Abstract
Difficult intubation in neonates has innumerable aetiologies. It especially poses a formidable challenge to save a newborn baby immediately after birth where antenatal details are unavailable. A late preterm neonate was born limp and apnoeic. Several attempts to intubate the baby were unsuccessful. Possibility of subglottic obstruction was considered. The baby died of severe perinatal asphyxia. Autopsy showed a mass around the airway which turned out to be ectopic thymus on histopathology. Ectopic thymus can present as periglottic mass without externally visible cervical swelling and can cause difficult intubation which may lead to serious adverse outcome including death if not anticipated early and managed accordingly.
Keywords: neonatal intensive care, congenital disorders, neonatal health
Background
Difficult intubation in neonates is not an uncommon scenario. It has diverse aetiologies as well. Subglottic mass usually presents as difficult airway requiring cricothyroidotomy as a life-saving procedure in emergency. Though subglottic haemangioma, subglottic stenosis, subglottic webs are the usual aetiologies but ectopic cervical thymus has also been reported rarely causing airway obstruction. One needs to have a strong suspicion of this condition and emergency team should be prepared to deal with such situations.
Case presentation
A baby boy with birth weight of 960 g was born to a primigravida mother at 36 weeks of gestation by emergency caesarean section in view of fetal bradycardia and severe oligohydramnios. Weight of the placenta was 270 g. Antenatal ultrasound done elsewhere at 35+4 weeks of gestational age revealed gross intrauterine growth restriction, amniotic fluid index of <1 cm, single umbilical artery, placental insufficiency, umbilical artery S/D (peak systolic/ end diastolic) ratio of 3.45 and middle cerebral artery Doppler suggestive of fetal hypoxia. Renal status was not mentioned in the report.
Baby was born limp and apnoeic with heart rate 70/min. Resuscitative measures were initiated immediately including bag and mask ventilation as per AAP (American Academy of Pediatrics) 2015 and NRP (Neonatal Resuscitation Program). Bag and mask ventilation failed as there was no increased in heart rate after doing corrective steps. Immediately endotracheal intubation was done and chest compression was initiated. Several attempts of endotracheal intubation failed with 2.5 mm endotracheal tube as it was difficult to negotiate the tube beyond glottis. Possibility of obstruction at the subglottic area was considered though there was no visible swelling appreciated on external examination in cervical region. Emergency tracheotomy was planned for this unanticipated event. But baby succumbed to death despite of all resuscitative measures. Baby was noted to have single umbilical artery and bilateral congenital talipes equinovarus deformity.
She presented to emergency room with tightness of abdomen and decreased fetal movement for 1 day. Non-stress test showed variable decelerations. Poor fetal prognosis explained and the mode of delivery discussed with the mother and her kin. A pathological autopsy was done after taking consent from parents. A team of pathologists and neonatologists performed the autopsy. Autopsy revealed that there were two nodes like structures of 5–6 mm in diameter compressing trachea at periglottic area (figures 1 and 2). Biopsy was taken from the mass which revealed ectopic thymus on histopathology (figure 3). Baby had bilateral renal agenesis with normal lung (weight of the lung was appropriate for gestational age). In addition, baby had tracheoesophageal fistula (type C), and a patent foramen ovale.
Figure 1.

Showing two periglottic mass encroaching the glottis from both sides.
Figure 2.
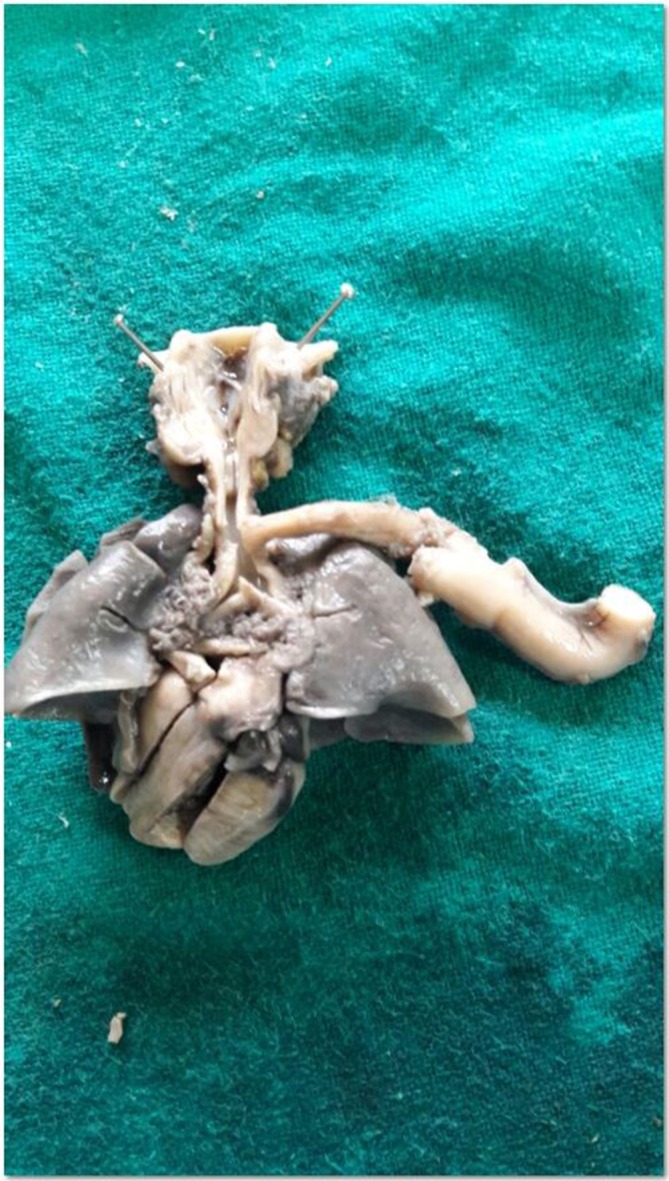
Narrowed infraglottic area is shown by the compression of masses.
Figure 3.
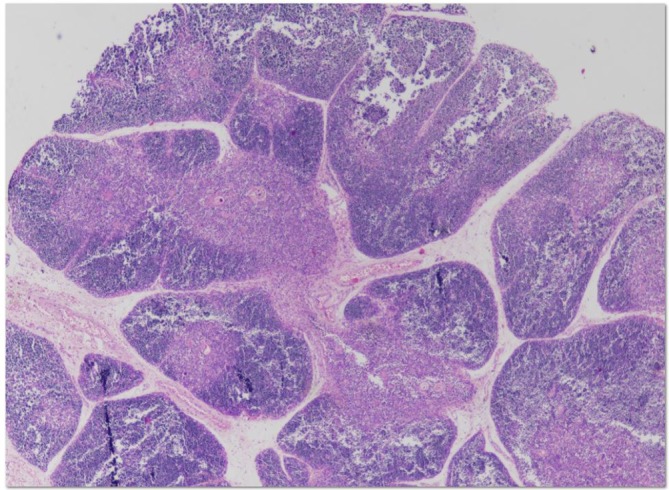
Thymus histologically shown, the outer cortex and the inner medulla. Fibrous septae arising from the capsule penetrate as far deep as the corticomedullary junction creating numerous thymic lobules.
Investigations
Pathological autopsy.
Differential diagnosis
Subglottic haemangioma.
Subglottic stenosis/web.
Ectopic thyroid.
Tracheal stenosis.
Tracheal atresia.
Outcome and follow-up
Patient died and pathological autopsy was done to find out the cause/anatomical defect.
Discussion
Ectopic thymus is an aberrant thymus tissue which presents at a location other than anterior mediastinum. This lesion generally occurs in the descent line of the thymus from the angle of the mandible to the superior mediastinum. Ectopic rest of thymic tissue could be due to failure of regression, arrested descent or abnormal migration. Ectopic thymus presenting as periglottic mass is a very rare entity. It can have varied locations and presentations.1 Ishida et al reported two cases with ectopic cervical thymus causing sudden infant death.2 Pai et al reported ectopic subglottic thymus in a 3-month-old infant presenting as congenital stridor which was surgically excised successfully.3 Ectopic thymus is rarely associated with congenital heart disease. It may include conotruncal malformations of the tetralogy of Fallot or truncus arteriosus.4 The age of presentation varies depending on the location of the ectopic thymus. Prenatal diagnosis and anticipation are key for management of these neonates. Any suspicion of cervical mass in ultrasound anomaly scan can be confirmed by MRI scan. The ectopic thymus may have an angulated configuration and moulded over adjacent structures rather than displacing or invading them. It can be confirmed by T1-weighted MRI showing homogeneous isointense to mild hyperintense tissue compared with muscle and T2-weighted image showing hyperintensity.5 Ectopic thymic mass is a benign lesion in which natural history is unclear. It should be managed conservatively in absence of any airway obstruction. A planned EXIT (Ex-Utero Intrapartum Treatment) procedure can be done and the mass can be excised endoscopically if required where airway obstruction is anticipated antenatally.6 Planned excision is preferred with infants presenting late with airway obstruction in postnatal period, though cricothyroidotomy can be done in emergency.7
Our index case was an unbooked one. It is very difficult to anticipate the airway obstruction in absence of any visible neck mass. Along with ectopic thymus, our case had bilateral renal agenesis which was resulting in severe oligohydramnios detected late in gestational age. We could not find any previous report with such association of bilateral renal agenesis with ectopic thymus in literature though chromosomal anomaly like trisomy 13 (Patau syndrome) has been associated with various anomalies related to thymus and kidney. The vertebral defect, anal atresia, cardiac defect, tracheoesophageal fistula/oesophageal atresia, renal defect and limb defect (VACTERL) association are rare conditions. Urinary tract abnormalities are seen in approximately 60%–90% of patients with VACTERL association, which is of varied severity and wide range of abnormality involved. Unilateral renal agenesis may be associated but bilateral renal agenesis is associated in severe cases but extremely rare.8 Bilateral renal agenesis is a common but lethal malformation. In few cases the aetiology is attributed to teratogenic, syndromic or single gene disorder.9 Our baby had most likely multiple congenital malformations likely due to chromosomal abnormality or VACTERL association with Potter syndrome. A karyotype and chromosomal analysis may have helped to get genetic diagnosis but was not done due to lack of facility. Parents have been counselled for future pregnancy and advised to be followed up and delivered at a tertiary/regional maternity centre for enhanced surveillance.
Learning points.
Ectopic thymus is a differential diagnosis in case of difficult intubation.
It needs a strong suspicion and MRI needs to be done to delineate the mass.
Planned EXIT procedure can be done and the mass can be excised endoscopically.
Cricothyroidotomy can be done as life-saving measure.
The delivery should be done in a tertiary setting with multidisciplinary team involvement.
Acknowledgments
We acknowledge Pruthwiraj Sethi (O and G), AIIMS Bhubaneswar, and Vandana Mohapatra (O and G), for their contribution.
Footnotes
Contributors: PKM and TKS wrote the manuscript. SP did the autopsy and AKS revised the manuscript and added valuable points. All authors finally accepted the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Ida JB, Guarisco JL, Rodriguez KH, et al. Obstructive lesions of the pediatric subglottis. Ochsner J 2008;8:119–28. [PMC free article] [PubMed] [Google Scholar]
- 2. Ishida T, Kotani H, Miyao M, et al. Ectopic cervical thymus associated with infant death: 2 case reports and literature review. Int J Pediatr Otorhinolaryngol 2013;77:1609–12. 10.1016/j.ijporl.2013.06.030 [DOI] [PubMed] [Google Scholar]
- 3. Pai I, Hegde V, Wilson PO, et al. Ectopic thymus presenting as a subglottic mass: diagnostic and management dilemmas. Int J Pediatr Otorhinolaryngol 2005;69:573–6. 10.1016/j.ijporl.2004.11.022 [DOI] [PubMed] [Google Scholar]
- 4. Freedom RM, Rosen FS, Nadas AS. Congenital cardiovascular disease and anomalies of the third and fourth pharyngeal pouch. Circulation 1972;46:165–72. 10.1161/01.CIR.46.1.165 [DOI] [PubMed] [Google Scholar]
- 5. Zielke AM, Swischuk LE, Hernandez JA. Ectopic cervical thymic tissue: can imaging obviate biopsy and surgical removal? Pediatr Radiol 2007;37:1174–7. 10.1007/s00247-007-0598-7 [DOI] [PubMed] [Google Scholar]
- 6. Pellicer M, Pumarola F, Peiró JL, et al. [EXIT procedure in the management of severe foetal airway obstruction. the paediatric otolaryngologist’s perspective]. Acta Otorrinolaringol Esp 2007;58:487–90. [PubMed] [Google Scholar]
- 7. Schloegel LJ, Gottschall JA. Ectopic cervical thymus: is empiric surgical excision necessary? Int J Pediatr Otorhinolaryngol 2009;73:475–9. 10.1016/j.ijporl.2008.10.031 [DOI] [PubMed] [Google Scholar]
- 8. Basuguy E, Akdeniz S, Ertugrul S. Bilateral renal agenesis, a severe anomaly in a premature infant with VACTERL association: a case report. Pediatric Urology Case Reports 2017;4:386–9. 10.14534/PUCR.2017632143 [DOI] [Google Scholar]
- 9. Harewood L, Liu M, Keeling J, et al. Bilateral renal agenesis/hypoplasia/dysplasia (BRAHD): postmortem analysis of 45 cases with breakpoint mapping of two de novo translocations. PLoS One 2010;5:e12375 10.1371/journal.pone.0012375 [DOI] [PMC free article] [PubMed] [Google Scholar]


