Abstract
Objectives. To examine whether stressful job exposure to the public could be associated with having long-term benzodiazepine use.
Methods. From the participants included between 2012 and 2016 in the French population-based CONSTANCES cohort, 13 934 men and 19 261 women declared a daily job exposure to the public and rated the frequency of stressful exposure. We examined benzodiazepine long-term use by using drug reimbursement administrative registries. Logistic regressions provided odds ratios (ORs) of benzodiazepine long-term use, with stratification for gender and adjustment for age, education, and area deprivation index. Occupational grade, job strain, depression, self-rated health, and alcohol use disorder were additional stratification variables.
Results. Benzodiazepine long-term use was positively associated with stressful exposure to the public (“often or always” vs “rarely or never”) in men (OR = 2.2; 95% confidence interval [CI] = 1.8, 2.8) and women (OR = 1.6; 95% CI = 1.4, 1.9), with dose-dependent relationships (P trends < .001). Adjustments and analyses in subgroups without other individual or environmental vulnerability factors led to similar results.
Conclusions. Stressful job exposure to the public increases the risk of benzodiazepine long-term use. Prevention programs aiming at reducing the burden of benzodiazepine long-term use would benefit in targeting this specific population.
Benzodiazepines are the most prescribed drugs worldwide and they are primarily used for their anxiolytic properties.1 For instance, in the United States, alprazolam was the most prescribed drug in 2013.2 In France, 17% of the entire population had used a benzodiazepine at least once in 2012,3 and about 4% to 5% of the Norwegian population used benzodiazepines daily in 2007.4 Moreover, benzodiazepine consumption frequently persists beyond the recommended short durations of prescriptions.1,4 For instance, in the United Kingdom, between 1991 and 2009, inappropriate consumption of benzodiazepines may represent two thirds of all benzodiazepine prescriptions.1
However, long-term exposure to benzodiazepines is associated with substantial side effects, including risk of dependency and related symptoms (e.g., craving, withdrawal symptoms) and potentially life-threatening side effects such as increased risks of falls, car crash, respiratory failure, cancers, and Alzheimer disease.1 Regarding psychological side effects, cognitive impairments, depressive mood, and sleep disorders have been described, as well as increased impulsivity that could lead to suicidal behaviors.1 To prevent these detrimental effects, screening for benzodiazepine long-term use is crucial. However, such screening may not be easily performed in primary care.5 In addition, not only is spontaneous self-reporting often unreliable, at least because of a lack of knowledge about the type of medication used and its associated risks,6 but misreporting is also likely during targeted screening. Indicators of an elevated risk of benzodiazepine long-term use would therefore be particularly useful to target at-risk populations for both screening and preventive strategies.
Several vulnerability factors of benzodiazepine long-term use have been described such as low occupational grade,7 depression,8 alcohol use disorder,9 and poor health status.10 In the context of occupational medicine, job strain (e.g., work overload or underload, low rewards) has been associated with detrimental mental health11 and with substance use,12 including psychotropic drug use.13–15 Nevertheless, even without experiencing job strain, some stressful work conditions have been related with substance use.14
Among these stressful conditions, emotional job demand is of major concern as the labor market turns increasingly to the tertiary sector. Emotional job demand is an occupational risk that could lead to high levels of interpersonal stress in the workplace. More precisely, emotional job demand refers to displaying demands (i.e., expressing positive, negative, and neutral emotions toward public), facing sensitivity demands (e.g., guessing what the public is feeling), and dealing with potential emotional mistreatments (e.g., facing the dissatisfaction of a client).16 As a consequence, emotional demand concerns jobs that are exposed to the public (e.g., customers, guests, users of a public service, patients).
Even if all types of jobs could potentially meet this criterion according to work organization and specific tasks within each company, some of them have been found to be particularly exposed to high levels of emotional demand because of the nature of the public encountered, such as in education and health care professions.17 For instance, teachers face a wide range of job stressors (e.g., poor pupil motivation, misbehavior) although they have to always model successful emotional control.18 Those in health care professions face daily highly emotionally charged situations, including suffering, fear, and death, as well as difficult interactions with patients, families, and others.19 These situations of work stress have been associated with detrimental health conditions, including substance use.19,20 Conversely, drug adverse effects can lead to additional difficulties while dealing afterward with emotional demand. However, all workers who are daily exposed to the public could be concerned by high levels of emotional demand and its related detrimental health behaviors. For instance, stressful job exposure to the public was found to be significantly associated with alcohol, tobacco, and cannabis use, even after adjustment for sociodemographic factors, depressive symptoms, and job strain.17
With regard to benzodiazepine long-term use, there are still very limited data. However, benzodiazepines are frequently used as a maladaptive way of coping with stressful situations, including interpersonal difficulties. For instance, self-reported psychotropic drug use, including use of benzodiazepines, has been associated with the tendency of hiding feelings at work or having to pretend to be in good mood.14
To the best of our knowledge, there is no previous study that specifically examined the associations between stressful job exposure to the public and benzodiazepine long-term use in a large population-based cohort of daily exposed workers, while measuring benzodiazepine use with administrative registries rather than self-reporting, and taking into account confounding effects of other individual or sociodemographic factors. The CONSTANCES cohort includes a large randomized sample of the French population from various occupational status types and sociodemographic factors.21 Its linkage with national databases of reimbursed drugs offers a unique opportunity to measure benzodiazepine long-term use independently from self-disclosure.
Here we took advantage of the CONSTANCES cohort to examine the cross-sectional associations between stressful exposure to the public and benzodiazepine long-term use among daily exposed workers. We hypothesized that such stressful exposure may be associated with an increased risk for having long-term use of benzodiazepines. In addition, the large sample size of the CONSTANCES cohort allowed us to examine this association in men and women separately. These gender-specific analyses were planned for several reasons. Both sensitivity and intensity of emotional demand may vary across gender,16,22 and women may be more prone to using drugs to cope with stressful environmental situations.14 Gender differences have also been found in examinations of the association between emotional demand and substance use.15,17 In addition, we examined whether any association between benzodiazepine long-term use and stressful exposure to the public may persist among participants with no other indicators of individual or environmental vulnerability, including low occupational grade,7 job strain,10,15 depressive symptoms,8 alcohol use disorder,9 and health status.10
METHODS
The CONSTANCES cohort is a national population-based cohort of randomly recruited participants, including volunteers aged 18 to 69 years at baseline in 22 selected health screening centers from the principal regions of France.21 In our study, we used the data collected at baseline for the participants included from February 2012 to September 2016 and having a job including a physical or a phone contact with the public (e.g., clients, patients, users) every day or almost every day. Within this subgroup, 33 195 (98%) responded to the assessment of the frequency of stressful job exposure to the public. All of them have been included in statistical analyses (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
Stressful Job Exposure to the Public
Participants were asked the following question, exclusively related to their occupational life: “Do you live stressful situations in your relationships with the public?” They had to choose 1 of the following 4 responses: (1) never or almost never, (2) rarely, (3) often, and (4) always or almost always. A previous study by our group showed that associations between emotional job demand and substance use were different when we used this measure of stressful job exposure to the public compared with a measure of exposure per se.17 In addition, associations with this measure were stronger in professional sectors associated with high levels of emotional demand, such as education and health care. Finally, the associations between this measure and substance use were independent from job strain. In the present study, job strain has been measured with the effort–reward imbalance (please see “Covariables”).
Benzodiazepine Long-Term Use
One of the unique features of the CONSTANCES cohort is its systematic linkage to the SNIIRAM (Système national d’information inter-régimes de l’Assurance maladie) database.21 This national administrative database contains detailed individual medical data for almost the whole French population and, in particular, reimbursement data including prescribed drugs.23 At the time of study, reimbursement data for CONSTANCES participants were available from January 2009 to December 2014.
Filled prescriptions for all benzodiazepines having a marketing authorization in France were extracted from the database. These benzodiazepines are the following: clonazepam, chlordiazepoxide, oxazepam, potassium clorazepate, lorazepam, bromazepam, clobazam, prazepam, alprazolam, nordazepam, ethyl loflazepate, and clotiazepam. Then, we used automated algorithms to search for sequences of prescription indicating a continuous period of prescription longer than the maximum duration authorized in France (i.e., 12 weeks).24 This long-term exposure, leading to side effects such as dependency, is inappropriate regarding the French good practice recommendations and was used to define benzodiazepine long-term use.24 On the basis of the assumption that a prescription usually covers 1 month, we considered that the sequences with the following criteria were likely to signal a long-term use: (1) at least 2 refills in the 12 weeks following the first prescription and (2) at least 1 refill in week 13 or 14 or at least 1 refill in week 15 or 16 if the last refill observed during the first 12 weeks occurs on week 11 or 12. On the basis of this classification, we computed a binary outcome for long-term use (i.e., presence vs absence).
Covariables
From the baseline questionnaires, we used age, gender, education based on the International Standard Classification of Education (i.e., levels 0–1, level 2, levels 3–4, levels 5–6), and occupational grade (i.e., farmer, blue-collar worker, and craftsman; clerk; intermediate worker; executive). These variables were collected as categorical ones, except for age. The area deprivation index was used as a proxy of spatial socioeconomic disparities.21 We computed this index on the basis of data from a population census in 2009 and we used reverse deciles so that increased values indicated increased deprivation.
We used the effort–reward imbalance, measured as a continuous variable, to search for job strain.25 We used this score as a binary variable corresponding to the affiliation to the first tertile (i.e., least vulnerable participants) or to the following 2. Depressive symptoms were collected as a continuous variable with the Center of Epidemiologic Studies Depression scale.26 As a global score of 19 or more may signal a clinically meaningful depressive state, we used this cut-off to provide a proxy of depressive state. Alcohol use risk categories were defined from the total score at the Alcohol Use Disorders Identification Test as follows: (1) mild (0–7), (2) dangerous (8–15), (3) problematic (16–19), and (4) dependence (20–40).27 We merged the 3 last categories to provide a binary variable regarding at-risk alcohol use. Self-rated health status was measured from the following question: “How do you judge your general health compared to a person of your entourage of the same age?” to provide a proxy of overall physical and psychological health condition, also in relation with mortality.28 We computed a binary variable to define a good general health (1–4) versus a poor one (5–8).
Statistical Analysis
We used our dependent variable (i.e., benzodiazepine long-term use) in 2-sided binomial logistic regressions, taking the absence of long-term use as reference category. Results are presented as estimated odds ratios (ORs) with their 95% confidence intervals (CIs).
In univariable analysis, we examined the associations between our dependent variable and each covariable. First, we computed the risk of benzodiazepine long-term use following gender and, thereafter, in accordance with our objective to examine the associations in men and women separately; all the other univariable analyses were stratified by gender.
In multivariable analysis, we examined the associations between stressful exposure to the public and benzodiazepine long-term use, while adjusting for age, education, and area deprivation index as continuous covariables. First, we introduced gender as additional covariable to search for an interaction between gender and stressful exposure to the public and, thereafter, we used gender as a variable of stratification for all the other multivariable analyses.
To avoid having too many small-size cells in multiadjusted models, stressful exposure to the public was mainly used as binary variable by aggregating categories (1) and (2) on the one hand, and categories (3) and (4) on the other hand (i.e., “never or rarely” vs “often or almost always”). However, we also searched for a potential dose–response relationship by using stressful exposure to the public in 4 categories, taking “never stressful exposure” as reference category.
Finally, we performed sensitivity analyses in subgroups to explore whether the associations would be persistent whatever occupational grade, effort–reward imbalance, depressive state, at-risk alcohol use, or self-rated health status. Stratifying was preferred over adjustment to provide further insight about the relevance of stressful job exposure to the public as an indicator of benzodiazepine long-term use in specific subgroups, especially those at low risk (i.e., high occupational grade, low job strain, no depression, no at-risk alcohol use, or good health status). More specifically, mere adjustment would not have allowed us to compute ORs within each stratum.
Thanks to the systematic linkage of the CONSTANCES cohort with the SNIIRAM database including drug reimbursement administrative registries, we had no missing data regarding our dependent variable. Regarding covariables, we had no missing data for gender, age, and area deprivation index. For the other covariables, missing data were managed by stochastic regression imputation to adjust the results of the entire sample for all covariables,29 as stated in Table A (available as a supplement to the online version of this article at http://www.ajph.org).
We performed analyses with IBM Statistics for Windows, version 22.0 (IBM Corp, Armonk, NY).
RESULTS
Among a total of 13 934 men and 19 261 women included in the present study, 306 men and 624 women had benzodiazepine long-term use between 2009 and 2014. The characteristics of included participants are displayed in Table A, stratified by gender. Women had a higher risk of benzodiazepine long-term use than men with an OR of 1.5 (95% CI = 1.3, 1.7). In both men and women, benzodiazepine long-term use was positively associated with age; being a clerk, farmer, blue-collar worker, or craftsman compared with an executive worker; effort–reward imbalance; depressive state; at-risk alcohol consumption; and poor self-rated health status and negatively associated with education (all P < .05; Table 1). Benzodiazepine long-term use was also positively associated with the area deprivation index in women and with being an intermediate worker rather than an executive worker in men (P < .05 for both; Table 1).
TABLE 1—
Associations Between Each Covariable and Benzodiazepine Long-Term Use Among 13 934 Men and 19 261 Women: CONSTANCES Cohort, France, 2012–2016
| Men | Women | |||
| Univariable, OR (95% CI) | Multivariable, OR (95% CI) | Univariable, OR (95% CI) | Multivariable, OR (95% CI) | |
| Continuous variables | ||||
| Age, y | 1.041 (1.029, 1.053) | 1.038 (1.025, 1.050) | 1.044 (1.035, 1.053) | 1.037 (1.029, 1.046) |
| Area deprivation index, deciles | 1.015 (0.976, 1.055) | 0.985 (0.946, 1.026) | 1.040 (1.012, 1.070) | 1.024 (0.995, 1.054) |
| Educationa | 0.716 (0.638, 0.803) | 0.750 (0.666, 0.844) | 0.632 (0.581, 0.689) | 0.691 (0.632, 0.755) |
| Categorical variables | ||||
| Stressful exposure to the public in the workplace | ||||
| Never or rarely (Ref) | 1 | 1 | 1 | 1 |
| Often or almost always | 2.202 (1.752, 2.767) | 2.201 (1.750, 2.768) | 1.609 (1.368, 1.892) | 1.653 (1.404, 1.946) |
| Occupational status | ||||
| Executive (Ref) | 1 | 1 | ||
| Intermediate worker | 1.510 (1.056, 2.159) | 1.224 (0.678, 2.209) | ||
| Clerk | 1.920 (1.411, 2.618) | 2.213 (1.738, 2.817) | ||
| Farmer, blue-collar worker, and craftsman | 1.377 (1.020, 1.860) | 1.349 (1.042, 1.745) | ||
| Effort–reward imbalanceb | ||||
| First tertile (Ref) | 1 | 1 | ||
| Second or third tertiles | 1.924 (1.533, 2.415) | 1.648 (1.404, 1.936) | ||
| Depressive statec | ||||
| No (Ref) | 1 | 1 | ||
| Yes | 5.473 (4.323, 6.930) | 4.526 (3.852, 5.318) | ||
| Alcohol use risk leveld | ||||
| Mild risk (Ref) | 1 | 1 | ||
| At risk | 1.605 (1.260, 2.045) | 1.396 (1.083, 1.800) | ||
| Self-rated health statuse | ||||
| Good (Ref) | 1 | 1 | ||
| Poor | 3.997 (3.125, 5.113) | 3.324 (2.790, 3.959) | ||
Note. CI = confidence interval; OR = odds ratio.
According to the International Standard Classification of Education in 5 levels.
Computed from 7 items regarding rewards and from 3 items regarding efforts as follows: effort–reward imbalance = (7/3)*(effort total score/reward total score), and with all the items assessed on a 4-point Likert scale.
Defined as a score ≥ 19 on the Center for Epidemiologic Studies Depression Scale.
Categories are defined from Alcohol Use Disorders Identification Test scores as follows: mild (0–7), at risk (8–40).
“How do you judge your general health compared to a person of your entourage of the same age?” defined a good self-rated health (1–4) vs a poor one (5–8). Odds ratios were computed through logistic regression models. Multivariable associations between stressful exposure to the public and benzodiazepine long-term use were adjusted for age, area deprivation index, and education.
Stressful Exposure to the Public and Long-Term Benzodiazepine Use
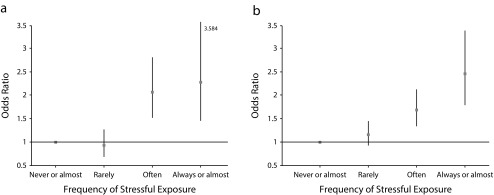
Benzodiazepine long-term use was positively associated with stressful job exposure to the public in both men and women (OR = 2.2; 95% CI = 1.8, 2.8 and OR = 1.6; 95% CI = 1.4, 1.9, respectively; Table 1). These associations provided similar effect estimates in multivariable analyses (Table 1), and we found an interaction between gender and stressful exposure to the public (Wald χ2 = 4.09; P = .043). When searching for a dose–response relationship, we found that both “often” and “always or almost [always]” exposures were associated with an increased risk of benzodiazepine long-term use and with increased ORs following the frequency of exposure: from 2.1 (95% CI = 1.5, 2.8) to 2.3 (95% CI = 1.5, 3.6) and from 1.7 (95% CI = 1.3, 2.1) to 2.5 (95% CI = 1.8, 3.4) in men and women, respectively (all P < .001 and P for linear trend < .001 in both genders; Figure 1).
FIGURE 1—
Odds Ratios of Benzodiazepine Long-Term Use According to the Frequency of Stressful Exposure to the Public in (a) 13 934 Men and (b) 19 261 Women: CONSTANCES Cohort, France, 2012–2016
Note. Figure 1 presents odds ratios (and their 95% confidence intervals) of benzodiazepine long-term use according to the frequency of stressful exposure to the public (rarely, often, and always or almost always, compared with never or almost never) in both men and women, and adjusted for age, education, and area deprivation index. P for trend for both men and women was < .001.
Sensitivity Analysis
In both genders, the positive associations between benzodiazepine long-term use and stressful exposure to the public, adjusted for age, education, and area deprivation index, persisted whatever the occupational grade, except for the “farmer, blue-collar worker, and craftsman” category (Table 2). When we stratified for effort–reward imbalance, depressive state, self-rated health status, and at-risk alcohol consumption, these associations persisted in men and women, with the only exceptions in women with at-risk alcohol consumption and poor self-rated health status, possibly because of limited statistical power, at least for alcohol consumption (Table 2).
TABLE 2—
Stratified Analyses of the Associations Between Benzodiazepine Long-Term Use and Stressful Exposure to the Public in the Workplace Among 13 934 Men and 19 261 Women: CONSTANCES Cohort, France, 2012–2016
| Stratification Variable | Men, ORa (95% CI) | Women, ORa (95% CI) |
| Occupational grade | ||
| Executive | 2.699 (1.735, 4.196) | 1.821 (1.179, 2.813) |
| Intermediate worker | 2.070 (1.363, 3.143) | 1.687 (1.267, 2.247) |
| Clerk | 2.556 (1.645, 3.970) | 1.651 (1.314, 2.074) |
| Farmer, blue-collar worker, and craftsman | 1.131 (0.572, 2.236) | 0.973 (0.258, 3.664) |
| Effort–reward imbalanceb | ||
| First tertile | 1.762 (1.255, 2.474) | 1.515 (1.202, 1.910) |
| Second or third tertile | 2.196 (1.570, 3.073) | 1.509 (1.184, 1.924) |
| Depressive statec | ||
| No depressive state | 1.767 (1.309, 2.385) | 1.367 (1.077, 1.734) |
| Depressive state | 1.966 (1.345, 2.874) | 1.398 (1.107, 1.766) |
| Alcohol use risk leveld | ||
| Mild risk | 1.747 (1.315, 2.322) | 1.667 (1.402, 1.981) |
| At risk | 3.379 (2.251, 5.072) | 1.443 (0.884, 2.356) |
| Self-rated health statuse | ||
| Good | 1.817 (1.370, 2.409) | 1.690 (1.389, 2.057) |
| Poor | 2.547 (1.677, 3.869) | 1.189 (0.883, 1.600) |
Note. CI = confidence interval; OR = odds ratio. Associations were adjusted for age, education, and area deprivation index.
Odds ratios were computed through multivariable logistic regression models. Stressful exposure to the public in the workplace was used as a binary variable as follows: “often or almost always” vs “never or rarely” as reference category.
Computed from 7 items regarding rewards and from 3 items regarding efforts as follows: effort–reward imbalance = (7/3)*(effort total score/reward total score), and with all the items assessed on a 4-point Likert scale.
Defined as a score ≥ 19 on the Center for Epidemiologic Studies Depression Scale.
Categories are defined from Alcohol Use Disorders Identification Test scores as follows: mild (0–7), at risk (8-40).
“How do you judge your general health compared to a person of your entourage of the same age?” defined a good self-rated health (1–4) vs a poor one (5–8).
DISCUSSION
Stressful job exposure to the public was positively associated with having benzodiazepine long-term use in a large population-based sample, in both men and women, and with dose-dependent relationships. These associations provided similar effect estimates after adjustment for age, education, and area deprivation index in both genders. Furthermore, it persisted even in the absence of other indicators of individual or environmental vulnerability.
Strengths and Limitations
To our knowledge, this is the first study that explored the specific association between stressful job exposure to the public and benzodiazepine long-term use in a large population-based sample of randomly recruited men and women while taking into account several potential confounding or moderating factors. In addition, our study relied on an objective assessment of benzodiazepine use, which was available without any missing data.21 Although the validity of our definition of long-term use could be questioned, we are not aware of a standard definition of long-term use against which it could be validated. Moreover, the results of univariable analyses were consistent with the literature regarding the association of benzodiazepine long-term use with female gender,7 older age,30 low education,7 low occupational grade,7 occupational stress,14,15 depressive symptoms,4,30 alcohol use disorder,9 and poor health status.1 This consistency with the literature thus provides a strong validity to our assessment of benzodiazepine long-term use.
Our study has some limitations. First, the observational cross-sectional design does not allow us to determine the direction of the association. Second, even if recruitment in the CONSTANCES cohort is based on a random sampling design, it is not representative per se of the general population because of selection effects associated with voluntary participation. Third, we could not ascertain that reimbursed medications were actually used, and this method of assessment did not include over-the-counter consumptions. However, going to the pharmacy to get benzodiazepines at least 4 times without actual intake may be unlikely. Moreover, benzodiazepines cannot be obtained without prescription in France; thus, over-the-counter consumption is more restricted than in other countries where these drugs can be purchased without prescription. Fourth, stressful exposure to the public was assessed by a unique question whose wording did not allow us to disentangle the role of exposure per se from the role of individual sensitivity to this exposure, which may differently relate to benzodiazepine long-term use. Anyway, we were interested in identifying an indicator of benzodiazepine long-term use related to occupational life rather than exploring the underlying psychological pathways that could lead to benzodiazepine inappropriate consumption.
Explanatory Hypotheses
Our results are in agreement with previous findings showing cross-sectional associations between psychotropic drug use in the past 12 months and emotional job demand in both men and women.14 However, this previous study did not discriminate among psychotropic drugs or between appropriate use and long-term use. Benzodiazepine consumption may result from an attempt to self-medicate stress and anxiety induced by a chronic exposure to emotional job demands13 thanks to the acute anxiolytic effect of benzodiazepines through GABA-mediated pathways. As benzodiazepine long-term use may lead to benzodiazepine use disorder, our findings are also in agreement with associations between stressful relationships with the public and the risk of substance use disorders.13 On the other hand, benzodiazepine long-term use could increase the likelihood of interpersonal difficulties. Indeed, they have short-term effects (e.g., disinhibition, impulsivity, attention disorders) and long-term effects (e.g., anxiety, depressive mood, dependence symptoms, neurocognitive impairment) that could have an impact on the likelihood of dissatisfaction of the public, triggering interpersonal difficulties.
We found greater size effects in men. First, gender differences may be explained by different public encountered by men and women. Indeed, women more often occupy jobs that imply high emotional demand, such as caregiving or social work. Moreover, adjustment for proxies of socioeconomic position does not totally rule out differences in work-related stress exposure according to gender22 such as lower income or more precarious jobs in women. One could hypothesize that women have developed better abilities than men to cope with emotional job demand, such as relational skills to defuse potential interpersonal conflicts. Second, women may be more prone than men to encounter stressors outside occupational life, especially family life and work–family conflicts, so that stress exposure at the workplace may be less central regarding the risk of benzodiazepine long-term use.31 Third, because women have higher levels of consumption than men when they use benzodiazepines,30 they might have an increased likelihood of side effects.2,4 Moreover, women may be more sensitive to emotional demand than men16 while they might be exposed to highest levels of emotional demand in the workplace.22 All these reasons could lead the most vulnerable women to be more frequently excluded from public exposure in the workplace.
Clinical Relevance and Future Research
With regard to screening, stressful job exposure to the public may ease early diagnosis of benzodiazepine long-term use by using existing validated tools to search for benzodiazepine inappropriate consumption and, if applicable, benzodiazepine use disorder.32 With regard to prevention, interventions exist to maintain an appropriate consumption or to provide a successful weaning, such as standardized advice and a scheduled tapering program including cognitive and behavioral therapy.32
Future research should provide a better understanding of the underlying pathways involved in the association between stressful exposure to the public and benzodiazepine long-term use. In particular, future studies with prospective designs should explore the directions of this association. Then, regarding prevention, psychological interventions to reduce the impact or the exposure to emotional job demands could be tested as a way to prevent benzodiazepine long-term use. For instance, strategies aiming at developing emotional skills or at reducing emotional dissonance at work may be particularly helpful.33 Other strategies such as mindfulness-based interventions, already used to improve emotion regulation, might also be proposed in the workplace.34 Employers should also promote an effective workplace stress policy in their companies—for example, through organizational changes aimed at reducing exposure to stressors in the workplace.35 Given the high prevalence of both job positions with exposure to the public and benzodiazepine long-term use, these interventions may have important public health implications. Finally, other settings of benzodiazepine inappropriate consumption such as over-the-counter consumption should be explored to extend our findings to these patterns of inappropriate consumption.
ACKNOWLEDGMENTS
CONSTANCES is accredited as a “National Infrastructure for Biology and Health” by the governmental Investissements d’avenir program and was funded by the Agence nationale de la recherche (ANR-11-INBS-0002 grant). The CONSTANCES cohort is supported by the National Health Insurance Fund (Caisse nationale d’assurance maladie des travailleurs salaries; CNAMTS). CONSTANCES also receives funding from MSD, AstraZeneca, and Lundbeck managed by INSERM-Transfert. This study has received funding from the Interministerial Mission for Combating Drugs and Addictive Behaviors (Mission Interministérielle de Lutte contre les Drogues et les Conduites Addictives).
The authors wish to thank the CNAMTS and its Health Screening Centres (Centres d’examens de santé), responsible for collecting a large part of the data.
CONFLICTS OF INTEREST
G. Airagnes has received speaker and consulting fees from Lundbeck and Pfizer. C. Lemogne has received speaker and consulting fees from Daiichi-Sankyo, Janssen, Lundbeck, Otsuka Pharmaceuticals, and Servier. F. Limosin has received speaker and consulting fees from Astra Zeneca, Euthérapie-Servier, Janssen, Lundbeck, Otsuka Pharmaceuticals, and Roche. R. Olekhnovitch, M. Goldberg, N. Hoertel, Y. Roquelaure, and M. Zins have nothing to declare.
HUMAN PARTICIPANT PROTECTION
The CONSTANCES cohort was approved by the institutional review board of the National Institute for Medical Research – INSERM (no. 01-011). Informed consent was received from all of the participants.
Footnotes
See also Siegrist, p. 18.
REFERENCES
- 1.Airagnes G, Pelissolo A, Lavallee M, Flament M, Limosin F. Benzodiazepine misuse in the elderly: risk factors, consequences, and management. Curr Psychiatry Rep. 2016;18(10):89. doi: 10.1007/s11920-016-0727-9. [DOI] [PubMed] [Google Scholar]
- 2.Ait-Daoud N, Blevins D, Khanna S, Sharma S, Holstege CP. Women and addiction. Psychiatr Clin North Am. 2017;40(2):285–297. doi: 10.1016/j.psc.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Panes A, Lassalle R, Bernard M-A, Dureaud-Pournin C, Pariente A, Fourrier-Réglat A. Misuse of benzodiazepines in the French population: a cohort study in the Échantillon Genéraliste de Bénéficiaires between 2007 and 2012. Rev Epidemiol Sante Publique. 2016;64:S132–S133. [Google Scholar]
- 4.Nordfjærn T. A population-based cohort study of anxiety, depression, sleep and alcohol outcomes among benzodiazepine and z-hypnotic users. Addict Behav. 2012;37(10):1151–1157. doi: 10.1016/j.addbeh.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 5.Ten Wolde GB, Dijkstra A, Van Empelen P, Knuistingh Neven A, Zitman FG. Psychological determinants of the intention to educate patients about benzodiazepines. Pharm World Sci. 2008;30(4):336–342. doi: 10.1007/s11096-007-9183-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glintborg B, Olsen L, Poulsen H, Linnet K, Dalhoff K. Reliability of self-reported use of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone, and opiates among acutely hospitalized elderly medical patients. Clin Toxicol (Phila). 2008;46(3):239–242. doi: 10.1080/15563650701586397. [DOI] [PubMed] [Google Scholar]
- 7.Fride Tvete I, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. 2015;33(4):252–259. doi: 10.3109/02813432.2015.1117282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lugoboni F, Mirijello A, Faccini M et al. Quality of life in a cohort of high-dose benzodiazepine dependent patients. Drug Alcohol Depend. 2014;142:105–109. doi: 10.1016/j.drugalcdep.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 9.Morel A, Grall-Bronnec M, Bulteau S et al. Benzodiazepine dependence in subjects with alcohol use disorders: what prevalence? Expert Opin Drug Saf. 2016;15(10):1313–1319. doi: 10.1080/14740338.2016.1221922. [DOI] [PubMed] [Google Scholar]
- 10.Niedhammer I, David S, Degioanni S, Drummond A, Philip P. Workplace bullying and psychotropic drug use: the mediating role of physical and mental health status. Ann Occup Hyg. 2011;55(2):152–163. doi: 10.1093/annhyg/meq086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rugulies R, Aust B, Madsen IE. Effort–reward imbalance at work and risk of depressive disorders. A systematic review and meta-analysis of prospective cohort studies. Scand J Work Environ Health. 2017;43(4):294–306. doi: 10.5271/sjweh.3632. [DOI] [PubMed] [Google Scholar]
- 12.Heikkilä K, Nyberg ST, Fransson EI et al. Job strain and alcohol intake: a collaborative meta-analysis of individual-participant data from 140,000 men and women. PLoS One. 2012;7(7):e40101. doi: 10.1371/journal.pone.0040101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sinha R. The role of stress in addiction relapse. Curr Psychiatry Rep. 2007;9(5):388–395. doi: 10.1007/s11920-007-0050-6. [DOI] [PubMed] [Google Scholar]
- 14.Lassalle M, Chastang J-F, Niedhammer I. Working conditions and psychotropic drug use: cross-sectional and prospective results from the French national SIP study. J Psychiatr Res. 2015;63:50–57. doi: 10.1016/j.jpsychires.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 15.Pelfrene E, Vlerick P, Moreau M, Mak RP, Kornitzer M, De Backer G. Use of benzodiazepine drugs and perceived job stress in a cohort of working men and women in Belgium. Results from the BELSTRESS-study. Soc Sci Med. 2004;59(2):433–442. doi: 10.1016/j.socscimed.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Rivera-Torres P, Araque-Padilla RA, Montero-Simó MJ. Job stress across gender: the importance of emotional and intellectual demands and social support in women. Int J Environ Res Public Health. 2013;10(1):375–389. doi: 10.3390/ijerph10010375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Airagnes G, Lemogne C, Goldberg M et al. Job exposure to the public in relation with alcohol, tobacco and cannabis use: findings from the CONSTANCES cohort study. PLoS One. 2018;13(5):e0196330. doi: 10.1371/journal.pone.0196330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kinman G, Wray S, Strange C. Emotional labour, burnout and job satisfaction in UK teachers: the role of workplace social support. Educ Psychol. 2011;31(7):843–856. [Google Scholar]
- 19.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 20.Wiegel C, Sattler S, Göritz AS, Diewald M. Work-related stress and cognitive enhancement among university teachers. Anxiety Stress Coping. 2016;29(1):100–117. doi: 10.1080/10615806.2015.1025764. [DOI] [PubMed] [Google Scholar]
- 21.Goldberg M, Carton M, Descatha A et al. CONSTANCES: a general prospective population-based cohort for occupational and environmental epidemiology: cohort profile. Occup Environ Med. 2017;74(1):66–71. doi: 10.1136/oemed-2016-103678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hooftman WE, van der Beek AJ, Bongers PM, van Mechelen W. Gender differences in self-reported physical and psychosocial exposures in jobs with both female and male workers. J Occup Environ Med. 2005;47(3):244–252. doi: 10.1097/01.jom.0000150387.14885.6b. [DOI] [PubMed] [Google Scholar]
- 23.Bezin J, Duong M, Lassalle R et al. The national healthcare system claims databases in France, SNIIRAM and EGB: powerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26(8):954–962. doi: 10.1002/pds.4233. [DOI] [PubMed] [Google Scholar]
- 24.Micallef J, Frauger E, Lapeyre-Mestre M. Misuse of benzodiazepines in France. In: Preedy VR, editor. Neuropathology of Drug Addictions and Substance Misuse. San Diego, CA: Academic Press; 2016. pp. 1101–1111. [Google Scholar]
- 25.Siegrist J, Wege N, Puhlhofer F, Wahrendorf M. A short generic measure of work stress in the era of globalization: effort–reward imbalance. Int Arch Occup Environ Health. 2009;82(8):1005–1013. doi: 10.1007/s00420-008-0384-3. [DOI] [PubMed] [Google Scholar]
- 26.Morin AJ, Moullec G, Maiano C, Layet L, Just JL, Ninot G. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in French clinical and nonclinical adults. Rev Epidemiol Sante Publique. 2011;59(5):327–340. doi: 10.1016/j.respe.2011.03.061. [DOI] [PubMed] [Google Scholar]
- 27.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. 2nd ed. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 28.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haukoos JS, Newgard CD. Advanced statistics: missing data in clinical research—part 1: an introduction and conceptual framework. Acad Emerg Med. 2007;14(7):662–668. doi: 10.1197/j.aem.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 30.Holm E, Fosbol E, Pedersen H et al. Benzodiazepine use in Denmark 1997–2008. Eur Geriatr Med. 2012;3(5):299–303. [Google Scholar]
- 31.Frone MR, Barnes GM, Farrell MP. Relationship of work–family conflict to substance use among employed mothers: the role of negative affect. J Marriage Fam. 1994;56(4):1019–1030. [Google Scholar]
- 32.Soyka M. Treatment of benzodiazepine dependence. N Engl J Med. 2017;376(12):1147–1157. doi: 10.1056/NEJMra1611832. [DOI] [PubMed] [Google Scholar]
- 33.Diefendorff JM, Gosserand RH. Understanding the emotional labor process: a control theory perspective. J Organ Behav. 2003;24(8):945–959. [Google Scholar]
- 34.Hülsheger UR, Alberts HJ, Feinholdt A, Lang JW. Benefits of mindfulness at work: the role of mindfulness in emotion regulation, emotional exhaustion, and job satisfaction. J Appl Psychol. 2013;98(2):310–325. doi: 10.1037/a0031313. [DOI] [PubMed] [Google Scholar]
- 35.O’Keefe LC, Brown KC, Christian BJ. Policy perspectives on occupational stress. Workplace Health Saf. 2014;62(10):432–438, quiz 439. doi: 10.3928/21650799-20140813-02. [DOI] [PubMed] [Google Scholar]