Abstract
Aims
Survival benefit of percutaneous mitral valve repair with the MitraClip over conservative treatment of functional mitral regurgitation (MR) remains unclear. The purpose of this meta‐analysis is to compare survival outcomes of MitraClip with those of medical therapy in patients with functional MR.
Methods and results
A comprehensive literature search of PubMed, MEDLINE, and Google Scholar was conducted including studies evaluating MitraClip vs. medical therapy with multivariate adjustment and with >80% of patients with functional MR. Death from any cause was the primary endpoint, while freedom from readmission was the secondary one, evaluated with random effects. These analyses were performed at study level and at patient level including only functional MR when available, evaluating the effect of MitraClip in different subgroups according to age, ischaemic aetiology, presence of implantable cardioverter defibrillator/cardiac resynchronization therapy, and left ventricular ejection fraction and volumes. We identified six eligible observational studies including 2121 participants who were treated with MitraClip (n = 833) or conservative therapy (n = 1288). Clinical follow‐up was documented at a median of 400 days. At study‐level analysis, MitraClip, when compared with medical therapy (P = 0.005), was associated with significant reduction of death (P = 0.002) and of readmission due to cardiac disease. At patient‐level analysis, including 344 patients, MitraClip confirmed robust survival benefit over medical therapy for all patients with functional MR and among the most important subgroups.
Conclusions
Compared with conservative treatment, MitraClip is associated with a significant survival benefit. Importantly, this superiority is particularly pronounced among patients with functional MR and across all the main subgroups.
Keywords: Mitral regurgitation, MitraClip, Medical therapy, Meta‐analysis
Introduction
Functional mitral regurgitation (MR) is a frequent complication in heart failure patients owing to left ventricular remodelling processes causing papillary muscle dislocation and leaflet tethering, and it is associated with an adverse prognosis.1, 2 Surgical correction for functional MR is controversial with no consistent outcomes for patients in terms of survival and quality of life and reports of suboptimal outcomes and significant perioperative mortality.3, 4 In addition, a large number of patients with functional MR are not referred for surgery, and many other patients are rejected for open‐heart surgery because of a predicted high surgical risk or co‐morbidities.5 Thus, when surgical risk is prohibitive, percutaneous mitral valve repair (PMVR) using the MitraClip system can be considered a valid option for patients with functional MR who remain symptomatic despite optimal medical therapy.6 Recently, several studies have confirmed that MitraClip procedure is safe with sustained improvement of haemodynamic and functional status even in patients with advanced heart failure, but its impact on survival has not been established.7, 8, 9, 10, 11 To date, there are few non‐randomized studies that globally report better survival outcome of PMVR than of conservative treatment in patients with left ventricular dysfunction and functional MR.12, 13, 14, 15, 16, 17
Therefore, we performed a meta‐analysis of observational studies selecting all‐cause mortality as primary outcome, in order to compare PMVR with MitraClip system combined with medical therapy to medical therapy alone for treatment of severe functional mitral regurgitation.
Methods
Search methods and resources
The present research was elaborated according to current guidelines, including the recent Preferred Reporting Items for Systematic Reviews and Meta‐Analyses amendment to the Quality of Reporting of Meta‐analyses statement and recommendations from The Cochrane Collaboration and Meta‐analysis of Observational Studies in Epidemiology.18, 19, 20 Pertinent articles were searched in PubMed, Cochrane, and Google Scholar for the following terms: ‘mitral regurgitation’ and ‘MitraClip’ and ‘medical therapy’. Two reviewers (C. G. and F. D. A.) independently reviewed all papers, with disagreements resolved by consensus. Inclusion criteria were (i) human studies, (ii) studies comparing MitraClip vs. medical therapy, (iii) follow‐up longer than 1 year, (iv) at least 80% of the patients with functional MR, and (v) studies with multivariate adjustment. In the case of duplicate reporting, the manuscript with the largest sample of patients was selected.
Data abstraction
The following data were independently abstracted by two unblinded reviewers (C. G. and F. D. A.) on pre‐specified electronic forms: authors, journal, year of publication, location of the study group, baseline, and procedural features. The corresponding authors of the relevant studies were queried for required quantitative details not in the published manuscripts. When available, only data for patients with functional MR were included.
Endpoints
All‐cause death was the primary endpoint, while re‐hospitalization for cardiac cause was the secondary one. At patient level, subgroup analysis stratified according to age, presence of implantable cardioverter defibrillator/cardiac resynchronization therapy, cardiomyopathy aetiology, left ventricular ejection fraction, and volumes was also performed.
Quality study evaluation
The quality of included studies was independently appraised by two reviewers (C. G. and F. D. A.), with disagreements resolved by consensus. Design of the study (multicentre or not), area of enrolment, and kinds of multivariate analysis were collected.
Statistical analysis
Continuous variables are reported as mean (standard deviation) or median (first and third quartiles). Categorical variables are expressed as n (%). Statistical pooling for incidence estimates was performed according to a random‐effects model with generic inverse‐variance weighting, computing risk estimates with 95% confidence intervals (CIs), using RevMan 5.2 (The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark). Hypothesis testing for superiority was set at the two‐tailed 0.05 level. Hypothesis testing for statistical homogeneity was set at the two‐tailed 0.10 level and based on the Cochran Q test, with I 2 values of 25%, 50%, and 75% representing mild, moderate, and severe heterogeneity, respectively.
Results
Study selection
The flow chart is shown in Figure 1 . The electronic search yielded 351 citations that were initially evaluated for eligibility in title and abstract levels. Once duplicate and irrelevant publications had been removed, six reports were evaluated in full text for eligibility and were finally used in the current meta‐analysis.12, 13, 14, 15, 16, 17 Individual patient data for patient‐level meta‐analysis were collected from three of the included studies.12, 14, 17
Figure 1.
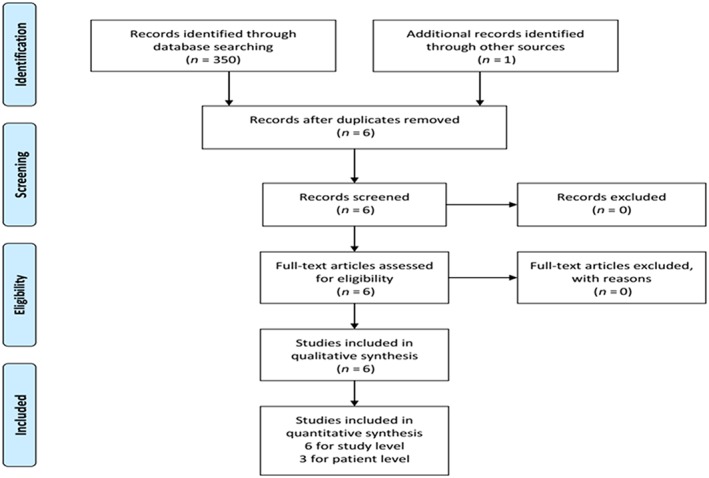
Preferred reporting items for systematic reviews and meta‐analyses chart.
Quality of evidence
No randomized controlled trials comparing MitraClip vs. medical therapy alone were identified. Of the six studies included in the meta‐analysis, four performed prospective enrolment at least in one of the two arms and two included multicentre registries. All studies appraised were from specialized tertiary referral centres. Only one report was published as an abstract.17 With the exception of two studies,16, 17 the other studies included >50 patients in each group of treatment. Four studies exclusively enrolled patients with functional MR14, 15, 17 while the remaining studies included both functional and degenerative MR.12, 13, 16 From the study of Swans et al., only outcome data for functional MR were included. 15 Otherwise, all patients collected for patient‐level meta‐analysis were affected by functional MR. All but one report12 used a propensity score matching in order to minimize imbalance in key baseline characteristics between the MitraClip and medical therapy alone groups. All studies explicitly stated a priori inclusion criteria.
Demographics characteristics
Baseline characteristics of overall population and according to the included different studies are summarized in Tables 1 and 2, respectively. Overall, 2121 participants who were treated with MitraClip (n = 833) or conservative therapy (n = 1288) were included. Patients enrolled were predominantly male (78%) and characterized by advance age (median age 71 years), high estimated surgical risk (median logistic EuroSCORE 21% and median Society of Thoracic Surgeons score 11%) and a high burden of co‐morbidities (i.e. chronic kidney disease 45%, chronic obstructive pulmonary disease 45%, diabetes mellitus 45%, a history of previous myocardial infarction 25%, and percutaneous coronary intervention 49%). Despite optimal medical therapy, all patients were symptomatic for dyspnoea, with 95% in New York Heart Association Class III–IV. The mechanism of MR was functional in 93% of patients with 67% of ischaemic aetiology. With the exception of one report, the patients' baseline characteristics were well matched between the two treatment groups in all studies.12
Table 1.
Baseline clinical profile of included patients (for study level, all data are reported as continuous or percentages with median and first and third inter‐quartiles; for patient level, as median or percentages)
| Characteristics |
Study‐level cohort (n = 2121) |
Patient‐level cohort (n = 344) |
|---|---|---|
| Age, years | 71 (65–82) | 74 (67–80) |
| Male gender | 78 (72–81) | 81 (67–88) |
| Body mass index, kg/m2 | 23 (22–29) | 25 (23–27) |
| Logistic EuroSCORE, % | 21 (18–23) | 22 (20–24) |
| STS score, % | 11 (8–12) | 12 (9–13) |
| Previous smoker | 28 (23–45) | 33 |
| Hypertension | 36 (32–45) | 40 |
| Hyperlipidaemia | 37 (32–43) | 33 |
| Diabetes mellitus | 45 (43–56) | 39 |
| Atrial fibrillation | 45 (43–65) | 49 |
| Chronic obstructive pulmonary disease | 45 (43–90) | 72 |
| Chronic kidney disease | 45 (43–64) | 50 |
| Dialysis | 9 (2–7) | 8 |
| Coronary artery disease | 67 (64–71) | 71 (69–81) |
| Previous myocardial infarction | 25 (24–38) | 29 |
| Previous percutaneous coronary intervention | 49 (43–54) | 54 |
| Ischaemic heart disease | 67 (64–81) | 70 (68–74) |
| Functional mitral regurgitation | 93 (91–97) | 100 |
| History of acute pulmonary oedema | 17 (12–20) | 13 |
| NYHA Class III–IV | 95 (90–97) | 91 (89–96) |
| ICD/CRT | — | 74 |
| ICD | — | 88 |
CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; NYHA, New York Heart Association; STS, Society of Thoracic Surgeons: predicted risk of operative mortality.
Table 2.
Baseline clinical profile of enrolled patients according to different studies included in the meta‐analysis
| Study | Number of patients | Functional MR | Age (years) | Male gender | STS score (%) | Logistic score (%) | Chronic kidney disease | Coronary artery disease | Chronic obstructive pulmonary disease | Atrial fibrillation | NYHA Class III–IV |
LV ejection fraction (%) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | PMVR | MT | |
| Swaans et al.12 | 139 | 59 | 92 | 93 | 76 ± 10 | 73 ± 10 | 68 | 54 | 13.5 ± 9 | 4.34 ± 4 | 23.9 ± 16 | 18.7 ± 13.2 | 40 | 31 | 51 | 76 | 22 | 32 | 52 | 41 | 88 | 86 | 37 ± 15 | 34 ± 17 |
| Velázquez et al.13 | 351 | 953 | 70 | 93 | 76 ± 11 | 69 ± 13 | 61 | 49 | 11.3 ± 7.7 | 9.7 ± 8.8 | — | — | 31 | 19 | 51 | 43 | 11 | 7 | 69 | 52 | 85 | 47 | 48 ± 14 | 37 ± 11 |
| Adamo et al.17 | 33 | 33 | 100 | 100 | 71 ± 9 | 71 ± 12 | 70 | 67 | — | — | — | — | 61 | 58 | 42 | 36 | 24 | 27 | 48 | 55 | 100 | 100 | 30 ± 9 | 30 ± 8 |
| Giannini et al.14 | 60 | 60 | 100 | 100 | 75 ± 8 | 76 ± 8 | 70 | 63 | 4.9 ± 4.2 | 3.8 ± 2.6 | 21.1 ± 14 | 20.9 ± 12.6 | 48 | 33 | 43 | 28 | 25 | 20 | 35 | 43 | 73 | 75 | 37 ± 15 | 35 ± 11 |
| Armeni et al.15 | 232 | 151 | 100 | 100 | 71 ± 10 | 71 ± 11 | 73 | 74 | — | — | — | — | — | — | 64 | 54 | 25 | 21 | 33 | 33 | — | — | 34 ± 13 | 32 ± 10 |
| Asgar et al.16 | 50 | 42 | 100 | 100 | 75 ± 9 | 68 ± 16 | 74 | 77 | — | — | — | — | — | — | 78 | 71 | — | — | 58 | 64 | 98 | 21 | 38 ± 16 | 32 ± 14 |
Values are mean ± SD or %.
LV, left ventricle; MR, mitral regurgitation; MT, medical therapy; NYHA, New York Heart Association; PMVR, percutaneous mitral valve repair with MitraClip.
In order to compare the effect of MitraClip with that of medical therapy among patients with functional MR only, we performed a meta‐analysis using individual participant data. Data from 344 patients with functional MR were collected for individual patient data analysis and matched after propensity score: 172 (50%) were treated with MitraClip and 172 (50%) conservatively. All reported baseline clinical characteristics of the individual patient‐level data cohort were similar to those of the overall cohort (Table 1). Baseline echocardiographic parameters are detailed in Table 3. The overall study population showed a severely impaired left ventricular systolic function with a median ejection fraction of 24% (23–36%). Individual patient data meta‐analysis further confirmed left ventricular systolic dysfunction with severely dilated left ventricle and atrial chambers and increased systolic pulmonary artery pressure (Table 3).
Table 3.
Baseline echocardiographic profile (for study level, all data are reported as continuous or percentages with median and first and third inter‐quartiles; for patient level, as median or percentages)
| Parameters | Study‐level cohort (n = 2121) | Patient‐level cohort (n = 344) |
|---|---|---|
| LV end‐diastolic volume, mL | — | 187 (148–224) |
| LV end‐diastolic volume > 200 ml | — | 20 |
| LV ejection fraction, % | 24 (23–36) | 30 (25–38) |
| LV ejection fraction < 25% | — | 33 |
| LA area, cm2 | — | 30 (25–35) |
| SPAP, mmHg | — | 47 (40–55) |
| SPAP > 60 mmHg | — | 30 |
LA, left atrium; LV, left ventricle; SPAP, systolic pulmonary artery pressure.
MitraClip procedure and in‐hospital outcome
Procedural results and in‐hospital adverse events are defined in Table 4. Overall procedural time, defined as the time from trans‐septal access with the guide catheter to guide removal from the vein, was 140 min. There was no procedural mortality or clip embolization. Profuse bleeding that required multiple transfusions were 13% (9–20%), whereas the incidence of new onset of atrial fibrillation occurred in 1% (0.5–4%). According to individual patient data, acute procedural success rate was 93%, with only two patients in whom it was not possible to implant a clip. In 61% of cases, a single clip was implanted; in 36% two clips; and in 3% three clips. Stroke, pericardial tamponade, myocardial infarction, and urgent cardiovascular surgery for adverse events were not observed. Vascular complication occurred in 20% while the incidence of acute renal failure was very low (1%). Pre‐discharge echocardiography showed a residual MR > 2 grade in 12% of patients.
Table 4.
Procedural results and in‐hospital outcomes in MitraClip patients (for study level, all data are reported as continuous or percentages with median and first and third inter‐quartiles; for patient level, as median or percentages)
| Characteristics | Study‐level cohort (n = 2121) | Patient‐level cohort (n = 344) |
|---|---|---|
| Number of clip | ||
| 1 | — | 61 |
| 2 | — | 36 |
| 3 | — | 3 |
| Procedural mortality | 0 | 0 |
| Procedural time, min | 140 (118–180) | 140 (118–180) |
| Pericardial tamponade | — | 0 |
| Urgent cardiovascular surgery | — | 0 |
| Vascular complication | — | 21 |
| Bleeding requiring transfusion | 13 (9–20) | 7 |
| Stroke | — | 0 |
| New onset of atrial fibrillation | 1 (0.5–4) | 2 |
| Acute renal failure | 1 | |
| Myocardial infarction | — | 0 |
| Clip embolization | 0 | 0 |
| MR grade at discharge | ||
| 1+/2+ | 80 (78–82) | 88 (87–91) |
| 3+ | 19 (18–23) | 12 (8–13) |
| 4+ | 1 (0–1) | 0 |
MR, mitral regurgitation.
Survival outcomes
Clinical follow‐up was documented at a median of 400 days (376 to 480). There was a total of 133 all‐cause mortality: 52 (30%) in the PMVR arm and 81 (47%) in the conservative group (P < 0.001). The summary estimate comparing PMVR using MitraClip System combined with medical therapy and medical therapy alone showed a statistically significant relative risk reduction of death from any cause in favour of PMVR with homogeneity across reports [odds ratio (OR) 0.79, 95% CI: 0.68–0.92, P = 0.002; I 2 = 96%; τ 2 = 0.03] (Figure 2 A). Through the follow‐up period, heart failure re‐hospitalization data were reported in three studies: 26 (48%) patients in the PMVR arm and 47 (60%) patients in the conservative group (P = 0.02). Overall, a significant difference in survival free from readmission due to cardiac disease favouring MitraClip over medical therapy alone was observed with homogeneity across reports (OR 0.73, 95% CI: 0.59–0.91, P = 0.005; I 2 = 89%; τ 2 = 0.03) (Figure 2 (B)).
Figure 2.
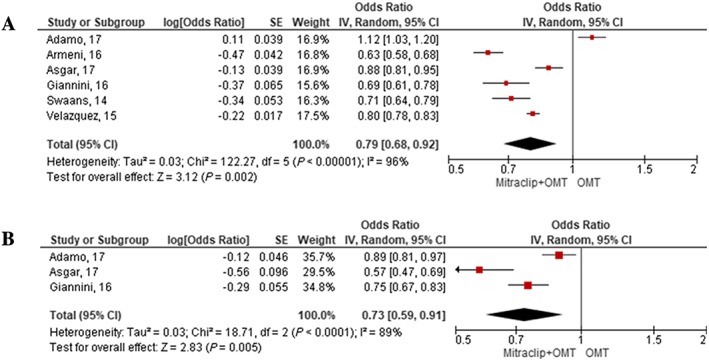
Random‐effects meta‐analysis of percutaneous mitral valve repair vs. conservative therapy for study‐level analysis. Forest plot showing the result of meta‐analysis of percutaneous mitral valve repair vs. conservative therapy for the primary outcome of death from any causes (A) and for the secondary outcome of re‐hospitalization (B) after a median follow‐up of 400 days (376 to 480). The estimate of the odds ratio (OR) of each study corresponds to the middle of the squares, and the horizontal line shows the 95% confidence interval (CI). For each subgroup, the sum of the statistics, along with the summary OR, is represented by the middle of the solid diamonds. A test of heterogeneity between the trials within a subgroup is given below the summary statistics. OMT, optimal medical therapy; IV, instrumental variable estimation; SE, standard error.
Subgroup analysis
Subgroup analysis was available only for individual patient data (344 participants with functional MR). After a median follow‐up of 304 days (172 to 725), there was evidence of survival benefit for MitraClip in patients with functional MR and among all the main subgroups (Figure 3 A). The effect in favour of MitraClip was also confirmed for the secondary outcome of re‐hospitalization across all subgroups except for patients with ischaemic aetiology and those with both left ventricle end‐diastolic volume < 200 and >200 mL (Figure 3 B).
Figure 3.
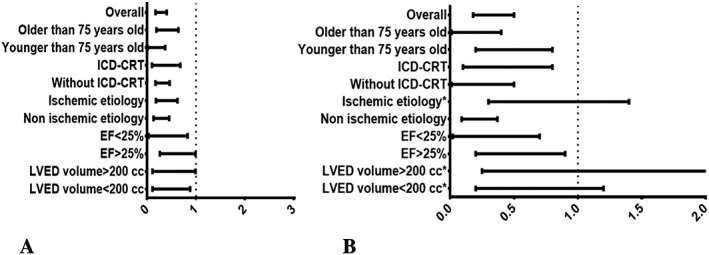
Subgroup analyses from individual patient‐level data for the primary outcome of death from any causes (A) and for the secondary outcome of re‐hospitalization (B) after a median follow‐up of 304 days (172 to 725). Odds ratio (OR) and corresponding confidence intervals for patients subgroups were pooled, and interactions were evaluated by random‐effects meta‐analyses. The vertical dashed line on plot represents the point estimate of OR = 1. Asterisk indicates no significant difference. ICD, implantable cardioverter defibrillator; CRT, cardiac resynchronization therapy; EF, ejection fraction; LVED, left ventricle end‐diastolic.
Discussion
The current meta‐analysis represents an attempt to assess the outcomes of PMVR vs. conservative therapy in patients with heart failure and severe MR.
The main novel findings of this meta‐analysis are summarized as follows:
Compared with medical therapy alone, PMVR with MitraClip resulted in a significant relative risk reduction of death from any cause in high‐risk patients with predominantly functional MR and advanced heart failure.
Mortality benefits with PMVR over medical therapy were confirmed in patients who only had functional MR and were consistent across all the main subgroups.
An overall marked reduction in hospital readmission for cardiovascular disease favouring MitraClip was also observed.
The effect in favour of MitraClip for re‐hospitalization was also consistent in patients with functional MR only and among all subgroups except for patients with ischaemic aetiology and those with both left ventricle end‐diastolic volume < 200 and >200 mL.
Functional MR is associated with a poor prognosis in heart failure patients with post‐ischaemic or idiopathic dilated cardiomyopathy.1 The presence of even mild degrees of functional MR identifies patients with left ventricular dysfunction who have a higher mortality risk than those without MR.2 The appropriateness of mitral valve surgery for patients with functional MR remains embroiled in controversy, because functional MR is the consequence and not the cause of left ventricular dysfunction.6, 21 Moreover, surgical mitral valve repair for functional MR is associated with not negligible perioperative mortality, and the number of patients with severe functional MR who are not referred for surgery because of high surgical risk, advanced age, and co‐morbidities is increasing.4, 5 The introduction of PMVR with the MitraClip device opened new perspectives for the treatment of patients with severe MR at very high surgical risk.7 Although less effective than surgery in reducing MR, the MitraClip showed fewer perioperative adverse events and achieved a similar durable improvement in functional MR.9, 22 A number of studies have compared the outcomes of MitraClip with those of surgical repair reporting similar survival rates.12, 23, 24 However, these findings should be interpreted with caution, because of higher risk profiles (higher age, lower ejection fraction, and higher predicted mortality) in the MitraClip group than in the surgical repair one. In particular, MitraClip implantation has been shown as an effective adjunctive therapy for patients with advanced heart failure and severe functional MR, offering the chance to obtain a relevant reverse cardiac remodelling and significant improvement in functional class even in highly symptomatic patients with severely dilated hearts.7, 25
What remains unknown is whether the PMVR with MitraClip device improves survival in patients with moderate to severe left ventricular failure causing functional MR. Up to now, there are few non‐randomized studies that globally report better survival outcome of PMVR compared with optimal medical therapy in patients with severe MR.12, 13, 15, 16 However, most of these studies include a wide spectrum of high‐risk patients with both functional and degenerative MR. Recently, we evaluated clinical outcome of patients with functional MR and reduced left ventricular function treated conservatively compared with those who received MitraClip device.14 After propensity analysis, we proved that transcatheter mitral valve repair was superior over conservative treatment. Overall survival rates were 89.7%, 61.4%, and 71.2% at 1, 2, and 3 years in the PMVR groups vs. 64.3%, 51.7%, and 34.9% at 1, 2, and 3 years in the conservative group, respectively (P = 0.007).
Therefore, we performed the current meta‐analysis of existing studies to confirm these findings. Six observational reports and >2121 participants with predominantly functional MR (93%) and high surgical risk were included. Our results highlight the worse outcomes of medically managed patients affected by severe MR and the better survival benefit of those treated with endovascular repair (P = 0.03). Furthermore, we performed a meta‐analysis using individual participant data to clarify the effect of MitraClip vs. medical therapy in patients with only functional MR. Patient‐level analysis confirmed that MitraClip therapy is superior to conservative treatment even in patients with functional MR and advanced heart failure and across all the main subgroups.
In particular, in the cohort of patients with functional MR, mortality benefit with PMVR over medical therapy is independent of age, ischaemic aetiology, presence of implantable cardioverter defibrillator/cardiac resynchronization therapy, and left ventricular ejection fraction and volumes. These finding are in contrast with those of a previous study that reported an increased risk of all‐cause death after MitraClip in patients presenting an ischaemic aetiology or those with severely dilated left ventricle.26 However, this study presents several limitations because it included a wide spectrum of high‐risk patients with both functional and degenerative MR. Recently, the results from Transcatheter Valve Treatment Sentinel Pilot Registry, including 452 patients with functional MR who underwent MitraClip procedure in 25 centres across Europe, confirmed our results, reporting no significant differences between the two aetiologies (ischaemic or non‐ischaemic) regarding survival at 1 year follow‐up.27
However, patients with advanced heart failure still have a poor prognosis despite MitraClip implantation. This could be related to advanced stage of evolution of their disease and may inspire researchers to analyse clinical predictors of futility of the MitraClip because of the relevant clinical and economic issues.23, 28, 29 Recent evidences have identified severe right ventricular failure as an independent predictor of cardiovascular mortality in patients with functional MR and advanced heart failure undergoing MitraClip treatment.28, 29
Finally, we reported that patients treated with PMVR experienced a lower incidence of readmission due to cardiac disease than did patients treated conservatively (P = 0.03). These results are comparable with the data from Lim et al. showing a decrease in re‐hospitalization in prohibitive‐surgical‐risk patients after MitraClip implantation.30 Transcatheter reduction of MR in these patients translated to significant benefits, including improvements in symptoms and functional status, favourable left ventricle remodelling, and consequently a decrease in hospitalizations.
Interestingly, we proved that the effect in favour of MitraClip for the secondary outcome of re‐hospitalization was robust across all subgroups except for patients with ischaemic aetiology. Our results are consistent with the data reported by Capodanno et al. showing a significant worsening in terms of re‐hospitalization in patients presenting with an ischaemic aetiology at 2 years' follow‐up.26 These findings suggest that an ischaemic setting potentially represents a more challenging scenario for percutaneous treatment of MR, stressing the importance of patient selection.
However, to investigate whether PMVR has superior survival benefit over conservative therapy in high‐surgical‐risk patients with functional MR, we need results from randomized clinical trials. The ongoing COAPT (Clinical Outcomes Assessment of the MitraClip Percutaneous Therapy for High Surgical Risk Patients) and MITRA FR (Multicentre Study of Percutaneous Mitral Valve Repair MiraClip Device in Patients with Severe Secondary Mitral Regurgitation) studies will provide important additional evidence.
Conclusions
The late outcome of MitraClip compared with medical therapy alone is crucial as the number of MitraClip continues to increase over the last few years. The current meta‐analysis shows that MitraClip is a safe therapeutic option for selected high‐surgical‐risk patients with severe functional mitral regurgitation and entails better survival outcomes than do conservative treatment. The hypothesis that transcatheter mitral valve repair has superior survival benefits vs. conservative therapy in high‐surgical‐risk patients with left ventricular dysfunction and functional MR needs to be tested with randomized clinical trials, and results from the ongoing clinical trials (COAPT and MITRA FR) will be helpful in this setting.
Study limitations
The present study has many limitations. First of all, no randomized trials were included in the meta‐analysis but only observational studies owing to the lack of publications comparing PMVR with conservative treatment. Second, meta‐regression analysis results should be read as hypothesis generating only, which need to be confirmed in larger studies. Third, one study included patients from a non‐published report but simply from abstract.17 Finally, clinical heterogeneity may derive from different selections of population in each centre: Actually, this innovative technique is reserved to patients at different stages of heart failure. In all but one report,12 a propensity score matching was used to minimize imbalance in key baseline characteristics between the MitraClip and medical therapy groups.
Conflict of interest
All authors have no conflict of interest except for Dr Swaans, Prof Petronio, Dr Velazquez, and Dr D'ascenzo, who are consultant for Abbott Vascular or received research grants from Abbott Vascular.
Giannini, C. , D'ascenzo, F. , Fiorelli, F. , Spontoni, P. , Swaans, M. J. , Velazquez, E. J. , Armeni, P. , Adamo, M. , De Carlo, M. , and Petronio, A. S. (2018) A meta‐analysis of MitraClip combined with medical therapy vs. medical therapy alone for treatment of mitral regurgitation in heart failure patients. ESC Heart Failure, 5: 1150–1158. 10.1002/ehf2.12339.
References
- 1. Grigioni F, Enriquez‐Sarano M, Zehr KJ, Bailey KR, Tajik AJ. Ischemic mitral regurgitation: long‐term outcome and prognostic implications with quantitative Doppler assessment. Circulation 2001; 103: 1759–1764. [DOI] [PubMed] [Google Scholar]
- 2. Enriquez‐Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet 2009; 373: 1382–1394. [DOI] [PubMed] [Google Scholar]
- 3. Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, Group ESD . 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017; 38: 2739–2791. [DOI] [PubMed] [Google Scholar]
- 4. Di Salvo TG, Acker MA, Dec GW, Byrne JG. Mitral valve surgery in advanced heart failure. J Am Coll Cardiol 2010; 55: 271–282. [DOI] [PubMed] [Google Scholar]
- 5. Mirabel M, Iung B, Baron G, Messika‐Zeitoun D, Détaint D, Vanoverschelde JL, Butchart EG, Ravaud P, Vahanian A. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J 2007; 28: 1358–1365. [DOI] [PubMed] [Google Scholar]
- 6. Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón‐Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M, ESC Committee for Practice Guidelines (CPG) , Bax JJ, Helmut Baumgartner , Ceconi C, Dean V, Deaton C, Fagard R, Funck‐Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Ž, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Document Reviewers :, Popescu BA, Von Segesser L, Badano LP, Bunc M, Claeys MJ, Drinkovic N, Filippatos G, Habib G, Kappetein AP, Kassab R, Lip GY, Moat N, Nickenig G, Otto CM, Pepper J, Piazza N, Pieper PG, Rosenhek R, Shuka N, Schwammenthal E, Schwitter J, Tornos Mas P, Trindade PT, Walther T. Guidelines on the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio‐Thoracic Surgery (EACTS) (version 2012). Eur Heart J 2012; 33: 2451–2496.22922415 [Google Scholar]
- 7. Franzen O, van der Heyden J, Baldus S, Schlüter M, Schillinger W, Butter C, Hoffmann R, Corti R, Pedrazzini G, Swaans MJ, Neuss M, Rudolph V, Sürder D, Grünenfelder J, Eulenburg C, Reichenspurner H, Meinertz T, Auricchio A. MitraClip® therapy in patients with end‐stage systolic heart failure. Eur J Heart Fail 2011; 13: 569–576. [DOI] [PubMed] [Google Scholar]
- 8. Whitlow PL, Feldman T, Pedersen WR, Lim DS, Kipperman R, Smalling R, Bajwa T, Herrmann HC, Lasala J, Maddux JT, Tuzcu M, Kapadia S, Trento A, Siegel RJ, Foster E, Glower D, Mauri L, Kar S, Investigators EI. Acute and 12‐month results with catheter‐based mitral valve leaflet repair: the EVEREST II (Endovascular Valve Edge‐to‐Edge Repair) High Risk Study. J Am Coll Cardiol 2012; 59: 130–139. [DOI] [PubMed] [Google Scholar]
- 9. Glower DD, Kar S, Trento A, Lim DS, Bajwa T, Quesada R, Whitlow PL, Rinaldi MJ, Grayburn P, Mack MJ, Mauri L, McCarthy PM, Feldman T. Percutaneous mitral valve repair for mitral regurgitation in high‐risk patients: results of the EVEREST II study. J Am Coll Cardiol 2014; 64: 172–181. [DOI] [PubMed] [Google Scholar]
- 10. D'ascenzo F, Moretti C, Marra WG, Montefusco A, Omede P, Taha S, Castagno D, Gaemperli O, Taramasso M, Frea S, Pidello S, Rudolph V, Franzen O, Braun D, Giannini C, Ince H, Perl L, Zoccai G, Marra S, D'Amico M, Maisano F, Rinaldi M, Gaita F. Meta‐analysis of the usefulness of MitraClip in patients with functional mitral regurgitation. Am J Cardiol 2015; 116: 325–331. [DOI] [PubMed] [Google Scholar]
- 11. Rudolph V, Huntgeburth M, von Bardeleben RS, Boekstegers P, Lubos E, Schillinger W, Ouarrak T, Eggebrecht H, Butter C, Plicht B, May A, Franzen O, Schofer J, Senges J, Baldus S. Clinical outcome of critically ill, not fully recompensated, patients undergoing MitraClip therapy. Eur J Heart Fail 2014; 16: 1223–1229. [DOI] [PubMed] [Google Scholar]
- 12. Swaans MJ, Bakker AL, Alipour A, Post MC, Kelder JC, de Kroon TL, Eefting FD, Rensing BJ, Van der Heyden JA. Survival of transcatheter mitral valve repair compared with surgical and conservative treatment in high‐surgical‐risk patients. JACC Cardiovasc Interv 2014; 7: 875–881. [DOI] [PubMed] [Google Scholar]
- 13. Velazquez EJ, Samad Z, Al‐Khalidi HR, Sangli C, Grayburn PA, Massaro JM, Stevens SR, Feldman TE, Krucoff MW. The MitraClip and survival in patients with mitral regurgitation at high risk for surgery: a propensity‐matched comparison. Am Heart J 2015; 170: 1050–1059.e3. [DOI] [PubMed] [Google Scholar]
- 14. Giannini C, Fiorelli F, De Carlo M, Guarracino F, Faggioni M, Giordano P, Spontoni P, Pieroni A, Petronio AS. Comparison of percutaneous mitral valve repair versus conservative treatment in severe functional mitral regurgitation. Am J Cardiol 2016; 117: 271–277. [DOI] [PubMed] [Google Scholar]
- 15. Armeni P, Boscolo PR, Tarricone R, Capodanno D, Maggioni AP, Grasso C, Tamburino C, Maisano F. Real‐world cost effectiveness of MitraClip combined with medical therapy versus medical therapy alone in patients with moderate or severe mitral regurgitation. Int J Cardiol 2016; 209: 153–160. [DOI] [PubMed] [Google Scholar]
- 16. Asgar AW, Khairy P, Guertin MC, Cournoyer D, Ducharme A, Bonan R, Basmadjian A, Tardif JC, Cohen DJ. Clinical outcomes and economic impact of transcatheter mitral leaflet repair in heart failure patients. J Med Econ 2017; 20: 82–90. [DOI] [PubMed] [Google Scholar]
- 17. Adamo Marianna, Curello Salvatore, Carubelli Valentina, Chiari Ermanna, Chizzola Giuliano, Fiorina Claudia, Lombardi Carlo, Locantore Elisa, Pezzotti Elena, Branca Luca, Quinzani Filippo, Metra Marco, Ettori F. MitraClip versus optimal medical therapy for patients with advanced heart failure and severe mitral regurgitation: a propensity‐score matched analysis. Milan, Italy: JIM; 2017. [Google Scholar]
- 18. S HJG . Cochrane Handbook for Systematic Reviews of Interventions; version 5.0.2 In: The Cochrane Collaboration; 2009; 2009. [Google Scholar]
- 19. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta‐analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta‐analyses. Lancet 1999; 354: 1896–1900. [DOI] [PubMed] [Google Scholar]
- 20. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 21. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM, Thomas JD, Members AATF. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129: e521–e643. [DOI] [PubMed] [Google Scholar]
- 22. Feldman T, Foster E, Glower DD, Glower DG, Kar S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L, Investigators EI. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011; 364: 1395–1406. [DOI] [PubMed] [Google Scholar]
- 23. Taramasso M, Denti P, Buzzatti N, De Bonis M, La Canna G, Colombo A, Alfieri O, Maisano F. MitraClip therapy and surgical mitral repair in patients with moderate to severe left ventricular failure causing functional mitral regurgitation: a single‐centre experience. Eur J Cardiothorac Surg 2012; 42: 920–926. [DOI] [PubMed] [Google Scholar]
- 24. Wan B, Rahnavardi M, Tian DH, Phan K, Munkholm‐Larsen S, Bannon PG, Yan TD. A meta‐analysis of MitraClip system versus surgery for treatment of severe mitral regurgitation. Ann Cardiothorac Surg 2013; 2: 683–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Giannini C, Petronio AS, De Carlo M, Guarracino F, Conte L, Fiorelli F, Pieroni A, Di Bello V. Integrated reverse left and right ventricular remodelling after MitraClip implantation in functional mitral regurgitation: an echocardiographic study. Eur Heart J Cardiovasc Imaging 2014; 15: 95–103. [DOI] [PubMed] [Google Scholar]
- 26. Capodanno D, Adamo M, Barbanti M, Giannini C, Laudisa ML, Cannata S, Curello S, Immè S, Maffeo D, Bedogni F, Petronio AS, Ettori F, Tamburino C, Grasso C, Investigators G‐I. Predictors of clinical outcomes after edge‐to‐edge percutaneous mitral valve repair. Am Heart J 2015; 170: 187–195. [DOI] [PubMed] [Google Scholar]
- 27. Pighi M, Estevez‐Loureiro R, Maisano F, Ussia GP, Dall'Ara G, Franzen O, Laroche C, Settergren M, Winter R, Nickenig G, Gilard M, Di Mario C; Transcatheter Valve Treatment Sentinel Registry (TCVT) Investigators of the EURObservational Research Programme (EORP) of the European Society of Cardiology. Immediate and 12‐month outcomes of ischemic versus nonischemic functional mitral regurgitation in patients treated with MitraClip (from the 2011 to 2012 Pilot Sentinel Registry of Percutaneous Edge‐To‐Edge Mitral Valve Repair of the European Society of Cardiology). Am J Cardiol 2017; 119: 630–637. [DOI] [PubMed] [Google Scholar]
- 28. Neuss M, Schau T, Schoepp M, Seifert M, Hölschermann F, Meyhöfer J, Butter C. Patient selection criteria and midterm clinical outcome for MitraClip therapy in patients with severe mitral regurgitation and severe congestive heart failure. Eur J Heart Fail 2013; 15: 786–795. [DOI] [PubMed] [Google Scholar]
- 29. Giannini C, Fiorelli F, Colombo A, De Carlo M, Weisz SH, Agricola E, Godino C, Castriota F, Golino P, Petronio AS. Right ventricular evaluation to improve survival outcome in patients with severe functional mitral regurgitation and advanced heart failure undergoing MitraClip therapy. Int J Cardiol 2016; 223: 574–580. [DOI] [PubMed] [Google Scholar]
- 30. Lim DS, Reynolds MR, Feldman T, Kar S, Herrmann HC, Wang A, Whitlow PL, Gray WA, Grayburn P, Mack MJ, Glower DD. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol 2014; 64: 182–192. [DOI] [PubMed] [Google Scholar]


