Abstract
War’s burden on the health and well-being of combatants, civilians, and societies is well documented. Although the examination of soldiers’ injuries in modern combat is both detailed and comprehensive, less is known about war-related injuries to civilians and refugees, including victims of torture. The societal burden of war-related disabilities persists for decades in war’s aftermath. The complex injuries of combat survivors, including multiple pain conditions and neuropsychiatric comorbidities, challenge health care systems to reorganize care to meet these survivors’ special needs.
We use the case study method to illustrate the change in pain management strategies for injured combat survivors in one national health system, the US Department of Veterans Affairs (VA). The care of veterans’ disabling injuries suffered in Vietnam contrasts with the care resulting from the VA’s congressional mandate to design and implement a pain management policy that provides effective pain management to veterans injured in the recent Middle East conflicts.
The outcomes-driven, patient-centric Stepped Care Model of biopsychosocial pain management requires system-wide patient education, clinician training, social networking, and administrative monitoring. Societies are encouraged to develop their health care system’s capacity to effectively respond to the victims of warfare, including combatants and refugees.
Three intersecting sociocultural phenomena elevate chronic pain to global consciousness. First, war causes physical and psychosocial pain for both warriors and civilians, and social burdens for the communities they reenter.1,2 Second, chronic pain is the leading cause of disability in industrialized and most emerging economies across the globe. Even where depression (India) or HIV (South Africa) is accorded “most disabling” status, both conditions are highly associated with chronic pain.3 Third, in some Western countries, chronic noncancer pain drives a rise of disability, substance use disorders, opioid overdose, suicide rates, and health care costs; at the same time, in much of the world there is a lack of access to basic pain care, including opioids and other analgesics, even for terminal cancer.
In this commentary, we review the socioeconomic burden of war and the rates of different injuries incurred in modern warfare. We then examine challenges faced by injured combatants returning home through the lens of an injured Vietnam veteran. Finally, we discuss how the US Department of Veterans Affairs (VA) and the Department of Defense (DoD) have together systematically addressed the challenges faced by the large cohort of severely injured combatants returning home from conflicts in the Middle East.
The physical and psychological injuries of combat survivors are well documented,4,5 unlike those of civilian survivors of accidental combat exposure or of purposeful bombing or chemical gas attacks. Many suffer chronic pain, often with comorbidities. Victims of war-related torture and sexual violence and families and communities displaced by war-forced migrations also suffer.6 War’s land mines and unexploded munitions remain public health hazards for decades.7 Less well documented are war’s persistent psychological and sociocultural consequences, such as reactive xenophobia—sometimes violent—toward refugees2,8 and war’s moral injuries. The interaction of pain and emotions is well established in the neuroscience pain literature.9 Violence causes painful physical and psychological injuries; when pain persists, and is encoded in the central nervous system with the remnants of war’s psychological trauma—such as posttraumatic stress and the more clinically impactful posttraumatic stress disorder (PTSD)—a reciprocal relationship occurs: stress and PTSD generally activate and worsen the severity of pain in painful conditions and pain usually activates stress and may trigger PTSD symptoms.10 Clinicians struggle to help patients “detoxify” from distressing memories and detach the pain and stress experiences.
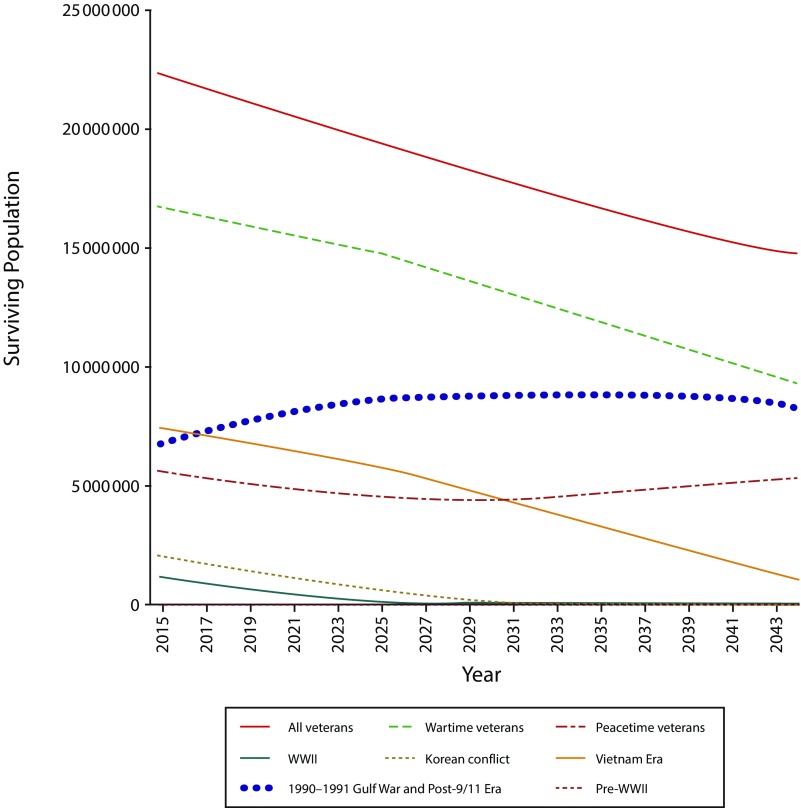
A measure of the socioeconomic burden of diseases and medical conditions associated with war, “years lived with disability,” declined globally between 1990 and 2013 through deaths in the large World War II cohort. However, war ranks highly as a cause of years lived with disability in nations involved in late–20th-century conflicts—for example, it ranks first in Cambodia, Nicaragua, and Rwanda and second in Vietnam.3 Countries in the Middle East and other war-torn regions can anticipate that future war-related years lived with disability will rise. Data gathered on injured military from Operation Iraqi Freedom and Operation Enduring Freedom (OIF–OEF) reveal the potential for war-related years lived with disability to persist in the United States (Figure 1).11 The US budgetary cost for recent conflicts in Afghanistan, Iraq, and Pakistan is projected to be $5632 billion (in 2017 dollars) through 2056, with an estimated 370 000 lives lost directly related to military operations and another estimated 800 000 civilian deaths indirectly.11
FIGURE 1—
Estimated Surviving Population of War Veterans From Different US War Eras: 2014–2043
Source. Hunt SC, Hoge CW. Health care for military veterans. In: Jameson JL, Fauci AS, Kasper DL, et al., eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw-Hill; 2018. Reprinted with permission.
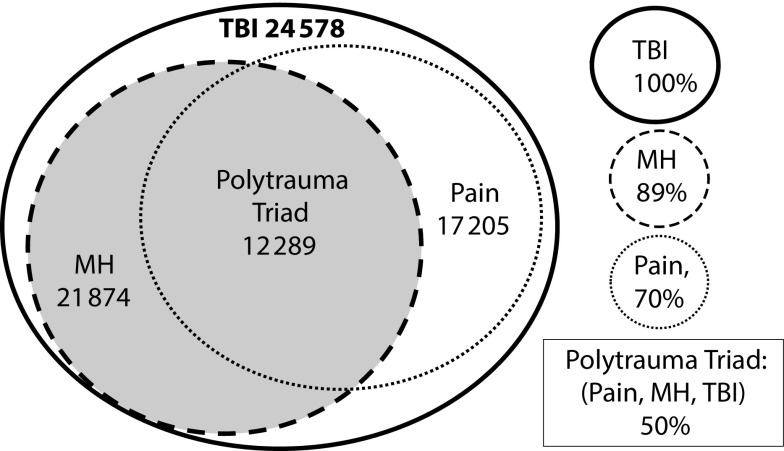
Early in OIF–OEF, it became apparent that advanced battlefield trauma medicine enabled survival of over 90% of wounded American combatants, compared with 76% survival in Vietnam.12 Of 771 874 veterans from OIF–OEF and Operation New Dawn who used VA services from 2002 through 2012, 52.3% suffered mental disorder, 44.3% a neurological condition (including traumatic brain injury and pain from nerve injury), and 56.3% musculoskeletal pain.4 In a sample of survivors with traumatic brain injury (6.7% of those injured), 89% suffered mental disorders, 70% head or spinal pain, and over half both pain and mental conditions, most commonly PTSD,13 representing far higher rates than in the general population. When combined, they create the signature injury of OIF–OEF, blast-related “polytrauma triad” (Figure 2). These troops returned home with severe, complex conditions requiring expanded competency in multimodel rehabilitative care to restore a meaningful quality of civilian life.1
FIGURE 2—
Numbers and Rates of Mental Health (MH) and Pain (Pain) Conditions in 24 578 Operation Iraqi Freedom–Operation Enduring Freedom Veterans With Traumatic Brain Injury (TBI) in the US Department of Veterans Affairs: 2009
Source. Taylor et al.13
When war-related injury occurs, what are the social consequences? Does war trauma socially embed within a culture by epigenetic parent–child transmission or by social constructs—for example, dictatorships that further traumatize a subjected population? Besides remnants of war injury such as PTSD and pain, does the desire for retribution maintain the cycle of violence? How do societies and health systems respond to lessen suffering and costs?
Our clinical organizations and communities must change policies and procedures to meet the needs of a traumatized population. We examine this challenge through the lens of two studies: first, a case study of a 60-year-old veteran injured in Vietnam with residual PTSD and pain; second, a review of how a health system with relatively limited resources, the VA, manages the personal, social, and community needs of a population of wounded warriors with pain struggling to reintegrate into families and society.
Vietnam Case Study
Joe returns from Vietnam combat having suffered a severe upper arm and shoulder wound while pulling wounded soldiers to safety and watching others die; from his own rescue craft, he watches a helicopter with wounded buddies ditch in the sea, all hands lost. For years, he’s suffered from PTSD as well as complex regional pain syndrome type II (CRPS II, or causalgia), a residual of the nerve injury to his arm, such that the slightest touch is exquisitely painful. He cannot return to his electrician’s job, so he teaches teenagers to be electricians. To honor fallen comrades, he requires students to cite the Pledge of Allegiance to the Flag, but culturally diverse kids chatter. Angry at the disrespect, he expels the students, angering both their parents and his supervisors. The resulting stress activates CRPS pain and disables him from the classroom. His pain and PTSD symptoms worsen, preventing sleep; at night he reads war novels and watches war films on TV.
After 30 years, a new multidisciplinary pain team manages neuropathic and emotional pain successfully with trials of various antidepressants, anticonvulsants, and low-dose methadone as he learns to implement pain-coping skills and avoid activating pain using cognitive-behavioral strategies. Prazosin for PTSD nightmares and sleep hygiene improve sleep. He and his wife behaviorally contract to avoid PTSD-activating war movies. He eventually retires but maintains daily structure as a volunteer handyman for his wife’s family business, pacing himself to avoiding pain-activating labor. Together, they seek survivors from his army company and national reunions where stories are shared and lost comrades honored. The dominance of PTSD and pain recede, and he gradually resumes hobbies following family “rules” about avoiding activities that provoke CRPS or PTSD. He no longer uses regular analgesics. (Details of this case have been altered to protect personal identity.)
Joe suffered for many years with conditions that the health care system had difficulty understanding and treating. Vietnam veterans often returned home stigmatized, socially isolated, and exposed to protests, anger, and misunderstanding.14 One veteran recalls trying to bus home from a town near his army base. The driver reviled him as a “killer,” not allowing him on the bus, while other passengers stared with obvious disdain.
The trauma and tragedy of veterans’ Vietnam War experience and transition home is well documented by Jonathan Shay’s 1994 Achilles in Vietnam: Combat Trauma and the Undoing of Character14 and by war films such as Platoon, Apocalypse Now, Coming Home, The Deer Hunter, Casualties of War, and, most thoroughly, a recent documentary, The Vietnam War: A Film by Ken Burns and Lynn Novick. Although pain is not directly addressed in these films, the pain of injuries portrayed is an unspoken subtext. During the Vietnam War, little was known about treating chronic pain, PTSD, or postconcussive syndrome. Pain clinics were unknown, as were mechanism-based pain treatments now commonly used (e.g., anticonvulsants, antidepressants, and cognitive-behavioral therapy). Surgery of the spine, the most common pain site, was generally ineffective, often leading to “failed back surgery syndrome.”15 Some veterans coped with drugs; others immersed themselves in jobs that moderated pain through distraction. PTSD sometimes emerges in clinical settings when veterans from older wars retire from work, which has sustained them for decades; for example, 2013 data show that 62 536 new cases of PTSD were diagnosed in VA patients from these cohorts.5
The Stepped Care Model for Pain
Has our society’s response to pain and its clinical epiphenomena in veterans changed since Vietnam? Our national health care system, beset with rising costs and inefficiency, fails to achieve the desired population-based health care outcomes and has little capacity to change the dynamics that perpetuate fragmented, generally ineffective pain management.1 However, the evolution of social values and clinical science has greatly improved the military’s and veterans’ chances in the VA. Veterans, now publicly respected and acclaimed, are generally welcomed by communities. However, at war’s outbreak in 2003, trained clinical teams were generally not available to manage both the growing cohort of newly injured veterans and existing cohorts from prior wars. Nor were there systems to coordinate smooth care transitions from military to VA care.1 Moreover, despite advocacy for pain training,16 academic medicine did not improve clinicians’ competency.17 Fortunately, the voices of injured veterans and their families were heard. One soldier powerfully wrote and lectured widely about his recovery from the pain of a traumatic leg amputation and severe concussion:
It’s now four years since I lay in the dirt, near death, on the side of the road in Fallujah. I’m grateful for all I have, and proud of the things I’ve accomplished. In the end though, I don’t measure how far I’ve come by goals achieved, or academic degrees earned, or running trophies won. For me, what counts is that pain no longer rules my life.18(p40)
Congress responded. The VA Pain Care Act (2008) and Military Pain Care Act (2008) required that these health systems improve pain care and train clinicians appropriately.1 The Stepped Care Model became policy for both systems through the VA’s 2009 Pain Management Directive and the DoD’s Pain Management Task Force Report.1 The Stepped Care Model calls for (1) a foundation of self-care and self-management and of patient, family, and caregiver education; (2) a well-trained primary care workforce for managing the common pain conditions with access to multimodal therapy options; and (3) ready access to specialty care, including interdisciplinary pain management teams at all facilities to support primary care teams in a collaborative fashion, with the involvement of specialty providers that matches the need of the patient regarding pain severity, intractability, and complexity. Recognizing that good outcomes require good pain management from the moment of injury to recovery, the Health Executive Council of the Undersecretaries for Health of the VA and DoD established the Pain Management Work Group (HEC-PMWG) to address system-wide implementation of these policies.1
Federal medicine’s advantages over other health systems in transforming pain care include access to a complete patient sample in its administrative database for measuring outcomes in quality improvement projects and clinical trials, no requirement for profitability, and a connected workforce self-selected to be mission focused, enabling coordinated program changes system-wide.1 Moreover, all eligible veterans are served; by law, there can be no patient exclusion based on clinical or personal profile or ability to pay—outcome measurements are population based. Small, highly motivated working groups, supported by the National Pain Program, coordinated regional planning across the system to improve care.1 To build awareness of the most salient clinical issues, national conferences on managing war injuries were held with clinical tracks on pain, PTSD, and traumatic brain injury. In every VA regional network, pain management work groups initiated programmatic changes to improve care supported by monthly interactive call-in conferences to report progress.
The VA, an early adopter of academic detailing strategies to improve pain care and reduce opioid overuse through the Opioid Safety Initiative, successfully reduces risky practices by combining systematic monitoring of prescribing and direct-to-clinician feedback, support, and education.1,19 To address deficits in pain management training, the DoD’s ECHO and the VA’s SCAN-ECHO, modeled after residency training, host weekly live video conferences combining brief lectures and clinical case supervision to train geographically dispersed primary care providers in the management of common pain conditions; these conferences also reinforce primary care—specialty team networks that promulgate collaborative care system-wide, supported by 20 interdisciplinary pain rehabilitation facilities.1,20 The Pain Mini-Residency teaches office-based pain management skills, including interviewing, physical examination, myofascial injections, and battlefield acupuncture.1 The HEC-PMWG sponsors system-wide training with two projects. “Tiered Acupuncture Training Across Clinical Settings” trained 2712 providers in battlefield (auricular) acupuncture across the DoD and VHA. This training is sustained by 111 physicians trained in medical acupuncture and 113 trainers as well as by a virtual “community of practice” that merged with the VA’s Integrative Health Coordinating Center to foster integrative health and the VA’s Whole Health program.21 To provide standardized, evidence-based pain management training materials for all education venues (e.g., local and regional seminars, Mini-Residency, and ECHO), topical experts from VA–DoD and academic institutions created the Joint Pain Education Project, consisting of 30 evidence-based training modules and instructional videos now also being converted to interactive online courses to accommodate diverse learning styles of busy clinicians.22
The HEC-PMWG developed two projects to support the development of a population-based pain database that supports real-time clinical decision-making, enables population-based epidemiological and implementation research, and facilitates clinical trials. The Defense and Veterans Pain Rating Scale, validated in both military and veteran populations, provides functional anchors to its numerical scale and adds four pain interference questions about comorbidities that critically affect outcomes: activity, sleep, mood, and stress.23 The Pain Assessment Screening Tool and Outcomes Registry, a patient-reported outcomes tool, includes measures related to pain care using the National Institutes of Health’s Patient-Reported Outcome Measurement Information System and the Defense and Veterans Pain Rating Scale.
VA and DoD pain leadership participate in important projects affecting national health care, such as the Comprehensive Addiction Recovery Act, which recognizes that ineffective management of pain precedes opioid overuse and calls for better education and training of interdisciplinary clinical pain teams. The US Department of Health and Human Services (HHS) National Pain Strategy cites the Stepped Care Model while outlining a roadmap toward achieving a system of care in which all people receive appropriate, high-quality, and evidence-based care for pain.24 An HHS Pain Management Best Practices Task Force is now funded to guide national efforts.
A Model of Pain Care for Torture Victims
The VA serves as only one model of many around the world that are grappling with the tragedy of war and the moral imperative to restore the health and well-being of its victims. Unfortunately, the barriers to treatment persist even in developed countries. Some with large numbers of refugees have adopted sociomedical responses to the special needs of war and torture victims. As just one example, in London, a “one stop shop” multidisciplinary clinic to treat pain in torture survivors was recently established by a pain specialist and clinical psychologist.25 Referrals came after the failure of several specialties sequentially consulted, instead of early treatment in an interdisciplinary biopsychosocial pain management model.1 These clinicians also note that patients are never asked about torture. The clinic includes a pain management program conducted in Arabic. Attendance is good despite the stigma associated with “psych” professionals in the survivors’ country of origin. Such culturally sensitive approaches to pain treatment in war survivors need to be replicated worldwide.
This review of one health system’s effort to improve the success of war-related pain care provides some key principles that may help guide other health systems struggling to adapt to meet the needs of war-related trauma and injury:
Both injured refugees adjusting to a new country and those returning to their communities after combat deserve the best clinical teams armed with good training and the heightened moral imperative of the health professions.
The scope of war-related physical and psychological injuries, related disability, and costs must be documented by both reliable data and personal testimony.
This documentation will help generate the high level of societal support needed to ensure that health systems are adequately resourced and staffed to meet the clinical challenge of war-related clinical cohorts.
Health system requirements include wide availability of interdisciplinary teams that combine biopsychosocial clinical competencies in medical and psychological diagnosis and illness formulation. These teams must develop a full awareness of victims’ sociocultural backgrounds and war-related experiences and of how fear of stigma and social anomie contribute to pain and suffering.
Health systems must continuously strive to develop data-gathering approaches that enable documentation of clinical outcomes and system performance.
Nothing less is acceptable.
ACKNOWLEDGMENTS
We are grateful for helpful suggestions from Steven Hunt, MD, MPH, of the Department of Veterans Affairs, and Chester (Trip) Buckenmaier, MD, of the Uniform Services University of the Health Sciences. We also salute the many dedicated leaders, clinicians, staff, veterans, and military personnel in the Department of Veterans Affairs, the Department of Defense, and worldwide who contribute to the mission described in this commentary. Patient information has been altered to protect privacy.
Note. This commentary is not an official representation of the Department of Veterans Affairs.
CONFLICTS OF INTEREST
The authors report no conflicts of interest.
Footnotes
REFERENCES
- 1.Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357–378. doi: 10.1016/j.anclin.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Morina N, Kuenburg A, Schnyder U, Bryant RA, Nickerson A, Schick M. The association of post-traumatic and postmigration stress with pain and other somatic symptoms: an explorative analysis in traumatized refugees and asylum seekers. Pain Med. 2018;19(1):50–59. doi: 10.1093/pm/pnx005. [DOI] [PubMed] [Google Scholar]
- 3.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. J Gen Intern Med. 2012;27(9):1200–1209. doi: 10.1007/s11606-012-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Final Assessment. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 6.Stark L, Asghar K, Yu G, Bakomere T, Assazenew A, Falb K. Prevalence and associated risk factors of violence against conflict-affected adolescents: a multi-country, cross-sectional study. J Glob Health. 2017;7(1):010416. doi: 10.7189/jogh.07.010416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lasch K, Lynch NT, Rutherford K, Sherman C, Webster D. Psychological and cultural influences on pain and recovery from landmine injury. Pain Med. 2006;7(suppl 2):S213–S217. doi: 10.1111/j.1526-4637.2006.00234_7.x. [DOI] [PubMed] [Google Scholar]
- 8.Varvin S. Our relations to refugees: between compassion and dehumanization. Am J Psychoanal. 2017;77(4):359–377. doi: 10.1057/s11231-017-9119-0. [DOI] [PubMed] [Google Scholar]
- 9.Hashmi JA, Baliki MN, Huang L et al. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain. 2013;136(pt 9):2751–2768. doi: 10.1093/brain/awt211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asmundson GJG, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47(10):930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 11.Crawford NC. United States budgetary costs of post-9/11 wars through FY2018: a summary of the $5.6 trillion in costs for the US wars in Iraq, Syria, Afghanistan and Pakistan, and post-9/11 Veterans Care and Homeland Security. Watson Institute for International and Public Affairs. 2018. Available at: https://watson.brown.edu/costsofwar/papers/2017/USBudgetaryCostsFY2018. Accessed April 29, 2018.
- 12.Gawande A. Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med. 2004;351(24):2471–2475. doi: 10.1056/NEJMp048317. [DOI] [PubMed] [Google Scholar]
- 13.Taylor BC, Hagel EM, Carlson KF et al. Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq War Veteran VA users. Med Care. 2012;50(4):342–346. doi: 10.1097/MLR.0b013e318245a558. [DOI] [PubMed] [Google Scholar]
- 14.Shay J. Achilles in Vietnam: Combat Trauma and the Undoing of Character. New York, NY: Scribner; 1994. [Google Scholar]
- 15.Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979–987. doi: 10.2147/JPR.S92776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubois M, Gallagher RM, Lippe P. Pain medicine position paper. Pain Med. 2009;10(6):972–1000. doi: 10.1111/j.1526-4637.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- 17.Fishman SM, Carr DB, Hogans B et al. Scope and nature of pain- and analgesia-related content of the United States Medical Licensing Examination (USMLE) Pain Med. 2018;19(3):449–459. doi: 10.1093/pm/pnx336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGinnis D. Exit Wounds: A Survival Guide to Pain Management for Returning Veterans and Their Families. Washington, DC: Waterford Life Sciences; 2009. [Google Scholar]
- 19.Lin LA, Bohnert ASB, Kerns RD, Clay MA, Ganoczy D, Ilgen MA. Impact of the Opioid Safety Initiative on opioid-related prescribing in veterans. Pain. 2017;158(5):833–839. doi: 10.1097/j.pain.0000000000000837. [DOI] [PubMed] [Google Scholar]
- 20.Frank JW, Carey EP, Fagan KM et al. Evaluation of a telementoring intervention for pain management in the Veterans Health Administration. Pain Med. 2015;16(6):1090–1100. doi: 10.1111/pme.12715. [DOI] [PubMed] [Google Scholar]
- 21.Niemtzow R, Baxter J, Gallagher RM et al. Building capacity for complementary and integrative medicine through a large, cross-agency, acupuncture training program: lessons learned from a Military Health System and Veterans Health Administration Joint Initiative Project. Mil Med. 2018 doi: 10.1093/milmed/usy028. Epub ahead of print March 26, 2018. [DOI] [PubMed] [Google Scholar]
- 22. Pain Management Work Group, Health Executive Committee, Department of Defense and Department of Veterans Affairs. Joint Pain Education and Training Project (JPEP). Available at: http://www.dvcipm.org/clinical-resources/joint-pain-education-project-jpep. Accessed April 3, 2018.
- 23.Polomano RC, Galloway KT, Kent ML et al. Psychometric testing of the Defense and Veterans Pain Rating Scale (DVPRS): a new pain scale for military population. Pain Med. 2016;17(8):1505–1519. doi: 10.1093/pm/pnw105. [DOI] [PubMed] [Google Scholar]
- 24.Interagency Pain Research Coordinating Committee. The National Pain Strategy: a comprehensive population health level strategy for pain. Available at: https://iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf. Accessed April 3, 2018.
- 25.Kuehler BM, Childs SR. One stop multidisciplinary pain clinic for survivors of torture. Pain Manag. 2016;6(5):415–419. doi: 10.2217/pmt-2016-0029. [DOI] [PubMed] [Google Scholar]