Abstract
Objective:
Cardiovascular diseases (CVD) are the main cause of death worldwide and despite a higher prevalence in men, mortality from CVD is higher among women. Few studies have assessed sex differences in chest pain management in ambulatory care. The objective of this post hoc analysis of data from a prospective cohort study was to assess sex differences in the management of chest pain in ambulatory care.
Setting:
We used data from the Thoracic Pain in Community cohort study that was realized in 58 primary care practices and one university ambulatory clinic in Switzerland.
Participants:
In total, 672 consecutive patients aged over 16 years attending a primary care practice or ambulatory care clinic with a complaint of chest pain were included between February and June 2001. Their mean age was 55.2 years and 52.5% were women.
Main outcome measures:
The main outcome was the proportion of patients referred to a cardiologist at 12 months follow-up. A panel of primary care physicians assessed the final diagnosis retained for chest pain at 12 months.
Results:
The prevalence of chest pain of cardiovascular origin (n = 108, 16.1%) was similar for men and women (17.5% vs 14.8%, respectively, p = 0.4). Men with chest pain were 2.5 times more likely to be referred to a cardiologist than women (16.6% vs 7.4%, odds ratio: 2.49, 95% confidence interval: 1.52–4.09). After adjustment for the patients’ age and cardiovascular disease risk factors, the estimates did not significantly change (odds ratio: 2.30, 95% confidence interval: 1.30–3.78).
Conclusion:
Although the same proportion of women and men present with a chest pain of cardiovascular origin in ambulatory care, there is a strong sex bias in their management. These data suggest that effort must be made to assure equity between men and women in medical care.
Keywords: ambulatory care, chest pain, sex differences, sex/gender bias
Introduction
Cardiovascular diseases are the main cause of death in both men and women.1 Despite a higher prevalence of cardiovascular disease in men below 75 years old, the global cardiovascular mortality is higher in women.1,2 Some explanations are given by the fact that women are older when an ischemic event occurs and have more comorbidities.3,4 Furthermore, women’s symptoms are more often described as «atypical», which may lead to under-appreciation of the situation’s severity and misdiagnosis or late diagnosis.
Chest pain is a common complaint in ambulatory care. It can be caused by a wide range of diseases like coronary heart disease, musculoskeletal disorders, gastro-intestinal diseases, respiratory diseases, or mental disorders. Many studies focused on the management of chest pain in the emergency department. In an acute context at the hospital, some studies have shown sex differences in the presentation and management of acute coronary syndrome. For example, women were more likely to have delayed presentation and presented more frequently with unstable angina and non-ST-segment elevation and without chest pain.5,6 Also, women were less likely to receive investigations such as cardiac catheterizations and stress tests compared to men.7,8
Only few studies looked at the evaluation and management of chest pain by primary care physicians (PCPs). A meta-analysis pooling data from five studies, including the Thoracic Pain in Community (TOPIC) study was recently published by the International Working Group on Chest Pain in Primary Care (INTERCHEST).9 The objective was to create a prediction rule for coronary artery disease for patients presenting with chest pain in primary care. Sex was not included in the score. However, there is increasing evidence that women in ambulatory care are investigated less intensively for coronary heart disease and are treated less aggressively than men when presenting with similar symptoms.10
The aim of this study is to assess sex differences in the management of chest pain in ambulatory care. We examined whether sex/gender bias exists in initial and subsequent management of chest pain by PCPs in ambulatory care.
Methods
Study design
We performed post hoc sub-analyses of data from the TOPIC study (Thoracic Pain in Community), a cohort study following patients presenting with a chest pain in ambulatory care. The study has been described in detail elsewhere.11,12 The aim of the study was to assess the occurrence, etiology, and management of chest pain in primary care practice. From February 2001 to June 2001, patients presenting with a chest pain as a primary or secondary complaint were consecutively recruited from 58 PCPs and from five residents in a University outpatient clinic, in urban, semi-urban, and rural areas in Switzerland. Inclusion criteria for patients were being 16 years old or older and being able to give an informed consent.
PCPs had to complete a questionnaire during the consultation. They provided information on the thoracic pain presentation, characteristics, accompanying symptoms, clinical examination, and cardiovascular risks factors. Medical appreciation by the PCPs was assessed at different times during the consultation: at the beginning of the consultation (T1), after the history was taken (T2), after the clinical examination (T3), and at the end of the consultation after the complementary analyses (T4). PCPs had to give an appreciation of the severity of the disease and choose between the following three options: «probably benign disease», «probably serious disease», and «I don’t know». Then, they had to inform on the additional exams they planned to perform; these could be done during the consultation or planned for later (none, electrocardiogram (ECG), creatine kinase enzyme (CK), X-ray of the thorax, or other exams) and the type of planned management (no follow-up, telephone follow-up, clinical follow-up, address to a specialist, hospitalization, and treatment).
At 3 months, PCPs were contacted again to provide information on the management procedure and evolution of the included participants. At 12 months, a final questionnaire was administered to the PCPs and information was collected on the management and diagnosis of chest pain. The diagnoses retained after 12 months of follow-up were grouped into six categories: musculoskeletal chest pain, cardiovascular origin, psychogenic, respiratory, digestive, and miscellaneous. A group of investigators discussed the case if the diagnosis of chest pain was inconsistent or uncertain during the follow-up. If the group of investigators were unable to confirm the diagnosis, or if the diagnosis at 12 months was missing, the patient was contacted for further information via his family practitioner. If the patient could not be contacted, the diagnosis at 3 months was retained. In total, 10% of all the case-report forms were revised by an independent expert panel evaluating the consistency of the final diagnosis.
The original TOPIC study was approved by the local ethics committee and all patients gave their informed consent to be included in the study. The present analyses were post hoc analyses of available data and considered as covered by the initial ethics committee approval.
Study outcome
The main outcome was referral to a cardiologist after a complaint of chest pain. The cardiologists ordered or performed almost all of the specific cardiac investigations, such as ergometry, scintigraphy, coronarography, echocardiography, or Holter monitor. Therefore, these were considered secondary endpoints as they did not reflect the decision made by the PCPs. Other secondary outcomes were complementary exams performed in emergency and/or in the practice, such as ECG, cardiac enzymes (CK, troponins), radiography, or non-cardiac specific investigations such as scanner, magnetic resonance imaging (MRI) or gastroscopy. These outcomes were ascertained just after the index consultation and at 3 and 12 months by asking retrospectively which examinations had been performed.
Statistical analyses
We described the baseline characteristics of the patients using means and standard deviations for continuous variables and number and proportions for categorical variables. We compared baseline characteristics between men and women using student t-test and chi-square tests. We assessed if the management of chest pain was different between men and women using logistic regression models. We built univariate models with cardiac investigation as the dependent variable and patients’ sex as the independent factor. We also assessed the association between cardiac investigation and other independent variables related to the patients’ characteristics (age and cardiovascular risks), mode of presentation of chest pain, clinical examination, and physicians’ characteristics. For the logistic regression related to the physicians’ characteristics, we adjusted for cluster using a random effect logistic model.
Finally, we built stepwise multivariable-adjusted logistic regression models adjusted for the patient characteristics, chest pain presentation, clinical examination, and physician characteristics. We built a final model including all variables.
We performed two sensitivity analyses, one restricting the analyses to patients with a new pain and the other restricting analyses to post-menopausal women and men of all ages. We used Stata 14.1 to perform the analyses (StataCorp LLC, College Station, TX, USA).
Results
Patient and primary care physician characteristics
In total, 672 patients presenting with a chest pain in an ambulatory care setting were included, 352 were women (52.4%) and 320 men (47.6%). Table 1 shows the baseline clinical characteristics of men and women included in the initial study.
Table 1.
Baseline characteristics of participants.
| Baseline characteristics of participants (n = 672) | Women (n = 352) | Men (n = 320) | Total (n = 672) | p value |
|---|---|---|---|---|
| Patients’ sociodemographic data and co-morbidities | ||||
| Age (years), mean (SD) | 56.8 (19.7) | 53.4 (18.8) | 55.2 (19.3) | 0.02 |
| Number of cardiovascular risk factors (n = 666), n (%) | 0.04 | |||
| None | 120 (34.5) | 81 (25.5) | 201 (30.2) | |
| 1–2 | 168 (48.3) | 166 (52.2) | 334 (50.2) | |
| ⩾3 | 43 (12.4) | 56 (17.6) | 99 (14.9) | |
| Unknown | 17 (4.9) | 15 (4.7) | 32 (4.8) | |
| History/presentation | ||||
| Emergency consultation (n = 669), n (%) | 106 (30.3) | 91 (28.5) | 197 (29.5) | 0.62 |
| Chest pain is the main complaint (n = 668), n (%) | 172 (49.1) | 183 (57.6) | 355 (53.1) | 0.03 |
| Temporality of complaint (n = 655), n (%) | 0.69 | |||
| New complaint | 163 (47.9) | 156 (49.5) | 319 (48.7) | |
| Recent complaint under investigation | 44 (12.9) | 34 (10.8) | 78 (11.9) | |
| Recurrent complaint | 133 (39.1) | 125 (39.7) | 258 (39.4) | |
| Chest pain during consultation (n = 655), n (%) | 181 (52.5) | 135 (43.6) | 316 (48.2) | 0.02 |
| Chest pain intensity (n = 664), n (%) | 0.39 | |||
| Weak | 60 (17.2) | 53 (16.8) | 113 (17.0) | |
| Moderate | 186 (53.3) | 183 (58.1) | 369 (55.6) | |
| Strong | 103 (29.5) | 79 (25.1) | 182 (27.4) | |
| Angina | 0.80 | |||
| Typical (retrosternal and triggered by effort) | 19 (5.4) | 14 (4.4) | 33 (4.9) | |
| Sub-typical (either retrosternal or triggered by effort) | 98 (27.8) | 87 (27.2) | 185 (27.5) | |
| Atypical (not retrosternal not triggered by effort) | 235 (66.7) | 219 (68.4) | 454 (67.6) | |
| Patient expresses anxiety (n = 667), n (%) | 207 (59.1) | 174 (54.9) | 381 (57.1) | 0.27 |
| Physician is worried about the pain (n = 667), n (%) | 0.88 | |||
| No | 268 (76.8) | 239 (75.2) | 507 (76.0) | |
| Does not know | 31 (8.9) | 30 (9.4) | 61 (9.2) | |
| Yes | 50 (14.3) | 49 (15.4) | 99 (14.8) | |
| Clinical exam | ||||
| Clinical signs of anxiety | 121 (34.4) | 83 (25.9) | 204 (30.4) | 0.02 |
| Tachycardia | 17 (4.8) | 10 (3.1) | 27 (4.0) | 0.26 |
| Chest pain reproducible at palpation | 182 (51.7) | 125 (39.1) | 307 (45.7) | 0.001 |
SD: standard deviation.
The mean age of the participants was 55.2 years, and women were older than men (56.8 vs 53.4, respectively, p = 0.02). The majority of patients had one to two cardiovascular disease risk factors. Women were more likely not to have any known cardiovascular risk factors (34.5% vs 25.5%, p = 0.04). Chest pain was the main complaint for more men than women (57.6% vs 49.1%, p = 0.03). For the majority of patients, the complaint was new (48.7%) or was recurrent (39.4%). Only a small proportion had a recent chest pain under investigation (11.9%). Women were more likely than men to have a thoracic pain still present during the visit (52.5% vs 43.6%, p = 0.02).
Regarding the pain characteristics, there was no significant sex difference in pain presentation between men and women. Angina was mostly atypical (not retrosternal and not triggered by effort) in 67.6% of patients, was sub-typical (either retrosternal or triggered by effort) in 27.5%, and had a typical presentation (retrosternal and triggered by effort) in only a small proportion of patients (4.9%). During the consultation, 57.1% of patients expressed some anxiety without significant difference between men and women. In the majority of the situations, PCPs reported not being worried about the pain (76.0%), without differences according to the patient’s sex. Clinically, women patients were more likely to have chest pain reproductive on palpation (51.7% vs 39.1%, p = 0.001).
Among the 58 PCPs, only eight were women. The mean age for all was 47 years. The majority practiced in an urban setting and had about 12.3 years of experience. On average, 11.4 patients were included by one practitioner. We do not have data on the sex, age, and clinical experience of the five residents who included 22 patients in the study.
Primary care physician assessment and management in emergency
During the initial consultation, at first glance (T1), the physicians estimated the situation as probably benign in 62% of the cases, potentially serious in 24%, and could not tell in 14%. The tendency to consider the chest pain as potentially benign increased during the consultation (T2, T3, and T4). There was no significant difference between female and male patients in the assessment of chest pain severity by the PCPs. Nevertheless, complementary exams in emergency (ECG and troponins/CK) were asked a little more frequently for men than for women (30.6% vs 26.9%, p = 0.29), without a significant difference.
Cardiac investigations during the follow-up
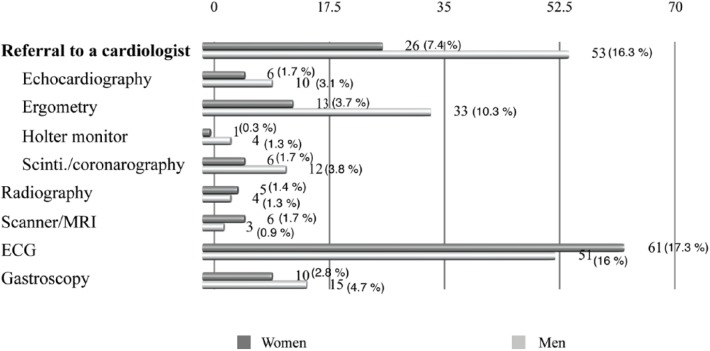
Despite a similar presentation, men were 2–3 times more likely to be referred for consultation to a cardiologist compared to women (53 men (16.6%) vs 26 women (7.4%), p ⩽ 0.0001, odds ratio (OR): 2.49, 95% confidence interval (CI): 1.52–4.09) (Figure 1). Hypothesizing that cardiologists ordered or performed most of the cardiac investigations, among the 79 patients addressed to cardiologists, there was a tendency toward less investigations for women (ergometry, Holter, echocardiography and scintigraphy/coronarography). Other investigations made for chest pain like radiography, scanner/magnetic resonance imaging (MRI), electrocardiograph (ECG), or gastroscopy, were realized without significant sex differences.
Figure 1.
Chest pain investigations during follow-up.
ECG: electrocardiogram; MRI: magnetic resonance imaging.
Other factors associated with increased likelihood for a patient to be addressed to a cardiologist, in univariate analyses, were the patient’s age, presence of cardiovascular risk factors, presence of chest pain during the consultation, pain intensity, and recurrence of pain (Table 2).
Table 2.
Univariate analyses at 12 months.
| OR | 95% CI | |
|---|---|---|
| Patients’ characteristics | ||
| Patients’ gender (female = reference) | 2.49 | 1.52–4.09 |
| Age (continuous), years | 1.02 | 1.01–1.03 |
| ⩽40 (Ref.) | Ref. | |
| 41–60 | 3.31 | 1.41–7.81 |
| 61–80 | 4.82 | 2.09–11.13 |
| >80 | 3.54 | 1.26–9.91 |
| CVD risk factors | ||
| None | Ref. | |
| 1–2 | 3.38 | 1.55–7.36 |
| ⩾3 | 9.51 | 4.14–21.85 |
| Unknown | 1.61 | 0.33–7.94 |
| Mode of presentation | ||
| Emergency consultation | 0.92 | 0.54–1.54 |
| Chest pain is the main complaint | 1.35 | 0.84–2.20 |
| Temporality of complaint | ||
| New complaint | Ref. | |
| Recent complaint under investigation | 0.8 | 0.34–1.88 |
| Recurrent complaint | 1.27 | 0.77–2.10 |
| Chest pain during consultation | 3.35 | 1.92–5.83 |
| Chest pain intensity | ||
| Weak | Ref. | |
| Moderate | 2.05 | 0.9–4.69 |
| Strong | 2.64 | 1.11–6.28 |
| Presentation of angina | ||
| Atypical (not retrosternal not triggered by effort) | Ref. | |
| Sub-typical (either retrosternal or triggered by effort) | 2.24 | 0.94–5.34 |
| Typical (retrosternal and triggered by effort) | 1.26 | 0.62–2.56 |
| Clinical examination | ||
| Clinical signs of anxiety | 1.00 | 0.60–1.67 |
| Tachycardia | 2.79 | 1.14–6.82 |
| Chest pain reproducible at palpation | 0.36 | 0.21–0.62 |
| Physicians’ characteristics a | ||
| Physicians’ gender (female = reference) | 0.61 | 0.34–1.09 |
| Physician is worried about the pain | ||
| No | Ref. | |
| Does not know | 2.64 | 1.27–5.51 |
| Yes | 4.77 | 2.74–8.3 |
| Physicians’ experience (years) | ||
| ⩽5 | Ref. | |
| 6–10 | 0.51 | 0.23–1.14 |
| 11–15 | 0.57 | 0.26–1.27 |
| 16–20 | 0.46 | 0.22–0.97 |
| >20 | 0.6 | 0.28–1.31 |
| Practice in rural setting | 0.9 | 0.51–1.58 |
OR: odds ratio; CI: confidence interval; CVD: cardiovascular disease.
Analyses adjusted to cluster.
Regarding PCP characteristics, men physicians tended to refer less women patients to cardiologists than women physicians (OR: 0.61, 95% CI: 0.34–1.09) but the difference was not statistically significant. The more the PCPs were worried about the pain, the more likely they were to refer their patient to a cardiologist (OR: 4.77, 95% CI: 2.74–8.3). However, the more experienced the PCPs, the fewer cardiac investigations they ordered. The localization of the practice (rural vs urban setting) did not influence the choice to do investigations.
In multivariable-adjusted analyses, after adjustment for patients’ age and cardiovascular risk factors, men were still two times more likely to be referred to a cardiologist compared to women (OR: 2.30, 95% CI: 1.37–3.86). Additional adjustment for chest pain presentation, clinical examination and physician characteristics did not change this association, with an OR of 2.43 (95% CI: 1.29–4.58) in the fully adjusted model (Table 3).
Table 3.
Multivariate analyses at 12 months.
| OR | 95% CI | p value | |
|---|---|---|---|
| Unadjusted patient gender (female = reference) | 2.49 | 1.52–4.09 | <0.0001 |
| Adjusted to patients’ age and cardiovascular risk factors | 2.30 | 1.37–3.86 | 0.002 |
| Adjusted to chest pain presentation | 2.22 | 1.30–3.78 | 0.004 |
| Adjusted to clinical examination | 2.36 | 1.42–3.92 | 0.001 |
| Adjusted to primary care physicians’ characteristicsa | 2.78 | 1.62–4.78 | <0.0001 |
| Adjusted to all variables above | 2.43 | 1.29–4.58 | 0.006 |
| Adjusted to significant variable in the univariate modelsb | 2.07 | 1.18–3.65 | 0.01 |
OR: odds ratio; CI: confidence interval.
Except for 22 residents.
Age, CVD risk factors, chest pain during the consultation, chest pain intensity, tachycardia, and physicians worried about the pain.
This means that the association between a patient’s sex and referral to a cardiologist was not explained by chest pain presentation, clinical signs, or the physician’s characteristics.
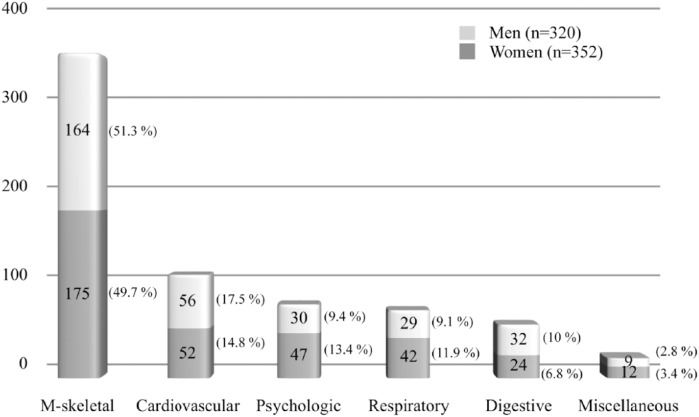
At the 12 months follow-up, the diagnoses retained were musculoskeletal pain (n = 339, 50.5%), cardiovascular disease (n = 108, 16.1%), psychogenic (n = 77, 11.5%), respiratory diseases (n = 7, 10.6%), digestive disorders (n = 55, 8.2%), and miscellaneous (n = 21, 3.1%) (Figure 2).
Figure 2.
Diagnostics considered at 12 months follow-up.
M-skeletal: musculoskeletal.
The proportion of men and women with a final diagnosis of cardiovascular disease was similar (14.7% women vs 17.5% men). Stable angina was the main cardiovascular diagnosis in 39 women (75%) and 35 men (66%). Only a few cases of rhythmic disorder (10 patients), hypertensive crisis (5), cardiac insufficiency (3), and pulmonary embolism (2) were diagnosed. To note, only a low proportion of patients had a final diagnosis of myocardial infarction, with one woman and three men.
PCPs had organized follow-up for the majority of patients at their office. Only some had no follow-up or telephone follow-up. In total, 16 women (4.6%) and 17 men (5.3%) were hospitalized. At the end of follow-up, 12 women (3.4%) and 13 men (4.1%) had died, 12 for reasons directly associated with chest pain (5 ischemic heart disease and 7 cancers). Due to the low number of deaths, we did not compare men and women.
Discussion
This post hoc analysis of data from a prospective cohort study of 672 patients showed that men are 2–3 times more likely to be referred to a cardiologist than women when presenting with chest pain in a primary care setting. This difference in management is not explained by patient characteristics such as age, cardiovascular risk factors, or a differential clinical presentation. Similarly, PCP characteristics such as sex, age, experience, or setting do not seem to explain this important difference in management between men and women either.
In our study, being a woman was an important factor for receiving less cardiac investigation when presenting with a chest pain in ambulatory care. This is in agreement with the study from Daly et al.8 that analyzed registry data from the Euro Heart Survey on the management and clinical outcomes of stable angina. In this study, women were less likely to undergo an ergometry and less likely to be referred for coronary angiography (OR: 0.59, 95% CI: 0.48–0.72). In a study performed in ambulatory care, Bosner et al.3 showed that men were more likely to be referred for an exercise test and be hospitalized than women, but the difference disappeared after adjusting for the typicality of chest pain. In our study, the difference remained present even after adjustment for the type of presentation. This sex disparity is in agreement with another study, highlighting the persistent gap in equity of care between men and women.13 Interestingly, a recent multicenter study that included 10,000 patients with suspected coronary artery disease demonstrated that women were more likely to be referred for imaging stress tests (particularly stress nuclear) compared to men, but women were less likely to have a positive test.10 Sex bias is also observed in the management of chest pain in the emergency department. When presenting with a possible acute coronary syndrome, Chang et al.7 observed that women received fewer cardiac catheterizations and fewer stress tests than men.
Studies have shown that women have higher mortality rates after a cardiovascular event than men.14,15 Several hypotheses can explain these sex differences. Non-specific electrocardiogram changes at rest, lower exercise capacity and smaller vessel sizes can contribute to a generally lower sensitivity and specificity of non-invasive testing in women. This is why the European Cardiac Society (ESC) guidelines advise stress imaging technique (SPECT, stress echocardiography) for specific situations.16
Women have obstructive artery disease less frequently and disturbances of the microcirculation are to be taken into account. Angina or acute coronary syndrome in women may be due to coronary microvascular disease; women have components of pathological vasoreactivity such as spasm and endothelial dysfunction more frequently than men.2 All these findings support biological differences between women and men. However, these biological factors do not justify under-investigation of women, only a poorer prognosis. Other hypotheses could also explain the increased mortality of women after a cardiovascular event. The prevalence of cardiovascular disease is lower in pre-menopausal women and cardiovascular disease has a later onset in women, who also present more often with atypical symptoms, or non-chest pain symptoms.17,18 These factors could lead to misdiagnosis, non-recognition, or later diagnosis and thus poorer management in women. Therefore, women might have worse outcomes than men, in part, because they receive lower quality care, referred to as gender disparity.19 Hence, failure to recognize and diagnose acute coronary syndrome in women constitutes a disparity in care. This disparity could be linked to the strong belief that cardiovascular diseases are almost exclusively masculine disorders and stereotype ideas among both physicians and patients.20 A recent survey interviewed 1000 American women (aged 25–60 years) and 200 PCPs about their awareness of cardiovascular disease.21 It showed that 45% of women were not aware that cardiovascular disease is the foremost killer of women. Cardiovascular disease was rated as a top concern less frequently than weight issues or breast health by PCPs. Consequently, awareness about sex and gender influence in cardiovascular diseases is one of the keys to preventing gender bias. Evidence-based guidelines for cardiovascular disease prevention in women are actually available and take into account both gender and sex specificities.2,22 Inversely, we could also interpret data as an over-investigation in men and indeed, based on this study’s data, we cannot conclude whether it means under-investigation in women or over-investigation in men.
Furthermore, socioeconomic and psychosocial factors may also contribute to explain worse outcomes women. Women are more likely to live in poverty than men and tend to have higher rates of depression and anxiety19 that may have powerful impact on cardiovascular outcomes in women. Finally, recent reports show that women remain under-represented in trials of cardiovascular disease prevention and treatment, although the absolute number of women in clinical trials has increased.20,23 Therefore, treatment and procedures might not be adapted for women.
The strengths of our study are that it was realized in an ambulatory context with more than 670 men and women presenting with chest pain from any origin. It provided a unique opportunity to study sex differences in this population. Many variables were collected, which allowed controlling the effect of factors susceptible to influence the management of chest pain, such as the age of the patient, the clinical presentation of chest pain, or the physician’s characteristics. Some limitations have to be acknowledged. The presence of dyspnea was not collected, therefore some women presenting with an atypical coronary syndrome may have been omitted. Furthermore, diagnoses at 12 months were confirmed by PCPs themselves. All final diagnoses were reviewed independently by a group of clinicians and discussed in case of incoherence. However, the best practice would have been a blinded independent reference panel. The present study uses data, which are almost two decades old and might not necessarily represent actual management. Nevertheless, in a recent review, Khamis et al.18 have suggested that there was increasing evidence of a difference in investigation of chest pain between men and women. The sample size was too small to allow analyses on the impact of different management between men and women on mortality or morbidity. Some socioeconomic markers or qualitative information could have been added to our approach and given us most of the pointers for a more global picture of differences in PCP management of men and women.
In conclusion, we observed important sex differences in PCP management of chest pain in ambulatory care. Women were less likely than men to be referred to a cardiologist. Sex bias is significant and does not appear to be explained by physician evaluation, patient cardiovascular risk factors, patient age, or atypical symptoms at initial presentation. Whether this means under-investigation in women or over-investigation in men remains to be determined. However, these data suggest that efforts must be made to assure equity between men and women in medical care and highlight the need for a sex- and gender-specific approach to chest pain.
Acknowledgments
The authors hereby declare that all illustrations and figures in the manuscript are entirely original and do not require reprint permission. F.V., L.H., B.F., T.D.F., and N.J.-S. contributed to study concept and design; L.H., F.V., and T.D.F. contributed to data acquisition; I.L., C.C., and P.V. contributed to statistical analysis; F.V., L.H., B.F., N.J.-S., and C.C. contributed to study supervision; I.L., P.V., C.C.L., and C.C. contributed to analysis and interpretation of data; C.C.L. and C.C. contributed to drafting of manuscript; and P.V., T.D.F., N.J.-S., L.H., F.V., B.F., I.L., and C.C. contributed to critical revision of the manuscript for important intellectual content.
Footnotes
Data sharing statement: Our data are not on a data repository. We agree to share data related to this research article. Only anonymized data may be shared.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: C.C. was partly supported by a “Medicine and gender” grant from the Faculty of Biology and Medicine, Lausanne, Switzerland and a grant from the Swiss National Science Foundation (PZ00P3_154732 Ambizione Grant). These are government and University grants, and the funders did not influence the design, analysis, or content of the work.
ORCID iD: Carole Clair  https://orcid.org/0000-0001-5281-0943
https://orcid.org/0000-0001-5281-0943
References
- 1. Writing Group Members, Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016; 133: e38–360. [DOI] [PubMed] [Google Scholar]
- 2. EUGenMed Cardiovascular Clinical Study Group, Regitz-Zagrosek V, Oertelt-Prigione S, et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J 2016; 37: 24–34. [DOI] [PubMed] [Google Scholar]
- 3. Bosner S, Haasenritter J, Hani MA, et al. Gender bias revisited: new insights on the differential management of chest pain. BMC Fam Pract 2011; 12: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bosner S, Haasenritter J, Hani MA, et al. Gender differences in presentation and diagnosis of chest pain in primary care. BMC Fam Pract 2009; 10: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khan NA, Daskalopoulou SS, Karp I, et al. Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern Med 2013; 173: 1863–1871. [DOI] [PubMed] [Google Scholar]
- 6. Crea F, Battipaglia I, Andreotti F. Sex differences in mechanisms, presentation and management of ischaemic heart disease. Atherosclerosis 2015; 241: 157–168. [DOI] [PubMed] [Google Scholar]
- 7. Chang AM, Mumma B, Sease KL, et al. Gender bias in cardiovascular testing persists after adjustment for presenting characteristics and cardiac risk. Acad Emerg Med 2007; 14: 599–605. [DOI] [PubMed] [Google Scholar]
- 8. Daly C, Clemens F, Lopez Sendon JL, et al. Gender differences in the management and clinical outcome of stable angina. Circulation 2006; 113: 490–498. [DOI] [PubMed] [Google Scholar]
- 9. International Working Group on Chest Pain in Primary Care, Aerts M, Minalu G, et al. Pooled individual patient data from five countries were used to derive a clinical prediction rule for coronary artery disease in primary care. J Clin Epidemiol 2017; 81: 120–128. [DOI] [PubMed] [Google Scholar]
- 10. Hemal K, Pagidipati NJ, Coles A, et al. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease: insights from the PROMISE trial. JACC Cardiovasc Imaging 2016; 9: 337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Verdon F, Burnand B, Herzig L, et al. Chest wall syndrome among primary care patients: a cohort study. BMC Fam Pract 2007; 8: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Verdon F, Junod M, Herzig L, et al. Predictive ability of an early diagnostic guess in patients presenting with chest pain: a longitudinal descriptive study. BMC Fam Pract 2010; 11: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cook NL, Ayanian JZ, Orav EJ, et al. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation 2009; 119: 2463–2470. [DOI] [PubMed] [Google Scholar]
- 14. Berger JS, Elliott L, Gallup D, et al. Sex differences in mortality following acute coronary syndromes. JAMA 2009; 302: 874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pancholy SB, Shantha GP, Patel T, et al. Sex differences in short-term and long-term all-cause mortality among patients with ST-segment elevation myocardial infarction treated by primary percutaneous intervention: a meta-analysis. JAMA Intern Med 2014; 174: 1822–1830. [DOI] [PubMed] [Google Scholar]
- 16. Montalescot G, Sechtem U, Achenbahc S, et al. 2013. ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2949–3003. [DOI] [PubMed] [Google Scholar]
- 17. Regitz-Zagrosek V. Sex and gender differences in health. Science & society series on sex and science. EMBO Rep 2012; 13: 596–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khamis RY, Ammari T, Mikhail GW. Gender differences in coronary heart disease. Heart 2016; 102: 1142–1149. [DOI] [PubMed] [Google Scholar]
- 19. Joynt KE, Mega JL, O’Donoghue ML. Difference or disparity: will big data improve our understanding of sex and cardiovascular disease? Circ Cardiovasc Qual Outcomes 2015; 8: S52–S55. [DOI] [PubMed] [Google Scholar]
- 20. Hamberg K. Gender bias in medicine. Womens Health 2008; 4: 237–243. [DOI] [PubMed] [Google Scholar]
- 21. Bairey Merz C, Andersen H, Sprague E, et al. Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the women’s heart alliance. J Am Coll Cardiol 2017; 70: 123–132. [DOI] [PubMed] [Google Scholar]
- 22. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation 2004; 109: 672–693. [DOI] [PubMed] [Google Scholar]
- 23. Bucholz EM, Krumholz HM. Women in clinical research: what we need for progress. Circ Cardiovasc Qual Outcomes 2015; 8: S1–S3. [DOI] [PMC free article] [PubMed] [Google Scholar]