to compare poor vs. successful outcomes. The only risk factor that was found to be significant was simultaneous vertical muscle surgery/SO palsy (P = 0.027). Sex was not found to be a risk factor for poor outcome, with 18/33 males in the poor outcome group vs. 32/66 males in the successful outcome group (two-sided P = 0.57).
Table 3.
Descriptive analysis of risk factors by the goal of surgery.
| Risk factor N (%) | Overall N = 99 |
Cosmetic N = 77 |
Binocular potential N = 15 |
Diplopia N = 4 |
AHPa N = 3 |
|---|---|---|---|---|---|
| ≥50P.D.b | 25 (25.3%) | 22 (28.6%) | 3 (20.0%) | 0 (0%) | 0 (0%) |
| Simultaneous vertical muscle surgery/SOc | 19 (19.2%) | 15 (19.5%) | 3 (20.0%) | 0 (0%) | 1 (33.3%) |
| CP/CNSDd | 21 (21.2%) | 15 (19.5%) | 3 (20.0%) | 3 (75.0%) | 0 (0%) |
| Prematurity/Down's syndrome | 15 (15.2%) | 11 (14.3%) | 4 (26.7%) | 0 (0%) | 0 (0%) |
| Prior squint surgery | 4 (4.0%) | 4 (5.2%) | 0 (0%) | 0 (0)% | 0 (0) % |
| Sixth nerve/Duane's Palsy | 10 (10.1%) | 5 (6.5%) | 2 (13.3%) | 1 (25.0%) | 2 (66.7%) |
| Othere | 10 (10.1%) | 8 (10.4%) | 1 (6.7%) | 1 (25.0%) | 0 (0%) |
| Amblyopia | 44 (44.4%) | 38 (49.4%) | 5 (33.3%) | 0 (0%) | 1 (33.3%) |
AHP = anomalous head posture.
P.D. = prism diopter.
SO = superior oblique palsy.
CP = cerebral palsy/CNSD = central nervous system tumors or surgery, seizure disorder, delayed milestones.
Other = Brown’s syndrome, midface deformity, syndromatic features.
Table 4.
Univariate analysis of risk factors using the chi-square/Fisher’s exact test.
| Risk factor N (%) | Overall N = 99 |
Poor outcome N = 33 (33.3%) |
Successful outcome N = 66 (66.7%) |
P value |
|---|---|---|---|---|
| Amblyopia | ||||
| Yes | 44 | 11 (33.3%) | 33 (50.0%) | 0.12 |
| No | 55 | 22 (66.7%) | 33 (50.0%) | |
| Presenting angle ≥ 50P.D.aET | ||||
| Yes | 26 | 12 (36.4%) | 14 (21.2%) | 0.11 |
| No | 73 | 21 (63.6%) | 52 (78.8%) | |
| CP/CNSDb | ||||
| Yes | 22 | 5 (15.2%) | 17 (25.8%) | 0.23 |
| No | 77 | 28 (84.8%) | 49 (74.2%) | |
| Prematurity/Down’s syndrome | ||||
| Yes | 15 | 3 (9.1%) | 12 (18.2%) | 0.23 |
| No | 84 | 30 (90.9%) | 54 (81.8%) | |
| Age category | ||||
| ≤60 | 41 | 13 (39.4%) | 28 (42.4%) | 0.77 |
| >60 | 58 | 20 (60.6%) | 38 (57.6%) | |
| Simultaneous vertical muscle surgery/SOc | ||||
| Yes | 18 | 10 (30.3%) | 8 (12.1%) | 0.027 |
| No | 81 | 23 (69.7%) | 58 (87.9%) | |
| Sixth nerve/Duane's Palsy | ||||
| Yes | 10 | 4 (12.1%) | 6 (9.1%) | 0.64* |
| No | 89 | 29 (87.9%) | 60 (90.9%) | |
| Prior strabismus surgery | ||||
| Yes | 4 | 2 (6.1%) | 2 (3.0%) | 0.51* |
| No | 95 | 31 (93.1%) | 64 (97.0%) | |
| Otherd | ||||
| Yes | 10 | 2 (6.1%) | 8 (12.1%) | 0.38* |
| No | 89 | 31 (93.9%) | 58 (87.9%) | |
P.D = prism diopter.
CP = cerebral palsy/CNSD = central nervous system tumors or surgery, seizure disorder, delayed milestones.
SO = superior oblique palsy.
Other = Brown’s syndrome, midface deformity, syndromatic features.
Fisher’s exact test.
The multivariate analysis model included the risk factors identified by the Pareto chart (Fig. 2) and showed that only simultaneous vertical muscle surgery/SO palsy was significantly associated with poor outcome of surgery (odds ratio = 3.15, 95% CI 1.11–8.99).
Fig. 2.
Pareto chart showing the potential risk factors for poor surgical outcome. The risk factors to the right of the triangle were included in the logistic regression model. ET, esotropia; Other, Brown’s syndrome, midface deformity, or syndromatic features; SO, superior oblique palsy.
No complications were reported intraoperatively in this study. One case developed transient ptosis after the Botox injection but recovered within 10 days, but there were no other post-operative complications.
Discussion
This surgical outcome audit was performed to investigate outcomes for an ophthalmic procedure that is frequently performed in strabismus unit. To our knowledge, no other similar studies have been conducted in the KSA, so our findings will help improve preoperative counseling for patients considering surgical treatment of ET. The ET rates in the KSA have been reported in a few hospital-based studies to be between 36.9% and 38%, but no population studies have assessed the burden of the disease or reported the number of ET cases requiring surgeries.17, 18
The overall excellent outcome rate (Table 1) was 70.7% at the first post-operative visit but dropped to 57.6% at the final assessment which points to unstable favorable outcome. This audit looked at >12 risk factors that were previously reported to be associated with poor outcome, but only having a simultaneous vertical muscle surgery and/or SO palsy influenced the final outcome.
In the cosmetic goal group, an excellent outcome was found in 68.8% at the first post-operative visit but dropped to 58.4% at the last visit, while a poor outcome was found in 20.8% at the first visit and increased to 32.5% at the last visit. These findings are generally similar to those in other studies.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 The reoperation rate was 10.1%, which is within the range of rates reported internationally (6–23.8%) in studies of patients with variable etiology of ET and of different ages.2, 4, 7, 8, 9 We still do not have any data concerning the long-term (≥10-year) follow-up outcomes in the KSA, in this study 75% of cases were followed for ≥5 years. One population study reported that 1 out of 2 operated cases required a second procedure during a 10-year follow-up period.13 Thus, the long-term expectations for surgical correction need to be clarified at KSA to clarify the stability of surgical outcome.
Outcome audits for any surgical procedures help improve quality of care, aid in case selection, help clarify and manage the expectations of patients and their families prior to the provision of informed consent. Correction of ET is a common procedure and mostly involves young patients with a long life expectancy. It is imperative that centers that perform ET correction surgeries also perform audits of the outcomes of surgery in order to maintain optimal quality of care. The findings of our audit may not be generalizable to other centers, depending on the etiology of ET and the age group treated, but a general comparison can be made using similar goal-determined metrics as an audit tool.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Remy C., Aracil P. History of strabismus surgery. J Fr Ophtalmol. 1984;7:493–498. [PubMed] [Google Scholar]
- 2.Kim E., Choi D.G. Outcomes after the surgery for acquired nonaccommodative esotropia. BMC Ophthalmol. 2017;17:130–135. doi: 10.1186/s12886-017-0527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumari N., Amitava A.K., Ashraf M., Grover S., Khan A., Sonwani P. Prognostic preoperative factors for successful outcome of surgery in horizontal strabismus. Oman J Ophthalmol. 2017;10:76–80. doi: 10.4103/ojo.OJO_133_2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grace S.F., Cavuoto K.M., Shi W., Capo H. Surgical treatment of adult-onset esotropia = characteristics and outcomes. J Pediatr Ophthalmol Strabismus. 2017;54:104–111. doi: 10.3928/01913913-20160929-02. [DOI] [PubMed] [Google Scholar]
- 5.Kiziltunc P.B., Atilla H., Çalış F., Alay C. Comparison of surgical success for infantile esotropia and strabismus associated with neurological impairment. Strabismus. 2016;24:97–100. doi: 10.1080/09273972.2016.1210173. [DOI] [PubMed] [Google Scholar]
- 6.Magli A., Rombetto L., Matarazzo F., Carelli R. Infantile esotropia risk factors associated with reoperation. Clin Ophthalmol. 2016;10:2079–2083. doi: 10.2147/OPTH.S116103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zehavi-Dorin T., Ben-Zion I., Mezer E., Wygnanski-Jaffe T. Long-term results of bilateral medial rectus nuscle recession in children with developmental delay. Strabismus. 2016;24:7–11. doi: 10.3109/09273972.2015.1130064. [DOI] [PubMed] [Google Scholar]
- 8.Bayramlar H., Karadag R., Yildirim A., Öçal A., Sari Ü. Medium-term outcomes of three horizontal muscle surgery in large-angle infantile esotropia. J Pediatr Ophthalmol Strabismus. 2014;51:160–164. doi: 10.3928/01913913-20140318-02. [DOI] [PubMed] [Google Scholar]
- 9.Magli A., Carelli R., Matarazzo F., Bruzzese D. Essential infantile esotropia: postoperative motor outcomes and inferential analysis of strabismus surgery. BMC Ophthalmol. 2014;14–35 doi: 10.1186/1471-2415-14-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ehrenberg M., Nihalani B.R., Melvin P., Cain C.E., Hunter D.G., Dagi L.R. Goal-determined metrics to assess outcomes of esotropia surgery. J AAPOS. 2014;211–216 doi: 10.1016/j.jaapos.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 11.Astudillo P., Cotesta M., Scholfield J., Kraft S., Mireskandari K. The effect of achieving immediate target angle on success of strabismus surgery in children. Am J Ophthalmol. 2015;160:913–918. doi: 10.1016/j.ajo.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 12.Gogate P.M., Rishikeshi N., Taras S., Aghor M., Deshpande M.D. Clinical audit of horizontal strabismus surgery in children in aharashtra, India. Strabismus. 2010;18:13–17. doi: 10.3109/09273970903567618. [DOI] [PubMed] [Google Scholar]
- 13.Louwagie C.R., Diehl N.N., Greenberg A.E., Mohney B.G. Long-term follow-up of congenital esotropia in a population-based cohort. J AAPOS. 2009;13:8–12. doi: 10.1016/j.jaapos.2008.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Curtis T.H., McClatchey M., Wheeler D.T. Epidemiology of surgical strabismus in Saudi Arabia. Ophthalmic Epidemiol. 2010;17:307–314. doi: 10.3109/09286586.2010.508351. [DOI] [PubMed] [Google Scholar]
- 15.Al-Wadaani F. Outcome of strabismus surgery by nonadjustable suture among adults attending a university hospital of Saudi Arabia. Niger J Clin Pract. 2017;20:335–340. doi: 10.4103/1119-3077.196086. [DOI] [PubMed] [Google Scholar]
- 16.Wensing P.M., Thomson R.G. Modern measurement for a modern health service. Qual Health Care. 2000;9:199–200. doi: 10.1136/qhc.9.4.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Darraj A., Barakat W., Kenani M. Common eye diseases in children in Saudi Arabia (Jazan) Ophthal Eye Dis. 2016;8:33–39. doi: 10.4137/OED.S39055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Tamimi E.R., Shakeel A., Yassin S.A., Ali S.I., Khan U.A. A clinic based study of refractive errors, strabismus, and amblyopia in pediatric age group. J Fam Community Med. 2015;22:158–162. doi: 10.4103/2230-8229.163031. [DOI] [PMC free article] [PubMed] [Google Scholar]