Abstract
We describe a case of a 15-year-old girl who presented to our clinic with long-standing right-sided rhinorrhoea which was occasionally foul-smelling and blood-stained with no other symptom of note. She had been treated many times with antibiotics. On examination, a rhinolith was discovered impacted posteriorly in right nasal cavity with mucopurulent discharge. Plain X-ray and later CT scan of paranasal sinuses confirmed the diagnosis but it was found to be large in size with irregular shape like a ‘staghorn’. It was removed under general anaesthesia and she recovered uneventfully. We also describe the review of literature.
Keywords: otolaryngology / ent; ear, nose and throat/otolaryngology
Background
Rhinolith is a relatively rare condition1 and is caused by gradual deposition and coating of different salts of calcium and magnesium from body fluids over an object inside the nasal cavity that could be endogenous (eg, thick mucus) or exogenous (piece of paper, seed). Since it is an insidious and slow process symptoms gradually develop over period of months and years causing persistent or recurrent nasal infections and foul-smelling and sometimes blood-stained rhinorrhoea usually unilaterally. This continues until someone discovers the rhinolith. We report this case of a 15-year-old girl who came with similar symptoms found to have a large rhinolith. Its peculiar radiological feature (visible in CT scan but not in plain film) and its large size and bizarre shape were so unusual that it warrants sharing with colleagues.
Case presentation
A 15-year-old girl presented to us with right-sided rhinorrhoea most of the times which was occasionally foul-smelling and blood-stained. There was no facial pain or headache and no other symptom of note. She did not have cognitive impairment and did not remember ever inserting anything in her nose. She had been treated with antibiotics from time to time for this condition. On examination there was mucopurulent blood-stained discharge in right nasal cavity and while suctioning revealed an irregular hard object impacted in the posterior nasal cavity (figure 1). Plain X-ray showed some haziness in right maxillary sinus and no obvious radio-opaque shadow (figure 2, left column). However, CT scan showed clearly quite a large irregularly shaped object with lots of spicules and wings and a part of it extended into the nasopharynx also. The object was radio-opaque with some areas of radiolucency (figure 2, right column).
Figure 1.

The rhinolith as seen with 0° nasendoscope.
Figure 2.
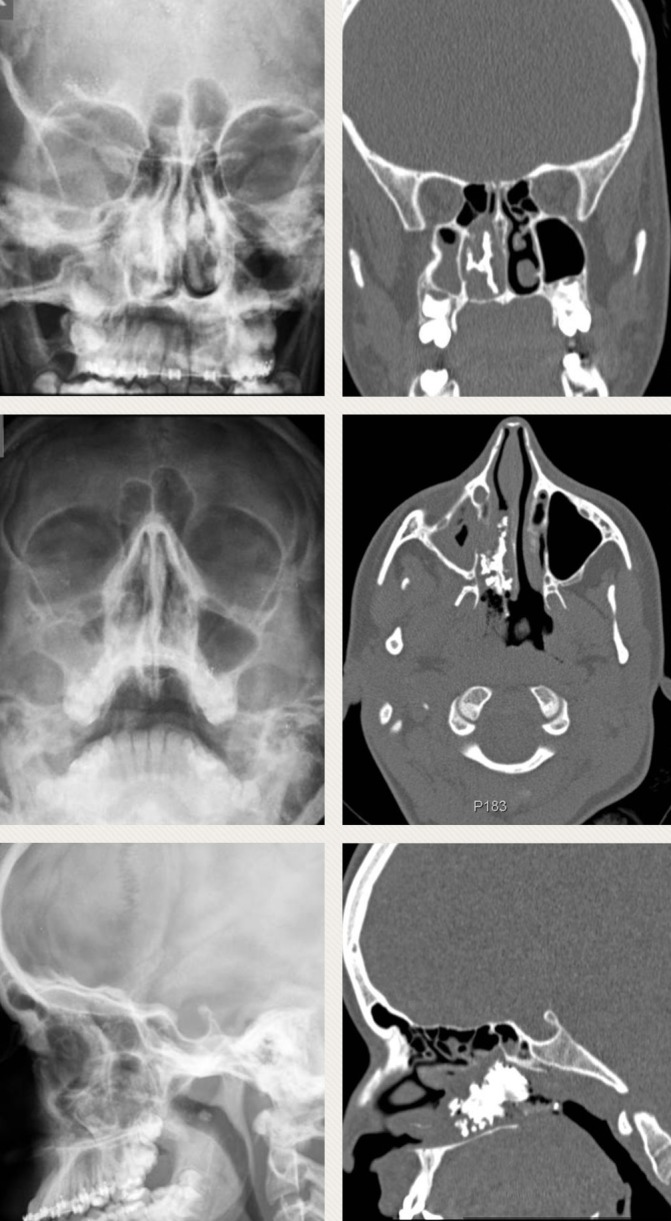
Radiology: the left column shows three views on plain X-ray sinuses and the right column shows CT images in three planes.
Investigations
Plain X-ray sinuses and CT scan were done as described earlier.
Differential diagnosis
From the clinical standpoint, an inflammatory condition like chronic sinusitis or allergic fungal sinusitis was more likely to be suspected. However, conditions like osteoma, odontoma or ossifying fibroma could also be suspected. The clinical examination and the X-ray and the CT scan ruled out inflammatory or neoplastic conditions.
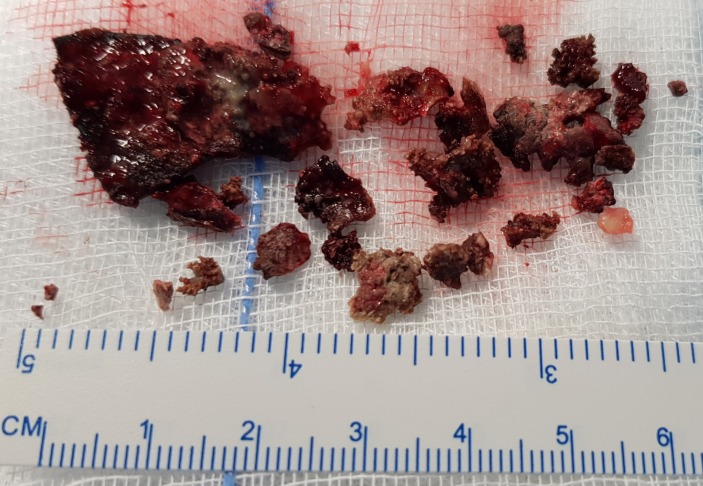
Treatment
Under general anaesthesia (GA), using the nasal endoscope, the rhinolith was removed completely piecemeal (figure 3) and right maxillary sinus was washed which came out clear and its ostium was widened. Silastic sheet was placed on right side to prevent adhesions and it was secured with silk suture to the septum. There was some ooze from the operated site but was controlled with right-sided nasal packing for 24 hours. Two of the fragments of the removed rhinolith when scraped revealed a rubbery plastic sheet that was probably the exogenous nidus she had introduced years ago as a child over which the rhinolith developed (figure 4).
Figure 3.
The removed rhinolith.
Figure 4.
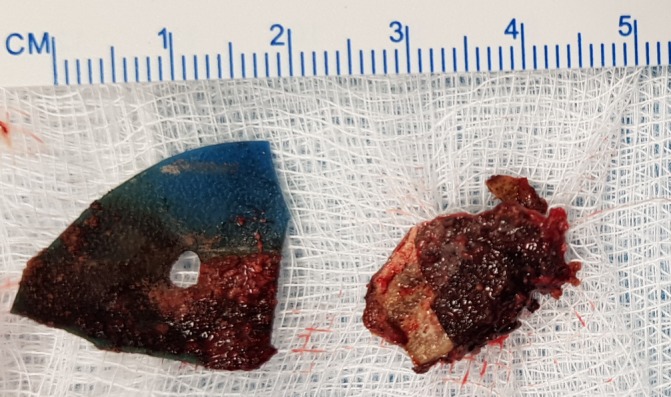
After scraping, the probable original foreign bodies were revealed which were like flexible rubber sheets.
Outcome and follow-up
She was given oral antibiotic for 5 days along with saline nasal sprays three to four times a day. The silastic sheet was removed after a week in the clinic and it was found in subsequent follow-up visit 3 weeks later that she made good recovery and her preoperative symptoms were resolved after the operation.
Discussion
Rhinolith is not very common; incidence reported as 1 in 10 000 ENT outpatients in one of the studies.1 It literally can be translated as ‘stone of the nose’.2 3 It is not a foreign body per se as it is not introduced from outside but it develops inside the nasal cavity by continuous, slow, layer-by-layer deposition of calcium and magnesium salts present in the nasal secretions over a nidus.4 This process takes years to develop.
The nidus may be endogenous or exogenous.5 Endogenous nidus means something that belongs to the body itself like thick inspissated mucus or a piece of mucus membrane or bone fragment. Exogenous nidus is always a foreign body like a piece of paper or tissue or a seed introduced into the nasal cavity. This is usually seen in small children or those who are mentally challenged.
As a result, the symptoms are slow and insidious and may consist of nasal blockade, unilateral persistent or intermittent rhinorrhoea, usually with a foul smell and occasionally blood-stained.2 Rarely, they may cause palatal perforation.4
The diagnosis of a foreign body nose can be made with this history alone but sometimes patients either do not seek medical care or are sometimes misdiagnosed and prescribed treatment on the lines of rhinosinusitis often over considerable period of time. Sometimes patients may have no nasal symptoms at all and may present with halitosis.2 Once foreign body of nose is suspected and on thorough examination of the nose, it is found to be of irregular shape and impacted surrounded by inflammation and foetid discharge, then it is more likely to be a rhinolith. These days, availability of rigid and fibre-optic nasal endoscopes can make the diagnosis really straightforward. A patient under GA for septoplasty was found to have a rhinolith behind the deviation and a nasal endoscopy in the clinic would have avoided this.1 Very rarely, the rhinolith is discovered as an incidental finding during radiological tests of skull for some other reason.2 Plain X-ray of skull usually corroborates the clinical diagnosis showing radio-opaque irregular object in the nasal cavity surrounded by haziness. However, CT scan sometimes has to be done3 5 as in our case, the rhinolith could hardly be discerned on plain radiography but clearly demonstrated in the CT scan. Moreover, 3-D reconstruction of CT image can clearly show the irregular shape of the object thus useful in planning removal. A rhinolith is usually of irregular shape but sometimes they grow quite big and their size and shape gives an appearance not unlike that of a staghorn calculus of renal pelvis. In our case, it was like that hence the name staghorn rhinolith is sometimes used.4 Although diagnosis of rhinolith is straightforward sometimes they have to be differentiated from inflammatory conditions like sinusitis and neoplastic conditions like osteoma, ossifying fibroma and odontoma and other malignancies. However, clinical and radiological examinations can easily rule them out.2
The next step is the removal and, unless it is small in size and easily accessible whereby it can be removed in the office followed by anterior nasal packing if needed, it needs to be removed under GA as its removal may require considerable manipulation with expected bleeding. Also if the patient is a small child or mentally challenged, then removal under GA is preferable. Afterwards if significant raw area is visible in both medial and lateral nasal walls, then to prevent adhesions and synechiae, it is highly recommended to place a silastic splint for a few days. Unless bleeding is very little, anterior nasal packing is usually needed for 24–48 hours. The patient usually makes full recovery afterwards with resolution of symptoms. Nowadays, while endoscopic removal is usually employed, very rarely lithotripsy and lateral rhinotomy have to be considered where endoscopic option is not available.2
Learning points.
Rhinolith is a relatively rare finding and should be suspected in cases of chronic foul-smelling rhinorrhoea with hard irregular palpable object in the nasal cavity.
Sometimes rhinolith may not manifest in plain X-ray and CT scan may be needed.
Large rhinolith requires removal under general anaesthesia and some bleeding may be expected.
Footnotes
Patient consent for publication: Next of kin consent obtained.
Contributors: The case was managed and later the manuscript was prepared and submitted by the author himself.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Vedasalam S, Sipaul F, Hill A, et al. Nasendoscopy for unusual nasal symptoms. BMJ Case Rep 2010;2010:bcr0420102911 10.1136/bcr.04.2010.2911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aziz Y, Chauhan J, Hasan SA, et al. Staghorn rhinolith in nasopharynx: an unusual case. Indian J Otolaryngol Head Neck Surg 2008;60:91–3. 10.1007/s12070-008-0029-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Singh AK, Gujar M, Shiral S, et al. Rhinolith: An unusual presentation. Indian J Otolaryngol Head Neck Surg 2004;56:297–8. 10.1007/BF02974393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shah FA, George S, Reghunanden N. A case presentation of a large rhinolith. Oman Med J 2010;25:230–1. 10.5001/omj.2010.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chatziavramidis A, Kondylidou-Sidira A, Stefanidis A, et al. Longstanding rhinolith leading to anatomical alterations of the ipsilateral inferior nasal meatus and turbinate. BMJ Case Rep 2010;2010:bcr0720103155 10.1136/bcr.07.2010.3155 [DOI] [PMC free article] [PubMed] [Google Scholar]