Description
A 67-year-old man presented with a 2-week history of worsening dysphagia and associated fevers. This was on a background of recent travel to Malaysia where he first noticed dysphagia to solids however worsening to the point of difficulty in swallowing liquids particularly over the last two days. The patient denied any odynophagia, shortness of breath or change in voice. His medical history was significant for type 2 diabetes, ischaemic heart disease, hypertension and hypercholesterolaemia. He was a current smoker (10–15 per day).
On examination, the patient’s vital observations were within normal limits. He appeared unwell however with obvious facial pallor. His voice normal and cranial nerves intact. Examination of his oral cavity and oropharynx was normal. Flexible nasoendoscopy was unremarkable apart from a subtle posterior pharyngeal wall fullness. He had normal neck range of motion. Blood tests demonstrated elevated inflammatory markers (white cell count=12×109/L, C reactive protein=98 mg/L).
Radiological investigation in the form of a CT neck and chest with contrast was arranged. This demonstrated a 19-cm-long multiseptated gas containing abscess in the pre-vertebral, retropharyngeal and retro-oesophageal spaces extending from C2 to T5 level with associated anterior displacement of the visceral space in the neck and the trachea and oesophagus in the upper thorax (figures 1–4).
Figure 1.
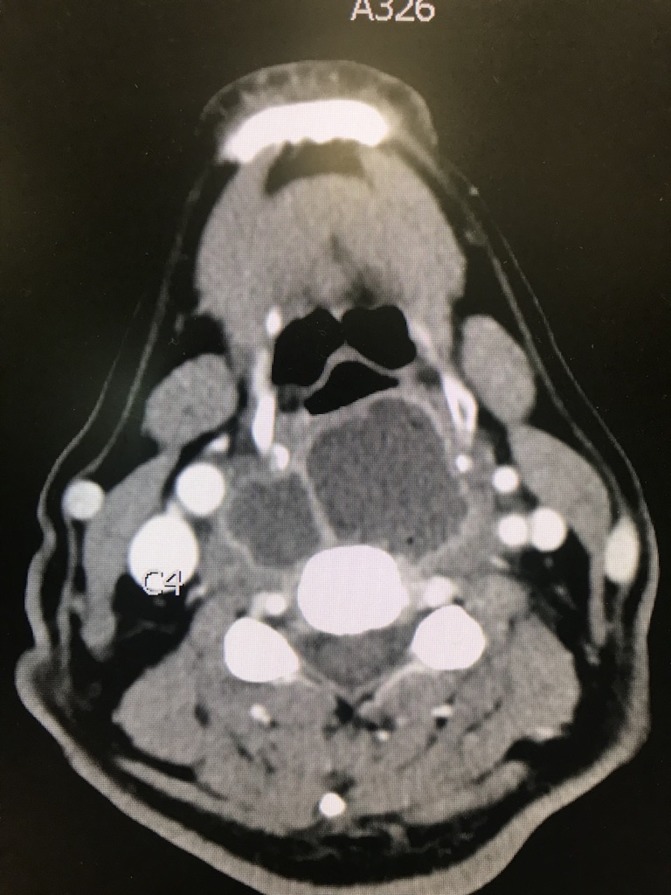
Axial CT neck with contrast indicating massive multiseptated retropharyngeal abscess at the level of C4.
Figure 2.
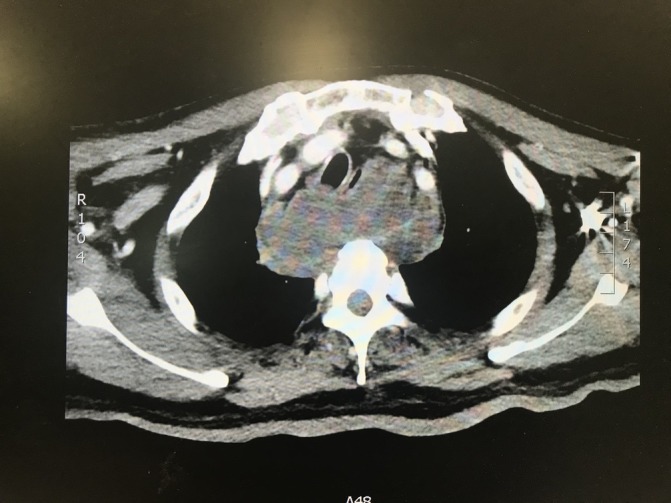
Axial CT chest with contrast indicating persistent mutliseptated retropharyngeal abscess into the mediastinum at the level of the carina.
Figure 3.

Sagittal CT neck with contrast showing the extent of the retropharyngeal abscess.
Figure 4.
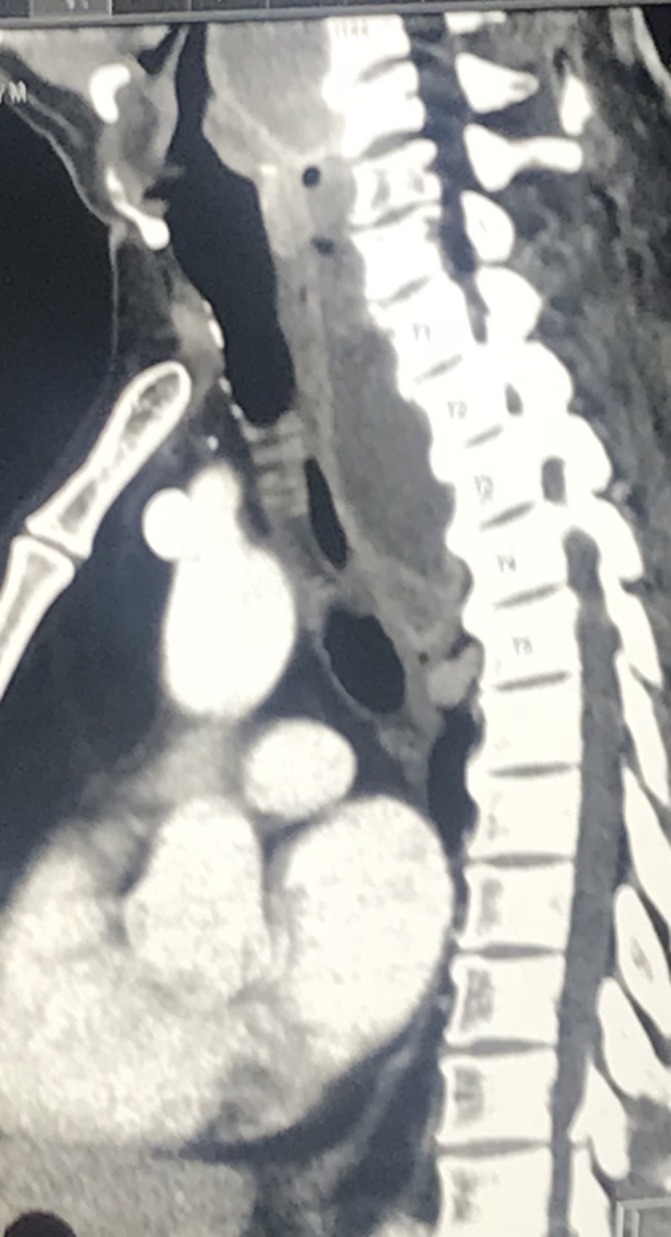
Sagittal CT chest with contrast demonstrating the extent of the retropharyngeal abscess into the posterior.
The patient was given immediate intravenous broad-spectrum antibiotics on advice from the infection’s disease doctors. He proceeded to undergo urgent transoral drainage of his retropharyngeal abscess. Intraoperatively, 400 mL of pus was drained trans-through a vertical incision over the fluctuant midline posterior pharyngeal wall swelling. Microbiology of the pus in addition to blood cultures revealed a methicillin-sensitive Staphylococcus aureus which directed treatment to intravenous flucloxacillin. Follow-up CT imaging was arranged on several occasions postoperatively (at 2 and 4 weeks) revealing significant reduction in volume of the loculated retropharyngeal/pre-vertebral abscess. He was treated with intravenous antibiotics for 6 weeks and made an excellent recovery without further accumulation of his retropharyngeal/pre-vertebral abscess.
Learning points.
The differential diagnosis of dysphagia is broad and extrinsic causes, although less common than other aetiologies, need to be excluded in the work-up of patients presenting with dysphagia.
Retropharyngeal abscesses in adults are uncommon and pose a diagnostic challenge for clinicians.
Examination is often unremarkable without clear abnormalities of the oral cavity/oropharynx or neck.
Complications of a retropharyngeal abscess can include mediastinitis and airway compromise due to mass effect.
This case highlights a rare pathology seen infrequently in adults masquerading as a common presenting complaint.
Radiological investigation of these patients without obvious clinical signs is important to exclude extrinsic aetiologies resulting in dysphagia.
Footnotes
Contributors: TH admitted the patient with assistance by MQ, and prepared the manuscript. MQ and PY were the operating surgeons involved in the case.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.


