Abstract
Background
Airway anastomotic complications are a leading cause of mortality after lung transplantation. Among the factors that cause airway complications, preoperative steroid use has been considered to be related with postoperative airway healing. We analyzed the influence of preoperative steroid use on postoperative airway complications.
Methods
The medical records of 66 double-lung transplant recipients from January 2014 to December 2015 were reviewed. Forty patients were prescribed steroids preoperatively. The daily steroid dose was standardized using the patient’s body mass index (BMI). Patients who received preoperative steroids were sub-divided into high-dose (HD) and low-dose (LD) groups (cut-off value, 1.6 mg/BMI/day).
Results
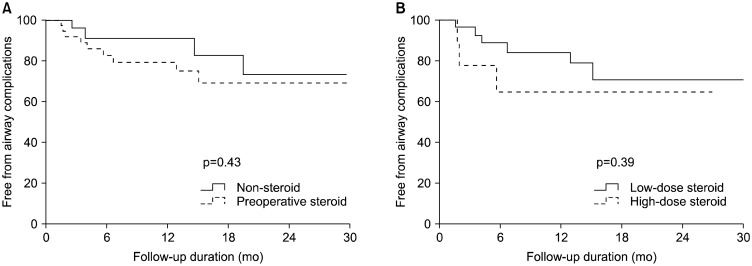
Thirteen patients suffered from airway complications postoperatively (bronchopulmonary fistula, 9; bronchial stenosis, 4). There was a tendency for early development of airway complications in the steroid use group compared to the non-steroid use group, but it was not significant (percentage free from airway complications in year 1: non-steroid group, 90.9% vs. steroid group, 79.2%; p=0.43). The percentage of patients in the LD and HD groups who were free from airway complications in year 1 was not significantly different (84.0% vs. 77.8%, p=0.39).
Conclusion
The airway complication rate did not vary significantly according to steroid use. Additionally, in patients who received preoperative steroids, the dose did not affect the rate of development of airway complications.
Keywords: Lung transplantation, Preoperative steroid, Airway, Complication
Introduction
Lung transplantation is the only viable treatment option for end-stage lung disease. The postoperative course and outcomes have gradually improved over the last few decades due to advances in surgical techniques and the development of immunosuppressants. However, critical complications can still occur, such as inadequate airway healing, infection, and rejection. Many patients with end-stage lung disease are prescribed corticosteroids to resolve inflammation. Preoperative steroid use has been considered to contribute to several postoperative complications, including poor bronchial anastomosis healing [1,2]. The reduction or discontinuation of high doses of corticosteroids is recommended before lung transplantation at most centers [3].
Previous international guidelines for the selection of lung transplantation candidates suggested that preoperative prednisone use was a contraindication for lung transplantation [2]. Other international guidelines for the selection of lung transplant candidates recommended making attempts to discontinue preoperative corticosteroids or at least to reduce the dose to ≥20 mg per day [4]. The debate about steroid dosing before lung transplantation is still ongoing. Several studies found no adverse effects of preoperative steroid use on survival, and a few studies reported that low doses of steroids (<0.3 mg/kg/day) could have a positive effect on bronchial stenosis [5,6]. Nevertheless, many centers still decrease or discontinue prednisone use before lung transplantation despite the limited evidence regarding the optimal preoperative dosing of steroids. In the field of transplantation, body mass index (BMI) has been repeatedly reported to affect the dose of immunosuppressive drugs, including prednisone [7].
The aim of this study was to evaluate the influence of preoperative steroid use on airway complications.
Methods
For this retrospective analysis, we reviewed our transplantation database and electronic medical records. Between January 2014 and December 2015, a total of 66 patients underwent double-lung transplantation, of whom 40 patients were prescribed steroids preoperatively and 26 were not. We defined preoperative steroid use as the use of steroids within 1 month prior to the transplantation. To standardize each patient’s daily dose of steroids, the preoperative steroid dose was converted to the corresponding dose of prednisolone and divided by the patient’s BMI. After ranking the quotients from lowest to highest, a mean result was obtained (prednisolone, 1.6 mg/BMI/day; range, 0.2 to 6.9 mg/BMI/day). Patients were divided into high-dose (HD) and low-dose (LD) groups. Patients with a daily prednisolone dose higher than 1.6 mg/BMI/day were assigned to the HD group (n=11). The other 29 patients who received <1.6 mg/BMI/day of prednisolone were assigned to the LD group. The median daily prednisolone dose in the HD group was 171.7 mg/day (range, 40.0 to 1,000 mg per day) and that in the LD group was 12.8 mg/day (range, 3.0 to 30.0 mg per day).
The induction and maintenance of immunosuppression were similar in all patients. Our postoperative immunosuppressive protocol was performed according to the triple immunosuppressive regimen, including tacrolimus, mycophenolate mofetil, and steroids [8]. Methylprednisolone (500 mg, intravenous [IV]) was administered just before reperfusion of the transplanted lungs, and its administration was continued to the third postoperative day at 0.5 mg/kg/day. On the fourth postoperative day, IV methylprednisolone was switched to oral prednisolone at 0.5 mg/kg/day. The daily dose of prednisolone was gradually tapered to 0.25 mg/kg/day. Tacrolimus administration started on the day of the operation. The dose was adjusted to maintain a serum level of 8 to 12 ng/mL. Mycophenolate mofetil was administered at 1,000 mg/day routinely, unless leukocytopenia occurred.
The operative technique and the initial postoperative care after lung transplantation followed routine procedural steps. Bronchial anastomosis was performed using the end-to-end method approximately 1 ring above the donor second carina. A running 4-0 polydioxanone suture was used for the membranous portion, while multiple interrupted 4-0 polydioxanone sutures were used for the cartilage portion [9]. The anastomosis site was wrapped with pericardial tissue using a Vicryl 4-0 suture to maintain its integrity.
Airway complications, such as bronchopulmonary fistula and bronchial stenosis, were confirmed from bronchoscopy findings. We defined bronchopulmonary fistula as the presence of air bubbles at the anastomosis site after a saline injection test using bronchoscopy. Bronchial stenosis was defined as the presence of granulation tissue or fibrosis in the airway lumen at the site of the airway anastomosis.
All data were collected retrospectively. General demographic data and postoperative variables were expressed as the mean±standard deviation, median (range), or as percentages. Comparisons between groups were performed using the chi-square and Fisher exact tests as appropriate. Survival curves were generated by Kaplan-Meier analysis and were compared by log-rank analysis. All p-values <0.05 were considered to indicate statistical significance. Statistical analyses were performed with IBM SPSS for Windows ver. 23.0 (IBM Corp., Armonk, NY, USA).
This study was approved by the Institutional Review Board of Yonsei University (IRB approval no., 4-2018-0958), and patient consent was waived.
Results
The mean age of the 66 transplant patients was 50.8±14.7 years. All of them underwent bilateral lung transplantation. Fifty-nine percent of the transplant recipients were males. The mean follow-up duration was 29.5±20.8 months. Table 1 presents the demographic profile of the patients. The disease entities were not significantly different between the steroid group and the non-steroid group (p=0.61). The most common disease in both groups was pulmonary fibrosis (n=43, 65.2%). The duration of time spent in the intensive care unit and the length of the post-transplantation follow-up interval were comparable. However, the length of hospital stay was slightly longer in the steroid group, although the difference was not statistically significant (83.8±88.2 days versus 62.7±63.5 days, p=0.30). The preoperative forced expiratory volume in 1 second did not show a statistically significant difference between the groups (p= 0.45).
Table 1.
Baseline characteristics of patients according to whether they received steroids preoperatively
| Characteristic | Total (n=66) | Preoperative steroid (n=40) | No steroid (n=26) | p-value |
|---|---|---|---|---|
| Age (yr) | 50.8±14.7 | 50.2±15.0 | 51.6±14.4 | 0.70 |
| Sex | 0.74 | |||
| Male | 39 (59.1) | 17 (42.5) | 16 (61.5) | |
| Female | 27 (40.9) | 23 (57.5) | 10 (38.5) | |
| Total follow-up duration (mo) | 29.5±20.8 | 26.8±18.2 | 33.7±24.0 | 0.19 |
| Disease entity | 0.61 | |||
| Pulmonary fibrosis | 43 (65.2) | 27 (67.5) | 16 (61.5) | |
| Organizing pneumonia | 14 (21.2) | 11 (27.5) | 3 (11.5) | |
| Lymphangioleiomyomatosis | 2 (3.0) | 0 | 2 (7.7) | |
| Bronchiectasis | 5 (7.6) | 2 (3.0) | 3 (11.5) | |
| Primary pulmonary hypertension | 2 (3.0) | 0 | 2 (7.7) | |
| Preoperative forced expiratory volume in 1 second | 1.70±0.55 | 1.63±0.56 | 1.81±0.54 | 0.45 |
| Airway complication | 13 (19.7) | 9 (22.5) | 4 (14.3) | 0.47 |
| Bronchopulmonary fistula | 9 (13.6) | 6 (15.0) | 3 (11.5) | |
| Bronchial stenosis | 4 (6.1) | 3 (7.5) | 1 (3.8) | |
| Length of stay (day) | 75.7±79.8 | 83.8±88.2 | 62.7±63.5 | 0.30 |
| Intensive care unit stay (day) | 23.7±32.4 | 23.5±30.2 | 24.1±36.2 | 0.95 |
Values are presented as mean±standard deviation or number (%).
Within the preoperative steroid group, the patients were sub-divided into HD and LD groups. There were no significant differences in the disease entities between these groups (Table 2). A total of 13 patients (19.7%) experienced airway complications postoperatively. Six of these patients belonged to the LD group. Of those 6 patients, 2 developed right bronchial stenosis at a site distal to the anastomosis site. After several balloon dilation procedures, they recovered. The remaining 4 developed bronchopleural fistula. They all died from sepsis during the first postoperative year. Three patients in the HD group experienced airway complications. Two of them suffered bronchial stenosis. One of these 2 patients recovered after 2 balloon dilation procedures, while the other died on postoperative day 49 due to ventricular fibrillation. One patient in the HD group developed bronchopleural fistula. He died due to sepsis on postoperative day 56.
Table 2.
Comparison between high-dose and low-dose groups among patients who received steroids preoperatively
| Variable | Low dose (n=29) | High dose (n=11) | p-value |
|---|---|---|---|
| Disease entity | 0.54 | ||
| Pulmonary fibrosis | 20 (68.0) | 7 (63.6) | |
| Organizing pneumonia | 7 (24.1) | 4 (36.4) | |
| Bronchiectasis | 2 (6.9) | 0 | |
| Prednisolone dose (mg/BMI/day) | 12.8 (3.0–30.0) | 171.0 (40.0–1,000.0) | 0.004 |
| BMI (kg/m2) | 21.1±3.9 | 20.2±4.3 | 0.49 |
| Prednisolone dose (mg/BMI) | 0.6±0.4 | 4.3±2.6 | 0.001 |
| Intensive care unit stay (day) | 23.9±32.4 | 22.5±7.5 | 0.67 |
| Length of hospital stay (day) | 62.7±46.4 | 97.8±113.0 | 0.01 |
| Airway complication | 6 (24.0) | 3 (27.3) | 0.65 |
| Bronchopulmonary fistula | 4 (16.0) | 2 (18.2) | |
| Bronchial stenosis | 2 (8.0) | 1 (9.1) |
Values are presented as number (%), median (range), or mean±standard deviation.
BMI, body mass index.
No statistically significant difference was found in the incidence of airway complications between the non-steroid and preoperative steroid groups, although there was a tendency for the early development of airway complications in the preoperative steroid group (percentage free from airway complications in year 1: non-steroid group, 90.9% versus steroid group, 79.2%; p=0.43) (Fig. 1A). Within the steroid-use sub-groups, there was no significant difference in the airway complication rate during follow-up according to dosage (percentage free from airway complications in year 1: LD group, 84.0% versus HD group, 77.8%; p=0.39) (Fig. 1B).
Fig. 1.
Freedom from airway complications in the (A) steroid versus non-steroid groups, (B) and the high-dose versus low-dose groups.
Discussion
Airway complications are among the leading causes of morbidity after lung transplantation. These complications continue to occur despite advances in operative techniques and perfusion preservation [6].
Several factors play a role in the etiology of airway complications. It was believed that perioperative steroid therapy might have a negative effect on bronchial anastomosis healing [10]. However, the use of corticosteroids for end-stage lung disease is common. Up to 66% of patients on the waiting list for lung transplantation have received preoperative corticosteroids. Preoperative corticosteroid therapy was initially considered an absolute contraindication to lung transplantation [2]. However, recent evidence has demonstrated that the previously reported negative effects of corticosteroids are equivocal [3,5]. A few clinical studies reported the possibility of normal bronchial healing despite the administration of corticosteroids [11]. From recent studies, it seems clear that a small to moderate dose of corticosteroids during the pre-transplant period does not adversely affect the postoperative outcome [5,12]. Moreover, some studies reported that patients on low doses of prednisolone (<0.42 mg/kg/m2) had better survival outcomes than those on high doses [3,5,10]. In this study population, the daily prednisolone dosage ranged from 3.0 to 1,000.0 mg. We used the BMI to standardize the optimal dose of steroids. The doses ranged from 0.2 to 6.9 mg/BMI/day. Sub-group analyses were performed to compare patients who received high and low doses. The median dosage was 1.6 mg/BMI/day.
In this study, regardless of the preoperative diagnosis and irrespective of when the patient underwent lung transplantation, the airway complication rate was not significantly different between the steroid and non-steroid groups. Sub-group analyses comparing the HD group with the LD group also revealed no statistically significant differences in terms of airway complications. However, although these findings were not statistically significant, our results showed a higher tendency for airway complications in the HD group during the first postoperative year. The possibility that the outcome of patients who received high doses of corticosteroids was poorer in the early postoperative period cannot be ignored. To determine the effect of low doses of corticosteroids, we additionally performed sub-group analyses of the non-steroid group and the LD group (data not shown). No significant differences in airway complications were found between these groups.
As is well known, bronchial dehiscence is a disastrous complication that occurs during the postoperative period in transplant recipients. Most cases involving bronchial dehiscence resulted in death due to sepsis. Bronchial dehiscence occurs early after lung transplantation and is difficult to treat. Bronchial stenosis is the most frequent complication after lung transplantation. Mechanical obstruction due to ingrown granulation tissue can be managed with rigid bronchoscopy by the removal of additional tissue and the insertion of silicone or an expendable stent. If this procedure fails, surgical resection of the obstructed portion can be considered [13]. In our cohort, 4 patients experienced bronchial stenosis after transplantation. Their conditions were successfully reversed after several balloon dilation procedures.
As in the present study, many recent studies found no correlation between pre-transplantation steroid use and early outcomes, especially airway complications. The results of this study provide further support for the acceptability of preoperative steroid use in patients on the lung transplant waitlist. However, the optimal dosage still remains uncertain. The lowest preoperative steroid dose in the HD group of this study was 40 mg/day or 1.75 mg/BMI/day, and the median preoperative steroid dose was 1.6 mg/BMI/day. Although there was no statistically significant difference in airway complications between the LD and HD groups, there seemed to be a trend for a higher airway complication rate in the HD group. Therefore, it is important to personalize the preoperative steroid dose and to limit the dosage in order to improve the early postoperative course.
In conclusion, preoperative corticosteroid use did not seem to affect the occurrence of airway complications after lung transplantation. Therefore, the use of corticosteroids should not be considered a contraindication for lung transplantation. However, the airways of patients who receive high doses of steroids must be carefully monitored during the early follow-up period.
Acknowledgments
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund no. KTCS04-111).
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Lima O, Cooper JD, Peters WJ, et al. Effects of methylprednisolone and azathioprine on bronchial healing following lung autotransplantation. J Thorac Cardiovasc Surg. 1981;82:211–5. [PubMed] [Google Scholar]
- 2.Schafers HJ, Wagner TO, Demertzis S, et al. Preoperative corticosteroids: a contraindication to lung transplantation? Chest. 1992;102:1522–5. doi: 10.1378/chest.102.5.1522. [DOI] [PubMed] [Google Scholar]
- 3.McAnally KJ, Valentine VG, LaPlace SG, McFadden PM, Seoane L, Taylor DE. Effect of pre-transplantation prednisone on survival after lung transplantation. J Heart Lung Transplant. 2006;25:67–74. doi: 10.1016/j.healun.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Maurer JR, Frost AE, Estenne M, Higenbottam T, Glanville AR. International guidelines for the selection of lung transplant candidates: the International Society for Heart and Lung Transplantation, the American Thoracic Society, the American Society of Transplant Physicians, the European Respiratory Society. Transplantation. 1998;66:951–6. doi: 10.1097/00007890-199810150-00033. [DOI] [PubMed] [Google Scholar]
- 5.Park SJ, Nguyen DQ, Savik K, Hertz MI, Bolman RM., 3rd Pre-transplant corticosteroid use and outcome in lung transplantation. J Heart Lung Transplant. 2001;20:304–9. doi: 10.1016/S1053-2498(00)00316-8. [DOI] [PubMed] [Google Scholar]
- 6.Alvarez A, Algar J, Santos F, et al. Airway complications after lung transplantation: a review of 151 anastomoses. Eur J Cardiothorac Surg. 2001;19:381–7. doi: 10.1016/S1010-7940(01)00619-4. [DOI] [PubMed] [Google Scholar]
- 7.Westenfeld R, Schlieper G, Woltje M, et al. Impact of sirolimus, tacrolimus and mycophenolate mofetil on osteoclastogenesis: implications for post-transplantation bone disease. Nephrol Dial Transplant. 2011;26:4115–23. doi: 10.1093/ndt/gfr214. [DOI] [PubMed] [Google Scholar]
- 8.Venuta F, van Raemdonck D. History of lung transplantation. J Thorac Dis. 2017;9:5458–71. doi: 10.21037/jtd.2017.11.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Griffith BP, Magee MJ, Gonzalez IF, et al. Anastomotic pitfalls in lung transplantation. J Thorac Cardiovasc Surg. 1994;107:743–53. [PubMed] [Google Scholar]
- 10.De Boer WJ, Mannes GP, van der Bij W. Preoperative corticosteroids: a contraindication to lung transplantation? Chest. 1994;105:1908. doi: 10.1378/chest.105.6.1908a. [DOI] [PubMed] [Google Scholar]
- 11.Miller JD, DeHoyos A. An evaluation of the role of omentopexy and of early perioperative corticosteroid administration in clinical lung transplantation: the University of Toronto and Washington University Lung Transplant Programs. J Thorac Cardiovasc Surg. 1993;105:247–52. [PubMed] [Google Scholar]
- 12.Groetzner J, Kur F, Spelsberg F, et al. Airway anastomosis complications in de novo lung transplantation with sirolimus-based immunosuppression. J Heart Lung Transplant. 2004;23:632–8. doi: 10.1016/S1053-2498(03)00309-7. [DOI] [PubMed] [Google Scholar]
- 13.Frye L, Machuzak M. Airway complications after lung transplantation. Clin Chest Med. 2017;38:693–706. doi: 10.1016/j.ccm.2017.07.010. [DOI] [PubMed] [Google Scholar]