Abstract
Animal experiments have confirmed that mesenchymal stem cells can inhibit motor neuron apoptosis and inflammatory factor expression and increase neurotrophic factor expression. Therefore, mesenchymal stem cells have been shown to exhibit prospects in the treatment of amyotrophic lateral sclerosis. However, the safety of their clinical application needs to be validated. To investigate the safety of intrathecal injection of Wharton’s jelly-derived mesenchymal stem cells in amyotrophic lateral sclerosis therapy, 43 patients (16 females and 27 males, mean age of 57.3 years) received an average dose of 0.42 × 106 cells/kg through intrathecal administration at the cervical, thoracic or lumbar region depending on the clinical symptoms. There was a 2 month interval between two injections. The adverse events occurring during a 6-month treatment period were evaluated. No adverse events occurred. Headache occurred in one case only after first injection of stem cells. This suggests that intrathecal injection of Wharton’s Jelly-derived mesenchymal stem cells is well tolerated in patients with amyotrophic lateral sclerosis. This study was approved by the Bioethical Committee of School of Medicine, University of Warmia and Mazury in Olsztyn, Poland (approval No. 36/2014 and approval No. 8/2016). This study was registered with the ClinicalTrials.gov (identifier: NCT02881476) on August 29, 2016.
Keywords: amyotrophic lateral sclerosis, stem cells therapy, intrathecal injections, Wharton’s jelly-derived mesenchymal stem cells, adverse events, safety, cerebrospinal fluid, neural regeneration
Chinese Library Classification No. R459.9; R741
Introduction
Amyotrophic lateral sclerosis (ALS) is a devastating and fatal disease with median survival from 37 to 49 months (Jablecki et al., 1989), which in its classical form affects both central and peripheral motor neurons (Stifani, 2014). There are two forms of ALS: sporadic (SALS) and familial (FALS) (Turner et al., 2013) but only about 5–10% of all cases are considered as FALS (Andersen and Al-Chalabi, 2011). In two-thirds of familial ALS cases and approximately 11% of sporadic ALS cases, several causative genes are the cause of the disease (Siddique et al., 1991; Rosen et al., 1993; Fecto et al., 2011; Renton et al., 2014). In other cases, the pathological factor which is responsible for this disease is still elusive (Logroscino et al., 2008). The prevalence of ALS is about 2/100000 (range from 1/100000 to even 8/100000 in some regions of Europe)(Chio et al., 2013; Rosenbohm et al., 2018). The main clinical symptoms of ALS comprise progressive muscle weakness, muscle atrophy, dysphagia, and dysarthria. In the last phase of the disease, respiratory failure occurs which is associated with respiratory muscle weakening. In rare cases, respiratory failure onset may be present (Rowland and Shneider, 2001; Kano et al., 2013). The diagnosis of ALS is established by clinical investigation and confirmed by electromyography (EMG) after excluding other diseases (Goutman, 2017).
The pathophysiology of this disease is still unknown (Gordon, 2011; Morgan and Orrell, 2016), although there are theories that may indicate the direction for researchers and drug inventors. Sequences of events may be divided into three steps. Some genetic, environmental or developmental factors (the 1st step) cause inappropriate glial activity, RNA/protein mishandling, excitotoxicity or oxidative stress (the 2nd step) and these processes lead to clinical features of ALS (the 3rd step) (Turner et al., 2013). Following this way of thinking, patients are given the hope for disease-modifying drug.
Tests conducted on animal models made it possible to introduce a hypothesis of intermediate MSCs (Mesenchymal Stem Cells) impact on ALS course, owing to application of growth factors, modulation of glial cells secretome and increased activity of T-regulatory lymphocytes (Treg). MSCs have been shown to play a role in protecting motoneurons, astrocytes, microglia, and they could also impact on their apoptosis (Forostyak and Sykova, 2017). Modulation of inflammatory response through decreasing the expression of tumor necrosis factor α (TNFα), interleukin-6 (IL-6), and nitric oxide synthase (iNOS) cytokines was also observed (Sun et al., 2014). Neuropathological tests showed an increased number of motor neurons at the lumbar level of the spinal cord, as well as an increased level of glial cell-derived neurotrophic factor (GDNF) and fibroblast growth factor (bFGF) on the murine model (Marconi et al., 2013). Thus, investigators put forward a hypothesis that ALS treatment with MSC application could result in an intensification of neuroprotective properties, which modulate biological functions of local glial cells (Marconi et al., 2013).
Combined culture of MSCs and peripheral blood mononuclear cells obtained from ALS patients resulted in an increased secretion of anti-inflammatory cytokines, including IL-4, IL-10, TGF-β, and growth of T-regulatory lymphocytes (Treg) (Kwon et al., 2014). A smaller quantity of Treg is a factor positively correlating with faster ALS progression (Henkel et al., 2009; Thonhoff et al., 2018). Endogenous Tregs are a factor associated with slower development of the illness (Beers et al., 2011, 2017). The impact of T cells on ALS was proved on animal models (Tada et al., 2011). T cells can have an impact on the microglial phenotype due to the secretion of cytokines that transform their phenotype from M1 into M2. M1-phenotype cells secrete superoxide radicals and pro-inflammatory cytokines while M2-phenotype cells play a vital role in tissue remodeling and repair process (Zhao et al., 2006; Tang and Le, 2016). Immunologic dysregulation of monocytes can also play a role in ALS pathogenesis. CD14+CD16– monocytes, originating from ALS patients, had weakened ability of chemotaxis and expression of adhesion molecules and, at the same time, the percentage of CD14+CD16+ monocytes was also decreased, which was negatively correlated with ALSFRS-R scale result (Cui et al., 2013).
The above described mechanisms prove the presence of multi-level interactions between cells in the organism of the ill and administered MSCs. Understanding the mechanisms owing to which MSCs create in vivo an environment leading to cell and tissue regeneration is the key to working out an effective therapeutic method taking advantage of MSC in ALS treatment. MSCs can be obtained from different sources, i.e., bone marrow (BM-MSC), adipose tissue (AT-MSC), embryonic tissue (E-MSC), cord blood (CB-MSC), reprogramming of mature cells (iMSC) and perinatal tissue – Wharton’s jelly (WJ-MSC) and amniotic membrane (Hass et al., 2011). WJ-MSC may be the easiest way to obtain MSCs and there are no ethical controversies (Frausin et al., 2015). Ex vivo experiment confirmed that WJ-MSCs maintain their immunomodulatory property through a long-term culture and preserve genetic stability for up to 15 passages without chromosomal changes and malignant transformation both in vitro and after MSCs injection into nude mice with a follow-up period of 4 weeks (Chen et al., 2014). Preclinical studies showed that MSCs express 12 neural genes and 11 transcription factors and are able to differentiate into neural and glial cells in appropriate media (Blondheim et al., 2006). Secretion of neurotrophic factors by MSCs may contribute to maintenance of motor neurons and glial cells in good condition. The life of neurons (including the life of motor neurons) depends on the proper state of glial cells (Lewis et al., 2014).
There is no really curable therapeutic method that can be proposed for ALS patients (Petrov et al., 2017). One existing pharmaceutic product – riluzole – can prolong life for about 3 months (Bensimon et al., 1994; Miller et al., 2007; Jaiswal, 2018). Nevertheless, the mechanism of action of this drug is not fully understood. Influence on oxidative stress and excitotoxicity is considered as a potential mechanism of action (Moujalled and White, 2016). The huge demand for a drug that could slow down the progress of the disease allowed FDA to accept (in May 2017) new drug for ALS known as edaravone (Mora, 2017; Rothstein, 2017; Writing and Edaravone, 2017). In a post hoc analysis, this molecule slowed down the disease progression measured by ALSFRS-R scale. The mechanism of action is based on free radical scavengers that can cross the blood-brain barrier (Writing and Edaravone, 2017). That drug has also an indication to use in acute phase of ischemic stroke (AIS) (Kikuchi et al., 2012).
The hope for ALS patients relies on a therapy with stem cells (Czarzasta et al., 2017). This study focuses on the safety of intrathecal injections of WJ-MSC as the therapy for ALS.
Subjects and Methods
Subjects
Study was conducted by the Instytut Terapii Komórkowych w Olsztynie (Cell Therapies Institute, FamiCord Group), Poland in cooperation with the Department of Neurology and Neurosurgery, School of Medicine, Collegium Medicum - University of Warmia and Mazury in Olsztyn, Poland and the University Clinical Hospital in Olsztyn, Poland. The study was approved by the Bioethical Committee of School of Medicine, University of Warmia and Mazury in Olsztyn, Poland (ethical approval No. 36/2014 in June 2014 and No. 8/2016 in February 2016). This study was performed in accordance with the Declaration of Helsinki. Patients involved in the study were recruited between April and December 2016 and signed a written informed consent.
The inclusion criteria are as follows: a) clinical diagnosis of definite ALS based on the El Escorial World Federation of Neurology criteria (i.e., electromyography testing was used to support the clinical diagnosis) (Brooks, 1994; Brooks et al., 2000); b) ventilator independent; c) age between 20 and 75 years; d) ability to visit the clinic with support or alone. Every patient had a blood test for the levels C-reactive protein (CRP), sodium, potassium, glucose, morphology, coagulation system, urea, creatinine and examination of the bottom of the eye. The exclusion criteria are as follows: a) medical or inflammatory disorders markedly interfering with the results of the therapy; b) active infections; c) severe cardiac insufficiency; d) severe renal or liver insufficiency.
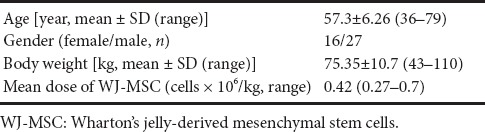
Forty-three patients, consisting of 16 females and 27 males, aged 57.3 years, were included in the final analysis. The mean weight of patients was 75.35 kg at the beginning of the therapy. The mean dose of WJ-MSC in one intrathecal injection was 0.42 × 106 cells/kg (Table 1). All patients were treated with riluzole 100 mg in 2 doses per day.
Table 1.
Demographic and patient-referred data
WJ-MSC preparation and implantation procedure
WJ-MSC, the part of the cord tissue, was obtained through the standard method during the childbirth, after a written consent had been received from the mother and stored in a stem cell bank - Polski Bank Komórek Macierzystych (PBKM, FamiCord Group). PBKM was also responsible for production of ATMP (Advanced Therapy Medicinal Product) for individual injections.
Human umbilical cords (n = 3) were obtained aseptically from full-term uncomplicated pregnancies with planned cesarean section (Written informed consent was obtained from each participant prior to the inclusion in the study). Cells were isolated using the explant isolation method, as described elsewhere, with minor modifications (Struys et al., 2011). After immersion in a sterile vessel containing 0.01 M phosphate-buffered saline (PBS, pH 7.2) supplemented with 1% penicillin-streptomycin (10,000:10,000; Sigma-Aldrich, St. Louis, MO, USA), the cords were transferred to the laboratory for further cell isolation. The cords were cut into small pieces (1–2 cm in length) and transferred to 60 × 15 mm Petri dishes, containing DMEM/F-12, GlutaMAX™ supplemented with 1% P/S and 10% fetal bovine serum (FBS; Sigma-Aldrich), and incubated at 37°C in a humidified atmosphere containing 5% CO2 for future culture.
Before implantation, the cells were maintained in basal MSC medium without serum, detached, and washed three times with PBS 1× and once with autologous cerebrospinal fluid. The cells were suspended in about 1 mL of autologous cerebrospinal fluid for all patients (Ge et al., 2015). During the study, 91 injections were performed: 14 patients received 3 injections, 20 patients received 2 injections, and 9 patients received 1 injection. The interval between two injections was 2 months. Adverse events were evaluated for 6 months. An average amount of 30 × 106 cells were injected intrathecally into the cervical, thoracic or lumbar region depending on the clinical symptoms by the same neurosurgeon.
Results
This study was designated to assess the safety of intrathecal injections of WJ-MSC as a therapy for ALS, which had no alternative treatment method. No serious adverse events (SAE) were observed during this study at the University Clinical Hospital and Instytut Terapii Komórkowych w Olsztynie (Cell Therapies Institute, FamiCord Group). Only one adverse event, i.e., headache (2.3% of the entire sample) was recorded during the first injection of WJ-MSC in a 62-year-old male who weighed 80 kg at the start of therapy. It was considered not serious by the physicians who conducted the study and resolved spontaneously after injection. The dose of WJ-MSC was 0.375 × 106 cells/kg – below the mean dose of the whole studied group. There was no any problem during the next two injections in this patient. No other adverse events were reported. Only adverse event occurring in one case was related to lumbar puncture. It manifested as a headache without any other signs and abnormalities at neurological examination. This can be explained in two ways: 1) neurosurgeons took a sample of 2 cm cerebrospinal fluid while puncturing the lumbar region and after that WJ-MSC mixture was injected into the spinal canal. There was no post-puncture lumbar syndrome observed because there was no leakage of cerebrospinal fluid. After the procedure, the patient had to lie for 3 hours, received intravenous injection of 1 mL of isotonic fluid immediately after the puncture, another 1 L of isotonic fluid 12 hours later, and 2 L of oral liquid per day. 2) All procedures were performed by highly trained neurosurgeons, with the utmost precision that neurosurgeons put.
Discussion
The first use of MSCs in a clinical setting of ALS was reported by Mazzini et al (2003). The investigators concluded that MSCs administration in ALS patients appeared to be safe and well-tolerated. No serious adverse events were present. Minor adverse events were as follows: four patients with intercostal pain in four patients and leg sensory dysesthesia in four patients (Mazzini et al., 2003). The route of administration of MSCs and the source of MSCs (allogeneic) were different in comparison to our study. The same patients were evaluated 4 years after the MSC therapy. During this time period, four patients died because of respiratory complications. Another patient was treated for pneumonia 24 months after implantation of MSC and tracheostomy was done. Sixteen months later, this patient died due to pulmonary disease. A slowdown of the decline of the forced vital capacity and ALS-functional rating scale scores was observed in five patients (Mazzini et al., 2006). The same therapeutic approach was repeated in 10 patients. No slowdown of ALS clinical course was observed, however, no disease acceleration or new tissue formation was reported. Seven patients suffered from pain, four patients had sensory light-touch impairment in one leg, six patients had a tingling sensation in one leg, and one patient experienced light touch impairment in sacral region (Mazzini et al., 2010). The same group of investigators published results regarding treatment in 19 patients and reported the slowdown of disease progression in 6 patients (Mazzini et al., 2012).
A study conducted by Prabhakar et al (2012) evaluated the influence of autologous BM-MSC on ALS disease course. Ten patients underwent a lumbar puncture with stem cell administration and no adverse effects were observed. The authors concluded that MSCs administration led to disease stabilization in 1-year period of follow-up since no significant deterioration in ALS Functional Rating Scale was noted (Prabhakar et al., 2012).
Another study involving administration of autologous MSC was performed in Belarus. Stem cells infused through lumbar puncture were committed to neuronal differentiation. Intact cells were infused via intravenous route. Disease progression was observed in the study (10 patients) and control (15 patients) groups; however, its dynamics was significantly slower in patients who received stem cell therapy. No serious adverse events were observed. Fever (37.2°C) occurred in 1 case and was associated with intravenous injection. Increased temperature was revealed after 2 hours. Headache after lumbar puncture was the second adverse event. Two patients complained about those symptoms (Rushkevich et al., 2015).
Oh et al. (2015) conducted an open label phase I clinical trial with intrathecal injections of autologous BM-MSC. Seven out of eight patients received 2 doses within1 month. No serious adverse effects were noted during 12 months of follow-up. Adverse drug reaction was noted in six patients (pyrexia, pain and headache). The course of the disease seemed to be slower after the therapy in comparison to the previous decline (Oh et al., 2015).
A retrospective analysis of 57 ALS patients in a study by Sharma et al. (2015), consisting of 20 controls and 37 patients treated with autologous bone marrow mononuclear cells, showed survival benefit of stem cell therapy. Major adverse events were not present. Minor adverse events were as follows: spinal headache (30, 43%), nausea (4, 34%), vomiting (4, 34%), pain at the site of injection (4, 34%), pain at the site of aspiration (8, 67%), and fatigue (4, 34%).
Petrou et al. (2016) published their work regarding a clinical trial concerning ALS patients treated with autologous MSC which were induced to secrete neurotrophic factor (NTF). This work showed not only safety of such therapy but also efficacy, as a secondary end point. No serious adverse events were noted. Decline of the vital capacity was reduced and ALS Functional Rating Scale showed slight improvement during a 6 month follow-up period (Petrou et al., 2016).
To our knowledge, this study is the first to perform intrathecal injection of allogeneic MSC in patients with ALS. WJ-MSC was used in some diseases like: graft versus host disease, multiple sclerosis, diabetes type 1 and 2, diabetic foot, Alzheimer’s disease, spinal cord injury, cerebral palsy, Duchenne muscular dystrophy, and autism (Kalaszczynska and Ferdyn, 2015). There was one clinical trial of WJ-MSC in ALS patients but no known results were reported (NCT01494480). In this study, hemorrhage, infections, or increased intracranial pressure was not observed, and only headache was observed. For this reason, it seems there are no disadvantages of this method, but there might be some limitations. For example, acute infections, hematological problems with coagulopathy, increased intracranial pressure were observed in other studies. Therefore, it is necessary to further investigate this promising method.
Conclusion
This study confirms the safety of intrathecal injections of WJ-MSC in patients with ALS. No serious adverse events were observed. There was one adverse event that did not interfere with the whole therapy. Absence of other reported adverse events confirms that this therapy is well tolerated. More studies using WJ-MSC are needed to confirm our results. A presentation of research results concerning the outcomes of the therapy is underway.
Additional file: Open peer review report 1 (259.2KB, pdf) .
Acknowledgments:
Authors wish to express their gratitude to the patients who participated in this study.
Footnotes
Conflicts of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest. Instytut Terapii Komórkowych w Olsztynie (Cell Therapies Institute, FamiCord Group) in Olsztyn is a private medical institution that specializes in innovative commercial therapy which uses mesenchymal stem cells.
Financial support: This research was supported by Instytut Terapii Komórkowych w Olsztynie (Cell Therapies Institute, FamiCord Group) in Olsztyn (to MB, SM and TS). The funding body played no role in the study design, in the collection, analysis and interpretation of data, in the writing of the paper, and in the decision to submit the paper for publication.
Institutional review board statement: The study was approved by the Bioethical Committee of School of Medicine, University of Warmia and Mazury in Olsztyn, Poland (ethical approval consent was given by the resolution no. 36/2014 of June 2014 and no. 8/2016 of February 2016). This study was performed in accordance with the Declaration of Helsinki. Patients involved in the study signed a written informed consent. This study was registered with the ClinicalTrials.gov (identifier: NCT02881476) on August 29, 2016.
Declaration of patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement: This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Biostatistics statement: The statistical methods of this study were reviewed by the biostatistician of School of Medicine, University of Warmia and Mazury in Olsztyn, Poland.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Individual data that underlie the results reported in this article, after deidentification will be shared. The study protocol, statistical analysis plans, analytic code, and informed consent form without signatures will be made available beginning 3 months and ending 5 years following article publication to investigators whose proposed use of the data has been approved by an independent review committee identified to achieve aims in the approved proposal. Proposals should be directed to corresponding author. To gain access, data requestors will need to sign a data access agreement and institutional IRB approval will be required.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Rodolfo Gabriel Gatto, University of Illinois at Chicago, USA.
P-Reviewer: Gatto RG; C-Editor: Zhao M; S-Editor: Li CH; L-Editor: Song LP; T-Editor: Liu XL
Funding: This research was supported by Instytut Terapii Komórkowych w Olsztynie (Cell Therapies Institute, FamiCord Group) in Olsztyn (to MB, SM, and TS).
References
- 1.Andersen PM, Al-Chalabi A. Clinical genetics of amyotrophic lateral sclerosis: what do we really know? Nat Rev Neurol. 2011;7:603–615. doi: 10.1038/nrneurol.2011.150. [DOI] [PubMed] [Google Scholar]
- 2.Beers DR, Henkel JS, Zhao W, Wang J, Huang A, Wen S, Liao B, Appel SH. Endogenous regulatory T lymphocytes ameliorate amyotrophic lateral sclerosis in mice and correlate with disease progression in patients with amyotrophic lateral sclerosis. Brain. 2011;134:1293–1314. doi: 10.1093/brain/awr074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beers DR, Zhao W, Wang J, Zhang X, Wen S, Neal D, Thonhoff JR, Alsuliman AS, Shpall EJ, Rezvani K, Appel SH. ALS patients’regulatory T lymphocytes are dysfunctional, and correlate with disease progression rate and severity. JCI Insight. 2017;2:e89530. doi: 10.1172/jci.insight.89530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bensimon G, Lacomblez L, Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994;330:585–591. doi: 10.1056/NEJM199403033300901. [DOI] [PubMed] [Google Scholar]
- 5.Blondheim NR, Levy YS, Ben-Zur T, Burshtein A, Cherlow T, Kan I, Barzilai R, Bahat-Stromza M, Barhum Y, Bulvik S, Melamed E, Offen D. Human mesenchymal stem cells express neural genes, suggesting a neural predisposition. Stem Cells Dev. 2006;15:141–164. doi: 10.1089/scd.2006.15.141. [DOI] [PubMed] [Google Scholar]
- 6.Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial “Clinical limits of amyotrophic lateral sclerosis” workshop contributors. J Neurol Sci. 1994;124(Suppl):96–107. doi: 10.1016/0022-510x(94)90191-0. [DOI] [PubMed] [Google Scholar]
- 7.Brooks BR, Miller RG, Swash M, Munsat TL World Federation of Neurology Research Group on Motor Neuron D. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–299. doi: 10.1080/146608200300079536. [DOI] [PubMed] [Google Scholar]
- 8.Chen G, Yue A, Ruan Z, Yin Y, Wang R, Ren Y, Zhu L. Monitoring the biology stability of human umbilical cord-derived mesenchymal stem cells during long-term culture in serum-free medium. Cell Tissue Bank. 2014;15:513–521. doi: 10.1007/s10561-014-9420-6. [DOI] [PubMed] [Google Scholar]
- 9.Chio A, Logroscino G, Traynor BJ, Collins J, Simeone JC, Goldstein LA, White LA. Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology. 2013;41:118–130. doi: 10.1159/000351153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cui F, Cai W, Wang Z, Ren Y, Li M, Sun Z, Huang X. New mutation in the SOD1 (copper/zinc superoxide dismutase-1) gene in a Chinese amyotrophic lateral sclerosis (ALS) patient. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:635–637. doi: 10.3109/21678421.2013.817589. [DOI] [PubMed] [Google Scholar]
- 11.Czarzasta J, Habich A, Siwek T, Czaplinski A, Maksymowicz W, Wojtkiewicz J. Stem cells for ALS: An overview of possible therapeutic approaches. Int J Dev Neurosci. 2017;57:46–55. doi: 10.1016/j.ijdevneu.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Fecto F, Yan J, Vemula SP, Liu E, Yang Y, Chen W, Zheng JG, Shi Y, Siddique N, Arrat H, Donkervoort S, Ajroud-Driss S, Sufit RL, Heller SL, Deng HX, Siddique T. SQSTM1 mutations in familial and sporadic amyotrophic lateral sclerosis. Arch Neurol. 2011;68:1440–1446. doi: 10.1001/archneurol.2011.250. [DOI] [PubMed] [Google Scholar]
- 13.Forostyak S, Sykova E. Neuroprotective potential of cell-based therapies in ALS: from bench to bedside. Front Neurosci. 2017;11:591. doi: 10.3389/fnins.2017.00591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frausin S, Viventi S, Verga Falzacappa L, Quattromani MJ, Leanza G, Tommasini A, Valencic E. Wharton's jelly derived mesenchymal stromal cells: Biological properties, induction of neuronal phenotype and current applications in neurodegeneration research. Acta Histochem. 2015;117:329–338. doi: 10.1016/j.acthis.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Ge W, Ren C, Duan X, Geng D, Zhang C, Liu X, Chen H, Wan M, Geng R. Differentiation of mesenchymal stem cells into neural stem cells using cerebrospinal fluid. Cell Biochem Biophys. 2015;71:449–455. doi: 10.1007/s12013-014-0222-z. [DOI] [PubMed] [Google Scholar]
- 16.Gordon PH. Amyotrophic lateral sclerosis: pathophysiology, diagnosis and management. CNS Drugs. 2011;25:1–15. doi: 10.2165/11586000-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 17.Goutman SA. Diagnosis and Clinical management of amyotrophic lateral sclerosis and other motor neuron disorders. Continuum (Minneap Minn) 2017;23:1332–1359. doi: 10.1212/CON.0000000000000535. [DOI] [PubMed] [Google Scholar]
- 18.Hass R, Kasper C, Bohm S, Jacobs R. Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal. 2011;9:12. doi: 10.1186/1478-811X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henkel JS, Beers DR, Zhao W, Appel SH. Microglia in ALS: the good, the bad, and the resting. J Neuroimmune Pharmacol. 2009;4:389–398. doi: 10.1007/s11481-009-9171-5. [DOI] [PubMed] [Google Scholar]
- 20.Jablecki CK, Berry C, Leach J. Survival prediction in amyotrophic lateral sclerosis. Muscle Nerve. 1989;12:833–841. doi: 10.1002/mus.880121008. [DOI] [PubMed] [Google Scholar]
- 21.Jaiswal MK. Riluzole and edaravone: A tale of two amyotrophic lateral sclerosis drugs. Med Res Rev. 2018 doi: 10.1002/med.21528. [DOI] [PubMed] [Google Scholar]
- 22.Kalaszczynska I, Ferdyn K. Wharton's jelly derived mesenchymal stem cells: future of regenerative medicine? Recent findings and clinical significance. Biomed Res Int 2015. 2015:430847. doi: 10.1155/2015/430847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kano O, Iwamoto K, Ito H, Kawase Y, Cridebring D, Ikeda K, Iwasaki Y. Limb-onset amyotrophic lateral sclerosis patients visiting orthopedist show a longer time-to-diagnosis since symptom onset. BMC Neurol. 2013;13:19. doi: 10.1186/1471-2377-13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kikuchi K, Takeshige N, Miura N, Morimoto Y, Ito T, Tancharoen S, Miyata K, Kikuchi C, Iida N, Uchikado H, Miyagi N, Shiomi N, Kuramoto T, Maruyama I, Morioka M, Kawahara KI. Beyond free radical scavenging: Beneficial effects of edaravone (Radicut) in various diseases (Review) Exp Ther Med. 2012;3:3–8. doi: 10.3892/etm.2011.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwon MS, Noh MY, Oh KW, Cho KA, Kang BY, Kim KS, Kim YS, Kim SH. The immunomodulatory effects of human mesenchymal stem cells on peripheral blood mononuclear cells in ALS patients. J Neurochem. 2014;131:206–218. doi: 10.1111/jnc.12814. [DOI] [PubMed] [Google Scholar]
- 26.Lewis KE, Rasmussen AL, Bennett W, King A, West AK, Chung RS, Chuah MI. Microglia and motor neurons during disease progression in the SOD1G93A mouse model of amyotrophic lateral sclerosis: changes in arginase1 and inducible nitric oxide synthase. J Neuroinflammation. 2014;11:55. doi: 10.1186/1742-2094-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Logroscino G, Traynor BJ, Hardiman O, Chio A, Couratier P, Mitchell JD, Swingler RJ, Beghi E. Eurals. Descriptive epidemiology of amyotrophic lateral sclerosis: new evidence and unsolved issues. J Neurol Neurosurg Psychiatry. 2008;79:6–11. doi: 10.1136/jnnp.2006.104828. [DOI] [PubMed] [Google Scholar]
- 28.Marconi S, Bonaconsa M, Scambi I, Squintani GM, Rui W, Turano E, Ungaro D, D’Agostino S, Barbieri F, Angiari S, Farinazzo A, Constantin G, Del Carro U, Bonetti B, Mariotti R. Systemic treatment with adipose-derived mesenchymal stem cells ameliorates clinical and pathological features in the amyotrophic lateral sclerosis murine model. Neuroscience. 2013;248:333–343. doi: 10.1016/j.neuroscience.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 29.Mazzini L, Fagioli F, Boccaletti R, Mareschi K, Oliveri G, Olivieri C, Pastore I, Marasso R, Madon E. Stem cell therapy in amyotrophic lateral sclerosis: a methodological approach in humans. Amyotroph Lateral Scler Other Motor Neuron Disord. 2003;4:158–161. doi: 10.1080/14660820310014653. [DOI] [PubMed] [Google Scholar]
- 30.Mazzini L, Mareschi K, Ferrero I, Vassallo E, Oliveri G, Boccaletti R, Testa L, Livigni S, Fagioli F. Autologous mesenchymal stem cells: clinical applications in amyotrophic lateral sclerosis. Neurol Res. 2006;28:523–526. doi: 10.1179/016164106X116791. [DOI] [PubMed] [Google Scholar]
- 31.Mazzini L, Mareschi K, Ferrero I, Miglioretti M, Stecco A, Servo S, Carriero A, Monaco F, Fagioli F. Mesenchymal stromal cell transplantation in amyotrophic lateral sclerosis: a long-term safety study. Cytotherapy. 2012;14:56–60. doi: 10.3109/14653249.2011.613929. [DOI] [PubMed] [Google Scholar]
- 32.Mazzini L, Ferrero I, Luparello V, Rustichelli D, Gunetti M, Mareschi K, Testa L, Stecco A, Tarletti R, Miglioretti M, Fava E, Nasuelli N, Cisari C, Massara M, Vercelli R, Oggioni GD, Carriero A, Cantello R, Monaco F, Fagioli F. Mesenchymal stem cell transplantation in amyotrophic lateral sclerosis: a phase I clinical trial. Exp Neurol. 2010;223:229–237. doi: 10.1016/j.expneurol.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Miller RG, Mitchell JD, Lyon M, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND) Cochrane Database Syst Rev. 2007:CD001447. doi: 10.1002/14651858.CD001447.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Mora JS. Edaravone for treatment of early-stage ALS. Lancet Neurol. 2017;16:772. doi: 10.1016/S1474-4422(17)30289-2. [DOI] [PubMed] [Google Scholar]
- 35.Morgan S, Orrell RW. Pathogenesis of amyotrophic lateral sclerosis. Br Med Bull. 2016;119:87–98. doi: 10.1093/bmb/ldw026. [DOI] [PubMed] [Google Scholar]
- 36.Moujalled D, White AR. Advances in the development of disease-modifying treatments for amyotrophic lateral sclerosis. CNS Drugs. 2016;30:227–243. doi: 10.1007/s40263-016-0317-8. [DOI] [PubMed] [Google Scholar]
- 37.Oh KW, Moon C, Kim HY, Oh SI, Park J, Lee JH, Chang IY, Kim KS, Kim SH. Phase I trial of repeated intrathecal autologous bone marrow-derived mesenchymal stromal cells in amyotrophic lateral sclerosis. Stem Cells Transl Med. 2015;4:590–597. doi: 10.5966/sctm.2014-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrou P, Gothelf Y, Argov Z, Gotkine M, Levy YS, Kassis I, Vaknin-Dembinsky A, Ben-Hur T, Offen D, Abramsky O, Melamed E, Karussis D. Safety and clinical effects of mesenchymal stem cells secreting neurotrophic factor transplantation in patients with amyotrophic lateral sclerosis: results of phase 1/2 and 2a clinical trials. JAMA Neurol. 2016;73:337–344. doi: 10.1001/jamaneurol.2015.4321. [DOI] [PubMed] [Google Scholar]
- 39.Petrov D, Mansfield C, Moussy A, Hermine O. ALS clinical trials review: 20 years of failure. Are we any closer to registering a new treatment? Front Aging Neurosci. 2017;9:68. doi: 10.3389/fnagi.2017.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prabhakar S, Marwaha N, Lal V, Sharma RR, Rajan R, Khandelwal N. Autologous bone marrow-derived stem cells in amyotrophic lateral sclerosis: a pilot study. Neurol India. 2012;60:465–469. doi: 10.4103/0028-3886.103185. [DOI] [PubMed] [Google Scholar]
- 41.Renton AE, Chio A, Traynor BJ. State of play in amyotrophic lateral sclerosis genetics. Nat Neurosci. 2014;17:17–23. doi: 10.1038/nn.3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, Donaldson D, Goto J, O’Regan JP, Deng HX, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362:59–62. doi: 10.1038/362059a0. [DOI] [PubMed] [Google Scholar]
- 43.Rosenbohm A, Liu M, Nagel G, Peter RS, Cui B, Li X, Kassubek J, Rothenbacher D, Lule D, Cui L, Ludolph AC Group ALSRSS. Phenotypic differences of amyotrophic lateral sclerosis (ALS) in China and Germany. J Neurol. 2018;265:774–782. doi: 10.1007/s00415-018-8735-9. [DOI] [PubMed] [Google Scholar]
- 44.Rothstein JD. Edaravone: A new drug approved for ALS. Cell. 2017;171:725. doi: 10.1016/j.cell.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 45.Rowland LP, Shneider NA. Amyotrophic lateral sclerosis. N Engl J Med. 2001;344:1688–1700. doi: 10.1056/NEJM200105313442207. [DOI] [PubMed] [Google Scholar]
- 46.Rushkevich YN, Kosmacheva SM, Zabrodets GV, Ignatenko SI, Goncharova NV, Severin IN, Likhachev SA, Potapnev MP. The use of autologous mesenchymal stem cells for cell therapy of patients with amyotrophic lateral sclerosis in belarus. Bull Exp Biol Med. 2015;159:576–581. doi: 10.1007/s10517-015-3017-3. [DOI] [PubMed] [Google Scholar]
- 47.Sharma AK, Sane HM, Paranjape AA, Gokulchandran N, Nagrajan A, D’sa M, Badhe PB. The effect of autologous bone marrow mononuclear cell transplantation on the survival duration in Amyotrophic Lateral Sclerosis - a retrospective controlled study. Am J Stem Cells. 2015;4:50–65. [PMC free article] [PubMed] [Google Scholar]
- 48.Siddique T, Figlewicz DA, Pericak-Vance MA, Haines JL, Rouleau G, Jeffers AJ, Sapp P, Hung WY, Bebout J, McKenna-Yasek D, et al. Linkage of a gene causing familial amyotrophic lateral sclerosis to chromosome 21 and evidence of genetic-locus heterogeneity. N Engl J Med. 1991;324:1381–1384. doi: 10.1056/NEJM199105163242001. [DOI] [PubMed] [Google Scholar]
- 49.Stifani N. Motor neurons and the generation of spinal motor neuron diversity. Front Cell Neurosci. 2014;8:293. doi: 10.3389/fncel.2014.00293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Struys T, Moreels M, Martens W, Donders R, Wolfs E, Lambrichts I. Ultrastructural and immunocytochemical analysis of multilineage differentiated human dental pulp- and umbilical cord-derived mesenchymal stem cells. Cells Tissues Organs. 2011;193:366–378. doi: 10.1159/000321400. [DOI] [PubMed] [Google Scholar]
- 51.Sun H, Sun C, Xiao W. Expression regulation of co-inhibitory molecules on human natural killer cells in response to cytokine stimulations. Cytokine. 2014;65:33–41. doi: 10.1016/j.cyto.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 52.Tada S, Okuno T, Yasui T, Nakatsuji Y, Sugimoto T, Kikutani H, Sakoda S. Deleterious effects of lymphocytes at the early stage of neurodegeneration in an animal model of amyotrophic lateral sclerosis. J Neuroinflammation. 2011;8:19. doi: 10.1186/1742-2094-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tang Y, Le W. Differential roles of M1 and m2 Microglia in neurodegenerative diseases. Mol Neurobiol. 2016;53:1181–1194. doi: 10.1007/s12035-014-9070-5. [DOI] [PubMed] [Google Scholar]
- 54.Thonhoff JR, Beers DR, Zhao W, Pleitez M, Simpson EP, Berry JD, Cudkowicz ME, Appel SH. Expanded autologous regulatory T-lymphocyte infusions in ALS: A phase I, first-in-human study. Neurol Neuroimmunol Neuroinflamm. 2018;5:e465. doi: 10.1212/NXI.0000000000000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Turner MR, Hardiman O, Benatar M, Brooks BR, Chio A, de Carvalho M, Ince PG, Lin C, Miller RG, Mitsumoto H, Nicholson G, Ravits J, Shaw PJ, Swash M, Talbot K, Traynor BJ, Van den Berg LH, Veldink JH, Vucic S, Kiernan MC. Controversies and priorities in amyotrophic lateral sclerosis. Lancet Neurol. 2013;12:310–322. doi: 10.1016/S1474-4422(13)70036-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Writing G, Edaravone ALSSG. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16:505–512. doi: 10.1016/S1474-4422(17)30115-1. [DOI] [PubMed] [Google Scholar]
- 57.Zhao W, Xie W, Xiao Q, Beers DR, Appel SH. Protective effects of an anti-inflammatory cytokine, interleukin-4, on motoneuron toxicity induced by activated microglia. J Neurochem. 2006;99:1176–1187. doi: 10.1111/j.1471-4159.2006.04172.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


