Abstract
Single coronary artery (SCA) is a very rare coronary anomaly. The accurate diagnosis of the entity requires multimodality imaging of the coronary anatomy. SCA is often incidentally diagnosed when patients are investigated for symptoms of suspected coronary artery disease with invasive or non-invasive coronary angiography. There are no established diagnostic electrocardiographic or echocardiographic criteria to identify the presence of SCA, which makes the diagnosis a far-reaching fruit. We present a young male patient presenting with a non-ST elevation myocardial infarction. He was found to have SCA on invasive coronary angiography, which was subsequently confirmed by CT coronary angiography.
Keywords: cardiovascular medicine, interventional cardiology
Background
The incidence of congenital absence of the left coronary system with single right coronary artery (RCA) supplying the whole heart is exceptionally rare. In clinical practice, acute coronary events can be fatal in these patients. The accurate diagnosis, appropriate treatment and patient education play vital roles in the management of these patients.
Case presentation
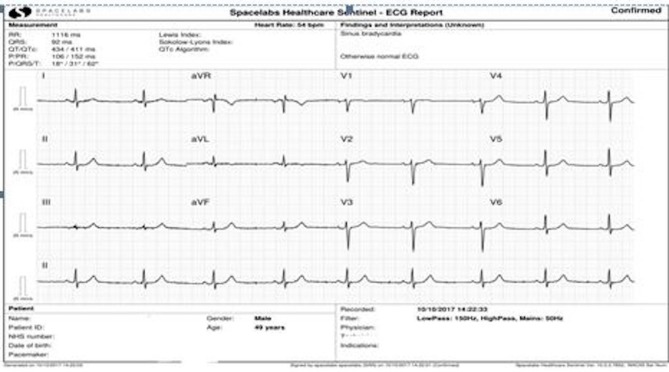
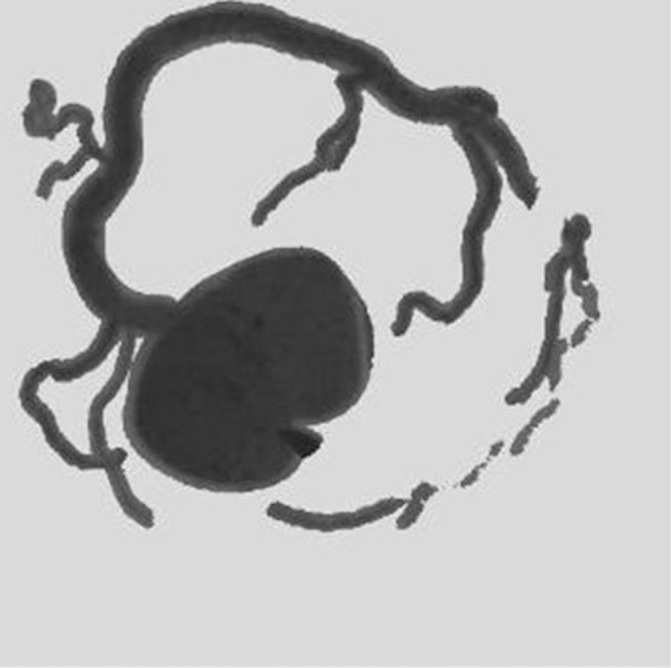
A 47-year-old male patient presented with cardiac chest pain with normal sinus rhythm ECG (figure 1). His medical history included high body mass index, hypertension and cigarette smoking. His blood pressure on admission was 125/78 mm Hg, and his heart rate was 70/min. Cardiovascular examination was normal. The high sensitivity-troponin T level was elevated, and he was treated for acute coronary syndrome (ACS) as per the National Institute for Health and Care Excellence guidelines. Invasive coronary angiography (figure 2) confirmed a large, hyperdominant RCA arising from the right coronary sinus supplying the anatomical right and the left coronary territory. There was mild plaque disease in the proximal segment of the artery without any flow limitation. Despite multiple attempts, we failed to find the left coronary ostium. The non-selective aortic root angiography (figure 3) revealed blunt left coronary sinus, and there was no evidence of aberrant left coronary artery or left coronary stump. Subsequently, the patient underwent CT coronary angiography (CTCA), which confirmed a single, gigantic and hyperdominant RCA (figures 4 and 5) arising from the right coronary sinus with branches supplying the left coronary territory. The blind left and non-coronary sinuses confirmed the absence of the left coronary system. The RCA with proximal non-flow-limiting, mild, non-calcified plaque had normal course bifurcating into posterior descending artery (PDA) and posterolateral ventricular artery (PLVA) branches. The small branch arising from the proximal RCA supplied the basal interventricular septum. The long PLVA branch itself supplied the anatomical left anterior descending (LAD) and diagonal artery territory. A small branch artery from the PLVA supplied the anatomical left circumflex artery territory along the left atrioventricular groove. The PDA supplied the base of the heart and part of the anatomical distal LAD territory of apex and apical septum.
Figure 1.
Normal sinus rhythm ECG.
Figure 2.

Invasive angiography showing large hyperdominant right coronary artery supplying both right and left coronary territories.
Figure 3.

Invasive aortic root angiography showing blunt left coronary sinus.
Figure 4.
CTCA confirming single gigantic right coronary artery arising from right coronary sinus with branches supplying to the left coronary territory.
Figure 5.
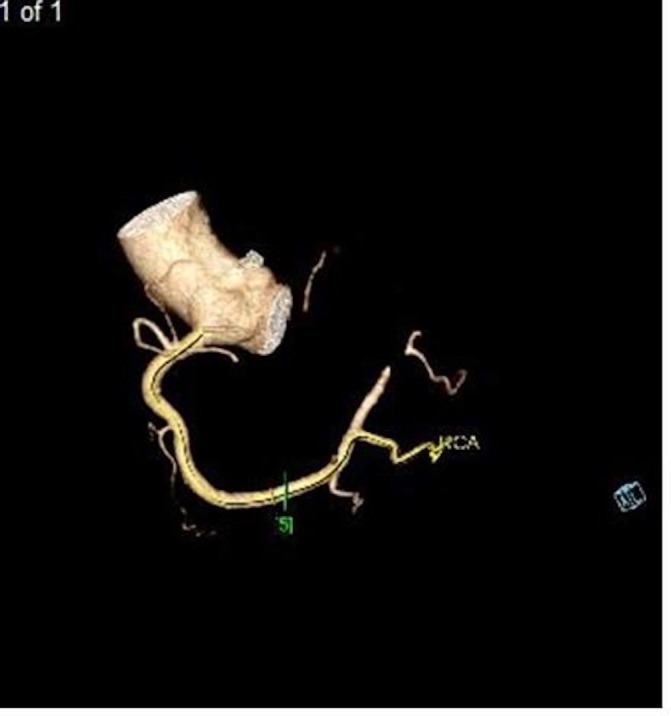
CTCA confirming single RCA with branches.
In view of the above, a diagnosis of single RCA with congenital absence of left coronary system was made. A transthoracic echocardiogram confirmed normal biventricular size and systolic function in addition to normal valvular anatomy and function.
The patient was informed of the importance of the unique diagnosis and managed according to the secondary prevention ACS treatment along with lifestyle modifications.
He regularly attends cardiac rehabilitation and remains well on follow-up. Our patient was educated about the importance of the diagnosis and risk factor modification, in addition to compliance with secondary prevention therapy.
Investigations
ECG.
High-sensitivity troponin level.
Invasive coronary angiogram.
CTCA.
Transthoracic echocardiogram.
Differential diagnosis
Chronically occluded left coronary artery system.
Treatment
Treated as per the local acute coronary syndrome protocol.
Educated about the diagnosis and the importance of lifestyle modifications for prognostic benefits.
Outcome and follow-up
Received regular cardiac rehabilitation sessions and currently under cardiology clinic follow-up on yearly basis.
Discussion
Congenital coronary anomalies like SCA are a rare find. However, the incidence of SCA with complete congenital absence of the left coronary system is extremely low at 0.024% with no gender difference.1 To date, there are very few case reports of similar cases published in the literature including three case reports of necropsy findings and three on live patients. All live cases were diagnosed accurately by CTCA. There are multiple variants of coronary anomalies with benign and malignant nature encountered in clinical practice. Lipton et al 1 proposed a classification of the coronary anomalies, which helps in better understanding of these anomalies and their management. Our case falls into the R1 variant type of Lipton’s classification. The classification of solitary coronary ostium in the aorta has been proposed by Shirani and Roberts,2 and our case fits appropriately into the type II variant of the classification.
SCA can present with multiple manifestations such as angina, syncope, myocardial infarction, malignant arrhythmia and cardiac failure.3 The risk of sudden cardiac death is higher in SCA patients.4 There have been reports of cases with other concomitant congenital cardiac anomalies particularly valvular anomalies.5 6
There is no unique clinical or diagnostic marker of SCA in a particular patient. SCA is usually diagnosed on coronary angiography as part of the investigation for coronary artery disease. However, invasive coronary angiography has diagnostic limitations due to its two-dimensional modality and other human factors. In addition, the blind sinus on invasive aortogram cannot confidently exclude the possibility of occluded left main stem at ostial level. In contrast, CTCA with its three-dimensional capability can diagnose coronary anomalies with certainty. Hence, rapid adoption of CTCA as first line of investigation tool for stable chest pain7 would help in detection of these anomalies accurately and earlier during the course of work-up of the patients.
Once diagnosed, the management of patients with SCA is again very challenging. Patients with SCA need to undergo echocardiography to exclude other concomitant congenital cardiac anomalies. In patients with significant coronary artery disease, the revascularisation strategy with coronary bypass grafting surgery if indicated would be tricky given the unidirectional blood flow with SCA.
Counselling these patients about the diagnosis and the risk reduction is quintessential for prognostic benefit. These patients need long-term surveillance to monitor for any symptoms and early treatment.
Learning points.
Single coronary artery system is a very rare congenital cardiac anomaly.
Patients with any suspicion about coronary anomaly or anatomy on invasive angiogram must undergo CT coronary angiography (CTCA) to exclude any rare anomalies.
CTCA remains the best test to detect coronary anatomy and course.
Patient education about the diagnosis and risk factors modification are very important management issues.
Footnotes
Patient consent for publication: Obtained.
Contributors: SGNU: corresponding author, involved in patient care, performed/reported coronary angiogram and CT coronary angiogram, planned and written the manuscript after literature search and case details and obtained the relevant pictures discussed with the patient regarding the publication and helped in obtaining consent. LHM: involved in discussion and writing the case report, obtained consent form the patient and contributed for writing up the manuscript. DC: consultant for the patient, currently managing the patient with follow-up, reported CTCA and helped in discussion, planning and writing up the case report. GL: parent consultant who supervised the invasive coronary angiogram, involved in planning, discussion and supervised the case report writing and contributed significantly.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Lipton MJ, Barry WH, Obrez I, et al. Isolated single coronary artery: diagnosis, angiographic classification, and clinical significance. Radiology 1979;130:39–47. 10.1148/130.1.39 [DOI] [PubMed] [Google Scholar]
- 2. Shirani J, Roberts WC. Solitary coronary ostium in the aorta in the absence of other major congenital cardiovascular anomalies. J Am Coll Cardiol 1993;21:137–43. 10.1016/0735-1097(93)90728-J [DOI] [PubMed] [Google Scholar]
- 3. Desmet W, Vanhaecke J, Vrolix M, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J 1992;13:1637–40. 10.1093/oxfordjournals.eurheartj.a060117 [DOI] [PubMed] [Google Scholar]
- 4. Taylor AJ, Rogan KM, Virmani R, et al. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol 1992;20:640–7. 10.1016/0735-1097(92)90019-J [DOI] [PubMed] [Google Scholar]
- 5. Topaz O, DeMarchena EJ, Perin E, et al. Anomalous coronary arteries: angiographic findings in 80 patients. Int J Cardiol 1992;34:129–38. 10.1016/0167-5273(92)90148-V [DOI] [PubMed] [Google Scholar]
- 6. Arinc H, Gunduz H, Tamer A, et al. Aberrant right ventricular branch of right coronary artery with mitral valve prolapse. Exp Clin Cardiol 2004;9:251–2. [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence. Chest pain of recent onset: assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin (update). Clinical guideline 95. London: NICE, 2016. [PubMed] [Google Scholar]