Abstract
Background/Objective: Recent interventions aim to heighten informal caregivers’ empathy levels assuming that this will lead to better well-being. However, previous studies have explored linear associations between empathy and aspects of well-being and yielded mixed results. We hypothesized that quadratic models may be more fitting to describe these relationships. Method: A cross-sectional study, with two groups (201 informal caregivers, and 187 non-caregivers) was conducted. Participants completed questionnaires on cognitive and affective empathy, and depression, anxiety, and caregiver burden. AN(C)OVA's and multiple hierarchical regression analyses including linear and quadratic terms were used to analyze the data. Results: For caregivers, there was a negative quadratic relationship between depression and cognitive empathy, and a positive linear relationship between anxiety and affective empathy, irrespective of sociodemographic characteristics. For non-caregivers, there were positive quadratic relationships between depression and cognitive and affective empathy, and between anxiety and affective empathy. The empathy levels did not differ between the groups. Conclusions: While caregivers and non-caregivers had the same amount of empathy, the relationships between empathy and depression and anxiety differed between the groups. Interventions for informal caregivers could aim to heighten cognitive empathy and to lower affective empathy to diminish depression and anxiety symptoms.
Keywords: Dementia, Depression, Empathy, Informal caregivers, Cross sectional study.
Resumen
Antecedentes/Objetivo: Intervenciones recientes tienen como objetivo aumentar los niveles de empatía de cuidadores informales suponiendo que ello mejorará el bienestar. Estudios previos que han explorado las asociaciones lineales entre empatía y bienestar mostraron resultados inconsistentes. Presumimos que los modelos cuadráticos pueden ser más adecuados para describir estas relaciones. Método: Se realizó un estudio transversal con dos grupos (201 cuidadores informales y 187 no cuidadores). Completaron cuestionarios sobre empatía cognitiva y afectiva, depresión, ansiedad y carga del cuidador. Se emplearon AN(C)OVA y análisis de regresión jerárquica múltiple incluyendo términos lineales y cuadráticos. Resultados: En los cuidadores se obtuvo una relación cuadrática negativa entre depresión y empatía cognitiva, y una relación lineal positiva entre ansiedad y empatía afectiva, independientemente de las características sociodemográficas. En los no cuidadores hubo relaciones cuadráticas positivas entre depresión y empatía cognitiva y afectiva, y entre ansiedad y empatía afectiva. Los niveles de empatía no difirieron entre ambos grupos. Conclusiones: Mientras ambos grupos tenían la misma cantidad de empatía, las relaciones de empatía con depresión y ansiedad difirieron entre ellos. Las intervenciones para cuidadores informales podrían apuntar a aumentar la empatía cognitiva y reducir la empatía afectiva para disminuir la depresión y los síntomas de ansiedad.
Palabras clave: Demencia, depresión, empatía, cuidadores informales, estudio transversal
The prevalence of dementia is rising, with an estimated number of 131.5 million people living with dementia in 2050 worldwide (Prince et al., 2015). Most people with dementia live at home where they are dependent on informal, or family, caregivers for their daily care. Informal caregivers are mostly spouses or children of the person with dementia, who do not get paid for caregiving. Informal caregivers can experience negative consequences of caregiving, with depression (Schoenmakers, Buntinx, & Delepeleire, 2010), anxiety, and caregiver burden as the most prevalent problems (Joling et al., 2015, Kasuya et al., 2000, Mahoney et al., 2005). Especially female (Mahoney et al., 2005, Schoenmakers et al., 2010), spousal caregivers (Joling et al., 2015, Meshefedjian et al., 1998, Schoenmakers et al., 2010), who have a low level of education (Chiao, Wu, & Hsiao, 2015) appear to be at risk for these negative consequences. Many interventions for informal caregivers have been developed to diminish these negative consequences, most of which are moderately effective (Jensen, Agbata, Canavan, & McCarthy, 2015). Recent research is beginning to focus on heightening informal caregivers’ empathy in an attempt to diminish caregiver depression, anxiety, and burden, and thereby enhance the lives of both the caregivers and the care receivers (Hattink et al., 2015, Jütten et al., 2017, Wijma et al., 2017).
Empathy is currently defined as a complex bio-psycho-social concept made up of at least two components (Baron-Cohen and Wheelwright, 2004, Decety and Jackson, 2004). These include a cognitive component: knowing or understanding what another person is feeling, or the ability to understand another persons’ perspective, sometimes referred to as Theory of Mind; and an affective or emotional component: feeling what another person feels, sometimes referred to as sympathy; sharing or feeling another person's emotional state. These two constructs are associated with largely separate neural systems. Cognitive empathy has been associated with higher order functioning attributed to the medial and dorsolateral regions of the prefrontal cortex (Shamay-Tsoory, 2011), whereas affective empathy has been linked to activation of both subcortical (e.g., amygdala, hypothalamus, and hippocampus) and cortical (e.g., anterior insula) structures (Decety, Michalska, & Kinzler, 2011). These conceptual and neurobiological distinctions highlight the importance of investigating the effects of affective and cognitive empathy separately, which is not always done by previous research.
Empathy is often regarded as an important quality ‘good’ doctors have and fundamental to good patient-clinician relationships. A review (Derksen, Bensing, & Lagro-Janssen, 2013) found that patients of empathic physicians had better health outcomes, lower levels of anxiety, and were more satisfied with the care they received. In addition, more empathy has been found to predict higher quality of care for the person with dementia (Panyavin et al., 2015). Because of these positive outcomes for patients, interventions aimed at professionals teaching them how to be empathic have been designed (Batt-Rawden, Chisolm, Anton, & Flickinger, 2013). Following these developments, interventions for informal caregivers are beginning to focus on heightening the caregiver's empathy, because it is believed that this could result in better well-being for the caregiver and subsequently better care for the person with dementia (Hattink et al., 2015, Jütten et al., 2017, Wijma et al., 2017). However, the influence of empathy on the empathizer's lives, especially for informal caregivers, is yet unclear and has only been examined in a few studies. More studies in this field have focused on the link between empathy and aspects of well-being (mostly anxiety) in the general population, while others have examined the link between empathy and burnout in healthcare professionals. Burnout encompasses symptoms caused by (work-related) stress, such as exhaustion, depersonalization, and reduced personal accomplishment (Schaufeli, Maslach, & Marek, 1993), and has been related to aspects of caregiver burden. The effects of empathy on these outcomes are not always positive for the empathizer.
In the general population, a cross-sectional study with parent-adolescent dyads found that parental empathy was associated with greater parental self-esteem, and purpose in life, but also with higher systematic inflammation (Manczak, DeLongis, & Chen, 2016). In addition, an experimental study found that participants with high trait empathy who had been instructed to actively appraise the thoughts and feelings of another distressed individual, more effectively learned to fear a neutral stimulus, than those who had not been instructed to do so (Olsson et al., 2016). Shu, Hassell, Weber, Ochsner, and Mobbs (2017) found a causal role for state empathy in the experience of vicarious anxiety: taking an empathic perspective increased the perception of vicarious anxiety and sustained effects of anxiety such as risk aversion and sleep disruption. For healthcare professionals, a recent review (Wilkinson, Whittington, Perry, & Eames, 2017), found evidence for both positive (more empathy–more burnout symptoms), and negative relationships (more empathy - fewer burnout symptoms). Lamothe, Boujut, Zenasni, and Sultan, 2014 found, in a cross-sectional survey-study among 296 general practitioners, that the combination of higher affective empathy and higher cognitive empathy predicted a lower proportion of burnout. On the other hand, they also found that general practitioners who had high levels of affective empathy, in combination with low levels of cognitive empathy, were at greater risk of burnout. A cross-sectional study among >1000 medical students (Thomas et al., 2007), found aspects of burnout to be inversely correlated with both cognitive and affective empathy. They also found that a higher quality of life and fewer depression symptoms were associated with more affective empathy.
For informal dementia caregivers, only three studies have examined the association between empathy and aspects of well-being (Lee et al., 2001, Shim et al., 2012, Sutter et al., 2014). Shim et al. (2012) conducted a qualitative study, among 57 spousal dementia caregivers. They found that caregivers with higher empathy levels were more positive, more acceptant of their loved one's changes, had a better relationship with the care receiver, and described caregiving as something satisfactory and meaningful to them; while those with lower empathy levels took a more negative stance to caregiving. Sutter et al. (2014) found, in a cross-sectional study among 90 informal dementia caregivers, that more empathy was significantly correlated with less depression, burden, and stress. However, in regression analyses, only stress was significantly predicted by empathy after controlling for sociodemographic variables. Lee et al. (2001) conducted a cross-sectional study among 140 informal dementia caregivers. In univariate analyses, they found that more cognitive empathy was significantly correlated with lower stress appraisal, lower threat appraisal, fewer depression symptoms, and more life satisfaction. On the other hand, affective empathy was found to be significantly correlated with higher stress appraisal. In multivariate linear regression analyses, they found that only life satisfaction was significantly predicted by less affective empathy they after controlling for caregiver age, sex, and spousal status. They found no predictive ability for neither affective nor cognitive empathy for depression.
Overall, it is not yet clear how empathy is related to aspects of well-being. All of the above-described studies have examined linear relationships between empathy and the empathizers’ well-being, meaning that the authors assumed that more (or less) empathy was systematically related to more (or less) anxiety/depression. However, since there is evidence for both a positive and a negative relationship, we hypothesized that quadratic models may be more appropriate to explain the relationships. We hypothesized that there exist quadratic, u-shape, relationships between empathy, and depression, anxiety, and burden. More specifically, that there exist ‘optimal’ levels of empathy, whereas too little or too much empathy may be detrimental. The theory behind this is that too much empathy, and taking on another person's feelings (affective empathy), and mentally replace oneself into the other person's shoes (cognitive empathy), can hypothetically cause people to take on another person's burden, and cause them to lose the ability to know or prioritize what they want or need themselves. Too little empathy, on the other hand, may be associated with a poorer understanding of the person with dementia. This may cause failure to recognize dementia symptoms as part of dementia instead of intentional acts of the person with dementia. We hypothesized that this may cause more arguments between caregiver and care receiver, and in turn more depression symptoms. If it is known how empathy relates to depression, anxiety, and burden in informal caregivers, it could be determined if interventions should focus on heightening or reducing (cognitive and/or affective) empathy to ultimately enhance the lives of both caregivers and the people with dementia. The primary aim of this study was to examine how empathy, depression, anxiety, and burden related to each other in informal caregivers. To be able to compare our findings to the general population, we also examined these relationships for non-caregivers. In addition, we examined if empathy levels (both affective and cognitive) differed between informal dementia caregivers and non-caregivers.
Method
Participants
There were two groups: (1) 201 adult (18+) informal caregivers who spent at least 8 hours per week on care for a relative, spouse, or friend with dementia who lived at home (not institutionalized and not prohibited from ‘normal’ care). This group was recruited for the longitudinal Into D’mentia study, of which the protocol can be found here (Jütten et al., 2017), describing the methods and procedure in greater detail. The second group consisted of 187 control group participants, comprising adults (18+) who did not provide care for a loved one with an illness. This group was recruited via (social) media, and both private and professional networks of the authors.
Procedure
All participants completed a semi-structured interview (containing questions about sociodemographic-, and dementia-related variables for the caregivers) and a questionnaire booklet. The interviews took place either at Tilburg University or at the participants’ homes; depending on their preference. Written informed consent was obtained and the study protocol has been approved by the local ethics committees.
Measures
Two subscales from the Interpersonal Reactivity Index (IRI; Davis, 1980) were used to measure empathy; Perspective Taking (PT) and Empathic Concern (EC). PT measures cognitive empathy, the tendency to take the psychological point of view of others (Cronbach's α = .67, λ-2 = .68). EC measures affective empathy, the ability to feel for others (Cronbach's α = .57, λ-2 = .58). Both subscales consist of 7 items, each rated on a 5-point Likert scale (0-4), with a maximum score of 28 per subscale (Davis, 1983).
Depression and anxiety were measured using the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983). The HADS is a self-report questionnaire consisting of 14 items; 7 for both depression (Cronbach's α = .78, λ-2 = .79) and anxiety (Cronbach's α = .81, λ-2 = .82). The responses are based on the relative frequency of symptoms over the past week, using a 4-point Likert scale ranging from 0 (not at all) to 3 (very often). The maximum score for both scales is 21; higher scores indicate more depression/anxiety symptoms.
Caregiver burden was assessed using the Caregiver Reaction Assessment–Dutch (CRA-D) (Nijboer, Triemstra, Tempelaar, Sanderman, & Van Den Bos, 1999), a self-report measure which includes the aspects self-esteem, financial problems, impact of caregiving on disrupted schedule, family support, and health problems. The subject reports to what extent he or she agrees with the statements on a 5-point scale (1-5). The scores were summed to one total score, with higher scores indicating more burden (maximum total score = 120, Cronbach's α = .87, λ-2 = .89). This questionnaire was completed by the informal caregiver group only because the questions are not applicable to non-caregivers.
The sociodemographic, control, variables were age (in years), sex (male/female), and level of education according to Verhage (recoded into low, medium, and high) (Verhage, 1964). For the caregivers, the type of relationship with the person with dementia (spouse/child/other), the time since diagnosis of the care receiver (in years), and the time providing care a week (in hours) were also examined.
Statistical analysis
Statistical analyses were performed using SPSS Statistics version 22 (SPSS Inc., 2013). Independent samples t-tests and χ2 tests were used to compare the groups on the sociodemographic variables age, sex, and educational level. To test if there were linear or quadratic relationships between empathy (PT and EC separately) and depression/anxiety/burden for the informal caregivers, 6 multiple hierarchical regression analyses were executed, each consisting of 3 blocks. Block 1 consisted of the (control) sociodemographic variables, Block 2 consisted of one empathy measure (PT or EC), and Block 3 consisted of the accompanying squared empathy measure (Keith, 2014). The continuous predictors (PT and EC) were group-centered. Within the blocks, the forced entry method was used to reduce the influence of random variation in the data and increase the replicability of the results (Field, 2009). For the non-caregivers, these analyses were repeated for the dependent variables depression and anxiety. The comparative analyses between the groups on the dependent variables PT, EC, depression, and anxiety were conducted using AN(C)OVA's. Because females generally score higher on empathy questionnaires (Eisenberg & Lennon, 1983), sex was added as a covariate in the ANCOVA's on PT and EC. A p-value of < .05 was considered statistically significant.
Results
The caregiver group (n = 201) had a mean age of 60.8 (SD = 12.03), and the control group (n = 187) had a mean age of 58.6 (SD = 13.4). Most participants were female (79% of the caregivers, and 71% of the non-caregivers), and most attained a high level of education (49% of the caregivers and 50% of the non-caregivers). Most caregivers cared for their spouse (41%) or their parent (45%), and 40% lived with the person with dementia. As shown in Table 1, the groups were matched on age, the proportion male/female participants, and the level of education.
Table 1.
Sociodemographic characteristics of the groups.
| Informal caregivers (n = 201) | Control group(n = 187) | Test-valuea | p-value | ||
|---|---|---|---|---|---|
| Age, M ± SD | 60.8 ± 12.03 | 58.6 ± 13.4 | 1.67 | .095 | |
| Sex, n, %male | 43, 21% | 55, 29% | 3.30 | .069 | |
| Level of educationb | n, %low | 30, 15% | 31, 16% | 0.29 | .860 |
| n, %middle | 72, 36% | 63, 34% | |||
| n, %high | 99, 49% | 93, 50% | |||
| Relationship with care receiver | n, %spouse | 82, 41% | – | – | – |
| n, %child | 90, 45% | ||||
| n, %other | 28, 14% | ||||
| Cohabiting with care receiver, n, %yes | 78, 40% | – | – | – | |
| Hours spent on care a week, M ± SD | 56.0 ± 63.1 | – | – | – | |
| Years since dementia diagnosis person with dementia, M ± SD | 3.1 ± 2.5 | – | – | – | |
Note. atest value: for continuous variables, t-values, for categorical variables X2 values; blevel of education according to Verhage (recoded into low, medium and high) (Verhage, 1964).
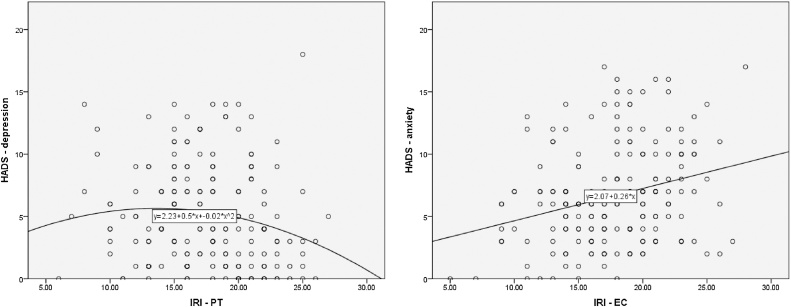
Table 2 shows the relationships between PT, EC, and depression, anxiety, and burden in informal caregivers. Depression was found to have a significant (negative) quadratic relationship with PT (β = −.14, p = .042), with the highest level of PT predicting the lowest level of depression. Anxiety was found to have a significant linear positive relationship with EC (β = .30, p < .001): higher levels of EC were related to more anxiety symptoms, see Figure 1. Neither PT nor EC significantly predicted caregiver burden.
Table 2.
Relationship between depression, anxiety, burden and empathy in informal caregivers.
| Depression |
Anxiety |
Burden |
||||
|---|---|---|---|---|---|---|
| ΔR2 | β | ΔR2 | β | ΔR2 | β | |
| Model 1. Perspective Taking | ||||||
| Block 1. Control variables | .169*** | – | .098* | – | .198*** | – |
| Block 2. PT | .001 | −.03 | .001 | .04 | .000 | .02 |
| Block 3. PT2 | .021* | −.14 | .007 | −.08 | .000 | .01 |
| Total R2 | .191*** | .106* | .199*** | |||
| Model 2. Empathic Concern | ||||||
| Block 1. Control variables | .161*** | – | .100* | – | .192*** | – |
| Block 2. EC | .017 | .13 | .087*** | .30 | .005 | .07 |
| Block 3. EC2 | .004 | −.06 | .002 | −.04 | .009 | −.09 |
| Total R2 | .183*** | .189*** | .206*** | |||
Note. Control variables included age, sex, level of education (low, high), type of relationship with care receiver (spouse, child), hours spent on care a week, and time since dementia diagnosis of the person with dementia. *p < .05, ***p < .001.
Figure 1.
The relationship between depression and PT, and anxiety and EC, in informal caregivers.
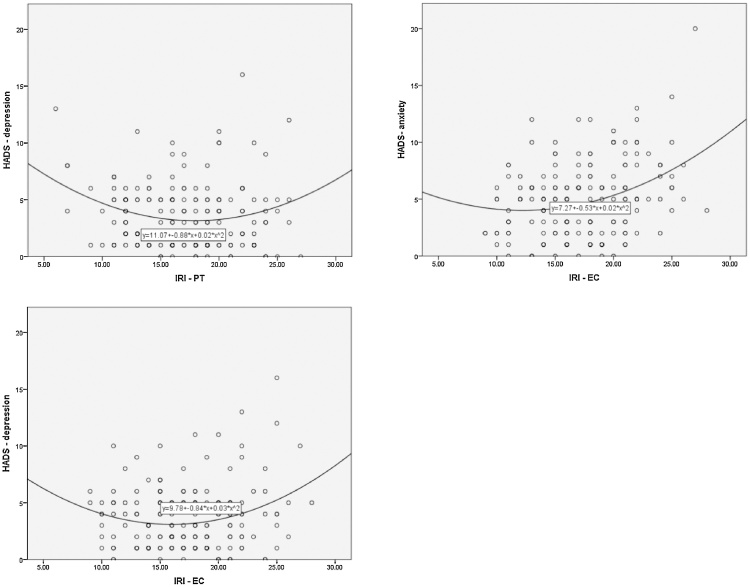
Table 3 and Figure 2 show the relationship between empathy and anxiety and depression for non-caregivers. There were significant positive quadratic relationships between depression and PT (β = .19, p = .010), depression and EC (β = .19, p = .009), and anxiety and EC (β = .04, p = .048). A positive quadrative relationship indicates that too much or too little empathy is associated with more depression or anxiety, whereas a ‘moderate’ level of empathy is associated with the least depression or anxiety symptoms.
Table 3.
Relationship beteween depression, anxiety, and empathy in non-caregivers.
| Depression |
Anxiety |
|||
|---|---|---|---|---|
| ΔR2 | β | ΔR2 | β | |
| Model 1. Perspective Taking | ||||
| Block 1. Control variables | .040 | – | .057* | – |
| Block 2. PT | .004 | −.06 | .001 | .03 |
| Block 3. PT2 | .036*** | .19* | .013 | −.11 |
| Total R2 | .080* | .071* | ||
| Model 2. Empathic Concern | ||||
| Block 1. Control variables | .047 | – | .053 | – |
| Block 2. EC | .013 | .12 | .071* | .28*** |
| Block 3. EC2 | .037* | .19* | .020* | .04* |
| Total R2 | .098* | .143* | ||
Note. Control variables included age, sex, and level of education (low, high). *p < .05, ***p < .001.
Figure 2.
The relationship between depression and PT and EC, and anxiety and EC, in non-caregivers.
Table 4 shows the comparative analyses between the groups. The groups did not differ significantly on PT or EC. Females had higher scores on both PT and EC than males (M = 17.6, SD = 4.3 versus M = 16.5, SD = 3.7, F = 4.64, p = .032, and M = 18.1, SD = 4.2 versus M = 16.1, SD = 3.9, F = 15.29, p < .001, for PT and EC respectively). The informal caregivers experienced significantly more depression (M = 5.04, SD = 4.0 versus M = 3.6, SD = 2.8, F = 16.38, p < .001) and more anxiety symptoms (M = 6.6, SD = 4.0 versus M = 5.0, SD = 3.3, F = 18.60, p < .001).
Table 4.
Empathy, depression, anxiety, and burden scores of the groups.
| Informal caregivers (n = 201) | Control group (n = 187) | F | p-value | Partial η2 | |
|---|---|---|---|---|---|
| IRI PT, M ± SD | 17.6 ± 4.1 | 17.0 ± 4.3 | 0.98 | .323 | .003 |
| IRI EC, M ± SD | 17.8 ± 4.2 | 17.4 ± 4.1 | 2.66 | .104 | .007 |
| HADS–depression, M ± SD | 5.0 ± 4.0 | 3.6 ± 2.8 | 16.38 | <.001 | .042 |
| HADS–anxiety, M ± SD | 6.6 ± 4.0 | 5.0 ± 3.3 | 18.60 | <.001 | .047 |
| CRA, M ± SD | 60.0 ± 12.3 | – | – | – | – |
Note. IRI = Interpersonal Reactivity Scale, PT = subscale Perspective Taking, EC = subscale Empathic Concern, HADS = Hospital Anxiety and Depression Scale, CRA = Caregiver Reaction Assessment. The CRA was filled out by the caregivers only. For PT and EC, sex was added as a covariate in the analyses.
Discussion
Interventions for informal caregivers are beginning to focus on heightening the empathy informal caregivers have for the person with dementia they care for. The idea is that this should subsequently enhance the lives of both the caregivers and the people with dementia. Yet, previous research on the impact of heightened empathy on the empathizer's well-being yielded contradictory results. However, these studies all investigated linear relationships between empathy and (aspects of) well-being. Since there is evidence for both positive and negative relationships, we hypothesized that quadratic models may be more appropriate to explain the relationships. For informal dementia caregivers, we found a negative quadratic relationship between cognitive empathy and depression, and a positive linear relationship between affective empathy and anxiety. For non-caregivers, we found positive quadratic relationships between both cognitive and affective empathy and depression, and affective empathy and anxiety. The levels of neither cognitive nor affective empathy differed between the groups.
To our knowledge, only two studies quantitatively examined the association between empathy and aspects of well-being in informal caregivers (Lee et al., 2001, Sutter et al., 2014). Lee et al. (2001) found, using univariate analyses, that more cognitive empathy was correlated with less stress, less depression, less threat appraisal, and higher life satisfaction. Sutter et al. (2014) also found, in univariate analyses, that more empathy was correlated with less depression, burden, and stress. However, in the study by Lee et al. (2001), neither affective nor cognitive empathy predicted depression in a multiple linear regression analysis when controlling for activities of daily living of the care receiver, caregiver age, sex, and spousal status. When Sutter et al. (2014) employed multiple regression analyses, empathy only predicted less stress. This finding is comparable to our results: we also did not find a linear relationship between depression and cognitive empathy. Instead, we tested a quadratic model, which provided a better fit: an average amount of empathy was associated with the most depression symptoms, whereas the highest amount of empathy was associated with the least depression symptoms. A systematic review (Wilkinson et al., 2017), focusing on the relationship between empathy and burnout in health professionals, found evidence for both a negative relationship and a positive relationship between the two. However, they found more evidence for a negative association (more empathy–less burnout), especially for cognitive empathy. This is largely in line with our findings for informal caregivers since the highest level of cognitive empathy corresponded to the lowest level of depression.
However, in contradiction with the review by Wilkinson et al. (2017) and the study with informal caregivers by Sutter et al. (2014), we found no (significant) relationship between empathy and caregiver burden, a concept related to burn-out. A possible explanation for this difference in results lies in the questionnaires used. We measured caregiver burden using the total score of the CRA, which consists of the subscales self-esteem, financial problems, impact of caregiving on disrupted schedule, family support, and health problems. These subscales are different from the subscales of the Maslach Burnout Inventory (MBI) (Maslach & Jackson, 1986), which was used by the studies in the review by Wilkinson et al. (2017); and the Zarit Burden Inventory (ZBI) used by Sutter et al. (2014). The burnout questionnaire MBI includes the subscales emotional exhaustion, depersonalization, and personal accomplishment. The ZBI is a unidimensional scale, but includes questions about exhaustion, personal strain, role strain, and guilt or self-criticism (Al-Rawashdeh, Lennie, & Chung, 2016) and may be more similar to questionnaires for burn-out such as the MBI. This difference in operationalisations can explain the difference in results. Future research about burden and empathy could include another questionnaire for burden, and examine if similar results are obtained. Suggestions for burden scales are the ZBI, or the The Inventory of Overburden in Alzheimer's Patient Family Caregivers with no Specialized Training (IPSO-CA24) for Spanish caregivers (Pérez-Fuentes, Gázquez Linares, Ruiz Fernández, & Molero Jurado, 2017).
Lee et al. (2001) found affective empathy to negatively predict life satisfaction, but they did not assess caregiver anxiety. In fact, the link between affective empathy and anxiety has not been researched before in informal caregivers. We found that more anxiety symptoms were predicted by more affective empathy. This result is in line with research in the general population: Olsson et al. (2016) found that greater empathy levels relate to more vicarious fear, and Shu et al. (2017) even argued for a causal pathway between empathy and anxiety, where more affective empathy leads to more anxiety. In addition, our results can be explained by the findings of a review by Wilkinson et al. (2017). They found studies supporting the theory of ‘compassion fatigue’, whereby clinicians who demonstrate high levels of affective empathy suffered from compassion fatigue, which then leads to burn out. Our finding, that too much affective empathy, or ‘feeling what another person feels’ is associated with more anxiety, can be explained by the same theory. For informal caregivers, this might especially be the case since the other person has dementia and informal caregivers are generally more anxious to get dementia themselves (Kim, Kim, & An, 2016). However, this review (Wilkinson et al., 2017) focused on health professionals, and not informal caregivers. Although they both ‘care for’ someone with dementia, the relationship between the caregiver and care receiver is intrinsically different for informal and professional carers. Informal caregivers are more personally involved, which should be taken into account when comparing these populations.
In fact, we found that while the levels of empathy did not differ between informal caregivers and non-caregivers, the relationships between (affective and cognitive) empathy and depression and anxiety, were different for caregivers and non-caregivers. For non-caregivers, as hypothesized, we found that too much, and too little, cognitive empathy predicted more depression symptoms. In addition, we found that too much, and too little affective empathy predicted both more anxiety and depression symptoms. These findings, compared with our findings for caregivers, might indicate that empathy has different effects on the empathizer when one cares for a person with dementia compared to when one does not. A possible explanation for these different relationships is that caregivers interpret the empathy questionnaire with their care receiver in mind, whereas non-caregivers think of more general scenarios without thinking of specific persons or situations. The Perspective Taking subscale of the IRI encompasses statements like “When I’m upset at someone, I usually try to “put myself in his shoes” for a while”. When caregivers positively reflect to these statements with the care receiver in mind, this might mean that they have fewer arguments with the care receiver, and a better relationship with each other, which in turn might lead to fewer depression symptoms. On the other hand, from the point of view of the non-caregivers, always trying to see things from another's’ perspective might be fatiguing. We think that, when one always (in any situation) acts according to this principle, this could cause them to lose the ability to prioritize what they want or need themselves. Then, too much cognitive empathy could in turn lead to more depression symptoms. We therefore think that one should be hesitant to compare the relationship between empathy, and anxiety or depression, in different populations.
Some limitations should be addressed. To measure empathy, we used the IRI, arguably the most-used measure to assess empathy, especially in the general (not professional/medical) population. However, some of our participants found the questions difficult to answer, even after giving further clarification if they asked for this during the interviews. In addition, the reliability of the questionnaire was quite low, and since empathy questionnaires rely on self-report, one could argue that instead of measuring cognitive and affective empathy, only the appraisal of empathy is measured: the participants’ opinion about how they would feel or act in a certain situation, rather than the emotion or behavior itself. A means to overcome these questionnaire-related problems in future studies is to also include objective measures of empathy (behavioral tasks or empathy accuracy tasks accompanied by psychophysiological methods (Devlin et al., 2014, Neumann and Westbury, 2011). Then, empathy itself could be related to aspects of well-being, instead of only the participants’ appraisal of their empathy. Last, the study was cross-sectional in design making it impossible to talk about cause-effect relationships. Strong points of this study are its large sample sizes, the unique examination of both linear and quadratic relationships, and the inclusion of both informal caregivers and non-caregiver controls to be able to put the results of the informal caregivers into perspective.
Conclusions
Our results have important implications for future research and clinical practice. We found that quadratic models examining the relationship between empathy and aspects of well-being fit better than linear models. For non-caregivers, there seems to be an ‘optimal’ level of (cognitive and affective) empathy, whereas too much or too little empathy is associated with more depression/anxiety symptoms. Future research into empathy and its consequences should bear this in mind. In addition, we conclude that caregivers have a ‘normal’ amount of empathy, compared to non-caregivers. In caregivers, this normal level of cognitive empathy was associated with the most depression symptoms, which might be detrimental to their well-being. The highest level of cognitive empathy might be ideal since this was associated with the least depression symptoms. In addition, less affective empathy was associated with fewer anxiety symptoms. Interventions for informal caregivers could aim to heighten cognitive empathy to diminish depression symptoms and to lower affective empathy to diminish anxiety symptoms. Possible strategies could include psycho-education, or role-play to increase perspective taking, and coping skill-training or counseling to diminish the tendency to share the emotions of the person with dementia.
Acknowledgments
This work was supported by the program Memorabel, of The Netherlands Organisation for Health Research and Development (ZonMw), part of The Netherlands Organisation for Scientific Research (NWO); and Alzheimer Nederland (project number: 733050608). However, solely the authors are responsible for the design and conduct of this study, study analyses, interpreting, drafting, and editing of this article. We thank the Alzheimer cafes, case managers, supervisors at day-time activity centers and De Wever in Tilburg for their efforts in helping us to recruit participants. We would especially like to thank all the people who participated in this study for their time.
References
- Al-Rawashdeh S.Y., Lennie T.A., Chung M.L. Psychometrics of the Zarit Burden Interview in caregivers of patients with heart failure. The Journal of Cardiovascular Nursing. 2016;31:E21. doi: 10.1097/JCN.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron-Cohen S., Wheelwright S. The empathy quotient: An investigation of adults with Asperger syndrome or high functioning autism, and normal sex differences. Journal of Autism and Developmental Disorders. 2004;34:163–175. doi: 10.1023/b:jadd.0000022607.19833.00. [DOI] [PubMed] [Google Scholar]
- Batt-Rawden S.A., Chisolm M.S., Anton B., Flickinger T.E. Teaching empathy to medical students: An updated, systematic review. Academic Medicine. 2013;88:1171–1177. doi: 10.1097/ACM.0b013e318299f3e3. [DOI] [PubMed] [Google Scholar]
- Chiao C.Y., Wu H.S., Hsiao C.Y. Caregiver burden for informal caregivers of patients with dementia: A systematic review. International Nursing Review. 2015;62:340–350. doi: 10.1111/inr.12194. [DOI] [PubMed] [Google Scholar]
- Davis M.H. A multidimensional approach to individual differences in empathy. Journal of Southern African Studies. 1980;10:85–104. [Google Scholar]
- Davis M.H. Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology. 1983;44:113–126. [Google Scholar]
- Decety J., Jackson P.L. The functional architecture of human empathy. Behavioral and Cognitive Neuroscience Reviews. 2004;3:71–100. doi: 10.1177/1534582304267187. [DOI] [PubMed] [Google Scholar]
- Decety J., Michalska K.J., Kinzler K.D. The developmental neuroscience of moral sensitivity. Emotion Review. 2011;3:305–307. [Google Scholar]
- Derksen F., Bensing J., Lagro-Janssen A. Effectiveness of empathy in general practice: A systematic review. British Journal of General Practice. 2013;63:e76–e84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devlin H.C., Zaki J., Ong D.C., Gruber J. Not as good as you think? Trait positive emotion is associated with increased self-reported empathy but decreased empathic performance. PloS One. 2014;9:e110470. doi: 10.1371/journal.pone.0110470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N., Lennon R. Sex differences in empathy and related capacities. Psychological Bulletin. 1983;94:100. [Google Scholar]
- Field A. Sage publications; Thousand Oaks, California: 2009. Discovering statistics using SPSS. [Google Scholar]
- Hattink B., Meiland F., van der Roest H., Kevern P., Abiuso F., Bengtsson J., Giuliano A., Duca A., Sanders J., Basnett F., Nugent C., Kingston P., Dröes R.M. Web-based STAR E-learning course increases empathy and understanding in dementia caregivers: Results from a randomized controlled trial in the Netherlands and the United Kingdom. Journal of Medical Internet Research. 2015;17:e241. doi: 10.2196/jmir.4025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen M., Agbata I.N., Canavan M., McCarthy G. Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: Systematic review and meta-analysis of randomised controlled trials. International Journal of Geriatric Psychiatry. 2015;30:130–143. doi: 10.1002/gps.4208. [DOI] [PubMed] [Google Scholar]
- Joling K.J., van Marwijk H.W., Veldhuijzen A.E., van der Horst H.E., Scheltens P., Smit F., van Hout H.P. The two-year incidence of depression and anxiety disorders in spousal caregivers of persons with dementia: Who is at the greatest risk? American Journal of Geriatric Psychiatry. 2015;23:293–303. doi: 10.1016/j.jagp.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Jütten L.H., Mark R.E., Janssen B.W.J.M., Rietsema J., Dröes R.-M., Sitskoorn M.M. Testing the effectivity of the mixed virtual reality training Into D’mentia for informal caregivers of people with dementia: Protocol for a longitudinal, quasi-experimental study. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-015702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasuya R.T., Polgar-Bailey M.P., Robbyn Takeuchi M.P.H. Caregiver burden and burnout a guide for primary care physicians. Postgraduate Medicine. 2000;108:119. doi: 10.3810/pgm.2000.12.1324. [DOI] [PubMed] [Google Scholar]
- Keith T.Z. Abingdon-on-Thames; Routledge: 2014. Multiple regression and beyond: An introduction to multiple regression and structural equation modeling. [Google Scholar]
- Kim J.S., Kim E.H., An M. Experience of dementia-related anxiety in middle-aged female caregivers for family members with dementia: A phenomenological study. Asian Nursing Research. 2016;10:128–135. doi: 10.1016/j.anr.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Lamothe M., Boujut E., Zenasni F., Sultan S. To be or not to be empathic: The combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Family Practice. 2014;15:1. doi: 10.1186/1471-2296-15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.S., Brennan P.F., Daly B.J. Relationship of empathy to appraisal, depression, life satisfaction, and physical health in informal caregivers of older adults. Research in Nursing and Health. 2001;24:44–56. doi: 10.1002/1098-240x(200102)24:1<44::aid-nur1006>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Mahoney R., Regan C., Katona C., Livingston G. Anxiety and depression in family caregivers of people with Alzheimer disease: The LASER-AD study. American Journal of Geriatric Psychiatry. 2005;13:795–801. doi: 10.1176/appi.ajgp.13.9.795. [DOI] [PubMed] [Google Scholar]
- Manczak E.M., DeLongis A., Chen E. Does empathy have a cost? Diverging psychological and physiological effects within families. Health Psychology. 2016;35:211. doi: 10.1037/hea0000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C., Jackson S. Consulting Psychologists Press, University of California; Palo Alto: 1986. MBI: Maslach Burnout Inventory. Manual Research edition. [Google Scholar]
- Meshefedjian G., McCusker J., Bellavance F., Baumgarten M. Factors associated with symptoms of depression among informal caregivers of demented elders in the community. The Gerontologist. 1998;38:247–253. doi: 10.1093/geront/38.2.247. [DOI] [PubMed] [Google Scholar]
- Neumann D., Westbury H. The psychophysiological measurement of empathy. In: Scapaletti D.J., editor. Psychology of empathy. Nova Science Publishers, Inc; Hauppauge, NY: 2011. pp. 119–142. [Google Scholar]
- Nijboer C., Triemstra M., Tempelaar R., Sanderman R., Van Den Bos G. Measuring both negative and positive reactions to giving care to cancer patients: Psychometric qualities of the Caregiver Reaction Assessment (CRA) Social Science and Medicine. 1999;48:1259–1269. doi: 10.1016/s0277-9536(98)00426-2. [DOI] [PubMed] [Google Scholar]
- Olsson A., McMahon K., Papenberg G., Zaki J., Bolger N., Ochsner K.N. Vicarious fear learning depends on empathic appraisals and trait empathy. Psychological Science. 2016;27:25–33. doi: 10.1177/0956797615604124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panyavin I., Trujillo M.A., Peralta S.V., Stolfi M.E., Morelli E., Perrin P.B., Lasa J.P., Arango-Lasprilla J.C. Examining the influence of family dynamics on quality of care by informal caregivers of patients with Alzheimer's dementia in Argentina. American Journal of Alzheimer's Disease & Other Dementias. 2015;30:613–621. doi: 10.1177/1533317515577129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Fuentes M.C., Gázquez Linares J.J., Ruiz Fernández M.D., Molero Jurado M.M. Inventory of overburden in Alzheimer's patient family caregivers with no specialized training. International Journal of Clinical and Health Psychology. 2017;17:56–64. doi: 10.1016/j.ijchp.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M., Wimo A., Guerchet M., Ali G., Wu Y., Prina M. Alzheimer's Disease International (ADI); London: 2015. World Alzheimer Report. The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. [Google Scholar]
- Schaufeli W.B., Maslach C., Marek T. Taylor & Francis; Philadeplphia, PA, US: 1993. Series in applied psychology: Social issues and questions. Professional burnout: Recent developments in theory and research. [Google Scholar]
- Schoenmakers B., Buntinx F., Delepeleire J. Factors determining the impact of care-giving on caregivers of elderly patients with dementia. A systematic literature review. Maturitas. 2010;66:191–200. doi: 10.1016/j.maturitas.2010.02.009. [DOI] [PubMed] [Google Scholar]
- Shamay-Tsoory S.G. The neural bases for empathy. The Neuroscientist. 2011;17:18–24. doi: 10.1177/1073858410379268. [DOI] [PubMed] [Google Scholar]
- Shim B., Barroso J., Davis L.L. A comparative qualitative analysis of stories of spousal caregivers of people with dementia: Negative, ambivalent, and positive experiences. International Journal of Nursing Studies. 2012;49:220–229. doi: 10.1016/j.ijnurstu.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Shu J., Hassell S., Weber J., Ochsner K.N., Mobbs D. The role of empathy in experiencing vicarious anxiety. Journal of Experimental Psychology: General. 2017;146:1164. doi: 10.1037/xge0000335. [DOI] [PubMed] [Google Scholar]
- SPSS Inc. IBM Corp.; Armonk, NY: 2013. IBM SPSS Statistics for Windows, Version 22.0. [Google Scholar]
- Sutter M., Perrin P.B., Chang Y.-P., Hoyos G.R., Buraye J.A., Arango-Lasprilla J.C. Linking family dynamics and the mental health of Colombian dementia caregivers. American Journal of Alzheimer's Disease & Other Dementias. 2014;29:67–75. doi: 10.1177/1533317513505128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas M.R., Dyrbye L.N., Huntington J.L., Lawson K.L., Novotny P.J., Sloan J.A., Shanafelt T.D. How do distress and well-being relate to medical student empathy? A multicenter study. Journal of General Internal Medicine. 2007;22:177–183. doi: 10.1007/s11606-006-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhage F. Van Gorcum; Assen: 1964. Intelligentie en leeftijd: Onderzoek bij Nederlanders van twaalf tot zevenenzeventig jaar. [Google Scholar]
- Wijma E.M., Veerbeek M.A., Prins M., Pot A.M., Willemse B.M. A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: Results of a pilot study. Aging & Mental Health. 2017;10:1–9. doi: 10.1080/13607863.2017.1348470. [DOI] [PubMed] [Google Scholar]
- Wilkinson H., Whittington R., Perry L., Eames C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burnout Research. 2017;6:18–29. doi: 10.1016/j.burn.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]