Abstract
The DREAMS Team research advocacy training program helps clinical faculty and health students introduce basic clinical research concepts to diverse older adults to galvanize their active involvement in the research process. Older adults are frequently underrepresented in clinical research, due to barriers to participation including distrust, historical mistreatment, and their lack of health literacy. The DREAMS Team program aims to involve diverse older adults throughout all phases of research and increase research participation, thereby contributing to the growth of quality patient-centered, evidence-based health care. This course was developed for clinical faculty to deliver to diverse adults aged 55+ in eight 50-minute lectures, followed by half-hour small group discussions moderated by health students. A pilot cohort of 24 individuals was assessed for satisfaction post-program, and self-efficacy before and after the program. Older adult participants improved on a survey measure of self-efficacy, and indicated satisfaction on a post-program questionnaire. All agreed or strongly agreed that they enjoyed participating, and that classes enhanced knowledge/skills about the topics, were high quality, and provided useful information. Twenty-two out of 24 individuals who completed the program indicated they planned to get involved as research advocates. The DREAMS Team program can be offered either on its own, or as a follow-up program to a general health education course led by health students and/or professional researchers or clinicians. Educating older adults about the research process and advocacy through interactive seminars led by congenial and respectful researchers and health students may remove some barriers to research participation and involvement among diverse older adults.
Older adults, particularly those from marginalized communities (i.e., low socio-economic status [SES], racial/ethnic minorities), are frequently underrepresented in research. Adults aged 65 and over account for approximately two-thirds of cancer cases but only about 30% of cancer clinical trial participants (Lewis et al., 2003). Racial and ethnic minorities and people with low income are critically underrepresented in research (Kaiser, Thomas, & Bowers, 2017), although they experience persistent health disparities (Kuczmarski et al., 2016). Community trust building and creation of community partnerships, including training underserved health ambassadors, have been identified as appropriate means for engaging underserved participants in research (Lang et al., 2013). Focus groups conducted by Perkins, Dillard, Hart, Wincek, and Hackney (In Review) with diverse older adults also revealed barriers to participation, including misconceptions about research, distrust of researchers and the medical community, and perceived ageism and lack of respect from scientists and health professionals. These barriers could be addressed through education and partnership building. Perkins et al. also conducted focus groups with clinical faculty at Emory School of Medicine in Atlanta, who acknowledged the role that researchers and the medical community could play in overcoming barriers, including improving communication with underrepresented communities and treating older adults as research partners instead of research subjects. The DREAMS program (acronym derived from title of original project, “Developing a Research Participation Enhancement and Advocacy Training Program for Diverse Seniors”), was therefore developed, with input from Patient Stakeholder Advisors (PSAs), to increase involvement of diverse older adults in research through education about research processes and current human research protections. The DREAMS program was also intended to grow community partnerships and build rapport between researchers, health students, and diverse seniors.
DREAMS was designed with two parts, which can be offered independently or in tandem. DREAMS Part I is a health education program led by health professions students in partnership with experienced researchers and physicians. This program gives older adults direct access to both medical professionals in-training and seasoned experts in a congenial setting where all questions are welcome and all comments are respected (a “toolkit” for implementation of Part I is available on the Patient Centered Outcomes Research Institute (PCORI) website). Part I was modeled after “Senior University” health education programs for older adults and individuals with Parkinson’s disease previously offered by Dr. Madeleine Hackney and Rebecca Dillard in collaboration with various senior groups.
The curriculum presented here was originally offered as “Part II” of the DREAMS program, for interested individuals who completed Part I (referred to as the DREAMS Team post-training). Presenters were recruited to teach topics based on syllabi from the Parkinson Disease Foundation’s successful Parkinson’s Advocates in Research (PAIR) Program (Parkinson’s Disease Foundation, 2017), through which our two PSAs for the inaugural DREAMS project were trained. The curriculum includes description of the research advocate role, the clinical research process, research ethics and protections of human research subjects, analysis and evaluation of research (including very basic statistical analysis), informed consent and health literacy, and an introduction to current studies taking place in the area. The program is appropriate to be offered at a research university, to nurture ties between the community and the institution. The majority of content can be delivered by clinical researchers (from any discipline) to facilitate interaction between researchers and older adult participants. Some presentations could feasibly be led by advanced health professions students, and the final presentation is intended to be presented by individuals from the community, who are already serving in the patient advocate role. Small group moderators can be health students or coordinators at any level.
To overcome hidden prejudices and reduce the negative impact of unintended ageism, racism, and other forms of discrimination in medical care (Basáñez, Blanco, Collazo, Berger, & Crano, 2013), it is important to include interaction with underserved and routinely undervalued patient groups in the continuing education of health students and professionals. A great way to increase comfort and effectiveness in interacting with diverse patients is to practice interactions with individuals of different SES, age, and race in a safe and open environment that encourages communication. The lecture-discussion format of DREAMS provides a platform on which to share information and start conversations about important topics. When implementing the inaugural DREAMS program, we found that some individuals prefer large group (full class) discussion in a question-answer format, while others appreciate breaking into small groups, so that everyone has a better opportunity to contribute to discussion. We concluded that the combination of engaging lectures, questions and comments directed at the presenter, and small group discussions was effective in encouraging the presenter to practice responding adequately and understandably to community stakeholders, and developing rapport between health students, professionals, and underserved older adults.
Educational programs for seniors led by health students or professionals have helped develop respect for perceptions and concerns of older adults and increased student comfort interacting with older adult patients (Hogan, 2015). DREAMS Part II, a.k.a. the DREAMS Team program, provides an opportunity to target current and future healthcare providers’ relationships with older adults of various SES and race, while addressing the current demand for greater patient involvement in healthcare development and implementation (Forsythe et al., 2017). The DREAMS Team program was developed to create a pool of educated research advocates primed to take on roles as community research partners. From serving on community advisory boards and assisting in the development of research ideas, to helping recruit for and implement studies, to assisting with accessible dissemination, the DREAMS Team can become a valuable lasting resource for bridging the gap between medical researchers and diverse older adult communities.
Methods
All participants provided informed consent, and the project was approved by the Emory Institutional Review Board.
The educational objectives of the intervention were to: 1) Identify considerations for recruitment and education of older individuals from various socioeconomic strata (SES), health literacy levels, and racial/ethnic backgrounds for a research advocacy training program; 2) provide an opportunity for health students and professionals to practice interpersonal skills and communication with a diverse older adult population; and 3) prepare diverse older adults to act as research advocates, who can join research teams as part of community advisory boards or as PSAs serving to propagate the mutual education of researchers and their peer groups.
General setup, description, and recruitment
Each DREAMS Team session lasts 1½ hours, with an approximately 50-minute lecture (including discussion), followed by a 5–10-minute break, then approximately 30 minutes of small group discussion. Lectures are given with an open invitation to ask questions throughout. During the break, participants can stand, walk around, use the restroom, or partake in provided snacks. Seating is rearranged during the break, so that the class can be splited into groups of 4–5 individuals with a health student or researcher moderator in each group to facilitate discussion.
An assigned lead moderator throughout the course can coordinate speakers, health students, and older adult participants, deal with technical issues, distribute materials and act as a timekeeper during the class. Timing flexibility is critical to allowing discussion to emerge; however, to respect the time of all involved, the program should end in a timely fashion. For this reason, in cases where a lively discussion has emerged involving the majority of the class, the full class discussion can take some of the time normally reserved for small group discussion, at the moderator’s discretion. The program coordinator/moderator can also take attendance and get to know the participants by name, which helps to establish consistency and familiarity for older adult participants, despite the speakers changing each week. Presentations may vary in length to accommodate the emergence of fruitful discussion, which should be encouraged and not stifled. Speakers should use techniques of elaboration, like summarization and questioning, to help make listening to lectures an active process (Mayer, 2003). Austin-Wells, Zimmerman, and McDougall (2003) found that PowerPoint was a preferred presentation format among older adults, and maintained attention better than overhead projection or use of flip charts.
In development of the program, participants from Part I provided mixed feedback on the small groups, which prompted adjustments. Having presentation-specific questions, and providing these questions as handouts or via a presentation slide to all participants, helped moderators guide discussion more effectively and helped conversations stay on-topic. One DREAMS Team participant (a retired school teacher, who had also participated in Part I) observed that having a handout with discussion questions “keeps us on track” and makes group discussions more fruitful. Learning strategies employed in group discussions, including recalling lecture information, drawing inferences, and relating new information to prior knowledge or experiences, contribute to information retention (Medin, Ross, & Markman, 2005). Appropriate clinical faculty should be invited to present with significant advance notice, so they can adequately prepare for the sessions, including developing a PowerPoint presentation and discussion questions for their assigned topic. Health students maybe recruited as moderators for the program through student clubs, email blasts, or campus advertisements. A ratio of approximately one moderator per 4–5 older adult participants is ideal. The faculty presenter can “float” around the room and join/provide input for various groups, because often the older adult participants are interested in getting their questions answered by the expert.
Enrolling a diverse group is ideal for program success. Some fruitful avenues for recruiting diverse older adults include sharing information at “research social” events, advertising the program at support groups and community educational meetings, directly visiting senior living communities or community senior centers to present information and distribute flyers, advertising on websites, and making contacts at local churches to distribute flyers or host research recruitment events. It is important to gain prior approval and buy-in from communities before distributing program information, and therefore, contacting and meeting with program coordinators or facility managers early on are essential to recruitment efforts. We recommend targeting recruitment of 25 older adults, plus 5–6 health students and a speaker for each class.
Materials
A laptop or desktop computer with projector and screen is required for presentation of the PowerPoint lectures, and the room should be able to comfortably accommodate 30 people, including individuals with disabilities or mobility challenges. Provision of healthy snacks and coffee/water is suggested for breaks. Printing large-print handouts from the PowerPoint slides for each participant can help those with vision problems and encourages review and retention of program material. Extra pens and paper should be available for those who want to take notes.
DREAMS Team curriculum
A description of each of the eight lessons is provided below. Many presentations are accompanied by content-specific discussion questions, but the following general discussion questions can also be used with any of the presentations:
Was there any information from today’s talk that surprised you, or stuck out to you as particularly interesting or important?
What did you know about this topic before you came here today?
How might you use the information from today’s talk as an advocate and educator?
Who from my network could I share this information with?
Presentation 1
“Advocates in Aging Research: Why, Who, & What” provides an overview of the DREAMS Team program curriculum, and introduces the idea of community involvement in research. This presentation addresses why we need advocacy in research related to the aging process, that is, to build trust with the research community, increase accessibility of research trials and information, reduce communication barriers between participants and researchers, and reduce racial and age-related disparities in research participation and health care. Important take home messages included that anyone (you!) can be an advocate, and that advocates can get involved and make a difference in a multitude of ways, including expressing needs, ideas, and preferences of older adults to the scientific community, increasing diversity in research trials across age/race/culture/location, educating peers about research, advocating for themselves and their peers, and recruiting others into research. The following discussion questions were provided:
What issues in aging-related research are important to me?
What areas of research or health care would I like to see changed (or conversely, stay the same)?
What groups, networks, friends, or peers could I educate about research and possibly help engage with clinical researchers?
What are my preferred ways to be involved as an advocate and educator?
Presentation 2
“The Clinical Research Process: Focus on Patient-Centered Outcomes Research” provides basic information about the clinical research process, including an explanation of “patient-centered” outcomes, interventional vs. observational studies, the phases of clinical research, and common research concepts like placebo, blinding, and randomization. Example studies are described from each phase of the clinical research process to apply concepts and enhance understanding. Important take home messages included the importance of clinical research in applying evidence for clinical practice, promoting innovation, reducing bias, and improving equity in health care, as well as the role of patient-centered outcomes in keeping research relevant for persons living with disease (i.e., by looking at measures that matter to patients such as function and health-related quality of life) and including patients in the process of research.
Presentation 3
“Ethics and Aging Research” addresses the importance of ethics in research. This section is particularly fruitful for discussion, and hearing from older adult participants about their perceptions and ideas related to how people participating in studies are treated and should be treated. The ethics presentation also provides an opportunity to address prominent past abuses of research (e.g., the Tuskegee syphilis study) and subsequent policy changes intended to protect human research subjects (including the establishment of Institutional Review Boards). Important take home messages included the potential benefit from research on chronic progressive diseases, which requires the participation as research subjects of older patients suffering from these diseases, why ethics is important both for protecting research participants and serving the interest of society or a particular group, and how involving members of the community in planning and implementing studies can improve the quality and ethicality of research.
Presentation 4
“Understanding and Interpreting Clinical Trials” introduces basic descriptive statistics, including mean and median, as well as the use and interpretation of “p values” to perform hypothesis testing in a fun, interactive lecture. For instance, the class can be surveyed with an uncontroversial and motivating question such as how many grandchildren they have, and the collected data can be used to fill in a histogram and visually identify descriptive statistical measures such as the minimum and maximum values, as well as the measures of central tendency including mean, median, and mode.
Based on previous didactic experience with undergraduates and graduates, the concept of dispersion was considered to be most effectively communicated visually on the histogram, rather than through the use of formulae for quantitative measures such as inter-quartile range and variance. Measures of IQ range and variance were considered to provide comparatively little additional intuitive understanding at the expense of substantially increased complexity and decreased pacing for this audience. Anecdotally, in the inaugural DREAMS Part II, the presence of one participant with a large number (>20) of grandchildren provided an opportunity for an engaging and entertaining extemporaneous discussion about how the presence of outlier values might or might not affect the sample mean and median.
After obtaining sample data in the form of a histogram, concepts related to hypothesis testing can be introduced in a concrete manner by comparing the class’ data to that of an available reference population—for example, the population of U.S. presidents, for whom these data are available online (Chalabi, 2014). In the inaugural DREAMS Part II, the class was encouraged to hypothesize whether the population of seniors in the Atlanta area, as a whole, had greater or fewer grandchildren than the population of U.S. presidents. Topics of discussion might include historical trends in number of grandchildren over time, socioeconomic differences between the class sample and the population of presidents, and other related issues. Finally, the hypothesis is formalized into a statistical test, and an appropriate p value (the probability of observing a difference between samples equally or more extreme given chance alone) is calculated using an appropriate online calculator in front of the class.
For simplicity, in the inaugural DREAMS Part II, rather than performing a comparison of central tendency, such as a t-test, which would require the introduction of concepts including the standard error of the mean and sample size guidelines informed by the central limit theorem—both of which are often time-consuming even for graduate students—it was decided to reframe the question as one that could be answered with a chi-squared test of homogeneity (i.e., whether the proportion of class participants with grandchildren was equal to the proportion of U.S. presidents with grandchildren), which is parameterized only by the sample proportion and size, and which can be quickly entered into an online calculator. Several participants indicated this was their favorite lecture due to the interactive and accessible presentation of information that they would most likely not have sought out or understood on their own.
It is stressed that in a statistical test, the p value is the probability of observing your result based on chance alone, not the probability that the result is “due to chance” although many interpret it that way. The following discussion questions were provided:
What are some differences between the average, or mean, and median?
Have you heard the terms “average” and “median” other places? Where? Do they mean the same thing as we discussed?
What does it mean when the p value is small? When it is large?
What is the p value that Dr. X (the presenter) is wearing pants?
Presentation 5
“Aging and Clinical Research: What’s in the Pipeline” is designed to give participants an introduction to current research studies going on locally and get them thinking about what kind of studies they may be interested in getting involved in, as well as to give local researchers an opportunity to advertise their studies. The presentation can also include national resources for finding studies online, such as https://ClinicalTrials.gov and https://ResearchMatch.org. A template slide (including project description, a brief why and how for the study, and a summary of findings or future plans) can be sent to research groups within your institution who may be interested in advertising current studies to a diverse older adult population. These slides are then compiled into the presentation in advance of the lecture. An individual familiar with many of the studies to be presented, such as a division or departmental head, is appropriate to present this lecture. Figure 1 depicts a template for a slide. The following discussion questions were provided:
Figure 1.
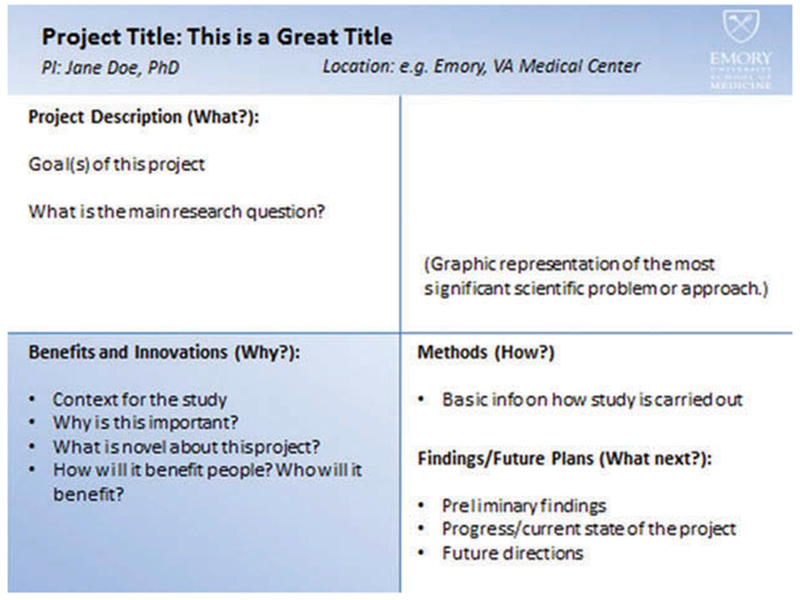
“Aging and Clinical Research: What’s in the Pipeline” template slide. A template PowerPoint slide was provided to interested research groups in order to make it as easy as possible for them to contribute to the lecture, and to help the presentation have a consistent appearance without extensive editing from the organizers.
Which of the studies presented today interest you the most? Why?
Can you imagine any specific barriers to carrying out any of these studies?
Do you have any ideas for how you might want to get involved in any of these projects? (e.g. by helping with recruiting)
How would you present this research to someone you know?
Are there other research studies (either actual studies that you know about or potential studies that you can imagine) that you would be interested in getting involved with as an advocate?
Presentation 6
“Informed Consent: Understanding the Issues and Health Literacy” defines health literacy and identifies associated challenges and consequences associated with low health literacy. These challenges include issues with the informed consent process, which community research advocates (e.g., the DREAMS Team) could potentially help alleviate. A list of questions to ask before participating in a study can be provided (e.g., what is the purpose of the study, what will I be asked to do, what are the possible risks and benefits, and how will the results be shared). Use of the teach-back method is also suggested for researchers or participants to initiate during the informed consent process (or during any participant-researcher interactions where accurate conveyance of information is important); to ensure accurate communication, the participant can say, “Let me tell you in my own words what I understand.” Important take home messages include the impact of low health literacy on health and the responsibility of the healthcare system, local community, and society to address health literacy challenges, as well as the key elements of the informed consent process participants should understand (e.g., the purpose of the study, who is conducting the study, potential benefits, possible or anticipated risks, what you will be doing during the study, and who to contact if you have questions during the study).
Presentation 7
“Effective Advocacy within the Clinical Research Process” was originally presented by a researcher who also does advocacy in the area of HIV/AIDS research. This section clarifies and reiterates what research advocates can do, and gives participants an opportunity to think about and discuss their own interests for getting involved in the clinical research process. Advocates can get involved in any and all stages of the research process: helping with study concept development by discussing with researchers what is important to the community, assisting in writing and reviewing grants, providing input on the study design such as barriers to recruitment or participation, helping with developing the informed consent protocol or even acting as a peer advocate during the consent process, disseminating study information through presenting or writing about results for lay audiences, and serving on an FDA advisory committee or other advisory committees requiring consumer/patient input. The following directions can be given following the presentation to lead into group discussion:
Talk to the person sitting next to you about the information on these slides and discuss what YOU would like to do.
Write down the questions that come up during your discussion.
In 10 minutes, we will meet as a group again to talk about your questions.
Presentation 8
“Hearing from the Ones in the Trenches, and Getting Started as an Advocate in Aging Research” is the one lecture not necessarily presented by researchers or faculty. For this lecture, organizers should invite 1–4 individuals currently acting as research advocates to share their personal stories, experiences, and tips for getting started. Organizations for specific conditions, such as Alzheimer’s disease, Parkinson’s disease, cancer, etc., can help identify and facilitate contact with patient advocates to present at this final lecture. These guest presenters may use a PowerPoint format if desired. A short biography should be provided by each speaker. The idea of Presentation 8 is to demonstrate what advocacy can look like through personal stories. In our program, two representatives from Parkinson’s disease foundations and one from a mitochondrial disease foundation presented; each shared their reasons for getting into advocacy, how they got involved, and what kind of activities they currently performed as a research advocate, thus providing inspiration for the newly trained DREAMS Team members.
After the course: Getting the DREAMS Team involved
The DREAMS Team curriculum is intended to be an introduction to research advocacy and can be made more effective by post-program follow-up and sharing of local resources/opportunities to stay involved. We refer to older adults who complete the program as “DREAMS Team” members to emphasize that they are a part of an active group, and encourage staying connected after the program’s end. In order to transition older adults from the training program into performing the patient advocate role, DREAMS Team members should be kept apprised of community and research events and should be supported and encouraged to present to groups they are associated with about what they learned. The authors created an abbreviated version of the DREAMS Team curriculum, in the form of a single 30-minute presentation, which has been presented by 4–5 DREAMS Team members at support groups and senior centers in Atlanta. This resource was developed with the help of DREAMS Team presenters. We recommend working closely with any DREAMS Team members who plan on presenting and getting their feedback to help tailor presentations to different audiences. Another possible event to help the DREAMS Team get started as advocates is the “speed dating” research social, in which newly trained DREAMS Team advocates sit opposite a researcher and chat for about 5 minutes, until a buzzer sounds and the researchers rotate to the next advocate. This unique set up for a research social ensures that everyone has the opportunity to talk and potentially make connections, which might lead to participation in future studies or involvement as Community Advisory Board members or PSAs. We learned that researchers should bring flyers or cards to share, and as much space as possible should be provided between “couples” to facilitate researchers and older adults being able to hear one another. These engagement activities provide opportunities to maintain and continue to build upon relationships with DREAMS Team members beyond program completion.
Evaluation
The Generalized Self Efficacy (GSE) scale assessment (a survey to assess perceived self-efficacy in dealing with daily hassles and adapting to stressful life events) was administered to participants immediately before, after, and 8 weeks after the DREAMS Team training program. We also administered a post-program satisfaction questionnaire arranged on a 5-point Likert scale, (1 = strongly disagree, 5 = strongly agree) which asked questions about enjoyment, usefulness of the information and willingness to continue such a program.
Results
Twenty-four diverse older adults completed six or more classes of the DREAMS Team program, and 24 completed post-testing (M age = 68.2 ± 7.1; Black [n = 12], White [n = 7], other ethnicity [n = 5]; female [n = 14], male [n = 10]). Participant scores increased significantly on the GSE scale (p < 0.001), and these gains were maintained 8-weeks after the classes ended. On the satisfaction questionnaire, participants agreed or strongly agreed with the statement “I enjoyed participating in this program” (M = 4.72 ± 0.46). Responses to “The classes or activities have enhanced my knowledge/skills about the topics” were similarly positive (M = 4.68 ± 0.48). There was also strong agreement with “The quality of the classes or activities and its content was high” (M = 4.60 ± 0.50) and “The classes or activities have provided me with information I can use” (4.60 ± 0.50).
One of the participants commented, “I think it’s a useful program, I think it’s very important. I think it’s useful not only for the researchers, but also for the people, and the participants. I did notice a lot the participants are pretty good and they ask what’s going on, and it changes their knowledge for the better.” Another, when asked what, if anything, had changed in their life after participating said, “I feel important. I feel like I make a difference. I feel like my voice needs to be heard more, and this is a platform in which it can be, and why not use more of it.” Participating in the program also encouraged students to take a more active role in their own health, that is, “I started digging deeper to find out more about the medications, about different ailments, as to how they affect people and what you can do.”
Presentations were developed by the original presenters, including six Emory faculty members, for example, the assistant program director for the Emory Center for Health in Aging, and faculty from Emory’s Schools of Medicine, Nursing, and Public Health. Each lecture was presented by an individual with interest or expertise aligning with the designated topic: for instance, the associate director of Emory’s Center for Ethics presented the lecture on ethics, and the assistant director of the Emory Center for AIDS Research (as both a researcher and advocate herself) presented Lecture 7 on effective advocacy within the research process. In our experience, faculty are often open to opportunities for community engagement and presenting to lay audiences, and inviting individuals with expertise or particular interest in the topic areas may enhance the quality and effectiveness of the program. Although no formal surveys were taken from faculty presenters, many gave verbal feedback that they enjoyed participating and found their interactions with our diverse group rewarding and enriching. Student moderators also gave positive feedback about their experience interacting with diverse older adult participants through the DREAMS Team classes.
By 6 months after the program’s end, DREAMS Team members had attended at least 20 community events, presented to groups (e.g., support groups, church groups, and at research socials) about research at least 11 times, and recruited more than 30 individuals into local studies. Importantly, 10 DREAMS Team trainees were paired with study teams (including study teams of clinical faculty presenters) as Community Advisory Board members or PSAs. The program thus succeeded in creating potentially lasting relationships between diverse older adults and clinical faculty and researchers and may have led to increased research participation.
Discussion
DREAMS, and in particular Part II, the DREAMS Team, fills a recognized need in scientific and medical communities for greater patient involvement and respect for patient input, as well as greater collaboration between myriad stakeholder groups. Throughout development of the DREAMS program, we received overwhelming support from a variety of faculty, student, and community stakeholders. We found that even the process of organizing and developing the DREAMS program initiated critical partnerships, which were built upon through the program itself upon implementation. For instance, the DREAMS program was made more successful through intense collaboration with our PSAs in all aspects of development and implementation, from determining questions to ask our first pre-program focus groups, to facilitating our crucial relationship with the Parkinson’s Disease Foundation’s PAIR program organizers, to disseminating project results. We also found that many faculty were happy to contribute to this mission, and connect with an important population of diverse, underserved older adults.
By design, DREAMS is intended to be a multi-directional exchange, in which presenters, health students, and diverse older adults can all learn from each other. Presenting for older adult stakeholders can help clinical faculty and students build relationships with diverse community members, and at the same time encourage and propagate the idea of involving input from older adults throughout the research process. Meanwhile, older adults can be empowered to find their voice in the research process through exposure to interactions with researchers who are willing to listen, who respect their questions, and who refrain from using condescending speech or behaviors. Future iterations will collect more formal feedback from participating health students and clinical faculty, to continue to meet educational and professional needs as the program evolves. The DREAMS Team lessons provide a curricular basis for a research advocacy training program, and an opportunity to facilitate discussions between stakeholders on all sides of the research process.
With increasing demand for patient-centered outcomes research and patient-centered health care, tools to develop and grow relationships between diverse older adults and the medical community are needed. The DREAMS Team program could feasibly be implemented in a variety of communities to successfully build connections between underrepresented individuals and clinical researchers. Plans are in process for continuing the DREAMS Team model at Emory, and disseminating the program to other sites, to continue to train community members to fill emerging, crucial roles as patient navigators, PSAs, and community advisory board members.
Acknowledgments
Funding
Research reported in this publication was partially funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (1099-EU). Additional support was provided through a National Parkinson Foundation (NPF) Community Grant (A-01).
Footnotes
Conflict of interest
The statements presented in this publication are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee. This manuscript has not been published elsewhere and has not been submitted simultaneously for publication elsewhere.
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/uedg.
References
- Austin-Wells V, Zimmerman T, & McDougall GJ (2003). An optimal delivery format for presentations targeting older adults. Educational Gerontology , 29 (6), 493–501. doi: 10.1080/713844396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basáñez T, Blanco L, Collazo JL, Berger DE, & Crano WD (2013). Ethnic groups’ perception of physicians’ attentiveness: Implications for health and obesity. Psychology, Health & Medicine, 18 (1), 37–46. doi: 10.1080/13548506.2012.672750 [DOI] [PubMed] [Google Scholar]
- Chalabi M (2014, April 22). All the presidents’ grandchildren. Retrieved April 10, 2017, from https://fivethirtyeight.com/datalab/all-the-presidents-grandchildren/
- Forsythe LP, Frank LB, Workman TA, Borsky A, Hilliard T, Harwell D, & Fayish L (2017). Health researcher views on comparative effectiveness research and research engagement. Journal of Comparative Effectiveness Research. doi: 10.2217/cer-2016-0063 [DOI] [PubMed] [Google Scholar]
- Hogan J (2015). Medical imaging workshop for seniors MedEdPORTAL Publications, 11, 10216. doi: 10.15766/mep_2374-8265.10216 [DOI] [Google Scholar]
- Kaiser BL, Thomas GR, & Bowers BJ (2017). A case study of engaging hard-to-reach participants in the research process: Community Advisors on Research Design and Strategies (CARDS)(R). Reseach in Nursing and Health, 40 (1), 70–79. doi: 10.1002/nur.21753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski MF, Adams EL, Cotugna N, Pohlig RT, Beydoun MA, Zonderman AB, & Evans MK (2016). Health literacy and education predict nutrient quality of diet of socioeconomically diverse, urban adults. Journal of Epidemiology and Preventative Medicine, 2 (1). doi: 10.19104/jepm.2016.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang R, Kelkar VA, Byrd JR, Edwards CL, Pericak-Vance M, & Byrd GS (2013). African American participation in health-related research studies: Indicators for effective recruitment. Journal of Public Health Management and Practice, 19 (2), 110–118. doi: 10.1097/PHH.0b013e31825717ef [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JH, Kilgore, ML, Goldman DP, Trimble EL, Kaplan R, Montello MJ, … Escarce JJ (2003). Participation of patients 65 years of age or older in cancer clinical trials. Journal of Clinical Oncology, 21 (7), 1383–1389. doi: 10.1200/JCO.2003.08.010 [DOI] [PubMed] [Google Scholar]
- Mayer RE (2003). Learning and Instruction. Upper Saddle River, NJ: Prentice-Hall. [Google Scholar]
- Medin DL, Ross BH, & Markman AB (2005). Cognitive psychology (4th ed.). Hoboken, NJ: Wiley. [Google Scholar]
- Parkinson’s Disease Foundation. (2017). Advocate for research. Retrieved from http://www.pdf.org/pair
- Perkins MM Dillard R Hart A Wincek R Hackney ME (In Review). A pre-intervention qualitative evaluation to inform implementation of a research participation enhancement and advocacy training program for diverse seniors: The DREAMS program. Journal of Applied Gerontology. [DOI] [PubMed] [Google Scholar]


