Key Teaching Points.
-
•
Nonfluoroscopic, electroanatomical guided ablation is feasible and safe in pregnant women with medical treatment–refractory arrhythmias.
-
•
The close relationship between non-coronary cusp (NCC) and right atrium tissue para-Hisian area allowed ablation of focal atrial arrhythmias originating in that location.
-
•
In this case there was a succesfull ablation of para-Hisian atrial tachycardia from the NCC without the use of fluoroscopy aided by electroanatomical mapping.
Introduction
Regular radiofrequency (RF) catheter ablation is not encouraged during pregnancy, owing to radiation exposure and the uncertainties about the maternal and fetal health, being postponed to the postpartum period. However, the intervention may be indispensable in pregnant women with severe drug-resistant tachyarrhythmia. In such cases, catheter ablation without fluoroscopy is recommended. The aim of this case report is to describe a successful atrial tachycardia catheter ablation on the non-coronary cusp, during pregnancy, and without fluoroscopy.
Case report
The patient was a 32-year-old woman, at 12th week of gestation, with a history of palpitations related to physical effort. The patient had undergone atrial tachycardia ablation in 2015 without success, when she was not pregnant. At that time, only right-sided mapping was performed with earliest activity on the septal region close to the His. Low-power (10 W) RF was applied in that region; however, the occurrences of fast junctional rhythm led to procedure interruption owing to the atrioventricular block risk. In the following 2 years, the arrhythmia remained under control with regular use of propafenone (300 mg twice a day).
During pregnancy, palpitations became more frequent and symptomatic, even under sotalol (80 mg twice a day). The echocardiogram showed normal left atrial and ventricle size and function and the patient was referred for a redo procedure owing to severe limitations induced by the atrial tachycardia that occurred during daily activities. The treadmill test confirmed the occurrence of atrial tachycardia in both peak of effort and initial phase of recovery with correlation with the symptoms.
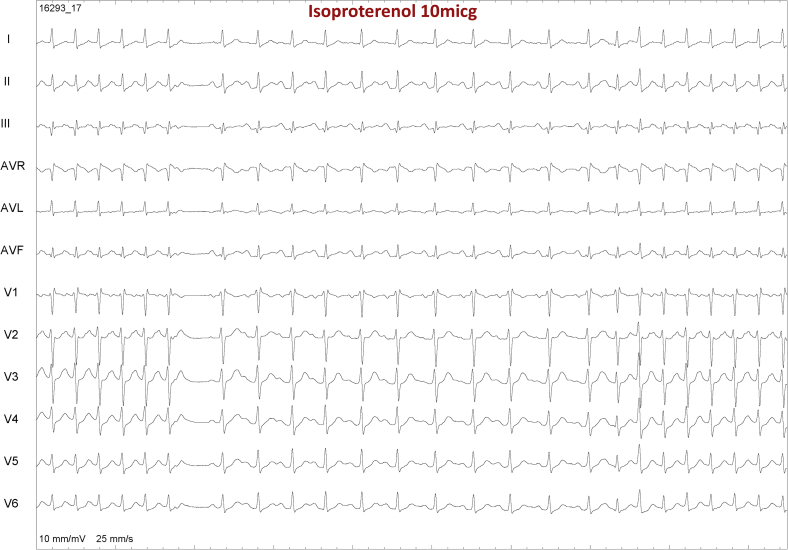
The procedure was performed in the 12th week of gestation with the patient awake and under local anesthesia. A triple puncture was performed via the right femoral vein and multipolar catheters were positioned carefully in the right atrium (RA) without fluoroscopy. Once in the RA, the nonfluoroscopic navigation system (EnSite NavX; Endocardial Solutions, Inc, Saint Paul, MN) was used to create the RA geometry. A decapolar catheter was introduced into the coronary sinus and a quadripolar catheter was positioned on the septum to record the His bundle electrogram. After isoproterenol infusion (10 μg), a 240 ms atrial tachycardia with 1:1 conduction was induced. The P-wave morphology (Figure 1) was positive in V1 and inferior leads and negative in lead I, and the P waves were narrower compared to sinus rhythm. The diagnosis of atrial tachycardia was confirmed by RV entraining maneuvers.
Figure 1.
The 12-lead electrocardiogram after 10 μg isoproterenol infusion shows P-wave morphology during sinus rhythm and tachycardia.
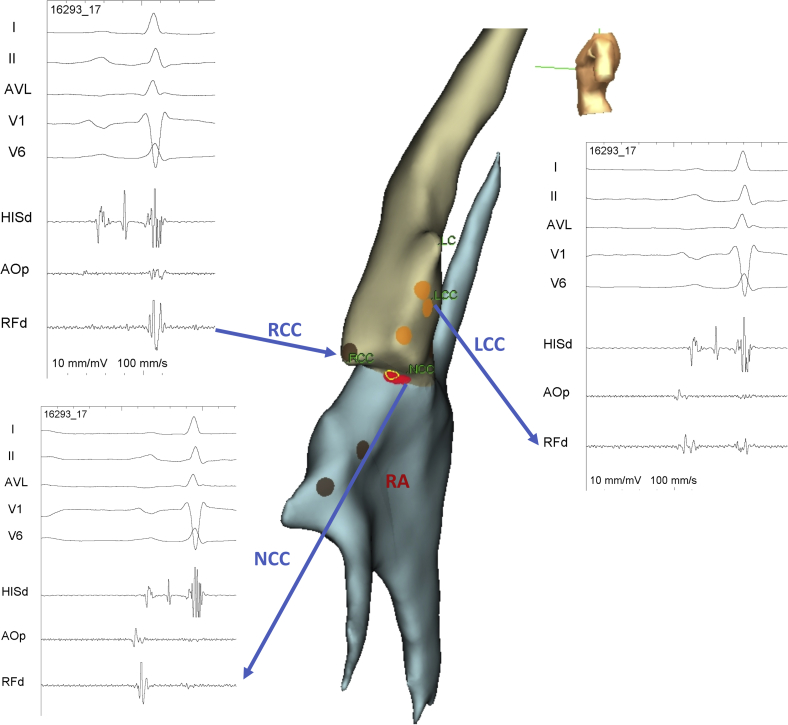
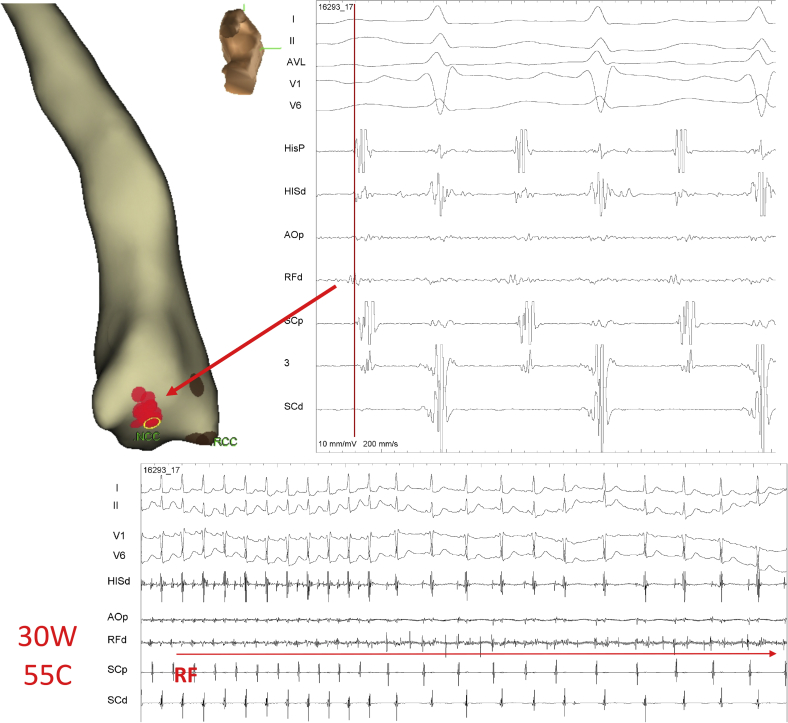
The electrophysiological mapping of the RA showed the earliest activation site (-25 ms) in the septal region in the area of the His bundle potential. Owing to prior information about junctional rhythm during low-power ablation, we decided to explore the non-coronary aortic cusp. Right femoral artery puncture was performed and a total of 10,000 units of heparin was infused in bolus. Aorta geometry was also constructed without fluoroscopy using the electroanatomical mapping system and all 3 aortic cusp positions were confirmed by electrogram in sinus rhythm (Figure 2). The mapping revealed the appropriate target in the transition of the non-coronary cusp to the right cusp (-32 ms to P wave). The RF (30 W; 55°C) delivery at this location resulted in atrial tachycardia interruption after 2 seconds (Figure 3). No junctional rhythm or PR interval prolongation was observed during application. Programmed atrial stimulation and isoproterenol did not induce any arrhythmia. All of the procedure (60 min) was performed without fluoroscopy. At the end, 5000 units of heparin were reversed to allow arterial sheath withdrawal.
Figure 2.
Right atrium (RA) and aorta geometry construction and anatomical and electrophysiology identification of all 3 coronary cusps. LCC = left coronary cusp; NCC = non-coronary cusp; RCC = right coronary cusp.
Figure 3.
Mapping on the non-coronary cusp allowed identification of earliest activation site, where radiofrequency (RF) applications (red tag) lead to atrial tachycardia interruption.
The patient remained asymptomatic and without arrhythmia on 24-hour Holter monitoring and she had a successful pregnancy with cesarean section delivery at 38 weeks (owing to obstetrical reasons), and a healthy (3150 g) infant was born. The patient remained asymptomatic without any arrhythmia after delivery.
Discussion
Prematurity, respiratory distress syndrome, and small fetus for gestational age occur more commonly (in about 20% of pregnancies) in women who suffered from antepartum severe arrhythmia. Although acute treatment of women with tachyarrhythmia using some intravenous antiarrhythmic agents is considered relatively safe for the fetus, long-term prophylactic treatment during pregnancy is a clinical problem.1
The potential long-term harmful effects of radiation exposure have generated questioning regarding the electrophysiological procedures in young patients. This issue is more complex when pregnant women are involved. Currently, no association with spontaneous abortion, congenital malformation, or growth restriction was reported in fetuses who absorbed a radiation dose less than 5 rad. However, there is evidence of an increased future risk of cancer (mainly leukemia), which is assigned to intrauterine radiation exposure.2 Thus, zero-fluoroscopy techniques are preferable in services where ionizing radiation is employed, even in small amounts.
The use of the 3-dimensional (3D) mapping system to reduce the amount of ionizing radiation during the atrial tachycardia ablation procedure has already been reported. In these reports, high success rates and low recurrence numbers were observed.3, 4 In our case, the para-Hisian location, which could be safely managed by the non-coronary cusp approach, was the difference. This approach was shown to be possible and safe owing to the close anatomical proximity between both structures.5
Although activation mapping is helpful for mapping focal arrhythmias, it was not performed in this case because when we did isoproterenol infusion, the catheter placed on the non-coronary cusp had an early activation, so we decided to ablate and not map the other cusps or perform activation mapping.
Although the studies cited above describe the approach of aortic cusps as being one of the limitations of the zero-fluoroscopy technique,1 this approach was possible in this case with the aid of electroanatomical mapping. Clearly identifying the geometry of the right and left coronary cusps was an important step to avoid the risk of applying RF close to the coronary artery ostium. Additionally, the analysis of the atrial electrogram (Figure 2), with no or only small V potential, could confirm the non-coronary cusp position, allowing safe RF application. One alternative, which was not used in this case, is the use of intracardiac echocardiogram to identify the coronary artery ostium.6
The entire procedure was performed without patient exposure to x-rays, only by analysis of the intracavitary electrograms. The anatomy was constructed using the 3D mapping system. The careful manipulation of the ablation catheter, mainly on the surface of the aortic cusps,7 was also important to minimize the risks of the procedure.
Conclusion
To the best of our knowledge, this is the first case of successful ablation of para-Hisian atrial tachycardia in a pregnant woman, in whom RF was used in the aortic cusps guided only by the 3D mapping system and intracavitary electrograms. It is important for electrophysiologists to know that pregnant women who are symptomatic may benefit from a zero-fluoroscopy technique, even if ablation in aortic cusps is required. Para-Hisian atrial tachycardia can be safely ablated from the non-coronary cusp in any patient.
References
- 1.Szumowski L., Szufladowicz E., Orczykowski M. Ablation of severe drug-resistant tachyarrhythmia during pregnancy. J Cardiovasc Electrophysiol. 2010;21:877–882. doi: 10.1111/j.1540-8167.2010.01727.x. [DOI] [PubMed] [Google Scholar]
- 2.Raman A.S., Sharma S., Hariharan R. Minimal use of fluoroscopy to reduce fetal radiation exposure during radiofrequency catheter ablation of maternal supraventricular tachycardia. Tex Heart Inst J. 2015;42:152–154. doi: 10.14503/THIJ-14-4173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferguson J.D., Helms A., Mangrum J.M., DiMarco J.P. Ablation of incessant left atrial tachycardia without fluoroscopy in a pregnant woman. J Cardiovasc Electrophysiol. 2011;22:346–349. doi: 10.1111/j.1540-8167.2010.01847.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen G., Sun G., Xu R., Chen X., Yang L., Bai Y., Yang S., Guo P., Zhang Y., Zhao C., Wang D.W., Wang Y. Zero-fluoroscopy catheter ablation of severe drug-resistant arrhythmia guided by Ensite NavX system during pregnancy: Two case reports and literature review. Medicine (Baltimore) 2016;95:e4487. doi: 10.1097/MD.0000000000004487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwai S., Badhwar N., Markowitz S.M., Stambler B.S., Keung E., Lee R.J., Chung J.H., Olgin J.E., Scheinman M.M., Lerman B.B. Electrophysiologic properties of para-Hisian atrial tachycardia. Heart Rhythm. 2011;8:1245–1253. doi: 10.1016/j.hrthm.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Liu C.F. The evolving utility of intracardiac echocardiography in cardiac procedures. J Atr Fibrillation. 2014;6:1055. doi: 10.4022/jafib.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sasaki T., Hachiya H., Hirao K., Higuchi K., Hayashi T., Furukawa T., Kawabata M., Takahashi A., Isobe M. Utility of distinctive local electrogram pattern and aortographic anatomical position in catheter manipulation at coronary cusps. J Cardiovasc Electrophysiol. 2011;22:521–529. doi: 10.1111/j.1540-8167.2010.01957.x. [DOI] [PubMed] [Google Scholar]