Short abstract
Congenital tuberculosis (CTB) after in vitro fertilization (IVF) is a major new problem in developing countries. Only 16 cases of CTB after IVF have been reported, and no tuberculosis (TB) tests were performed before IVF in these cases. However, on the basis of data in the literature and from the World Health Organization, the incidence of CTB has been substantially underestimated. We describe two cases of CTB after IVF in detail in our center and provide new insight into the important issue of controlling TB vertical transmission in developing countries. Performing an early diagnosis of CTB, mostly based on evidence of maternal infection and a high index of clinical suspicion, is a challenge. However, most mothers have no symptoms of TB infection during prepartum, and infertility may be the only symptom. Infertility caused by genital TB is common in countries with a high TB burden, and IVF is considered to be an effective treatment to improve their fertility. Therefore, this may lead to more CTB cases without thorough TB tests before IVF. We suggest that thorough TB tests should be conducted in infertile women before IVF to prevent CTB.
Keywords: Congenital tuberculosis, anti-tuberculosis therapy, in vitro fertilization, vertical transmission, infertility, twins
Introduction
Congenital tuberculosis (CTB) is considered to be rare, with only approximately 400 cases reported in the literature.1,2 This may be because of a high infertility rate in women with genital tuberculosis (TB).3 However, since the usefulness of in vitro fertilization (IVF) in TB-caused infertility was demonstrated in 1985, IVF has become a popular treatment for infertile women.4,5 Genital TB, as a common cause of infertility, was detected in up to 60% of infertile women in a recent investigation in India.3 However, TB tests are not routine before IVF.5,6 A high infertility rate has become a serious problem. As reported by the World Health Organization (WHO) in 2004, the infertility rate ranges from approximately 10% to more than 50% in women of childbearing age in developing countries under investigation.7 The high infertility rate, widespread genital TB in infertile women in countries with a high TB burden, the popularity of IVF in infertile women, and the lack of TB tests before IVF have resulted in CTB after IVF becoming a new major issue in developing countries.8 We report two cases of CTB following IVF, including the first twin case described in the literature, where only one of the twins was affected.
Case Presentation
Case 1
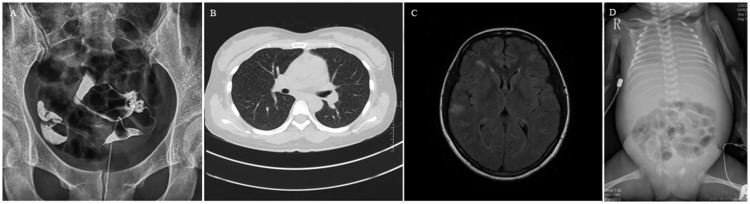
Case 1 was a male neonate who was one of twins born at 30 weeks’ gestation via primary cesarean delivery because of fever and serious headache in the mother. The mother received IVF because of salpingitis (Figure 1a) and had a history of persistent fever, despite treatment for chorioamnionitis and nosocomial pneumonia. Her serum anti-mycobacterium tuberculosis (MTB) antibody was positive. Chest computed tomography and cerebral magnetic resonance imaging showed pulmonary TB and TB meningitis 5 days before delivery (Figure 1b and c). She received anti-TB therapy with isoniazid and rifampicin 2 days before delivery. The mother had a history of spontaneous abortion. Evaluation of endometrial receptive status via ultrasonographic scanning before IVF was normal. A TB test was not performed before IVF. The neonate, who weighted 1.35 kg, with an Apgar score of 9-10-10, manifested with respiratory distress 30 minutes after birth. He was separated from his mother and managed with assisted ventilation. Acid-fast bacillus (AFB) staining and culture obtained from gastric aspirate and tracheal aspirates were negative and blood culture for bacteria was also negative. The neonate was diagnosed with neonatal respiratory distress syndrome and had a good general condition soon after treatment. However, on day of life (DOL) 41, he developed apnea, bradycardia, and edema of the skin. Chest radiography showed “white lung” (Figure 1d). An evaluation for sepsis was promptly conducted, which included blood and cerebrospinal fluid cultures. These cultures were negative. Polymerase chain reaction (PCR) for MTB DNA from tracheal aspirates was performed and the result was positive. He was promptly treated with isoniazid (10 mg/kg/day) and rifampicin (10 mg/kg/day). However, he developed progressive respiratory failure and septic shock, and died at DOL 56. A biopsy was not performed because his parents rejected it. His sister, who had a good general condition, also went had a thorough TB investigation and the results were negative. She is currently being followed and is still healthy.
Figure 1.
Hysterosalpingography, chest computed tomography, and cerebral magnetic resonance imaging of the mother and chest radiography of the neonate (case 1) (a) Hysterosalpingography suggests a normal uterus and salpingitis. (b) Maternal chest computed tomography shows miliary nodules in both lungs. (c) Maternal cerebral magnetic resonance imaging shows infiltration of brain parenchyma and meninges. (d) Chest radiography of the neonate shows diffuse infiltration of both lungs.
Case 2
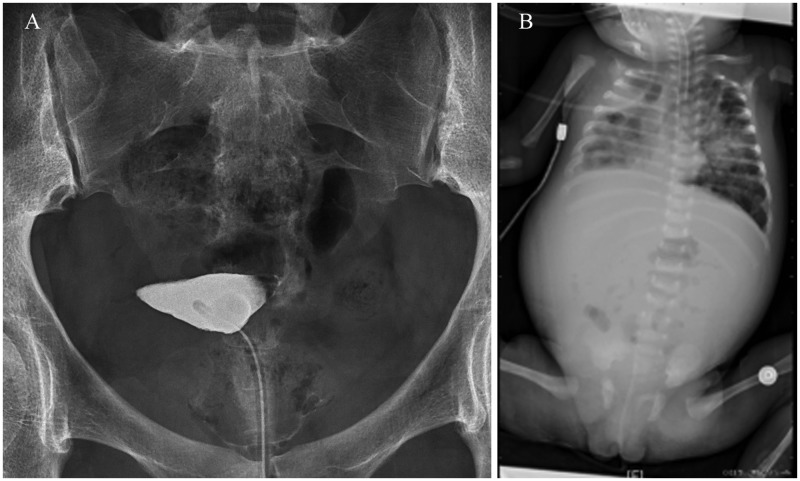
Case 2 was a female neonate who weighed 1.43 kg and was born via primary cesarean delivery at 31 weeks’ gestation. She was admitted as a very low birth weight infant and isolated from her mother after birth. Her mother received IVF because of tubal obstruction (Figure 2a). She had no history of TB, and a TB test was not performed before IVF. The neonate developed apnea, respiratory insufficiency, and fever on DOL 26, and was considered to have neonatal pneumonia based on chest radiography (Figure 2b). She was managed with assisted ventilation and multiple antibiotics. However, she still had persistent fever and apnea. She was then transferred to our neonatal intensive care unit. TB was suspected and bronchoalveolar lavage was performed in the neonate. Her mother was recommended to have an investigation for TB. Interferon gamma release assay and tuberculin skin test (TST) results were positive for the mother. AFB staining and culture obtained from leukorrhea were also positive. She was diagnosed with genital TB. The neonate’s AFB stain of the aspirate was positive and MTB PCR testing of the isolate confirmed the diagnosis of CTB on DOL 28. Tests for cerebrospinal fluid were normal. Anti-tTBtherapy with isoniazid, rifampicin, and pyrazinamide was started in this neonate. However, she still progressed to respiratory failure and acrocyanosis, even with aggressive respiratory and circulatory support. The infant’s condition deteriorated and the family withdrew support on DOL 56. She expired soon after circulatory support and a post-mortem examination was rejected by her parents.
Figure 2.
Hysterosalpingography of the mother and chest radiography of the neonate (case 2). (a) Hysterosalpingography shows tubal obstruction of both sides, but the uterus is normal. (b) Chest radiography shows extensive patchy cloudy opacity and areas of consolidation mainly in the right lung.
Ethics approval and consent
No ethical approval was required. The authors obtained written informed consent for publication from the patients’ parents.
Discussion and conclusion
CTB can be diagnosed by the primary criterion (the presence of proven TB disease) and at least one of the secondary criteria as defined by Cantwell’s criteria.9 These secondary criteria are as follows: (i) lesions in the newborn during the first week of life; (ii) a primary hepatic complex or caseating hepatic granulomata; (iii) TB infection of the placenta or the maternal genital tract; and (iv) exclusion of the possibility of postnatal transmission by investigation of contacts. Both of our neonatal patients were isolated from their mothers and admitted to the neonatal intensive care unit after birth. TB infection was confirmed by the MTB PCR test and/or AFB staining and culture. The diagnosis of CTB was confirmed.
Early diagnosis of CTB is difficult. Clinical manifestations of CTB, such as fever, cough, respiratory distress, apnea, and cyanosis, are unspecific. These manifestations are easily confused with sepsis and pneumonia.2,9 Additionally, TST results are often negative because of a low T cell response.9 Therefore, diagnosis of CTB depends on a history of maternal infection and a high index of clinical suspicion.1 However, in an analysis of 170 cases of CTB, many of the mothers were asymptomatic during prepartum.1 In these infertile women, infertility may be the only symptom. Subramani and colleagues reported significantly reduced levels of endometrial receptivity markers and metabolic perturbations in endometrial tissue that were detected via proton nuclear magnetic resonance spectra in women with dormant genital TB.10,11 These authors thought that these factors were a possible cause for repeated implantation failure. Because of limitations in the presently available diagnostic tests for genital TB, these metabolic markers may be feasible for early diagnosis of dormant genital TB.10,11 CTB is almost lethal without anti-TB therapy and early diagnosis is still a major challenge1,2,9 Therefore, more importance should be placed on prevention of CTB by thorough TB tests in infertile women before IVF.
TB vertical transmission is defined as transplacental transmission through umbilical veins to the fetal liver and lungs, or aspiration and swallowing of infected amniotic fluid in utero or intrapartum.1 TB infection of the uterus or placenta is a necessity in CTB.12,13 However, infants do not necessarily develop CTB, even with maternal genital TB, as we found in the case 1 twin. Only case 1 was infected, but not the other twin. We speculate that only one placenta was involved. This is the first twin case described in the literature, where only one of the twins was affected by CTB. This possibility may also explain why some women with genital TB who can be fertile have a healthy newborn without CTB. Further investigation is warranted for TB vertical transmission in women with genital TB and the possible factors that may affect the outcome.
The TB vertical transmission rate is estimated to be 16%, including all maternal statuses of TB infection.14 Women who have only pulmonary TB are not likely to infect the fetus, unless in utero infection occurs after maternal MTB bacillemia. However, there are no data specifically on the vertical transmission rate of genital TB. On the basis of the investigation of genital TB in infertile women and the vertical transmission rate in all types of conditions (which may be much higher in genital TB), the real incidence of CTB has been substantially underestimated, particularly in developing countries. This is likely because of diagnostic difficulty and medical staff’s lack of awareness.14 In countries with a high TB burden, such as China, the incidence of TB is 67/100,000, with 296,000 total female infections.8 The incidence of CTB is likely to be much higher considering the 16% vertical transmission rate. According to a recent investigation of women with genital TB in India, more than half of them suffered from infertility.4 IVF in these women could improve their pregnancy outcome. However, TB tests before IVF are not routine.5,6,10,13–22 Infertility caused by genital TB is common in countries with a high TB burden, and IVF is considered to be an effective treatment to improve fertility. Therefore, this may lead to more CTB cases without thorough TB tests before IVF. We suggest that thorough TB tests should be conducted in infertile women before IVF, especially in women with tubal factor infertility, because TB is most commonly seen in the uterine tube. There is no gold standard for genital TB. Therefore, a combination of the TST, interferon gamma release assay, imaging, and endometrial biopsy with an AFB smear, culture, and DNA PCR for MTB in women before IVF, along with anti-TB chemotherapy in women with TB infection, may be the best choices in countries with a high TB burden to prevent CTB.3,5 New markers, such as endometrial receptivity markers, could also be useful for early diagnosis of genital TB.10,11 More investigation on diagnostic tests for genital TB are required. We emphasize the urgency for recommending TB tests as routine in infertile women in developing countries to reduce the incidence of CTB.
Contributions
All of the authors have revised the manuscript and contributed to drafting of the manuscript. They confirm that the manuscript is an original version and has not been published in any other scientific journal or elsewhere. Ren ZX, Yang HM, and Zhang XL collected the patient’s information and drafted most of the report; Zhang Q, Chen L, and Xu F provided the images and wrote the figure legends; Yang J edited the manuscript and wrote the Discussion section; Liu FH helped analyze the TB tests in infertile women in the Assisted Reproductive Center.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Peng W, Yang J, Liu E. Analysis of 170 cases of congenital TB reported in the literature between 1946 and 2009. Pediatr Pulmonol 2011; 46: 1215–1224. [DOI] [PubMed] [Google Scholar]
- 2.Patel S, DeSantis ER. Treatment of congenital tuberculosis. Am J Health Syst Pharm 2008; 65: 2027–2031. [DOI] [PubMed] [Google Scholar]
- 3.Kulshrestha V, Kriplani A, Agarwal N, et al. Genital tuberculosis among infertile women and fertility outcome after antitubercular therapy. Int J Gynecol Obstet 2011; 113: 229–234. [DOI] [PubMed] [Google Scholar]
- 4.Soussis I, Trew G, Matalliotakis I, et al. In vitro fertilization treatment in genital tuberculosis. J Assist Reprod Genet 1998; 15: 378–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hongbo L, Li Z. Miliary tuberculosis after in vitro fertilization and embryo transplantation. Afr Health Sci 2015; 15: 701–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flibotte JJ, Lee GE, Buser GL, et al. Infertility, in vitro fertilization and congenital tuberculosis. J Perinatol 2013; 33: 565. [DOI] [PubMed] [Google Scholar]
- 7.Shea O, Rutstein IHS, World Health Organization. DHS Comparative Reports 9: Infecundity, Infertility, and Childlessness in Developing Countries. 2004.
- 8.World Health Organization, Use of high burden country lists for TB by WHO in the post-2015 era. 2015. (WHO/HTM/T/201.29).
- 9.Mittal H, Das S, Faridi MM. Management of newborn infant born to mother suffering from tuberculosis: current recommendations & gaps in knowledge. Indian J Med Res 2014; 140: 32–39. [PMC free article] [PubMed] [Google Scholar]
- 10.Subramani E, Madogwe E, Ray CD, et al. Dysregulated leukemia inhibitory factor and its receptor regulated signal transducers and activators of transcription 3 pathway: a possible cause for repeated implantation failure in women with dormant genital tuberculosis? Fertil Steril 2016; 105: 1076–1084.e5. [DOI] [PubMed] [Google Scholar]
- 11.Subramani E, Jothiramajayam M, Dutta M, et al. NMR-based metabonomics for understanding the influence of dormant female genital tuberculosis on metabolism of the human endometrium. Hum Reprod 2016; 31: 854–865. [DOI] [PubMed] [Google Scholar]
- 12.Gleeson LE, Varghese C, Ryan E, et al. Untreated chronic tuberculous salpingitis followed by successful in vitro fertilization conception and congenital tuberculosis. QJM 2015; 108: 899–901. [DOI] [PubMed] [Google Scholar]
- 13.Loto OM, Awowole I. Tuberculosis in pregnancy: a review. J Pregnancy 2012; 2012: 379271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Schutter I, Schepers K, Singh M, et al. Latent tuberculosis in a newborn: diagnostic challenges. Eur J Pediatr 2010; 169: 1155–1158. [DOI] [PubMed] [Google Scholar]
- 15.Mony VK, Polin J, Adler E, et al. Congenital tuberculosis: a missed opportunity. J Pediatric Infect Dis Soc 2014; 3: e45–e47. [DOI] [PubMed] [Google Scholar]
- 16.Altunhan H, Keser M, Pekcan S, et al. Congenital tuberculosis in premature twins after in vitro fertilisation. BMJ Case Rep 2009; 2009. doi:10.1136/bcr.05.2009.1894 [DOI] [PMC free article] [PubMed]
- 17.Zheng Y, Bai G, Zhang H. Congenital tuberculosis detected by T-SPOT.TB assay in a male infant after in vitro fertilization and followed up with radiography. Ital J Pediatr 2014; 40: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emiralioglu N, Dogru D, Oguz B, et al. Congenital tuberculosis after in-vitro fertilization in a woman previously undiagnosed with tuberculosis salpingitis. Pediatr Neonatol 2016; 57: 539–540. [DOI] [PubMed] [Google Scholar]
- 19.Stuart RL, Lewis A, Ramsden CA, et al. Congenital tuberculosis after in-vitro fertilisation. Med J Aust 2009; 191: 41–42. [DOI] [PubMed] [Google Scholar]
- 20.Doudier B, Mosnier E, Rovery C, et al. Congenital tuberculosis after in vitro fertilization. Pediatr Infect Dis J 2008; 27: 277–278. [DOI] [PubMed] [Google Scholar]
- 21.Wong R, Wong K. Atypical presentation of congenital tuberculosis in a preterm infant. HK J Paediatr (New Series) 2007; 12: 133–136. [Google Scholar]
- 22.Bonnet C, Michel F, Nicaise C, et al. Congenital tuberculosis in preterm neonate: a case report. Arch Pediatr 2009; 16: 439–443. [DOI] [PubMed] [Google Scholar]