Abstract
During the ‘Heart Failure and World Congress on Acute Heart Failure 2018’, many sessions and lectures focused on cardio‐oncology. This important field of research is constantly growing, and therefore, a great amount of time during the congress focused on it. Prevention and early recognition of side effects is very important in cancer patients. One of the most common and potentially severe problems during antineoplastic therapy is cardiotoxicity. Hence, cardio‐oncology is vital in managing cancer patients. This paper will summarize the topics discussed in three main sessions and many additional lectures throughout the ‘Heart Failure and World Congress on Acute Heart Failure 2018’. The covered topics included pathophysiological mechanisms in the development of heart failure, risk factors, and early signs of cardiotoxicity detectable with different circulating and imaging biomarkers, as well as cardioprotective treatments recommended by different guidelines and position papers.
Keywords: Heart failure, Cancer, Cardiotoxicity
Introduction
Cardio‐oncology has become a large, expanding, and important translational research area in modern medicine, which is gaining rapid interest.1, 2 Unfortunately, chemotherapy, immunotherapy, radiation therapy, and targeted therapies do not only effect cancer cells but also effect cardiomyocytes and vascular cells.3 This can result into minor, asymptomatic cardiac lesions, detectable with circulating biomarkers or strain echocardiography, and also into life‐threatening conditions, like severe heart failure (HF) or fulminant myocarditis.4, 5 During the ‘Heart Failure and World Congress on Acute Heart Failure 2018’, three full scientific sessions as well as a number of additional lectures within broader‐subject sessions were dedicated to cardio‐oncology. The sessions aimed to help improve the mechanistic understanding of cardiotoxicity as well as to help clinicians with practical advice and treatment strategies for cancer patients receiving potentially cardiotoxic oncology therapies. The congress was attended by 5881 participants with >300 faculty members from 47 countries and took place in Vienna, Austria, from May 26, 2018, to May 29, 2018.
The first cardio‐oncology session started from pathophysiological studies on the crosstalk of HF and cancer mechanisms and then addressed how to approach cardiotoxicity in cancer patients with preclinical markers of left ventricular dysfunction (LVD) and in patients with confirmed cardiotoxicity. The second session discussed the prevalence of cardiac dysfunction in cancer patients and the underlying mechanisms. The third session reviewed the current recommendations and gaps in evidence from the different cardio‐oncology guidelines and position statements. Additional lectures addressed cardiomyopathy in cancer and the prevention of HF. Detailed listing of all sessions can be found in Table S1 .
Prevention and treatment of cardiotoxicity
In modern‐day oncology, cardiotoxicity is a growing problem1 and may be caused by cytotoxic chemotherapy, radiotherapy, molecular targeted therapies, and immune‐modulating agents. In this scenario, active collaboration among different medical specialists is required to integrate cardiac imaging in cardio‐oncology and to guide cardiovascular (CV) monitoring (Figure 1). Various definitions of CV toxicity exist depending upon the modalities used and whether clinical symptoms are required. Regarding direct myocardial toxicity, one common definition is a reduction of left ventricular ejection fraction (LVEF) by >10 percentage points and below the lower limit of normality (depending on local standard operating procedure 50–55%).1 Cardiomyopathy in cancer is becoming an increasingly recognized entity, as Professor Dimitrios Farmakis from Athens, Greece, stressed during a session dedicated to cardiomyopathies. Besides anthracyclines, several additional agents may predispose to the development of cardiomyopathies, while recent evidence has shed some new light on the underlying pathophysiology. Professor Farmakis emphasized that the two main challenges of modern‐day cardio‐oncology are the integration of subtle cardiac dysfunction surrogates into clinical practice and proving that cardio‐active therapies are effective in preventing cardiomyopathies in cancer patients.
Figure 1.
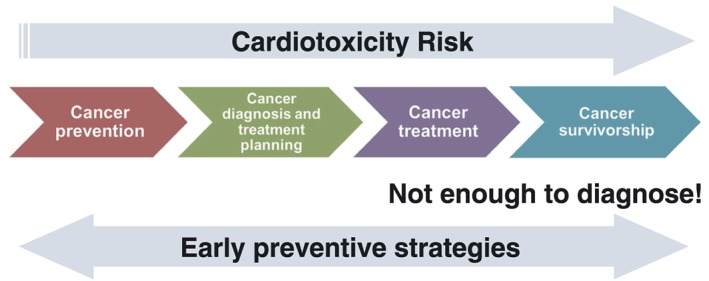
How to best deliver care.
Dr Teresa López‐Fernández from Madrid, Spain, described the established relevant risk factors for developing cardiotoxicity: young (<18 years) or advanced age (>65 years), simultaneous chemotherapy with other potential cardiotoxic agents, previous radiation therapy, chronic kidney disease, and established CV disease or risk factors.1, 6 Consequently, before initiation of anti‐cancer therapy treatment, it is important to assess the patient's individual risk of cardiotoxicity.7 Dr López‐Fernández highlighted the need to perform a baseline comprehensive CV screening, including echocardiography assessment, to exclude relevant cardiac problems and to optimize CV therapy when needed8, 9 (Figure 2). During and after cancer treatment, cardiac biomarkers and new echocardiography techniques are crucial in detecting LVD. Moreover, she recommended using an automated quantification of three‐dimensional ejection fraction, as it requires less time and has a higher reproducibility.10 Another important question is if cardiac monitoring just based on LVEF is enough. Serum cardiac biomarkers and deformation parameters have demonstrated to be more sensitive to detect subclinical myocardial damage.1, 11 An increase in cardiac troponins or a relative reduction of global longitudinal strain measured using speckle echocardiography by >15% from baseline can help identifying patients at increased risk of LVD with a good negative predictive value.1, 12 In addition, if LVEF remains within the normal limits, but subclinical damage is detected, Dr López‐Fernández explained that these patients may benefit from additional cardioprotective medication [angiotensin‐converting enzyme (ACE)‐inhibitors, angiotensin receptor blockers, and/or beta‐blockers] in order to reduce the risk of future events.13 There is an urgent need for randomized, double‐blind controlled trials to confirm such benefits because early HF treatment does not always allow full recovery of ventricular function in patients who have developed cardiotoxicity. Recent data from Cardinale et al.14 confirmed the need for early cardiotoxicity diagnosis. In 2625 patients treated with anthracyclines, with a prevalence of cardiotoxicity of 9%, it was demonstrated that 98% of events occur within the first year of treatment. If cardiotoxicity occurred, beta‐blocker and ACE‐inhibitor treatment were started and increased to the highest tolerated dose. With this therapy, a partial recovery of LVEF >50% was observed in 82% of patients, but only 11% of patients achieved a full LVEF recovery. If chronic HF develops nonetheless, it is associated with high treatment costs15 and even on its own with disappointing 1 and 5 year survival rates of just 85 and 50%.16, 17, 18, 19 A very important part of modern‐day research is the many different multi‐centre registries.20, 21, 22, 23 They help us to better understand the diverse problems24, 25, 26 and needs27, 28, 29 of our patients in day‐to‐day life,30, 31, 32 monitor the quality of treatment,33, 34, 35 and identify new risk factors.36, 37
Figure 2.
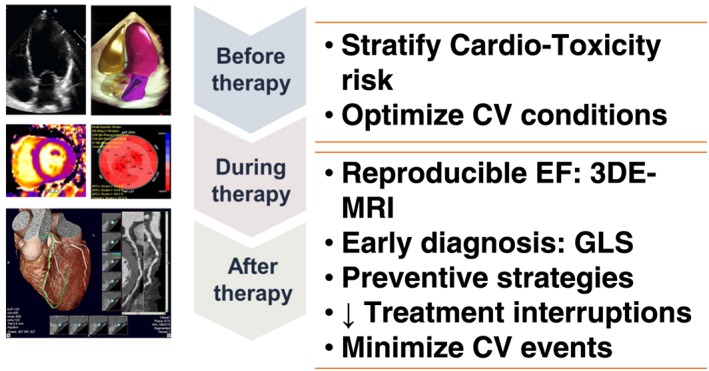
Role of cardiac imaging in cardio‐oncology.
Thus, the prevention of HF in cancer patients is very important. Professor Alain Cohen‐Solal from Paris, France, addressed a study conducted in 273 low CV risk adult cancer patients treated with low cumulative doses of anthracycline chemotherapy called ‘The International CardioOncology Society‐One’ trial.38 There were two arms in the study: in the first, enalapril was only administered during chemotherapy cycles if troponin levels increased, and in the second, enalapril was administered before and during the entire chemotherapy regime. With regard to the occurrence of cardiotoxicity, both strategies resulted in similar results. The authors concluded that the administration of enalapril may be suitable for patients with an increase of troponin values during anthracycline treatment, and Alain Cohen‐Solal emphasized that quick initiation of CV treatment after detection of subclinical LVD is vital in cancer patients.39 During a session on prevention of HF, Professor Dimitrios Farmakis addressed the interaction between HF and cancer, two entities that share several common risk factors, while the one seems to increase the risk and worsen the outcome of the other. Professor Farmakis grouped the strategies for the prevention of HF in cancer into three main categories, including ‘primordial prevention’ that is applicable before cancer therapy in patients without any evidence of CV abnormalities, ‘primary prevention’ during cancer therapy in the presence of subtle abnormalities such as increase in cardiac biomarkers or worsening of left ventricular global longitudinal strain, and ‘secondary prevention’ during or after cancer therapy in the presence of clear LVEF decline. All three approaches are important in preventing HF in cancer patients.40
In the next congress presentation, Professor Thomas Suter from Bern, Switzerland, discussed the alternative clinical strategies to prevent cardiotoxicity. Professor Suter explained that in some cases, also non‐anthracycline chemotherapies are an option, because these drugs are often associated with a lower chance of cardiotoxicity during treatment for high‐risk patients but still can be effective in treating cancer.1, 41 Furthermore, to reduce the likelihood of LVD and cardiotoxicity even further in some patients, he reviewed using liposomal doxorubicin or concomitant dexrazoxane (DEX).1, 42 Newer options for cancer patients include targeted therapies like trastuzumab, which can also be associated with increased occurrence of cardiotoxicity.43 Treatment duration of trastuzumab therapy is relevant to risk, and the benefit on HER2+ malignancies is significant and must be remembered when considering the risk:benefit balance.44
The intersection between cardiology and oncology
In patients with HF, many different co‐morbidities can influence the patients' burden of disease.45, 46 Common co‐morbidities in patients with HF include iron deficiency,47, 48 anaemia,49, 50 liver dysfunction,51, 52 chronic kidney disease,53, 54 central sleep apnoea,55, 56 chronic obstructive pulmonary disease,57, 58 sexual dysfunction,59, 60 cachexia,61, 62 sarcopenia,63, 64 anorexia,65, 66 and also cancer.67, 68 Professor Rudolf De Boer from Groningen, the Netherlands, presented several studies, which have shown that cancer patients have an increased risk to develop HF and that patients with both, cancer and HF, demonstrate even worse prognosis than both diseases alone.69, 70 Interestingly, many cancers and HF share similar risk factors like hypertension, smoking, diabetes, and overweight.71, 72, 73 Rudolf De Boer concluded that HF per se might promote tumour growth through inflammatory mechanisms and circulating biochemical factors.74
The relatively frequent occurrence of HF in cancer patients, which can lead to higher CV mortality75 and worse overall prognosis, which is substantially attributed to anti‐cancer therapy,76 was discussed by Jochen Springer from Göttingen, Germany. New theories are being investigated, and it has been shown that cancer cells secrete factors (e.g. Ataxin‐10) that interfere with the metabolism of cardiomyocytes and can cause wasting of the cardiac muscle,77 which may result into a negative effect on prognosis.67 Furthermore, cardiac muscle wasting in patients with lung, pancreatic, and gastrointestinal cancers has been shown recently.78, 79 Elevated circulating CV biomarkers, as predictors of mortality,80 as well as impairments in the cardiopulmonary function,81 were also found in chemotherapy naïve tumour patients. A recent multivariate survival analysis in patients with colorectal, pancreatic, and non‐small lung cancer has shown that a resting heart rate ≥75 beats per minute was independently associated with worse survival.82 This might represent an activation of the sympathetic nervous system like it has already been observed in patients with HF.83 Consequently, more research into this area is needed to better understand systemic effects of cancer on the CV system.
Drs Javid Moslehi from Nashville, USA, and Carlo Gabriele Tocchetti from Naples, Italy, compared classical and new anti‐cancer therapies and put an emphasis on different mechanisms of cardiotoxicity.84, 85 Substantial research is currently focused on understanding novel mechanisms of short‐term and long‐term effects of anthracycline cardiotoxicity on the heart muscle,86 and also newer therapies like immunotherapies87 and target therapies (e.g. tyrosine kinase inhibitors and trastuzumab)88 have been shown to be associated with cardiac dysfunction in some patients.1 Recently, immune checkpoint inhibitors have been shown to cause fulminant myocarditis.89 Martin Štěrba from Hradec Králové, Czech Republic, discussed the potential use of ACE‐inhibitors/angiotensin receptor blocker in prevention against chronic anthracyclines cardiotoxicity referring to rabbit models90 and positive outcomes in the OVERCOME91 and PRADA92 trials. He also introduced the demanding necessity to better analyse the antioxidant mechanisms of DEX: in fact, a recent preclinical study93 hypothesized that the depletion of topoisomerase 2β isoform, induced by DEX, might be the key process involved in the DEX cardioprotection.94
Breast cancer in a patient with heart failure
The management of HF in patients with breast cancer as a co‐morbidity was discussed in this session, with regard to directives of the current guidelines. Dr Thomas Suter reported two different approaches towards HF with reduced ejection fraction and HF with preserved ejection fraction. In the first case, he said, it is recommended to avoid both anthracyclines and trastuzumab if LVEF is <40%. In general, chemotherapy drugs like taxanes and liposomal doxorubicin may be used to minimize cardiotoxic side effects.95 When the patient is affected by HF with preserved ejection fraction, both anthracycline‐based chemotherapy and targeted therapies can sometimes still be used, but it is important to discuss this in a multidisciplinary team and define appropriate screening intervals for clinical monitoring of the patients.
Guidelines on anti‐cancer treatment in patients with HF were reviewed and analysed by Dr Alexander Lyon, London, UK, and gaps in evidence commented by Dr Markus Anker from Berlin, Germany. According to the current European Society of Cardiology 2016 position paper on cardiotoxicity,1 patients with higher risk (lifestyle risk factors, CV risk factors, current cardiac disease, and previous cardiotoxic treatment) should be identified and surveilled, for example, by regular clinical echocardiographic examination and cardiac biomarker screening. In 2012, the ‘European Society of Medical Oncology Cardiotoxicity Guidelines’96 recommended frequent cardiac monitoring of patients with high‐dose doxorubicin chemotherapy or/and pre‐existing CV disease. In the ‘American Society of Clinical Oncology Guidelines 2017’,97 the potential cardioprotective effect of DEX in high‐risk patients was positively documented, but its administration to cancer patients is associated with more frequent occurrence of leukopenia with respect to a meta‐analysis.98 Moreover, Cardinale et al.14 demonstrated that prompt cardioprotective intervention with combination of ACE‐inhibitors and beta‐blockers is a possible option for recovery of LVEF after early detection of cardiac damage in echocardiograms. The recent position paper from the Heart Failure Association Cardio‐oncology Study Group provides a contemporary review and framework for the patient with HF who develops cancer.74 Markus Anker also discussed the neutral double‐blind, placebo‐controlled CECCY99 trial that assessed the use of carvedilol for the prevention of anthracycline toxicity in a low CV risk cancer population and noted a short period of follow‐up time in this trial. He concluded that future trials in cardio‐oncology should have longer follow‐up times, assess patients, who have a greater risk of cardiotoxicity, and test relevant (higher) doses of cardiotoxic chemotherapy.
Conclusions
During the ‘Heart Failure and World Congress on Acute Heart Failure 2018’, three sessions focused on the quickly growing field of cardio‐oncology, along with some additional lectures during broader‐themed sessions. The main focus of the sessions was how to recognize and treat cardiotoxicity in the clinical setting. More research including randomized clinical studies is needed to learn more about the prevention of cardiotoxicity and the long‐term treatment of cancer patients with cardiac dysfunction.
Conflict of interest
A.L., S.H., Y.B., J.B.‐K., A.C.‐S., D.F., R.P., and T.S. report no conflict of interest. M.S.A. reports receiving personal fees from Servier. The UMCG, which employs R.A.d.B., has received research grants and/or fees from AstraZeneca, Abbott, Bristol‐Myers Squibb, Novartis, Roche, Trevena, and Thermo Fisher GmbH. R.A.d.B. is a minority shareholder of scPharmaceuticals, Inc., and received personal fees from MandalMed Inc., Novartis, and Servier. S.v.H. has been a paid consultant for Chugai, Vifor, BRAHMS, Roche, Boehringer Ingelheim, Novartis, Bayer, Hexal, Grünenthal, and Helsinn. T.L.‐F. reports speaker fees from Servier, Pfizer, Novartis, and Janssen‐Cilag Ltd. C.G.T. received speaker fees from Alere. A.R.L. reports grants from Servier and Pfizer and speaker fees, advisory board fees, and/or consultancy fees from Servier, Pfizer, Novartis, Roche, Takeda, Boehringer Ingelheim, Amgen, Clinigen Group, Ferring Pharmaceuticals, Bristol‐Myers Squibb, Eli Lily, and Janssen‐Cilag Ltd.
Funding
None.
Supporting information
Table S1. Cardio‐oncology sessions during ‘Heart Failure and World Congress on Acute Heart Failure 2018’.
Anker, M. S. , Lena, A. , Hadzibegovic, S. , Belenkov, Y. , Bergler‐Klein, J. , de Boer, R. A. , Cohen‐Solal, A. , Farmakis, D. , von Haehling, S. , López‐Fernández, T. , Pudil, R. , Suter, T. , Tocchetti, C. G. , Lyon, A. R. , and for the Heart Failure Association Cardio‐Oncology Study Group of the European Society of Cardiology (2018) Modern‐day cardio‐oncology: a report from the ‘Heart Failure and World Congress on Acute Heart Failure 2018’. ESC Heart Failure, 5: 1083–1091. 10.1002/ehf2.12386.
References
- 1. Zamorano JL, Lancellotti P, Rodruguez Munoz D, Aboyans R, Galderisi M, Habib G, Lenihan DJ, Lip GYH, Lyon AR, Lopez Fernandez T, Mohty D, Tamargo J, Torbicki A, Suter ZM, ESC Scientific Document Group . 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 2768–2801. [DOI] [PubMed] [Google Scholar]
- 2. Bellinger AM, Arteaga CL, Force T, Humphreys BD, Demetri GD, Druker BJ, Moslehi JJ. Cardio‐oncology: how new targeted cancer therapies and precision medicine can inform cardiovascular discovery. Circulation 2015; 132: 2248–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Angsutararux P, Luanpitpong S, Issaragrisil S. Chemotherapy‐induced cardiotoxicity: overview of the roles of oxidative stress. Oxid Med Cell Longev 2015; 2015: 795602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnson DB, Balko JM, Compton ML, Chalkias S, Gorham J, Xu Y, Hicks M, Puzanov I, Alexander MR, Bloomer TL, Becker JR, Slosky DA, Phillips EJ, Pilkinton MA, Craig‐Owens L, Kola N, Plautz G, Reshef DS, Deutsch JS, Deering RP, Olenchock BA, Lichtman AH, Roden DM, Seidman CE, Koralnik IJ, Seidman JG, Hoffman RD, Taube JM, Diaz LA Jr, Anders RA, Sosman JA, Moslehi JJ. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med 2016; 375: 1749–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berg DD, Vaduganathan M, Nohria A, Davids MS, Alyea EP, Torre M, Padera RF Jr. Immune‐related fulminant myocarditis in a patient receiving ipilimumab therapy for relapsed chronic myelomonocytic leukaemia. Eur J Heart Fail 2017; 19: 682–685. [DOI] [PubMed] [Google Scholar]
- 6. Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the ‘Silver Tsunami’: prevalence trajectories and co‐morbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev 2016; 25: 1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Armenian SH, Lachhetti C, Barac A, Carver J, Constine LS, Denduluri N, Dent S, Douglas PS, Durand JB, Ewer M, Fabian C, Hudson M, Jessup M, Jones LW, Ky B, Mayer EL, Moleshi J, Oeffinger K, Ray K, Ruddy K, Lenihan D. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2017; 35: 893–911. [DOI] [PubMed] [Google Scholar]
- 8. Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer‐Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP, Banchs J, Cardinale D, Carver J, Cerqueira M, DeCara JM, Edvardsen T, Flamm SD, Force T, Griffin BP, Jerusalem G, Liu JE, Magalhães A, Marwick T, Sanchez LY, Sicari R, Villarraga HR, Lancellotti P. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2014; 27: 911–939. [DOI] [PubMed] [Google Scholar]
- 9. López‐Fernández T, Martín García A, Santaballa Beltrán A, Montero Luis Á, García Sanz R, Mazón Ramos P, Velasco Del Castillo S, López de Sá Areses E, Barreiro‐Pérez M, Hinojar Baydes R, Pérez de Isla L, Valbuena López SC, Dalmau González‐Gallarza R, Calvo‐Iglesias F, González Ferrer JJ, Castro Fernández A, González‐Caballero E, Mitroi C, Arenas M, Virizuela Echaburu JA, Marco Vera P, Íñiguez Romo A, Zamorano JL, Plana Gómez JC, López Sendón Henchel JL. Cardio‐onco‐hematology in clinical practice. Position paper and recommendations. Rev Esp Cardiol (Engl Ed) 2017; 70: 474–486. [DOI] [PubMed] [Google Scholar]
- 10. Tamborini G, Piazzese C, Lang RM, Muratori M, Chiorino E, Mapelli M, Fusini L, Ali SG, Gripari P, Pontone G, Andreini D, Pepi M. Feasibility and accuracy of automated software for transthoracic three‐dimensional left ventricular volume and function analysis: comparisons with two‐dimensional echocardiography, three‐dimensional transthoracic manual method, and cardiac magnetic resonance imaging. J Am Soc Echocardiogr 2017; 30: 1049–1058. [DOI] [PubMed] [Google Scholar]
- 11. Lang RM, Badano LP, Mor‐Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28: 1–39 e14. [DOI] [PubMed] [Google Scholar]
- 12. Thavendiranathan P, Poulin F, Lim K‐M, Plana JC, Woo A, Marwich TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol 2014; 63: 2751–2768. [DOI] [PubMed] [Google Scholar]
- 13. López‐Fernández T, García AM, Beltrán AS, Luis AM, Sanz RG, Ramos PM, del Castillo SV, de Sá Areses EL, Barreiro‐Pérez M, Baydes RH, de Isla LP, López SCV, González‐Gallarza RD, Calvo‐Iglesias F, Ferrer JJG, Fernández AC, González‐Caballero E, Mitroi C, Arenas M, Echaburu JAV, Vera PM, Romo AI, Zamorano JL, Plana Gómez JC, Henchel JLLS. Cardio‐onco‐hematology in clinical practice. Position paper and recommendations. Rev Esp Cardiol 2017; 70: 474–486. [DOI] [PubMed] [Google Scholar]
- 14. Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, Civelli M, Lamantia G, Colombo N, Curigliano G, Fiorentini C, Cipolla CM. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 2015; 131: 1981–1988. [DOI] [PubMed] [Google Scholar]
- 15. Salem K, ElKhateeb O. Gender‐adjusted and age‐adjusted economic inpatient burden of congestive heart failure: cost and disability‐adjusted life‐year analysis. ESC Heart Fail 2017; 4: 259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mamas MA, Sperrin M, Watson MC, Coutts A, Wilde K, Burton C, Kadam UT, Kwok CS, Clark AB, Murchie P, Buchan I, Hannaford PC, Myint PK. Do patients have worse outcomes in heart failure than in cancer? A primary care‐based cohort study with 10‐year follow‐up in Scotland. Eur J Heart Fail 2017; 19: 1095–1104. [DOI] [PubMed] [Google Scholar]
- 17. Cohen‐Solal A, Jacobson AF, Piña IL. Beta blocker dose and markers of sympathetic activation in heart failure patients: interrelationships and prognostic significance. ESC Heart Fail 2017; 4: 499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yoshihisa A, Watanabe S, Yokokawa T, Misaka T, Sato T, Suzuki S, Oikawa M, Kobayashi A, Takeishi Y. Associations between acylcarnitine to free carnitine ratio and adverse prognosis in heart failure patients with reduced or preserved ejection fraction. ESC Heart Fail 2017; 4: 360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fornaro A, Olivotto I, Rigacci L, Ciaccheri M, Tomberli B, Ferrantini C, Coppini R, Girolami F, Mazzarotto F, Chiostri M, Milli M, Marchionni N, Castelli G. Comparison of long‐term outcome in anthracycline‐related versus idiopathic dilated cardiomyopathy: a single centre experience. Eur J Heart Fail 2018; 20: 898–906. [DOI] [PubMed] [Google Scholar]
- 20. Pasco JA, Mohebbi M, Holloway KL, Brennan‐Olsen SL, Hyde NK, Kotowicz MA. Musculoskeletal decline and mortality: prospective data from the Geelong Osteoporosis Study. J Cachexia Sarcopenia Muscle 2017; 8: 482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Martone AM, Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, Di Bari M, Maggio M, Manca GM, Marzetti E, Rizzo MR, Rossi A, Volpato S, Landi F. The incidence of sarcopenia among hospitalized older patients: results from the Glisten study. J Cachexia Sarcopenia Muscle 2017; 8: 907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lancellotti P, Galderisi M, Donal E, Edvardsen T, Popescu BA, Farmakis D, Filippatos G, Habib G, Lestuzzi C, Santoro C, Moonen M, Jerusalem G, Andarala M, Anker SD. Protocol update and preliminary results of EACVI/HFA Cardiac Oncology Toxicity (COT) Registry of the European Society of Cardiology. ESC Cardiac Oncology Toxicity Long‐Term Registry Investigators. ESC Heart Fail 2017; 4: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schwaneberg T, Weitmann K, Dösch A, Seyler C, Bahls T, Geidel L, Stahl D, Lee M, Kraus M, Katus HA, Hoffmann W. Data privacy management and data quality monitoring in the German Centre for Cardiovascular Research's multicentre TranslatiOnal Registry for CardiomyopatHies (DZHK‐TORCH). ESC Heart Fail 2017; 4: 440–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fruhwald F, Lassner D, Fruhwald S, Gross UM, Dapunt O, Schultheiss HP. Immunosuppressive treatment in fulminant myocarditis and gene expression pattern associated with, but no histological confirmation of giant cell myocarditis. ESC Heart Fail 2017; 4: 190–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sotiropoulos K, Yerly P, Monney P, Garnier A, Regamey J, Hugli O, Martin D, Metrich M, Antonietti JP, Hullin R. Red cell distribution width and mortality in acute heart failure patients with preserved and reduced ejection fraction. ESC Heart Fail 2016; 3: 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nishikawa H, Enomoto H, Ishii A, Iwata Y, Miyamoto Y, Ishii N, Yuri Y, Hasegawa K, Nakano C, Nishimura T, Yoh K, Aizawa N, Sakai Y, Ikeda N, Takashima T, Takata R, Iijima H, Nishiguchi S. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J Cachexia Sarcopenia Muscle 2017; 8: 915–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paris MT, Lafleur B, Dubin JA, Mourtzakis M. Development of a bedside viable ultrasound protocol to quantify appendicular lean tissue mass. J Cachexia Sarcopenia Muscle 2017; 8: 713–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Spinar J, Jarkovsky J, Spinarova L, Vitovec J, Linhart A, Widimsky P, Miklik R, Zeman K, Belohlavek J, Malek F, Cihalik C, Spac J, Felsoci M, Ostadal P, Dusek L, Kettner J, Vaclavik J, Littnerova S, Monhart Z, Malek J, Parenica J, AHEAD Registry Investigators . Worse prognosis of real‐world patients with acute heart failure from the Czech AHEAD registry in comparison to patients from the RELAX‐AHF trial. ESC Heart Fail 2017; 4: 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vagnildhaug OM, Blum D, Wilcock A, Fayers P, Strasser F, Baracos VE, Hjermstad MJ, Kaasa S, Laird B, Solheim TS, European Palliative Care Cancer Symptom Study Group . The applicability of a weight loss grading system in cancer cachexia: a longitudinal analysis. J Cachexia Sarcopenia Muscle 2017; 8: 789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rastogi A, Novak E, Platts AE, Mann DL. Epidemiology, pathophysiology and clinical outcomes for heart failure patients with a mid‐range ejection fraction. Eur J Heart Fail 2017; 19: 1597–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Seyler C, Meder B, Weis T, Schwaneberg T, Weitmann K, Hoffmann W, Katus HA, Dösch A. TranslatiOnal Registry for CardiomyopatHies (TORCH)—rationale and first results. ESC Heart Fail 2017; 4: 209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mebazaa A, Motiejunaite J, Gayat E, Crespo‐Leiro MG, Lund LH, Maggioni AP, Chioncel O, Akiyama E, Harjola VP, Seferovic P, Laroche C, Julve MS, Roig E, Ruschitzka F, Filippatos G, ESC Heart Failure Long‐Term Registry Investigators . Long‐term safety of intravenous cardiovascular agents in acute heart failure: results from the European Society of Cardiology Heart Failure Long‐Term Registry. Eur J Heart Fail 2018; 20: 332–341. [DOI] [PubMed] [Google Scholar]
- 33. Nesteruk J, Voronina N, Kundt G, Donndorf P, Klopsch C, Kaminski A, Duckers HJ, Steinhoff G. Stem cell registry programme for patients with ischemic cardiomyopathy undergoing coronary artery bypass grafting: what benefits does it derive? ESC Heart Fail 2017; 4: 105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pose A, Almenar L, Gavira JJ, López‐Granados A, Blasco T, Delgado J, Aramburu O, Rodríguez A, Manzano L, Manito N. Benefit of tolvaptan in the management of hyponatraemia in patients with diuretic‐refractory congestive heart failure: the SEMI‐SEC project. ESC Heart Fail 2017; 4: 130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rooks DS, Laurent D, Praestgaard J, Rasmussen S, Bartlett M, Tankó LB. Effect of bimagrumab on thigh muscle volume and composition in men with casting‐induced atrophy. J Cachexia Sarcopenia Muscle 2017; 8: 727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Loumaye A, de Barsy M, Nachit M, Lause P, van Maanen A, Trefois P, Gruson D, Thissen JP. Circulating activin A predicts survival in cancer patients. J Cachexia Sarcopenia Muscle 2017; 8: 768–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Neefjes ECW, van den Hurk RM, Blauwhoff‐Buskermolen S, van der Vorst MJDL, Becker‐Commissaris A, de van der Schueren MAE, Buffart LM, Verheul HMW. Muscle mass as a target to reduce fatigue in patients with advanced cancer. J Cachexia Sarcopenia Muscle 2017; 8: 623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cardinale D, Ciceri F, Franzosi MG LR, Sandri MT, Civelli M, Cucchi G, Menatii E, Mangiavacchi M, Cavina R, Barbieri E, Gori S, Colombo A, Curigliano G, Salvatici M, Rizzo A, Ghisoni F, Bianchi A, Falci C, Aquilina M, Rocca A, Monopoli A, Milandri C, Rossetti G, Bregni M, Sicuro M, Malossi A, Nassiacos D, Verusio C, Giordano M, Staszewsky L, Barlera S, Nicolis EB, Magnoli M, Masson S, Cipollla CM, ICOS‐ONE Study Investigators . Anthracycline‐induced cardiotoxicity: a multicenter randomized trial comparing two strategies for guiding prevention with enalapril: the International CardioOncology Society‐One trial. Eur J Cancer 2018; 94: 126–137. [DOI] [PubMed] [Google Scholar]
- 39. Cardinale D, Colombo A, Lamantia G, Colombo N, Civelli M, De Giacorni G, Rubino M, Veglia F, Fiorentini C, Cipolla CM. Anthracycline‐induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol 2010; 55: 213–220. [DOI] [PubMed] [Google Scholar]
- 40. Hamo CE, Bloom MW, Cardinale D, Ky B, Nohria A, Baer L, Skopicki H, Lenihan DJ, Gheorghiade M, Lyon AR, Butler J. Cancer therapy‐related cardiac dysfunction and heart failure part 2: prevention, treatment, guidelines, and future directions. Circ Heart Fail 2016; 9: e002843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Banke A, Fosbøl EL, Møller JE, Gislason GH, Andersen M, Bernsdorf M, Jensen MB, Schou M, Ejlertsen B. Long‐term effect of epirubicin on incidence of heart failure in women with breast cancer: insight from a randomized clinical trial. Eur J Heart Fail 2018; 20: 1447–1453. [DOI] [PubMed] [Google Scholar]
- 42. O'Brien ME, Wigler N, Inbar M, Rosso R, Grischke E, Santoro A, Catane R, Kieback DG, Tomczak P, Ackland SP, Orlandi F, Alland L, Tendler C, CAELYX Breast Cancer Study Group . Reduced cardiotoxicity and efficiacy in a phase III trial of pegylated liposomal doxorubicin HCI (CAELYX/Doxil) versus conventional doxorubicin for first‐line treatment of metastatic breast cancer. Ann Oncol 2004; 15: 440–449. [DOI] [PubMed] [Google Scholar]
- 43. De Azambuja E, Procter MJ, van Velduisen DJ, Agbor‐Tarh D, Metzger‐Filho O, Steinseifer J, Untch J, Smith IE, Gianni L, Baselga J, Jackisch C, Cameron DA, Bell R, Leyland‐Jones B, Dowsett M, Gelber RD, Piccart‐Gebhart MJ, Suter TM. Trastuzumab‐associated cardiac events at 8 years of median follow‐up in the Herceptin Adjuvant trial (BIG1‐01). J Klein Oncol 2014; 32: 2159–2165. [DOI] [PubMed] [Google Scholar]
- 44. Pivor X, Romieu G, Debled M, Pierga JY, Kerbrat P, Bachelot T, Lortholary A, Espié M, Fumoleau P, Serin D, Jacquin JP, Jouannaud C, Rios M, Abadie‐Lacourtoisie S, Tubiana‐Mathieru N, Cany S, Khayat D, Pauporté I, Kramar A, PHARE Trial Investigators . 6 months versus 12 months of adjuvant trastuzumab for patients with HER2‐positive early breast cancer (PHARE): a randomised phase 3 trial. Lancet Oncol 2013; 14: 741–748. [DOI] [PubMed] [Google Scholar]
- 45. Triposkiadis F, Giamouzis G, Parissis J, Starling RC, Boudoulas H, Skoularigis J, Butler J, Filippatos G. Reframing the association and significance of co‐morbidities in heart failure. Eur J Heart Fail 2016; 18: 744–758. [DOI] [PubMed] [Google Scholar]
- 46. Konishi M, Ishida J, Springer J, von Haehling S, Akashi YJ, Shimokawa H, Anker SD. Heart failure epidemiology and novel treatments in Japan: facts and numbers. ESC Heart Fail 2016; 3: 145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Núñez J, Monmeneu JV, Mollar A, Núñez E, Bodí V, Miñana G, García‐Blas S, Santas E, Agüero J, Chorro FJ, Sanchis J, López‐Lereu MP. Left ventricular ejection fraction recovery in patients with heart failure treated with intravenous iron: a pilot study. ESC Heart Fail 2016; 3: 293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Theidel U, Väätäinen S, Martikainen J, Soini E, Hardt T, Doehner W. Budget impact of intravenous iron therapy with ferric carboxymaltose in patients with chronic heart failure and iron deficiency in Germany. ESC Heart Fail 2017; 4: 274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Clevenger B, Gurusamy K, Klein AA, Murphy GJ, Anker SD, Richards T. Systematic review and meta‐analysis of iron therapy in anaemic adults without chronic kidney disease: updated and abridged Cochrane review. Eur J Heart Fail 2016; 18: 774–785. [DOI] [PubMed] [Google Scholar]
- 50. Tang YD, Katz SD. Anemia in chronic heart failure: prevalence, etiology, clinical correlates, and treatment options. Circulation 2006; 113: 2454–2461. [DOI] [PubMed] [Google Scholar]
- 51. Parissis J, Nikolaou M, Mebazaa A. The model for end‐stage liver disease score in acute heart failure: hepatorenal dysfunction hides behind. Eur J Heart Fail 2016; 18: 1522–1523. [DOI] [PubMed] [Google Scholar]
- 52. Koyama S, Kuragaichi T, Sato Y, Kuwabara Y, Usami S, Horie T, Baba O, Hakuno D, Nakashima Y, Nishino T, Nishiga M, Nakao T, Arai H, Kimura T, Ono K. Dynamic changes of serum microRNA‐122‐5p through therapeutic courses indicates amelioration of acute liver injury accompanied by acute cardiac decompensation. ESC Heart Fail 2017; 4: 112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ikeda S, Ohshima K, Miyazaki S, Kadota H, Shimizu H, Ogimoto A, Hamada M. Impact of chronic kidney disease on the diuretic response of tolvaptan in acute decompensated heart failure. ESC Heart Fail 2017; 4: 614–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sokolski M, Zymliński R, Biegus J, Siwołowski P, Nawrocka‐Millward S, Todd J, Yerramilli MR, Estis J, Jankowska EA, Banasiak W, Ponikowski P. Urinary levels of novel kidney biomarkers and risk of true worsening renal function and mortality in patients with acute heart failure. Eur J Heart Fail 2017; 19: 760–767. [DOI] [PubMed] [Google Scholar]
- 55. Pietrock C, von Haehling S. Sleep‐disordered breathing in heart failure: facts and numbers. ESC Heart Fail 2017; 4: 198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Savage HO, Khushaba RN, Zaffaroni A, Colefax M, Farrugia S, Schindhelm K, Teschler H, Weinreich G, Grueger H, Neddermann M, Heneghan C, Simonds A, Cowie MR. Development and validation of a novel non‐contact monitor of nocturnal respiration for identifying sleep‐disordered breathing in patients with heart failure. ESC Heart Fail 2016; 3: 212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Staszewsky L, Cortesi L, Tettamanti M, Dal Bo GA, Fortino I, Bortolotti A, Merlino L, Latini R, Roncaglioni MC, Baviera M. Outcomes in patients hospitalized for heart failure and chronic obstructive pulmonary disease: differences in clinical profile and treatment between 2002 and 2009. Eur J Heart Fail 2016; 18: 840–848. [DOI] [PubMed] [Google Scholar]
- 58. Coiro S, Girerd N, Rossignol P, Ferreira JP, Maggioni A, Pitt B, Tritto I, Ambrosio G, Dickstein K, Zannad F. Association of beta‐blocker treatment with mortality following myocardial infarction in patients with chronic obstructive pulmonary disease and heart failure or left ventricular dysfunction: a propensity matched‐cohort analysis from the High‐Risk Myocardial Infarction Database Initiative. Eur J Heart Fail 2017; 19: 271–279. [DOI] [PubMed] [Google Scholar]
- 59. Koutsampasopoulos K, Ziakas A, Vogiatzis I. Sexual function of patients with heart failure: distinct phenotypes, distinct sexual function? ESC Heart Fail 2017; 4: 319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jaarsma T. Sexual function of patients with heart failure: facts and numbers. ESC Heart Fail 2017; 4: 3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. von Haehling S, Anker MS, Anker SD. Prevalence and clinical impact of cachexia in chronic illness in Europe, USA, and Japan: facts and numbers update 2016. J Cachexia Sarcopenia Muscle 2016; 7: 507–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Clark AL, Coats AJS, Krum H, Katus HA, Mohacsi P, Salekin D, Schultz MK, Packer M, Anker SD. Effect of beta‐adrenergic blockade with carvedilol on cachexia in severe chronic heart failure: results from the COPERNICUS trial. J Cachexia Sarcopenia Muscle 2017; 8: 549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sente T, Van Berendoncks AM, Hoymans VY, Vrints CJ. Adiponectin resistance in skeletal muscle: pathophysiological implications in chronic heart failure. J Cachexia Sarcopenia Muscle 2016; 7: 261–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Barazzoni R, Gortan Cappellari G, Palus S, Vinci P, Ruozi G, Zanetti M, Semolic A, Ebner N, von Haehling S, Sinagra G, Giacca M, Springer J. Acylated ghrelin treatment normalizes skeletal muscle mitochondrial oxidative capacity and AKT phosphorylation in rat chronic heart failure. J Cachexia Sarcopenia Muscle 2017; 8: 991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Saitoh M, Dos Santos MR, Emami A, Ishida J, Ebner N, Valentova M, Bekfani T, Sandek A, Lainscak M, Doehner W, Anker SD, von Haehling S. Anorexia, functional capacity, and clinical outcome in patients with chronic heart failure: results from the Studies Investigating Co‐morbidities Aggravating Heart Failure (SICA‐HF). ESC Heart Fail 2017; 4: 448–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Morley JE. Anorexia of ageing: a key component in the pathogenesis of both sarcopenia and cachexia. J Cachexia Sarcopenia Muscle 2017; 8: 523–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Springer J, Tschirner A, Haghikia A, von Haehling S, Lal H, Grzesiak A, Kaschina E, Palus S, Pötsch M, von Websky K, Hocher B, Latouche C, Jaisser F, Morawietz L, Coats AJ, Beadle J, Argiles JM, Thum T, Földes G, Doehner W, Hilfiker‐Kleiner D, Force T, Anker SD. Prevention of liver cancer cachexia‐induced cardiac wasting and heart failure. Eur Heart J 2014; 35: 932–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Versace VL, Berry NM, Chowdhury MH, Ullah S, McCarthy AL, Atherton JJ, Koczwara B, Roder D, Clark RA. Characteristics of patients with haematological and breast cancer (1996–2009) who died of heart failure‐related causes after cancer therapy. ESC Heart Fail 2016; 3: 253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Banke A, Schou M, Videbæk L, Møller JE, Torp‐Pedersen C, Gustafsson F, Dahl JS, Køber L, Hildebrandt PR, Gislason GH. Incidence of cancer in patients with chronic heart failure: a long‐term follow‐up study. Eur J Heart Fail 2016; 18: 260–266. [DOI] [PubMed] [Google Scholar]
- 70. Hasin T, Gerber Y, McNallan SM, Weston SA, Kushwaha SS, Nelson TJ, Cerhan JR, Roger VL. Patients with heart failure have an increased risk of incident cancer. J Am Coll Cardiol 2013; 62: 881–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation 2016; 133: 1104–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ameri P, Canepa M, Anker MS, Belenkov Y, Bergler‐Klein J, Cohen‐Solal A, Farmakis D, López‐Fernández T, Lainscak M, Pudil R, Ruschitska F, Seferovic P, Filippatos G, Coats A, Suter T, Von Haehling S, Ciardiello F, de Boer RA, Lyon AR, Tocchetti CG, Heart Failure Association Cardio‐oncology Study Group of the European Society of Cardiology . Cancer diagnosis in patients with heart failure: epidemiology, clinical implications and gaps in knowledge. Eur J Heart Fail 2018; 20: 879–887. [DOI] [PubMed] [Google Scholar]
- 73. Vaduganathan M, Prasad V. Cardiovascular risk assessment in oncological clinical trials: is there a role for centralized events adjudication? Eur J Heart Fail 2016; 18: 128–132. [DOI] [PubMed] [Google Scholar]
- 74. Meijers WC, Maglione M, Bakker SJL, Oberhuber R, Kieneker LM, de Jong S, Haubner BJ, Nagengast WB, Lyon AR, van der Vegt B, van Veldhuisen DJ, Westenbrink BD, van der Meer P, Silljé HHW, de Boer RA. The failing heart stimulates tumor growth by circulating factors. Circulation 2018; 138: 678–691. [DOI] [PubMed] [Google Scholar]
- 75. Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res 2011; 3: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Nadruz W, West E, Sengeløv M, Grove GL, Santos M, Groarke JD, Forman DE, Claggett B, Skali H, Nohria A, Shah AM. Cardiovascular phenotype and prognosis of patients with heart failure induced by cancer therapy. Heart 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Schäfer M, Oeing CU, Rohm M, Baysal‐Temel E, Lehmann LH, Bauer R, Volz HC, Boutros M, Sohn D, Sticht C, Gretz N, Eichelbaum K, Werner T, Hirt MN, Eschenhagen T, Müller‐Decker K, Strobel O, Hackert T, Krijgsveld J, Katus HA, Berriel Diaz M, Backs J, Herzig S. Ataxin‐10 is part of a cachexokine cocktail triggering cardiac metabolic dysfunction in cancer cachexia. Mol Metab 2015; 5: 67–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Barkhudaryan A, Scherbakov N, Springer J, Doehner W. Cardiac muscle wasting in individuals with cancer cachexia. ESC Heart Fail 2017; 4: 458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Loncar G, Springer J, Anker M, Doehner W, Lainscak M. Cardiac cachexia: hic et nunc. J Cachexia Sarcopenia Muscle 2016; 7: 246–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Pavo N, Raderer M, Hülsmann M, Neuhold S, Adlbrecht C, Strink G, Goliasch G, Gisslinger H, Steger GG, Hejna M, Köstler W, Zöchbauer‐Müller S, Marosi C, Kornek G, Auerbach L, Schneider S, Parschalk B, Scheithauer W, Pirker R, Drach J, Zielinski C, Pacher R. Cardiovascular biomarkers in patients with cancer and their association with all‐cause mortality. Heart 2015; 101: 1874–1880. [DOI] [PubMed] [Google Scholar]
- 81. Cramer L, Hildebrandt B, Kung T, Wichmann K, Springer J, Doehner W, Sandek A, Valentova M, Stojakovic T, Scharnagl H, Riess H, Anker SD, von Haehling S. Cardiovascular function and predictors of exercise capacity in patients with colorectal cancer. J Am Coll Cardiol 2014; 13: 1310–1319. [DOI] [PubMed] [Google Scholar]
- 82. Anker MS, Ebner N, Hildebrandt B, Springer J, Sinn M, Riess H, Anker SD, Landmesser U, Haverkamp W, von Haehling S. Resting heart rate is an independent predictor of death in patients with colorectal, pancreatic, and non‐small cell lung cancer: results of a prospective cardiovascular long‐term study. Eur J Heart Fail 2016; 18: 1524–1534. [DOI] [PubMed] [Google Scholar]
- 83. van Bilsen M, Patel HC, Bauersachs J, Böhm M, Borggrefe M, Brutsaert D, Coats AJS, de Boer RA, de Keulenaer GW, Filippatos GS, Floras J, Grassi G, Jankowska EA, Kornet L, Lunde IG, Maack C, Mahfoud F, Pollesello P, Ponikowski P, Ruschitzka F, Sabbah HN, Schultz HD, Seferovic P, Slart RHJA, Taggart P, Tocchetti CG, Van Laake LW, Zannad F, Heymans S, Lyon AR. The autonomic nervous system as a therapeutic target in heart failure: a scientific position statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2017; 19: 1361–1378. [DOI] [PubMed] [Google Scholar]
- 84. Moslehi JJ. Cardiovascular toxic effects of targeted cancer therapies. N Engl J Med 2016; 375: 1457–1467. [DOI] [PubMed] [Google Scholar]
- 85. Moslehi J, Amgalan D, Kitsis RN. Grounding cardio‐oncology in basic and clinical science. Circulation 2017; 136: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Li M, Sala V, De Santis MC, Cimino J, Cappello P, Pianca N, Di Bona A, Margaria JP, Martini M, Lazzarini E, Pirozzi F, Rossi L, Franco I, Bornbaum J, Heger J, Rohrbach S, Perino A, Tocchetti CG, Lima BHF, Teixeira MM, Porporato PE, Schulz R, Angelini A, Sandri M, Ameri P, Sciarretta S, Lima‐Júnior RCP, Mongillo M, Zaglia T, Morello F, Novelli F, Hirsch E, Ghigo A. Phosphoinositide 3‐kinase gamma inhibition protects from anthracycline cardiotoxicity and reduces tumor growth. Circulation 2018; 138: 696–711. [DOI] [PubMed] [Google Scholar]
- 87. Tocchetti CG, Galdiero MR, Varricchi G. Cardiac toxicity in patients treated with immune checkpoint inhibitors: it is now time for cardio‐immuno‐oncology. J Am Coll Cardiol 2018; 71: 1765–1767. [DOI] [PubMed] [Google Scholar]
- 88. Sysa‐Shah P, Tocchetti CG, Gupta M, Rainer PP, Shen X, Kang BH, Belmonte F, Li J, Xu Y, Guo X, Bedja D, Gao WD, Paolocci N, Rath R, Sawyer DB, Naga Prasad SV, Gabrielson K. Bidirectional cross‐regulation between ErbB2 and β‐adrenergic signalling pathways. Cardiovasc Res 2016; 109: 358–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Mahmood SS, Fradley MG, Cohen JV, Nohria A, Reynolds KL, Heinzerling LM, Sullivan RJ, Damrongwatanasuk R, Chen CL, Gupta D, Kirchberger MC, Awadalla M, Hassan MZO, Moslehi JJ, Shah SP, Ganatra S, Thavendiranathan P, Lawrence DP, Groarke JD, Neilan TG. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol 2018; 71: 1755–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Pokorna Z, Brazdova P, Jirkovsky E, Adamcova M, Mazurova Y, Štěrba M. Study of cardioprotective effects of the ACE inhibitor perindopril against chronic anthracycline cardiotoxicity on dexrazoxane‐validated in vivo model. Poster no. P1309. Eur J Heart Fail 2018; 20: 5–638.29878595 [Google Scholar]
- 91. Bosch X, Rovira M, Sitges M, Domènech A, Ortiz‐Pérez JT, de Caralt TM, Morales‐Ruiz M, Perea RJ, Monzó M, Esteve J. Enalapril and carvedilol for preventing chemotherapy‐induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol 2013; 61: 2355–2362. [DOI] [PubMed] [Google Scholar]
- 92. Gulati G, Heck SL, Ree AH, Hoffmann P, Schulz‐Menger MW, Gravdehaug B, von Knobelsdorff‐Brenkenhoff F, Bratland Am Storas TH, Hagve TA, Rosjo H, Steine K, Geisler J, Omland T. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo‐controlled, double‐blind clinical trial of candesartan and metoprolol. Eur Heart J 2016; 37: 1671–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Jirkovská‐Vávrová A, Roh J, Lenčová‐Popelová O, Jirkovský E, Hrušková K, Potůčková‐Macková E, Jansová H, Hašková P, Martinková P, Eisner T, Kratochvíl M, Šůs J, Macháček M, Vostatková‐Tichotová L, Geršl V, Kalinowski DS, Muller MT, Richardson DR, Vávrová KI, Štěrba M, Šimůnek T. Synthesis and analysis of novel analogues of dexrazoxane and its open‐ring hydrolysis product for protection against anthracycline cardiotoxicity in vitro and in vivo . Toxicol Res 2015; 4: 1098–1114. [Google Scholar]
- 94. Schroeder PE, Hasinoff BB. The doxorubicin‐cardioprotective drug dexrazoxane undergoes metabolism in the rat to its metal ion‐chelating form ADR‐925. Cancer Chemother Pharmacol 2002; 50: 509–513. [DOI] [PubMed] [Google Scholar]
- 95. Jones S, Holmes FA, O'Shaughnessy J, Blum JL, Vukelja SJ, McIntyre KJ, Pippen JE, Bordelon JH, Kirby RL, Sandbach J, William J, Hyman RDA, Mennel RG, Boehm KA, Meyer LAWG, Mackey D, Riedel S, Muss H, Savin MA. Docetaxel with cyclophosphamide is associated with an overall survival benefit compared with doxorubicin and cyclophosphamide: 7‐year follow‐up of US Oncology Research Trial 9735. J Clin Oncol 2009; 27: 1177–1183. [DOI] [PubMed] [Google Scholar]
- 96. Bovelli D, Plataniotis G, Roila F. On behalf of the ESMO Guidelines Working Group; Cardiotoxicity of chemotherapeutic agents and radiotherapy‐related heart disease: ESMO Clinical Practice Guidelines. Ann Oncol 2010; 21:277–282. [DOI] [PubMed] [Google Scholar]
- 97. Armenian SH, Lacchetti C, Lenihan D. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline Summary. J Clin Oncol 2017; 13: 270–275. [DOI] [PubMed] [Google Scholar]
- 98. Van Dalen EC, Caron HN, Dickinson HO, Kremer LCM. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev 2008; Art. No.: CD003917. [DOI] [PubMed] [Google Scholar]
- 99. Avila MS, Ayub‐Ferreira SM, de Barros Wanderley MR Jr, des Dores Cruz F, Goncalves Brandao SM, Rigaud VOC, Higuchi‐Dos‐Santos MH, Hajjar LA, Kalli Filho PM, Sahade M, Ferrari MSM, de Paula Costa RL, Mano MS, Bittencourt Viana Cruz CB, Abduch MC, Lofrano Alves MS, Guimaraes GV, Issa VS, Bittencourt MS, Bocchi EA. Carvedilol for prevention of chemotherapy‐related cardiotoxicity: the CECCY trial. J Am Coll Cardiol 2018; 71: 2281–2290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Cardio‐oncology sessions during ‘Heart Failure and World Congress on Acute Heart Failure 2018’.


