Abstract
Purpose
Many patients suffer a stroke at a significant distance from a specialized center capable of delivering endovascular therapy. As a result, they require rapid transport by helicopter emergency medical services, sometimes while receiving a recombinant tissue plasminogen activator infusion (drip and ship). Despite its critical role in the new era of reperfusion, helicopter emergency medical services remains a poorly evaluated aspect of stroke care.
Method
Comprehensive narrative review of all published articles of helicopter emergency medical services related to acute stroke care in the inter-hospital and pre-hospital settings, including technical aspects and physical environment implications.
Findings
Helicopter emergency medical services transports are conducted during a critical early time period when specific interventions and ancillary care practices may have a significant influence on outcomes. We have limited knowledge of the potential impact of the unusual physical factors generated by the helicopter on the ischemic brain, which affects our ability to establish rational guidelines for ancillary care and the delivery of specific interventions.
Discussion
Unlike the pre-hospital and hospital settings where stroke interventions are delivered, the inter-hospital helicopter emergency medical services transfer setting remains a “black box” for acute stroke care and research. This gap is particularly relevant for many patients living in rural areas, or in congested urban areas, that depend on helicopter emergency medical services for rapid access to a tertiary stroke center.
Conclusion
Addressing the helicopter emergency medical services stroke gap in clinical trials and acute care delivery would homogenize capabilities through all care settings, thus minimizing potential disparities in research access and outcomes based on geographical location.
Keywords: Helicopter emergency medical services, acute stroke therapy, stroke systems of care
Impact of air medical transport in acute stroke
This study was narrative review summarizing the field of helicopter transportation of stroke patients. A Pubmed search was conducted June 2016 using the search terms “Helicopter & stroke” and “HEMS & stroke” and “helicopter & cerebrovascular disorder” (to enhance capture before year 2000). These lead to 134, 13, and 131 articles, respectively. All articles were reviewed, and 19 were selected based on their relevance to this review.
Stroke is a common contributor to disability in the World, with over 16.9 million new patients affected each year.1 Helicopter emergency medical services (HEMS) is an important element in the system for delivering acute stroke care for patients that suffer a stroke at a significant distance from a tertiary stroke center, approximately 20% of the US population,2,3 and many other areas of the world. In addition to intravenous recombinant tissue plasminogen activator (rtPA) treatment, endovascular mechanical thrombectomy (MT) recently became the new standard of care in patients with a stroke due to a proximal arterial occlusion.4 But unlike widely available intravenous rtPA, MT is a complex therapy that requires specific equipment and human expertise only available at a limited number of tertiary centers in the United States.5 Given the geographic dispersion of the US population, transfer of a great number of patients to an MT-capable center is required.5 Because MT is a time-dependent therapy tied to viable ischemic penumbra within a short window of opportunity,4 emergent HEMS is often required.6
Consequently, HEMS is largely used in the United States for inter-hospital transfer from a community hospital to a comprehensive stroke center, often while receiving rtPA while in route to a tertiary center.7,8 It is also used in lesser amount for direct field to hospital operations, mostly in very remote (frontier) or isolated geographical situations,9,8 such as islands, sea,10 or mountains. There are approximately 400,000 total HEMS missions flown a year in the United States.11 A large 10-year sample of HEMS flights has shown a gradual increase in the ischemic stroke related missions which comprised 4% of the flight missions in 2011.8 Based on that estimation, there are 16,000 ischemic stroke helicopter missions flown each year in the United States. However, that data might be an underestimation since it preceded the establishment of MT, which requires expeditious transportation.6,12 It is therefore expected that the use of HEMS will significantly increase with the widespread implementation of MT. The number of acute stroke-related fixed-wing operations is not known. But given the delays caused by the logistics and since airplane flights require out of hospital take-off and landing, fixed-wing operations are probably not a big additional contributor to acute reperfusion therapy.
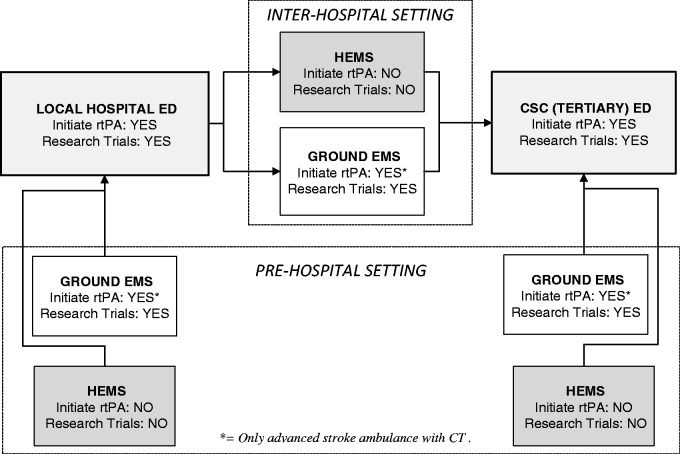
Air medical crews are generally composed of flight paramedics and flight nurses, which are sometimes joined by emergency medicine physicians and residents. The procedures to be selected as part of a crew are rigorous, which results in a very skillful yet small number of professionals that cover a large spectrum of patients.13,14 As a result, HEMS is staffed by a group of highly trained professionals capable of delivering excellent care during critical early time periods when specific interventions and ancillary care practices may have a significant influence on outcomes. But despite the obvious and growing relevance of HEMS for acute stroke care, it remains a gap in knowledge and research capabilities (Figure 1).
Figure 1.
HEMS: A gap in acute stroke delivery and research.
HEMS: helicopter emergency medical services; rtPA: recombinant plasminogen activator; CSC: comprehensive stroke center; ED: emergency department; EMS: emergency medical services.
Inter-hospital HEMS in stroke
The most common (72%) use of HEMS in the United States applies to inter-hospital transfer.8
It is important to highlight the important differences between the pre-hospital and the inter-hospital settings (Table 1). They occur in two different time periods in acute stroke care since the inter-hospital setting is preceded by care received at a local emergency department (ED) (Figure 1). As a result, there is more cumulative expertise and imaging and laboratory capability in the inter-hospital setting. These patients had been already evaluated at a community hospital and underwent laboratory investigations and a computerized tomography (CT) scan of the brain.15,14 In some regional systems, patients are required to be transported to a stroke center to receive rtPA.16 But the lack of local stroke expertise in these EDs may be compensated by telephonic or telemedicine consultation with a tertiary center,17 so treatment with rtPA is often initiated locally (“drip & ship”). As a result, patients transported through the inter-hospital setting are a much more selective population than those encountered in the pre-hospital setting18. Ischemic stroke mimics, such as intracranial hemorrhage, or hypoglycemia have been typically excluded (Table 1).
Table 1.
Comparison between the pre-hospital and the inter-hospital stroke environments.
| Pre-hospital | Inter-hospital | |
|---|---|---|
| Stroke expertise | No (other than pre-hospital scales)a | Telephonic consultation, telestroke, local physician (local ED-based) |
| Laboratory capability | Accu-check | Basic tests (local ED-based) |
| Imaging capability | Nonea | CT scan (local ED-based) |
| rtPA treatment | Noa | Yes |
| Type of patients | Mixed ischemic stroke, brain hemorrhages, mimics | Diagnosed ischemic stroke, diagnosed brain hemorrhages, excluded some mimics |
This does not include advanced stroke ambulance with CT.27
HEMS: helicopter emergency medical services; ED: emergency department; rtPA: recombinant tissue plasminogen activator.
A variety of factors and local regulations play into determining the choice of using HEMS versus ground ambulances for inter-hospital transport. For example, in the United States the Emergency Medical Treatment and Active Labor Act authorize the referring physician to choose the mode of transport. The severity of symptoms, use of rtPA, and need for interventional therapy, as well as system limitations such as distance to the stroke center and availability of critical care air or ground ambulances all play a role.8,19 Beside the difference in speed,16 HEMS-transported patients were receiving higher rates of IV thrombolysis locally20 as well as more specialized care and interventions.6 For these reasons, HEMS has been endorsed by the air medical community as the most appropriate method of inter-hospital transportation for acute stroke,21 a recommendation that preceded the establishment of MT as the new standard of care. This has obviously become even more relevant now since for many patients living in rural areas, or in traffic congested urban areas, HEMS might be the best chance to arrive on time to an MT center. Alternatively, HEMS could be used to transport an interventionalist to treat the patient at hospitals that have the necessary equipment but lack the human expertise.
Still, HEMS has some intrinsic limitations. It is more vulnerable to weather conditions than ground ambulances. Bad weather might result in either not flying at all, or flying at an unjustifiably increased risk. A study showed 182 HEMS crashes in the United States during 1983–2005.22 While that risk is still relatively low, crashes were more likely to occur in darkness and during instrument-based flying (bad weather).22 To minimize this issue, flight crews are typically instructed to make their go/no-go decision solely based in operational aeronautical factors. They are deliberately kept blinded to the age and diagnosis of the patient until they are airborne in order to avoid medical/personal biases in their aeronautical decision.23 Another important limitation is the cost. The use of HEMS for facilitation of intravenous thrombolytic treatment was analyzed regarding cost-effectiveness. A computer model based cost-analysis deemed HEMS to be cost-effective24 when thrombolytic treatment was only started after transport. A small single center retrospective cohort study raised concerns about the benefit of HEMS unless endovascular therapy is considered.25
Field to hospital use of HEMS
Direct field to stroke center is a pre-hospital HEMS approach that is most appropriate for very remote (frontier) states with little access to stroke-ready hospitals.9 Local availability of a primary or comprehensive stroke center is of great importance in determining the destination for a HEMS scene transport. This approach was used for 28% of HEMS transports in one large cohort of 25,332 cases.8 By transporting patients rapidly to a stroke center, it might allow the administration of rtPA9 or MT. As this is a pre-hospital setting (Table 1), the patients seen are similar to that encountered by ground emergency medical services (EMS). This includes a combination of ischemic and hemorrhagic strokes, as well as stroke mimics.
There are several differences between ground EMS and HEMS (Table 2). Because space is much more limited in air transport, and helicopters cannot easily interrupt their flight in case of unexpected events such as circulation arrest, sudden drop of blood pressure or urination. Patients transported with HEMS need more transport preparation than those transported with ground EMS. Because distances from ground EMS base stations to the scene are usually shorter than outbound distances of HEMS, possible delays to arrival need to be taken into account when decisions are made regarding the mode of transportation. Time savings by HEMS can only be expected in settings with long distances from scene to hospital. An evaluation of inter-hospital transports within a large German TeleStroke network reported a shorter transfer time only when distances between hospitals were longer than 50 km.26
Table 2.
Comparison between ground ambulances and HEMS.
| Ground ambulances | HEMS | |
|---|---|---|
| Type human expertise | EMTs, voluntary firefighters (rural areas), physicians (outside United States) | EMT, nurses (in-flight), physicians and physician extenders (local ED), stroke specialists (phone/telemedicine) |
| Speed of transport | + | +++ |
| Vulnerability to weather/altitude/humidity | + | +++ |
| Weight restrictions | _ | +++ |
| Space limitations | + | +++ |
| CT-carrying capabilities | Yes | No |
| Potential impact of physical factors on stroke patients | + | +++ |
| Cost | + | +++ |
| Availability | +++ | + |
EMT: emergency medical technician; ED: emergency department; HEMS: helicopter emergency medical services.
Advanced pre-hospital stroke work-up and treatment
The new specialized stroke ambulance concept with CT and telemedicine capability27 aboard ground ambulances allows diagnosis and early treatment before hospital arrival. Studies have shown relevant time-to-treatment reduction in intravenous rtPA application28,29 with much higher percentage of patients treated within 60 min from onset,30 this approach is still rarely used and probably limited to the large metropolitan areas where their cost might be justified by the large volumes.31 Keeping this in mind, it seems unlikely that CT-carrying stroke ambulances would be implemented in dispersed rural areas with a smaller density of strokes and sometimes limited human expertise (e.g. in the United States typically staffed by voluntary firefighters).14,32 HEMS could be an alternative to specialized stroke ambulances for rural areas, allowing the field initiation of rtPA in frontier states.27,33 So far, the main limitation for specialized stroke HEMS is the lack of imaging capability. A small study has shown the feasibility of transcranial Doppler (TCD) during HEMS,34 but this technique requires expertise and is not sufficient to exclude intracranial hemorrhage before initiation of rtPA treatment.
An approach similar to the portable CT used by ground ambulances could be considered to increase HEMS capability.27 There are technical and regulatory barriers to overcome before installing a CT onboard a Medevac helicopter (Table 3). Of all the limitations of a helicopter, weight most adversely affects the performance. Other factors that limit helicopter performance are hot ambient temperatures and altitude. This might limit the ability to rescue very heavy patients, or fly longer distances when more fuel is required. Typically, there is little room for extra weight on board most HEMS helicopters. With full fuel, a Eurocopter EC-135 helicopter has a remaining useful load of around 925 kg, which have to be distributed between the four people on board with winter clothing, patient stretcher, survival, monitoring and resuscitation equipment, emergency medical supplies, and additional crew items. This leaves realistically around 200 kg extra at the most, which may accommodate specialized CT scanners that have been lightened for flight. The EC-145 is a slightly larger machine that, when fully fueled, can carry a payload of 1035 kg and therefore would leave a capacity of around 310 kg for a mobile CT scanner. For the significantly larger Bell 412, that available capacity would be 582 kg, making the installation of a portable CT scanner and supporting accessories quite feasible. Larger aircraft such as the Sikorski UH-60M or similar machines would leave around 3500 kg available for installation of a CT scanner. This significant capacity would make the installation quite straightforward but such large helicopters are costly to operate and may not be suitable for smaller landing zones or helipads. There are also issues of radiation isolation in such close quarters, excessive electrical power consumption that may steal mechanical power from the drive train, and electromagnetic interference with the aircraft avionics.
Table 3.
Potential barriers to transform helicopters into CT-carrying advanced stroke ambulances.
| Potential barrier | Reason |
|---|---|
| Weight of CT scanner Power demand on generators | Degraded flight performance Limited operation range Restriction on flying conditions based on temperature/altitude |
| Volume CT scanner | Difficult to accommodate into cramped space Difficult to provide radiation protection for crew |
| Electromagnetic interference (scanner, wireless data link) | Potential interference with avionics |
| Dedicated flying unit would only be used for stroke missions (limited percentage total flights) | Limited use could render it unaffordable |
| Ethical/Operational | Crew would have to be made aware of diagnosis before making the “go/no-go” decision |
Implications of the HEMS-specific physical environment
Several aspects of HEMS have to be considered for transportation during the critical early period of stroke care. It involves unusual physical factors for stroke patients such as vibration,35 noise,36 accelerations,37 and rapid changes in barometric pressure and partial pressure of oxygen,38 all of which could potentially affect arterial clot constitution and lysis, reperfusion, and other aspects of neurophysiologic response to ischemic stroke (Table 4). Some of these factors could be potentially harmful for the ischemic brain. For example, the hypobaric environment could worsen the ischemic penumbra, or acceleration in three axes might result in nausea and vomiting that could increase the intracranial pressure and aspiration risk. The extreme noise might result in increased blood pressure and reperfusion injury. In addition, low frequency vibration might increase blood brain barrier permeability,39 and could potentially affect the efficacy of a rtPA infusion which is supposed not to be shaken after it is reconstituted (Alteplase prescribing information). On the other hand, some of these factors might be beneficial. For example, accelerations and low frequency vibrations40 might be synergistic with thrombolysis, and thus enhance the therapeutic efficacy of rtPA. Despite these conflicting and potentially significant factors, the effect of HEMS on an ischemic brain is not known. Retrospective series have suggested no negative net effect, but these studies are naturally limited by selection biases and offer limited sensitivity for changes in outcomes.25,41 Randomized controlled studies of an actual helicopter exposure in stroke patients would be difficult due to obvious ethical and logistical concerns. A randomized pilot study on a murine embolic model suggested that helicopter transport did not negatively influence outcomes, and in fact the trend was towards smaller infarctions and hemorrhage.42 Clearly, the potential influence of HEMS physical factors on stroke outcomes needs to be studied further. It is crucial to understand the net effect and interaction of those physical factors in order to optimize the delivery of thrombolytic agents, best medical care, and eventual neuroprotective agents, for drip and ship stroke patients.42
Table 4.
Potential effects of HEMS-associated physical factors.
| Physical factor | Potential effect |
|---|---|
| Vibration35 | Enhanced clot lysis due to mechanical effect Decreased pharmacological effectiveness rtPA Increased blood brain barrier permeability |
| Noise36 | Blood pressure elevation and reperfusion injury |
| Accelerations37 | Motion sickness, increased intracranial pressure, aspiration pneumonia/pneumonitis |
| Hypobaric changes38 | Worsening of ischemic penumbra |
rtPA: recombinant tissue plasminogen activator.
Current ancillary care in patients transported through HEMS
The care of patients transported by HEMS is determined by the physician responsible for the medical oversight of that specific program.43 In the absence of specific national guidelines, the local rules are typically inspired and adapted from the current guidelines of ground-based stroke management including post-rtPA care.43 Treatment of patients within the HEMS environment is a combination of standard EMS care as well as ED and ICU level care. Traditional ground ambulance EMS care of stroke patients focuses on early recognition, rapid transport, and early notification to the receiving center.43 HEMS units transporting patients directly from scene to a hospital typically follow these guidelines as imaging would not have been obtained to rule out hemorrhage. But the HEMS units transporting patients in an inter-hospital capacity are expected to provide care similar to an intensive care unit or an ED, with the obvious limitations of the helicopter capabilities. This includes appropriate blood pressure control, especially in the setting of tPA delivery, airway control, and early identification of complications. While there are ground critical care EMS services that can operate at a similar level to HEMS units, many regions of the country do not have these units available. They are especially scarce in rural regions. HEMS ancillary-care guidelines are typically based on expert opinion without necessarily taking into consideration the unique physical HEMS environment.42
Inter-hospital HEMS: An underutilized clinical research opportunity
Pre-hospital HEMS research might be possible with a similar approach as that employed by ambulance based ground trials,44 with the additional advantage of enhanced human expertise and limited amount of co-investigators that are needed. However, there is a much greater potential for research in the inter-hospital transfer. It provides a unique opportunity to test specific interventions to preserve the penumbra and mitigate reperfusion injury in transit.23 Such interventions are particularly relevant for patients with relative access to intravenous (IV) rtPA, but distant from a center that could provide endovascular rescue therapy. Given the time-sensitivity of such interventions, it is important to minimize delays between IV and IA reperfusion treatments. Thus, a HEMS-delivered neuroprotective and reperfusion-mitigating strategy could potentially compensate for this delay, and help mitigate potential differences in outcome based on geographical location.14 Also, HEMS provides an opportunity to help traditional tertiary-based acute stroke trials by expediting the informed consent process. Patients with stroke transported by HEMS who are incapacitated and unable to provide informed consent typically arrive to the tertiary center well before their relatives who use ground transportation.13,23 This temporal patient–surrogate dissociation inevitably results in either delays in enrollment, or ineligibility to enroll at all due to missing the time window. HEMS crews could significantly help this problem by screening and consenting surrogates and, therefore, enrolling subjects at the outside hospital ahead of their arrival to the tertiary institution.23
The feasibility of HEMS-initiated research approach has been demonstrated in a single-center randomized controlled intervention pilot trial23 in Iowa that may be generalizable to other academic-based helicopter services. The HEMS personnel from the University of Iowa showed an unanticipated degree of enthusiasm in becoming co-investigators in trials, including completing all the regulatory documents, training, and certification.23 They also demonstrated an ability to screen patients using simple clinical and laboratory variables that are available at the time patients would be picked up at an outside hospital.23 That included obtaining an accurate NIH Stroke Scale Score,23 a finding that was later validated by an independent group.45 The HEMS crews successfully obtained a signed consent for a low risk vehicle intervention for 52% of the approached subjects. The study also shows that the downtime of the outbound flight to pick up the patient can also be used to potentiate research. If the HEMS crews were successful in talking with the patient or family members about the study using the onboard 800 MHz radiophone before their arrival, the consent rate increased to 69% for a low-risk intravenous intervention.23 This illustrates the benefit of advance notification about the study for promoting subsequent informed consent in a very time-pressured environment.
Another potential barrier to HEMS-based research, the oversight of institutional research board (IRB), was also addressed. We learned that the transfer of legal care to the tertiary emergency department occurs the moment the University based HEMS team arrives at the outside hospital and meets the patient.23 Consequently, the University of Iowa IRB determined that research activities could also be initiated at that same time under the umbrella of the University IRB that supervises the emergency department.23 In rural areas, HEMS services cover a large area with multiple community/critical access hospitals. Involving and certifying each of these institutions as research centers would be logistically problematic, if not impossible. Many of these small hospitals do not even have an IRB. Therefore, university-based IRB agreement is crucial for HEMS-based stroke research in order to ensure adequate subject protection. Because HEMS research is performed by a handful of experienced university-based HEMS crews that serve a large catchment area, it greatly facilitates maintaining their credentials and competence as co-investigators.23
Based on this preliminary experience, and the accuracy of the diagnosis in this environment, inter-hospital HEMS provides a unique opportunity to test interventions to minimize penumbral expansion and reperfusion injury before arriving to the comprehensive stroke center (CSC).23 It also provides an opportunity to test specific interventions for intracranial hemorrhages. Given the potential for interaction between the helicopter physical factors and reperfusion and BBB permeability, the ancillary care provided en route and the dosages of neuroprotective interventions might need to be adapted.42
Summary/Conclusions
In the era of mechanical reperfusion, HEMS can be a powerful instrument for improving acute stroke delivery and research that is currently underutilized. The speed of HEMS may allow reperfusion for a large number of patients that would not have immediate access due to geography or traffic congestion. Also, HEMS critical early time period after a stroke where specific interventions to preserve penumbra and prevent reperfusion injury may have a significant influence on outcomes. The impact of physical factors generated by the helicopter on the ischemic brain needs to be studied. HEMS are also an opportunity to increase recruitment of patients in standard clinical trials. Addressing the HEMS stroke gap is necessary to homogenize the delivery of acute stroke care and research capabilities through all care settings, therefore minimizing disparities in outcomes based in geographical location.
Acknowledgements
We thank the AirCare crews from the University of Iowa for advancing stroke care and research.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent
Not applicable.
Ethical approval
Not applicable.
Guarantor
EL.
Contributorship
EL researched literature and conceived the study and wrote the first draft of the manuscript. All authors contributed to this review with substantial intellectual content, reviewed and edited the manuscript and approved the final version of the manuscript.
References
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: Findings from the global burden of disease study 2010. Lancet 2014; 383: 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adeoye O, Albright KC, Carr BG, et al. Geographic access to acute stroke care in the United States. Stroke 2014; 45: 3019–3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United States Bureau of the Census. Urban and rural population 2010 (www.Census.Gov), 2005.
- 4.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 5.Carr BG, Branas CC, Metlay JP, et al. Access to emergency care in the United States. Ann Emerg Med 2009; 54: 261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lukovits TG, von Iderstine SL, Brozen R, et al. Interhospital helicopter transport for stroke. Air Med J 2013; 32: 36–39. [DOI] [PubMed] [Google Scholar]
- 7.Tekle WG, Chaudhry SA, Hassan AE, et al. Drip-and-ship thrombolytic treatment paradigm among acute ischemic stroke patients in the United States. Stroke 2012; 43: 1971–1974. [DOI] [PubMed] [Google Scholar]
- 8.Hutton CF, Fleming J, Youngquist S, et al. Stroke and helicopter emergency medical service transports: An analysis of 25,332 patients. Air Med J 2015; 34: 348–356. [DOI] [PubMed] [Google Scholar]
- 9.Silliman SL, Quinn B, Huggett V, et al. Use of a field-to-stroke center helicopter transport program to extend thrombolytic therapy to rural residents. Stroke 2003; 34: 729–733. [DOI] [PubMed] [Google Scholar]
- 10.Lambert R, Cabardis S, Valance J, et al. Fibrinolysis and acute stroke in maritime search and rescue medical evacuation. Ann Fr Anesth Reanim 2008; 27: 249–251. [DOI] [PubMed] [Google Scholar]
- 11.The association of air medical services (AAMS), http://aams.Org/member-services/fact-sheet-faqs/ (accessed December 2015).
- 12.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 13.Leira EC, Lamb DL, Nugent AS, et al. Feasibility of acute clinical trials during aerial interhospital transfer. Stroke 2006; 37: 2504–2507. [DOI] [PubMed] [Google Scholar]
- 14.Leira EC, Hess DC, Torner JC, et al. Rural-urban differences in acute stroke management practices: A modifiable disparity. Arch Neurol 2008; 65: 887–891. [DOI] [PubMed] [Google Scholar]
- 15.Leira EC, Pary JK, Davis PH, et al. Slow progressive acceptance of intravenous thrombolysis for patients with stroke by rural primary care physicians. Arch Neurol 2007; 64: 518–521. [DOI] [PubMed] [Google Scholar]
- 16.Hesselfeldt R, Gyllenborg J, Steinmetz J, et al. Is air transport of stroke patients faster than ground transport? A prospective controlled observational study. Emerg Med J 2014; 31: 268–272. [DOI] [PubMed] [Google Scholar]
- 17.Saler M, Switzer JA, Hess DC. Use of telemedicine and helicopter transport to improve stroke care in remote locations. Curr Treat Options Cardiovasc Med 2011; 13: 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sequeira D, Martin-Gill C, Kesinger MR, et al. Characterizing strokes and stroke mimics transported by helicopter emergency medical services. Prehosp Emerg Care 2016. [DOI] [PubMed] [Google Scholar]
- 19.Thomson DP, Thomas SH. Guidelines for air medical dispatch. Prehosp Emerg Care 2003; 7: 265–271. [DOI] [PubMed] [Google Scholar]
- 20.Reiner-Deitemyer V, Teuschl Y, Matz K, et al. Helicopter transport of stroke patients and its influence on thrombolysis rates: Data from the Austrian stroke unit registry. Stroke 2011; 42: 1295–1300. [DOI] [PubMed] [Google Scholar]
- 21.Hutton K, Sand C. Appropriateness of medical transport and access to care in acute stroke syndromes. Air Med J 2005; 24: 220–221. [DOI] [PubMed] [Google Scholar]
- 22.Baker SP, Grabowski JG, Dodd RS, et al. EMS helicopter crashes: What influences fatal outcome? Ann Emerg Med 2006; 47: 351–356. [DOI] [PubMed] [Google Scholar]
- 23.Leira EC, Ahmed A, Lamb DL, et al. Extending acute trials to remote populations: A pilot study during interhospital helicopter transfer. Stroke 2009; 40: 895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silbergleit R, Scott PA, Lowell MJ, et al. Cost-effectiveness of helicopter transport of stroke patients for thrombolysis. Acad Emerg Med 2003; 10: 966–972. [DOI] [PubMed] [Google Scholar]
- 25.Olson MD, Rabinstein AA. Does helicopter emergency medical service transfer offer benefit to patients with stroke? Stroke 2012; 43: 878–880. [DOI] [PubMed] [Google Scholar]
- 26.Audebert HJ, Clarmann von Clarenau S, Schenkel J, et al. Problems of emergency transfers of patients after a stroke. Results of a telemedicine pilot project for integrated stroke accommodation in southeast Bavaria (Tempis). Dtsch Med Wochenschr 2005; 130: 2495–2500. [DOI] [PubMed] [Google Scholar]
- 27.Ebinger M, Fiebach JB, Audebert HJ. Mobile computed tomography: Prehospital diagnosis and treatment of stroke. Curr Opin Neurol 2015; 28: 4–9. [DOI] [PubMed] [Google Scholar]
- 28.Ebinger M, Winter B, Wendt M, et al. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: A randomized clinical trial. JAMA 2014; 311: 1622–1631. [DOI] [PubMed] [Google Scholar]
- 29.Walter S, Kostopoulos P, Haass A, et al. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: A randomised controlled trial. Lancet Neurol 2012; 11: 397–404. [DOI] [PubMed] [Google Scholar]
- 30.Ebinger M, Kunz A, Wendt M, et al. Effects of golden hour thrombolysis: A prehospital acute neurological treatment and optimization of medical care in stroke (Phantom-s) substudy. JAMA Neurol 2015; 72: 25–30. [DOI] [PubMed] [Google Scholar]
- 31.Gyrd-Hansen D, Olsen KR, Bollweg K, et al. Cost-effectiveness estimate of prehospital thrombolysis: Results of the Phantom-s study. Neurology 2015; 84: 1090–1097. [DOI] [PubMed] [Google Scholar]
- 32.Warach S. Prehospital thrombolysis for stroke: An idea whose golden hour has arrived. JAMA Neurol 2015; 72: 9–10. [DOI] [PubMed] [Google Scholar]
- 33.Holscher T, Dunford JV, Schlachetzki F, et al. Prehospital stroke diagnosis and treatment in ambulances and helicopters-a concept paper. Am J Emerg Med 2013; 31: 743–747. [DOI] [PubMed] [Google Scholar]
- 34.Holscher T, Schlachetzki F, Zimmermann M, et al. Transcranial ultrasound from diagnosis to early stroke treatment. 1. Feasibility of prehospital cerebrovascular assessment. Cerebrovasc Dis 2008; 26: 659–663. [DOI] [PubMed] [Google Scholar]
- 35.Carchietti E, Cecchi A, Valent F, et al. Flight vibrations and bleeding in helicoptered patients with pelvic fracture. Air Med J 2013; 32: 80–83. [DOI] [PubMed] [Google Scholar]
- 36.Kupper T, Jansing P, Schoffl V, et al. Does modern helicopter construction reduce noise exposure in helicopter rescue operations? Ann Occup Hyg 2013; 57: 34–42. [DOI] [PubMed] [Google Scholar]
- 37.Thomson DP. Effects of flight. Emergency medical services, New York, NY: John Wiley & Sons, Ltd, 2015, pp. 368–371. [Google Scholar]
- 38.Knotts D, Arthur AO, Holder P, et al. Pneumothorax volume expansion in helicopter emergency medical services transport. Air Med J 2013; 32: 138–143. [DOI] [PubMed] [Google Scholar]
- 39.Iakubovich TG, Getsel' Kh A. The effect of vibration on the permeability of the blood-brain barrier. Fiziol Zh SSSR Im I M Sechenova 1972; 58: 845–850. [PubMed] [Google Scholar]
- 40.Andrew Hoffman HG. Externally applied vibration at 50 Hz facilitates dissolution of blood clots in-vitro. Am J Biomed Sci 2012; 4: 274–284. [Google Scholar]
- 41.Chalela JA, Kasner SE, Jauch EC, et al. Safety of air medical transportation after tissue plasminogen activator administration in acute ischemic stroke. Stroke 1999; 30: 2366–2368. [DOI] [PubMed] [Google Scholar]
- 42.Leira EC, Zaheer A, Schnell T, et al. Effect of helicopter transport on neurological outcomes in a mouse model of embolic stroke with reperfusion: Air-mice pilot study. Int J Stroke 2015; 10: 119–124. [DOI] [PubMed] [Google Scholar]
- 43.Jauch EC, Saver JL, Adams HP, Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44: 870–947. [DOI] [PubMed] [Google Scholar]
- 44.Saver JL, Starkman S, Eckstein M, et al. Prehospital use of magnesium sulfate as neuroprotection in acute stroke. N Engl J Med 2015; 372: 528–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kesinger MR, Sequeira DJ, Buffalini S, et al. Comparing national institutes of health stroke scale among a stroke team and helicopter emergency medical service providers. Stroke 2015; 46: 575–578. [DOI] [PubMed] [Google Scholar]