Abstract
Objective:
Current guidelines recommend high-priority treatment of severe sickle cell disease (SCD) pain with opioids; however, patients with SCD have historically been undertreated. We used mixed methods to assess pediatric residents’ perceptions towards opioid use in SCD pain management.
Methods:
We distributed a survey to 88 residents at an urban pediatric medical center in a cross-sectional study. Participants responded to questions about perceived barriers to acute SCD pain management and attitudes towards patients with SCD. Responses were examined using bivariate analyses. Five pediatric residents were interviewed, to provide more in-depth understanding of barriers to SCD pain management.
Results:
Fifty-three residents (60%) completed the survey. Participants were divided into “more experienced” (had seen ≥ 21 patients with SCD; 45.3%) or “less experienced.” Both groups reported potential for tolerance and dependence as major barriers to opioid use in SCD. Less experienced residents reported a greater need for additional training in SCD pain management (p<.05), more concern about addiction, and greater empathy for patients with SCD (p<.05). Both groups agreed that patients with SCD were “frustrating to care for.” Thematic analysis revealed that increased patient and provider barriers led to distrust, ultimately leading to under-treatment of pain and inadequate care.
Conclusion:
While more experienced residents reported feeling more comfortable treating acute SCD pain and were less concerned with addiction compared with less experienced residents, certain negative views of patients with SCD were prevalent amongst all residents. Findings suggest that residency training must address provider attitudes as well as knowledge about SCD.
Keywords: sickle cell disease, pain, opioids, medical education
Introduction
Sickle cell disease (SCD) is a genetic disorder that causes erythrocytes to become rigid and “sickle” shaped, causing episodes of severe pain, termed vaso-occlusive episodes (VOE)1. VOEs are associated with microvascular occlusion and tissue ischemia, which can cause increased morbidity and mortality2. The National Heart, Lung and Blood Institute’s (NHLBI) recently published guidelines for SCD management recommend immediate and high priority treatment for patients with SCD presenting with VOE, with opioids recommended as the first line treatment3. While opioids are a necessity in SCD pain management, challenges in the use of opioids with any patient includes respiratory, cognitive, and psychomotor side effects, as well as the potential for misuse4.
It is well documented that sickle cell pain is often undertreated5–7. Negative provider attitudes towards patients with SCD have been shown to present significant barriers to patients receiving adequate pain management7. Studies have shown that some healthcare providers hold false beliefs that patients with SCD are drug-seeking, drug-abusing, or manipulative7. There is often a lack of trust on the part of both providers and patients, inadequate knowledge in the medical community about SCD treatment, and an overall inequity in access to adequate SCD care5. Furthermore, the current opioid epidemic has heightened the medical community’s awareness and fear of prescribing opioids. As a result, physicians today may be more cautious in prescribing opioids, even in the treatment of VOE8. Little research has been done into medical residents’ attitudes towards patients with SCD. This study is the first to our knowledge to specifically evaluate residents’ perceptions and attitudes about SCD and pain management. Our aim was to assess perceived barriers to pain management in SCD, attitudes toward caring for patients with SCD, and whether clinical experience influences these outcomes.
Methods
This study was conducted as part of a larger initiative funded by NHLBI, the Sickle Cell Disease Implementation Consortium (SCDIC). The SCDIC was established to use implementation science9 to address the pervasive and longstanding disparities that youth and adults with SCD face in receiving acute and preventative care. The SCDIC investigators developed a set of survey and qualitative tools to conduct needs assessments of barriers to care at participating sites. We modified the SCDIC instruments to create surveys and interviews that we administered to pediatric residents at UCSF Benioff Children’s Hospital Oakland (BCHO).
Participants
Eighty-eight pediatric residents at BCHO, an urban pediatric medical center in California, were eligible to participate. Five of the pediatric residents volunteered for separate individual interviews on pain management in SCD. All study procedures were approved by the BCHO Institutional Review Board.
Instrumentation
We distributed a survey (online) to all BCHO pediatric residents via an email list serve and also announced and handed out a paper version to them at their monthly residency meeting. The survey consisted of 13 questions, including demographics (age, ethnicity, race, gender, and year of residency), approximate numbers of patients with SCD seen clinically, comfort level in treating patients with SCD, perceived barriers to treatment of VOE with opioids, and attitudes towards patients with SCD (Supplementary File). Survey questions about barriers to pain management were adapted from a survey about a range of chronic nonmalignant pain conditions10. Questions about attitudes towards patients with SCD were modified from questions previously developed for emergency department providers11. Participants’ completion of the survey served as their consent to be in the research study.
Interviews
The residents’ interview questions were adapted from the semi-structured interview guides from the SCDIC needs assessment qualitative data collection. Interview topics included an introductory section on the residents’ experience with SCD, primary and specialty care, hydroxyurea treatment, opioids and pain, and emergency department management (interview guide available upon request). For this study, only interview topics including experience level with SCD and pain management were coded and analyzed. Each interview for the five participating residents took about 30–45 minutes to complete and was conducted by an interviewer (AF) and a note taker (JK). Audio recordings of each interview were transcribed by a professional transcription service and the research team reviewed transcripts for accuracy prior to coding.
Data Analysis
All survey data was collected and organized in a Research Electronic Data Capture (REDCap12), a secure, web-based research database. Survey responses were exported to Stata v. 13.1 for analysis. Descriptive statistics were computed and bivariate analyses assessed associations between variables of interest. Significance level was set at p< .05. Differences between residents with clinical experience caring for 21 or more patients with SCD compared to those who had cared for fewer than 21 patients with SCD were examined using chi-square analyses. Variations in survey responses between the two groups to questions on comfort level in SCD pain management, perceived barriers to treatment of VOE with opioids, and attitudes towards patients with SCD were examined.
The interview transcripts were imported into NVivo, a qualitative database (qsrinternational.com), and analyzed using thematic analysis13. We used successive coding passes to identify common themes and codes within the interview transcripts. Themes and codes were organized into a descriptive framework of the residents’ ideas and experiences with opioids in treatment of sickle cell related pain episodes (codebook available upon request). One researcher (AF) created the initial codebook and themes were discussed with the senior researcher (MJT) to verify the validity of the codebook. Trained research assistants for the larger SCDIC study at BCHO coded the interviews. The research assistants met frequently with the senior researcher to insure accuracy and consistency in coding and to resolve any discrepancies by consensus. The semi-structured interviews were conducted with the pre-specified plan to achieve saturation in codes and themes14.
Results
Fifty-three of 88 (60.2%) residents completed the survey (Table 1). The majority of the 53 participants were female (69.8%), aged 25–29 years (67.9%), and white (51.0%). All participants reported clinical experience with at least one patient with SCD during their medical career. Residents who reported clinical experience with 21 or more patients with SCD (45.3%) were categorized as “more experienced” residents, and those who reported having seen fewer than 21 patients with SCD were categorized as “less experienced.”
Table 1.
Characteristics of pediatric residents (n = 53) who participated in the survey
| Characteristic | n (%) |
|---|---|
| Gender | |
| Female | 37 (69.8%) |
| Male | 16 (30.2%) |
| Age Category | |
| 25 – 29 years | 36 (67.9%) |
| 30 – 34 years | 15 (28.3%) |
| 35 years and older | 2 (3.8%) |
| Racea | |
| Asian | 22 (43.1%) |
| African-American/Black | 1 (2.0%) |
| White | 26 (51.0%) |
| Other | 6 (11.8%) |
| Ethnicity | 6 (11.5%) |
| Hispanic | |
| Year of Pediatric Residencyb | |
| First | 14 (26.9%) |
| Second | 17 (32.7%) |
| Third | 21 (40.4%) |
| Number of patients with SCD seen clinically | |
| 1 – 20 patients | 29 (54.7%) |
| 21 or more patients | 24 (45.3%) |
Totals add up to greater than 100% as more than one race could be selected
One respondent did not provide this information
More experienced residents (n = 24) reported feeling significantly more comfortable (responded “somewhat comfortable” or “very comfortable”) in treating acute pain in SCD compared with less experienced residents (n = 29; 79.2% vs. 44.8%; p<.05). Table 2 compares more experienced to less experienced residents’ responses to potential barriers to opioid use in treatment of VOE. Many of the total sample of residents reported tolerance (52.8%) and dependence (45.3%) as major barriers to use of opioids in treatment of VOE. Few residents reported regulatory oversight (13.2%) as a major barrier to opioid use. There was a high rate of “do not know” responses to the diversion question among both groups of residents. Less experienced residents reported lack of training as a significantly greater barrier compared with more experienced residents (16.7% vs. 51.7%; p<.05). Less experienced residents also tended to report addiction as a greater barrier to pain management compared with more experienced residents (44.8% vs. 29.2%; p=.058).
Table 2.
Percent of residents (n = 53) responding that each perceived barrier to treatment of VOE with opioids was a “moderate” or “complete” barrier
| Less Experienced (n = 29) | More Experienced (n = 24) | |
|---|---|---|
| n (%) | n (%) | |
| Tolerance | 16 (55.2%) | 12 (50.0%) |
| Lack of training | 15 (51.7%) | 4 (16.7%)* |
| Dependence | 13 (44.8%) | 11 (45.8%) |
| Addiction | 13 (44.8%) | 7 (29.2%) |
| Regulatory oversight | 5 (17.2%) | 2 (8.3%) |
| Potential for diversion | 2 (6.9%) | 2 (8.3%) |
p < .05
Table 3 shows responses to attitudinal statements about patients with SCD. The majority of residents (62.3%) reported that patients with SCD “are frustrating to take care of.” Few residents reported that patients with SCD “over-report their pain” (11.3%), but few also expressed that patients with SCD “make me feel glad I went into medicine” (20.8%). Less experienced residents reported that they felt that patients with SCD are significantly easier to empathize with, compared to more experienced residents (69.0% vs. 41.7%; p<.05).
Table 3.
Percent of residents responding to positive or negative attitude statements about patients with sickle cell disease (SCD) with “somewhat” to “strongly” agree
| Less Experienced (n = 29) | More Experienced (n = 24) | |
|---|---|---|
| n (%) | n (%) | |
| Patients with SCD…. | ||
| Are easy to empathize with | 20 (69.0%) | 10 (41.7%)* |
| Are frustrating to care for | 16 (55.2%) | 17 (70.8%) |
| Make me glad I went into medicine | 8 (27.6%) | 3 (12.5%) |
| Over-report pain | 3 (10.3%) | 3 (12.5%) |
p < .05
The five pediatric residents who were interviewed were primarily female (80%), white (60%), aged 30–34 years (60%), and categorized as “more experienced” residents (60%). The five narratives provided more in-depth understanding of our survey findings, and saturation was achieved with consistent codes and overarching themes generated (Supplementary Table S1). The first theme was related to provider barriers and included fear of over-prescription, concerns about worrisome behaviors (such as non-adherence), institutional barriers (such as insurance coverage, lack of SCD resources, etc.), and challenges with managing pain due to its subjectivity. The most common patient-level barrier cited was psychosocial difficulties, sub-categorized as social stressors, stigma, and discrimination. Additional patient-level barriers included patients’ lack of follow-up/non-adherence and structural barriers (housing, transportation, financial, etc.). The third theme touched on facilitators of care, including access to pain plans in the electronic medical record (EMR) and positive communication between patients and providers within the context of longer term relationships.
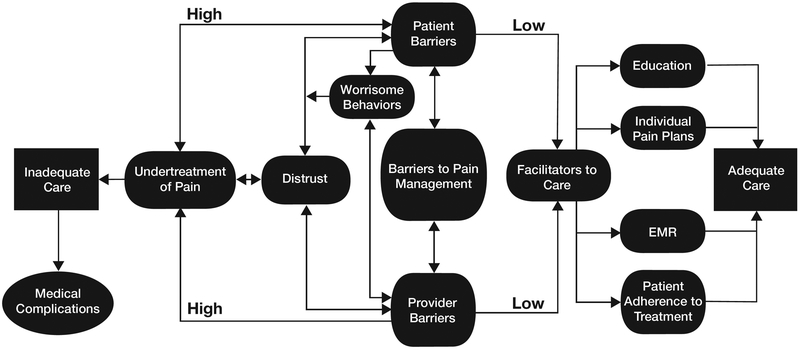
We organized these themes and codes into a preliminary schematic illustrating how patient and provider barriers might lead to distrust within the patient-provider relationship, ultimately leading to under-treatment of pain and inadequate care of patients with SCD (Figure 1). The interviewees described patients with increased barriers as commonly having more distrust of the healthcare system, often due to negative past medical experiences and inadequate care. Interviewees expressed that providers seemed to be more distrustful of patients with increased barriers and had more difficulty caring for them. Barriers included psychosocial problems, “worrisome behaviors” (“red flag” behaviors that are associated with drug-seeking behavior or addiction), and lack of follow up/non-adherence.
Figure 1.
Themes identified from residents’ interviews organized into preliminary schematic illustrating how patient and provider barriers might lead to distrust within the patient-provider relationship, under-treatment of pain and inadequate care of patients with SCD.
The interviewees noted that more positive views of patients with SCD could be developed with more outpatient exposure to “healthier kids.” They commented on increased trust in the patient-provider relationship that could be established when patients had a long-standing outpatient relationship with the medical providers who “know their story…background and history.” Residents reported that inclusion of patients’ individualized pain plans or documentation of the patients’ adherence to treatment could contribute to more positive provider-patient relationships. Stronger relationships contributed to fewer barriers to care, increased patient-provider communication, and a perceived decrease in under-treatment of pain. Additionally, provider education about SCD and pain management led to increased perceptions of quality of care.
Discussion
We describe, for the first time, perspectives of pediatric residents about barriers to pain management in SCD and their attitudes toward caring for patients with SCD, considering level of experience with caring for patients with SCD as a differentiating factor. We found that residents that we surveyed reported concerns about tolerance and dependence as major barriers to use of opioids in treatment of acute pain in SCD. Both tolerance (caused by adaptations in neuronal cells resulting in decreased pharmacological effects of a dose of a drug with repeated use) and physiological dependence (neuronal changes that require continued administration of a drug to prevent withdrawal symptoms) are legitimate concerns in the use of opioids15. These concerns are a result of limited pharmacologic options for SCD treatment and present yet another barrier to SCD care.
Less experienced residents were more likely to perceive addiction as a greater barrier to use of opioids in treatment of VOE than more experienced residents. Studies have shown that providers often assume much higher rates of addiction in the SCD community than actual rates show16. One study showed that medical residents and nurses perceived higher rates of opioid dependence in patients with SCD than physicians; while all groups’ perceptions were still much higher than the actual rates of opioid dependence15. While many providers are concerned about addiction, dependence, and potential overdose in patients with SCD, a recent study showed that of the 12,261 total deaths of patients with SCD from 1999 to 2013, only 0.77% (n=95) were related to opioid pain relievers8. This is considerably lower than most other non-cancer disorders such as fibromyalgia (4.4%), low back pain (2.1%), and migraines (4.5%)8. Barriers and provider fears related to the opioid epidemic thus are often incorrectly generalized to patients with SCD, even when use of opioids is necessitated in treatment of VOE. While it is possible that training in the context of the opioid epidemic has negatively affected the BCHO residents’ views and use of opioids in SCD pain management, our findings did not support this claim. Regardless of level of training, concerns about regulatory oversight in relation to opioid use was rarely cited as an issue by participants in this study. The high rate of “do not know” responses” to the question on diversion may have been due to residents being unsure if patients were diverting their home opioid prescriptions. The term “diversion” is highly publicized within the context of the opioid crisis17, so we can speculate that this is indeed what the residents meant by their responses. Unfortunately, the interviews did not inform this particular question.
More than half of the less experienced residents identified lack of training as a barrier to the use of opioids in the treatment of VOE, a statement that was also articulated throughout the interviews. This highlights the need for targeted education early in residency training so that physicians develop the skills to safely and responsibly provide effective, evidence-based treatments for patients in pain. A variety of curricular approaches, including traditional didactic sessions, experiential case-based methods, patient panels, and digital toolkits can be utilized by training programs to better equip residents to care for patients with pain and attend to those who develop substance use disorders7.
Our qualitative analysis of the residents’ perceptions supported the idea that residents of varying levels of experience felt that SCD should be considered as a separate category compared to other chronic nonmalignant pain requiring treatment with opioids. Our analysis also captured how a vicious cycle can ensue wherein providers do not trust patients who question their ability to adequately manage SCD pain, and patients escalate in requests for more pain medications and/or increase monitoring of their health care providers. Our findings are consistent with previous reports from adults with SCD about their reluctance to seek needed care even when faced with potentially life-threatening complications or severe pain, due to negative interactions with providers18,19. Lack of adherence among adults with SCD has also been associated with patients’ negative interpersonal experiences and lower levels of trust in their providers20,21.
Certain negative views, such as “patients with SCD are frustrating to take care of,” were prevalent amongst the pediatric residents. Qualitative analyses provided insights into the complexity of barriers that patients with SCD often face, including their disease and its complications, psychosocial barriers, and distrust of the healthcare system, as a potential reason for negative provider attitudes. These findings are consistent with SCD literature which show how negative provider attitudes can diminish trust in a patient-provider relationship, resulting in inadequate care7. Previous studies have also shown that negative provider attitudes are associated with higher volumes of patients with SCD as well as decreased provider adherence to NHLBI guidelines in treatment of acute SCD pain22, potentially increasing the morbidity and mortality of patients with SCD. Higher volumes of patients could result in increased frustration due to increased barriers to care and “empathy fatigue”23, potentially explaining why we found that more experienced residents reported less empathy for patients with SCD than less experienced residents. Research that has demonstrated that videos of firsthand experiences from patients with SCD can be effective in improving attitudes towards patients with SCD can inform efforts to support residents in maintaining empathy over time7. Exposure to “healthier kids” in the outpatient setting was cited in this study as critical to maintaining a perspective on the few patients who may need frequent hospital admissions and ED visits.
A prior study found that pediatric providers had more positive attitudes towards patients with SCD than adult providers22. While our study did find negative attitudes amongst pediatric residents, future studies should compare attitudes between residents who provide care for children versus adult patients with SCD, including a broad range of residency training programs. This could allow us to gain a better understanding of challenges in the care of patients with sickle cell disease encountered in a diversity of settings. Future studies should also investigate whether negative attitudes translate into decreased adherence to NHLBI guidelines in treatment of VOE and decreased quality of SCD care. Prospective evaluation of the effectiveness of strategies aimed at tackling some of the negative attitudes and deficiencies that emerge early on in residency training are also needed.
This study has several limitations. First, the study population was from one hospital with a well-established comprehensive sickle cell center. The BCHO residency program does represent a diverse segment of the national pediatric residency population with trainees that hail geographically from all around the country. Furthermore, our sickle cell population mirrors that of other major national programs with regard to patient socio-demographics. The authors acknowledge that the single center design limits the external validity of the study despite the representative patient and residency population. However, surveying another residency program is beyond the scope of the project at this time.
Second, although there was an adequate survey return rate, the small sample size and volunteer basis of the study may still be considered a limitation. Third, the surveys are subject to self-report bias and therefore, the survey response data may or may not reflect the actual behaviors or thoughts of residents, although residents still willingly expressed a range of negative views about patients with SCD. Finally, we recognize that our qualitative analysis can only contribute to a preliminary model of how patient and provider barriers might lead to distrust within the patient-provider relationship, and ultimately lead to undertreatment of SCD related pain. However, responses from the five residents were quite consistent and the themes were consistent with other literature.
Conclusion.
Both survey and interview data showed that pediatric residents perceived a number of barriers to acute SCD pain management and endorsed certain negative views of patients with SCD. These biases may contribute to the ongoing disparities in care encountered by patients with SCD. We believe that the information gleaned from this mixed methods research will help inform the development of strategies to better educate residents about SCD. Cultural humility24,25 and exposure to first-person accounts of patient perspectives, whether via videos or the opportunity to provide preventive care, rather than exclusively inpatient or ED care, may help providers remain patient-centered. Focused exploration of both explicit and implicit biases may be key to mitigating ongoing disparities in the care of patients experiencing vaso-occlusive pain. Through this research, we aim to enhance medical residents’ SCD education to encompass their attitudes as well as knowledge, thereby contributing to the development of a workforce that provides better care for patients with SCD.
Supplementary Material
Supplementary File 1. Survey distributed to residents
Acknowledgements:
Research reported in this publication was supported by the National Heart, Lung and Blood Institute of the National Institutes of Health under Award Number U01HL134007 (Marsha Treadwell and Elliott Vichinsky, PIs). The research was also supported by a grant from the National Institutes of Health R25 #HL125451: Short Term Research Education Program to Increase Diversity in Health Related Research/Bay Area Summer Research Internship Program (Bertram Lubin and Ellen Fung, PIs). These funders did not have any role in study design; in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to support the article for publication. The authors wish to thank the Graduate Medical Education/Pediatric Residency Program at UCSF Benioff Children’s Hospital Oakland for their support, and Natasha Dean for her assistance with the preparation of the manuscript.
List of abbreviations
- BCHO
UCSF Benioff Children’s Hospital Oakland
- EMR
Electronic medical record
- NHLBI
National Heart, Lung and Blood Institute
- REDCap
Research Electronic Data Capture
- SCD
Sickle Cell Disease
- SCDIC
Sickle Cell Disease Implementation Consortium
- UCSF
University of California San Francisco
- VOE
Vaso-occlusive episode
Footnotes
Conflict of Interest Statement: None, for all authors.
References
- 1.McClish DK, Smith WR, Levenson JL, et al. Comorbidity, Pain, Utilization, and Psychosocial Outcomes in Older versus Younger Sickle Cell Adults: The PiSCES Project. Biomed Res Int. 2017;2017:4070547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGann PT, Nero AC, Ware RE. Current management of sickle cell anemia. Cold Spring Harb Perspect Med. August 1 2013;3(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. September 10 2014;312(10):1033–1048. [DOI] [PubMed] [Google Scholar]
- 4.Wallwork RS, Chipidza FE, Stern TA. Obstacles to the Prescription and Use of Opioids. Prim Care Companion CNS Disord. 2016;18(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maxwell K, Streetly A, Bevan D. Experiences of hospital care and treatment seeking for pain from sickle cell disease: qualitative study. BMJ. June 12 1999;318(7198):1585–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Labbe E, Herbert D, Haynes J. Physicians’ attitude and practices in sickle cell disease pain management. J Palliat Care. Winter 2005;21(4):246–251. [PubMed] [Google Scholar]
- 7.Haywood C Jr., Williams-Reade J, Rushton C, Beach MC, Geller G. Improving Clinician Attitudes of Respect and Trust for Persons With Sickle Cell Disease. Hosp Pediatr. July 2015;5(7):377–384. [DOI] [PubMed] [Google Scholar]
- 8.Ruta NS, Ballas SK. The Opioid Drug Epidemic and Sickle Cell Disease: Guilt by Association. Pain Med. October 2016;17(10):1793–1798. [DOI] [PubMed] [Google Scholar]
- 9.King AA, Baumann AA. Sickle cell disease and implementation science: A partnership to accelerate advances. Pediatr Blood Cancer. November 2017;64(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grahmann PH, Jackson KC 2nd, Lipman AG. Clinician beliefs about opioid use and barriers in chronic nonmalignant pain. J Pain Palliat Care Pharmacother. 2004;18(2):7–28. [PubMed] [Google Scholar]
- 11.Freiermuth CE, Haywood C Jr., Silva S, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Adv Emerg Nurs J. Oct-Dec 2014;36(4):335–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. April 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Creswell JW. Qualitative inquiry and research design: Choosing among five traditions. 2nd ed Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- 14.Braun V, Clarke V. Successful qualitative research: A practical guide for beginners. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- 15.Waldrop RD, Mandry C. Health professional perceptions of opioid dependence among patients with pain. Am J Emerg Med. September 1995;13(5):529–531. [DOI] [PubMed] [Google Scholar]
- 16.Zempsky WT. Treatment of sickle cell pain: fostering trust and justice. JAMA. December 9 2009;302(22):2479–2480. [DOI] [PubMed] [Google Scholar]
- 17.Berge KH, Dillon KR, Sikkink KM, Taylor TK, Lanier WL. Diversion of drugs within health care facilities, a multiple-victim crime: patterns of diversion, scope, consequences, detection, and prevention. Mayo Clin Proc. July 2012;87(7):674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Treadwell MJ, Hassell K, Levine R, Keller S. Adult sickle cell quality-of-life measurement information system (ASCQ-Me): conceptual model based on review of the literature and formative research. Clin J Pain. October 2014;30(10):902–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evensen CT, Treadwell MJ, Keller S, et al. Quality of care in sickle cell disease: Cross-sectional study and development of a measure for adults reporting on ambulatory and emergency department care. Medicine (Baltimore). August 2016;95(35):e4528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haywood C Jr., Lanzkron, Ratanawongsa N, Bediako SM, Lattimer-Nelson L, Beach MC. Hospital self-discharge among adults with sickle-cell disease (SCD): associations with trust and interpersonal experiences with care. J Hosp Med. May-Jun 2010;5(5):289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haywood C Jr., Lanzkron S, Bediako S, et al. Perceived discrimination, patient trust, and adherence to medical recommendations among persons with sickle cell disease. J Gen Intern Med. December 2014;29(12):1657–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glassberg JA, Tanabe P, Chow A, et al. Emergency Provider Analgesic Practices and Attitudes Toward Patients With Sickle Cell Disease. Ann Emerg Med. April 2 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jablow M. Compassion Fatigue: The Toll of Being a Care Provider. 2017.
- 24.Ansari A. Battling biases with the 5 Rs of cultural humility. 2017. Accessed January 02, 2017.
- 25.Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. May 1998;9(2):117–125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary File 1. Survey distributed to residents