Abstract
Introduction
Adolescents are at high risk for negative health outcomes associated with high-risk sexual behaviors (HRSBs), and researchers have attempted to identify factors that influence such behavior so that meaningful prevention and intervention programs may be developed.
Aim
To investigate the associations between CSA experience and HRSBs in Chinese youth aged 15-24 years old.
Methods
Data were from the Survey of Youth Access to Reproductive Health in China, a national sample survey conducted in 2009. The following behaviors were classified as HRSBs: condom non-use during the first sexual experience, having sex with multiple partners, taking part in casual sex, engaging in commercial sex, taking part in anal sex, and condom non-use during the most recent sexual encounter. Differences in HRSBs between the sexes were examined. The χ2 test and binary logistic regression were used to estimate the association between CSA experience and HRSBs.
Main Outcome Measure
The sexual behaviors of condom non-use during the first sexual experience, sexual activity with multiple partners, taking part in casual sex, engaging in commercial sex (defined as paying or receiving money/gifts in exchange for sex), taking part in anal sex, and condom non-using during the most recent sexual intercourse were classified as HRSBs.
Results
4,974 Sexually active youth were included in this study, 150 respondents (3.0%) reported CSA experience, and 3,950 (79.4%) sexually active youth had engaged in at least 1 type of HRSBs. The odds of having sex with multiple partners (odds ratio [OR] 4.31, 95% CI 3.07–6.07), casual sex (OR 3.65, 95% CI 2.55–5.24), commercial sex (OR 7.43, 95% CI 5.13–10.77), anal copulation (OR 2.54, 95% CI 1.57–4.12), or any of these HRSBs (OR 5.02, 95% CI 2.33–10.80) were significantly higher among those who had experienced CSA. There was a gender-specific difference in the associations of CSA with different types of HRSBs.
Conclusion
Sexual abuse experience in childhood is highly correlated with HRSBs among Chinese youth, and the pattern of this association differs between males and females. Public knowledge and social assistance systems needs to be improved for children and youth in China. Gender-specific counter-measures may be more efficient for interventions.
Ding R, Wen X, He P, et al. Association Between Childhood and Adolescent Sexual Abuse Experiences and High-Risk Sexual Behaviors Among Chinese Youth. Sex Med 2018;6:273–281.
Key Words: Childhood Sexual Abuse, High-Risk Sexual Behaviors, Youth, China
Introduction
High-risk sexual behaviors (HRSBs) are major problems among adolescents and young people.1 The majority of people become sexually active during their adolescence period, and the development of autonomy and peer pressure often leads to increased sexual risky behaviors, including unprotected intercourse and engaging in sex with multiple partners.2 These HRSBs are the leading cause of unintended pregnancy and infection with HIV and other sexually transmitted diseases (STDs), which are recognized as serious health issues among youth.3 Youth currently account for almost 50% of all newly acquired STD cases4 and one third of new HIV infections around the world. In addition, approximately 3 million unsafe abortions are performed in girls and women aged 15–19 years old globally.5 In China, 60% of sexually transmitted HIV infections occur among people aged 15–29 years old,6 and in 2009, more than one fifth of sexually active Chinese female youth were pregnant outside of marriage, accounting for 2 to 3 million abortions.7 These data further highlight the urgent need to address HRSBs among Chinese youth.
Childhood sexual abuse (CSA) has been established as a risk factor for HRSBs in later life. On one hand, as a major childhood trauma, CSA is considered to disrupt the self-development process in children,8 with long-term negative consequences for both mental health and socioemotional factors. It can lead to low self-esteem, dissociation, alcohol use, lower danger awareness, and social isolation, which can lead further to many types of risky health behaviors including unprotected sexual intercourse, having multiple sexual partners, sex trading, and promiscuity.9 On the other hand, since most CSA victims are socioeconomically disadvantaged and relatively powerless,10 they may also be more vulnerable to HRSBs in an intimate relationship consequently. Importantly, the societal tendency to “blame the victim” in some cultural contexts may further facilitate later sexual re-victimization.11
Growing evidence suggests that CSA experience is significantly associated with HRSBs in later life.9 For females, several studies in United States and African countries12, 13, 14, 15 have found that having a history of CSA is associated with younger age at first intercourse, more sexual partners, a greater risk for substance use before sex, and more episodes of unprotected intercourse, as well as a greater chance of being diagnosed with an STD. Relatively few studies have investigated this association in males. Research from the United States16 has suggested that a history of CSA is associated with a greater likelihood of having multiple sexual partners, sex trading, and more episodes of unprotected sex among males. Some studies17, 18 in the United States have also reported an increased risk of having unprotected anal intercourse among CSA-experienced men who have sex with men. Although a systematic review12 indicated a greater odds of HRSBs among female CSA victims, most previous research13, 19 has found no significant gender difference in this association.
There is limited empirical evidence regarding the association between CSA and HRSBs in China. Comparing with other countries, the overall prevalence of CSA from previous studies20, 21 in China is relatively modest, ranging from 4.2% to 7.0%. However, most of them21, 22 are regional studies or only focused on part of adolescents and youth, unable to describe the whole picture in China. Therefore, we investigated the association between CSA experience and HRSBs among Chinese youth aged 15–24 years old based on a nationally representative survey.
Methods
Data Source
Data were from the 2009 Survey of Youth Access to Reproductive Health in China,23 which aimed to describe the knowledge, attitude, and behaviors of sexual health and explore the accessibility to reproductive health services among Chinese adolescents. There were 6 sections: individual and family information, reproductive health knowledge, knowledge of contraception and STD, reproductive health service utilization, and relationships and additional questions in the survey, with totally 152 close-ended items. The study protocol was reviewed and approved by the Institutional Review Board of Peking University. We obtained informed consent from all respondents; for participants under 18 years, the consents were obtained from their guardians.
Participants
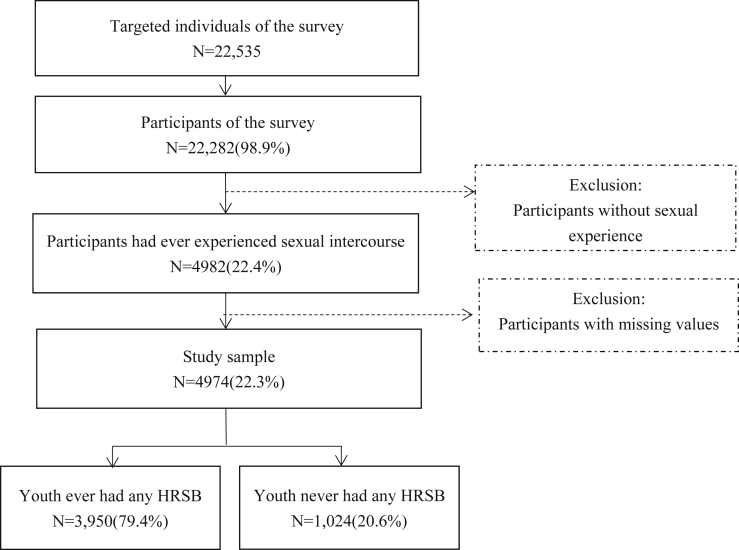
Participants were unmarried youth aged 15 to 24 years old living in mainland China. Three subpopulations were included: school youth (in school, either living on campus or in a community), household youth (living with family, either employed or unemployed), and collective household youth (employed, living in a communal house). Adolescents living in Tibet, Hong Kong, Macao, and Taiwan were excluded due to geographic, political, economic, and cultural reasons. With a refusal rate of 24.9%, 22,288 valid questionnaires were ultimately collected; Since we focused on the association between CSA and HRSBs, the study sample was restricted to subjects who had ever had sexual intercourse. Due to incomplete questionnaire, we eliminated 8 participants with missing values, and these participants were not different with total sample on sociodemographic information. A total of 4,974 cases were included in this study (Figure 1).
Figure 1.
Flowchart of the study sample. HRSBs = high-risk sexual behaviors.
Procedure
A pilot study was conducted in May 2009, and the formal survey was conducted between October 20 and November 30 of the same year. Stratified, multi-stage, and probability proportional to size sampling methods were used. The allowed sampling error, appropriation budget, time schedule, as well as data aggregation requirement were considered during the sample size estimation. The final estimated sample size was 22,535, distributed in a total of 40 cities and counties from 25 provinces, autonomous regions, and municipalities in China, with a sampling ratio of 11.4 per 100,000. 579 Interviewers were trained by the survey expert committee using the standard set; independent environments and anonymity were ensured, and all subjects were interviewed face-to-face without a third-party present. Self-administration was applied for the survey part related to sexual experience. After being completed, questionnaires were collected in ballot boxes. Additionally, sex was respected in the process, with youth being interviewed by interviewers of the same sex.
Measures
Demographic and Socioeconomic Characteristics
Age at the time of the survey was defined as a continuous variable; gender was defined as male or female; and residence was classified as urban or rural. Employment status was classified as student, worker, or unemployed; education was categorized as “junior high school or below,” “high school,” or “college or above”; and family income was classified as low, intermediate, or high.
High-Risk Sexual Behaviors
The question “Have you ever had a sexual experience (whether it was with your current/latest girlfriend/boyfriend or with any others)?” was used to determine whether a respondent was sexually experienced, if the answer was “yes,” then the participant was rated as sexually experienced. Integrating the definition of HRSBs,24 which were defined as any sexual activity that might bring a person into potential contact with the semen, blood, or vaginal secretions of a person infected with HIV, the following behaviors were classified as HRSBs: not using a condom during the first sexual experience, engaging in sexual activity with multiple partners, taking part in casual sex, engaging in commercial sex (defined as paying or receiving money/gifts in exchange for sex), taking part in anal sex, and not using a condom during the most recent sexual encounter. We also used “any HRSBs” to include any of the above 6 behaviors. All 7 variables were binary (ie, with yes or no answers).
Childhood Sexual Abuse
We employed the question “Some young people are forced to touch or be touched in sensitive body parts by others (non-boy/girlfriends). Have you ever had such an experience?” to determine whether a respondent had ever experienced sexual abuse. For “yes” responses, we extracted the age at first sexual abuse from the question “How old were you when these things first happened?” Since we were investigating the association between CSA and HRSBs, a respondent was defined as having experienced CSA when it first happened at an age equal to or younger than 18 years old.
Statistical Analysis
Data from this survey were imputed, cleaned, checked, and analyzed using software (Stata, Version 13.0; StataCorp, College Station, TX, USA). We summarized descriptive data and used χ2 tests to explore demographics, social characteristics, and CSA experiences associated with HRSBs. Adjusted odds ratios (aORs) and 95% CIs were computed using logistic regression to estimate the association between CSA and HRSBs. A P value less than .05 was considered statistically significant.
Results
Characteristics of Sample and CSA Experience
Among 4,974 sexually active youth, 150 respondents (3.0%) reported being sexually abused before the age of 18 years old, of which 16 (0.32%) respondents were sexually abused before the age of 14 years old. There were 2,863 (57.6%) males, and the average age of the study sample was 20.81 ± 2.33 years old. More than half (59.1%) of the studied youth were living in urban areas. Male participants were less likely to experience CSA than their female counterparts (2.2% vs 4.2%, P < .001). Other demographic and socioeconomic characteristics of the respondents are shown in Table 1.
Table 1.
Characteristics of Chinese youth by gender
| Total |
Male |
Female |
|
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Total | 4,974 | 2,863 (57.6) | 2,111 (42.4) |
| Age, y, mean (SD) | 20.81 (2.33) | 20.79 (2.33) | 20.82 (2.32) |
| Residence | |||
| Rural | 2,034 (40.9) | 1,174 (41.0) | 860 (40.7) |
| Urban | 2,940 (59.1) | 1,689 (59.0) | 1,251 (59.3) |
| Employment | |||
| Student | 1,599 (32.2) | 992 (34.7) | 607 (28.8) |
| Employed | 2,778 (55.8) | 1,551 (54.2) | 1,227 (58.1) |
| Unemployed | 597 (12.0) | 320 (11.2) | 277 (13.1) |
| Education | |||
| Junior high school or below | 754 (15.2) | 430 (15.0) | 324 (15.4) |
| High school | 2,367 (47.6) | 1,351 (47.2) | 1,016 (48.1) |
| College or above | 1,853 (37.25) | 1,082 (37.8) | 771 (36.5) |
| Family income | |||
| Quintile 1 (lowest) | 1,414 (28.4) | 788 (27.5) | 626 (29.7) |
| Quintile 2 | 1,875 (37.7) | 1,098 (38.4) | 777 (36.8) |
| Quintile 3 (highest) | 1,685 (33.9) | 977 (34.1) | 708 (33.5) |
| CSA experience | |||
| No | 4,824 (97.0) | 2,801 (97.8) | 2,023 (95.8) |
| Yes | 150 (3.0) | 62 (2.2) | 88 (4.2) |
CSA = childhood sexual abuse.
HRSBs Among Unmarried Chinese Youth, by CSA Experience
Overall, 79.4% of sexually active youth had engaged in at least 1 type of HRSBs (Table 2). The most common type of HRSBs was condom non-use during the first sexual experience (66.1%). The rates for sexual activity with multiple partners, casual sex, commercial sex, anal copulation, and condom non-use during the most recent sexual encounter were 21.2%, 14.6%, 9.4%, 6.5%, and 33.5%, respectively. Except condom non-use during the first sexual experience, All the other types of HRSBs were significantly more prevalent among males (P < .05).
Table 2.
Prevalence of high-risk sexual behaviors among Chinese youth, by childhood sexual abuse experience
| CSA experience | HRSBs, N (%) |
||||||
|---|---|---|---|---|---|---|---|
| Condom non-use during the first sexual experience | Sexual activity with multiple partner | Casual sex | Commercial sex | Anal copulation | Condom non-use during most recent sexual encounter | Any HRSBs | |
| Total sample | |||||||
| All | 3,286 (66.1) | 1,056 (21.2) | 728 (14.6) | 465 (9.4) | 321 (6.5) | 1,666 (33.5) | 3,950 (79.4) |
| No | 3,197 (66.3) | 980 (20.3) | 673 (14.0) | 404 (8.4) | 299 (6.2) | 1,607 (33.3) | 3,807 (78.9) |
| Yes | 89 (59.3) | 76 (50.7) | 55 (36.7) | 61 (40.7) | 22 (14.7) | 59 (39.3) | 143 (95.3) |
| χ2 (P) | 3.13 (.08) | 80.14 (<.001) | 60.08 (<.001) | 179.00 (<.001) | 17.28 (<.001) | 2.37 (.12) | 23.98 (<.001) |
| Male sample | |||||||
| All | 1,915 (66.9) | 732 (25.6) | 515 (18.0) | 334 (11.7) | 206 (7.2) | 1,010 (35.3) | 2,339 (81.7) |
| No | 1,888 (67.4) | 694 (24.8) | 485 (17.3) | 296 (10.6) | 192 (6.9) | 988 (35.3) | 2,280 (81.4) |
| Yes | 27 (43.6) | 38 (61.3) | 30 (48.4) | 38 (61.3) | 14 (22.6) | 22 (35.5) | 59 (95.2) |
| χ2 (P) | 15.59 (<.001) | 42.50 (<.001) | 39.70 (<.001) | 151.44 (<.001) | 22.47 (<.001) | 0.001 (.97) | 7.68 (.006) |
| Female sample | |||||||
| All | 1,371 (65.0) | 324 (15.4) | 213 (10.1) | 131 (6.2) | 115 (5.5) | 656 (31.1) | 1,611 (76.3) |
| No | 1,309 (64.7) | 286 (14.1) | 188 (9.3) | 108 (5.3) | 107 (5.3) | 619 (30.6) | 1,527 (75.5) |
| Yes | 62 (70.5) | 38 (43.2) | 25 (28.4) | 23 (26.1) | 8 (9.1) | 37 (42.1) | 84 (95.5) |
| χ2 (P) | 1.22 (.27) | 54.76 (<.001) | 33.97 (<.001) | 62.67 (<.001) | 2.37 (.12) | 5.16 (.02) | 18.61 (<.001) |
CSA = childhood sexual abuse; HRSBs = high-risk sexual behaviors.
Table 2 depicts the relationship between CSA experience and HRSBs. Compared with participants without CSA experience, those who had experienced CSA reported significantly higher rates of engaging in sexual activity with multiple partners, casual sex, commercial sex, and anal copulation. There were some differences between full-sample and gender-specific results. The prevalence of condom non-use during the first sexual experience was significantly lower among males who had experienced CSA. In females, the prevalence of condom non-use during the most recent sexual encounter was significantly higher among those who had experienced CSA. No statistically significant differences in the prevalence of anal copulation were found between female youth with and without CSA experience.
Association Between CSA Experience and HRSBs
Table 3 presents the results of logistic regression analyses for different types of HRSBs as outcome variables. After adjusting for demographic and socioeconomic characteristics, the odds of engaging in sexual activity with multiple partners (odds ratio [OR] 4.3, 95% CI 3.1–6.1), casual sex (OR 3.7, 95% CI 2.6–5.2), commercial sex (OR 7.4, 95% CI 5.1–10.8), anal copulation (OR 2.5, 95% CI 1.6–4.1), and any such HRSBs (OR 5.0, 95% CI 2.3–10.8) were significantly higher among those who had experienced CSA. There were no significant associations between CSA and other types of HRSBs.
Table 3.
Association of child sexual abuse experience with high-risk sexual behaviors: adjusted odds ratio and 95% CIs
| Characteristics | HRSBs, aOR (95% CI) |
||||||
|---|---|---|---|---|---|---|---|
| Condom non-use during the first sexual experience | Sexual activity with multiple partner | Casual sex | Commercial sex | Anal copulation | Condom non-use during most recent sexual encounter | Any HRSBs | |
| CSA experience | |||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 0.7 (0.5–1.0)∗ | 4.3 (3.1–6.1)† | 3.7 (2.6–5.2)† | 7.4 (5.1–10.8)† | 2.5 (1.6–4.1)† | 1.3 (0.9–1.8) | 5.0 (2.3–10.8)† |
| Covariates | |||||||
| Age | 0.93 (0.90–0.96)† | 0.91 (0.87–0.95)† | 0.85 (0.83–0.90)† | 0.94 (0.88–0.99)∗ | 0.95 (0.89–1.02) | 0.99 (0.96–1.03) | 0.88 (0.85–0.92)† |
| Gender | |||||||
| Male | 1.1 (1.0–1.3) | 2.1 (1.8–2.4)† | 2.1 (1.8–2.6)† | 2.3 (1.8–2.9)† | 1.4 (1.1–1.8)‡ | 1.2 (1.1–1.4)‡ | 1.5 (1.3–1.7)† |
| Female | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Residence | |||||||
| Rural | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Urban | 1.0 (0.9–1.2) | 1.1 (1.0–1.3) | 1.5 (1.3–1.8)† | 1.4 (1.1–1.7)∗ | 1.3 (1.0–1.7) | 1.1 (1.0–1.3) | 1.1 (1.0–1.3) |
| Employment | |||||||
| Student | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Employed | 1.5 (1.2–1.8)† | 1.4 (1.1–1.7)‡ | 1.5 (1.1–1.9)‡ | 0.7 (0.5–0.9)∗ | 1.0 (0.7–1.4) | 0.9 (0.8–1.1) | 1.4 (1.1–1.7)‡ |
| Unemployed | 1.8 (1.4–2.2)† | 1.5 (1.2–2.0)† | 1.8 (1.3–2.3)† | 0.7 (0.5–1.0)∗ | 1.2 (0.8–1.7) | 1.0 (0.8–1.2) | 1.5 (1.2–2.0)† |
| Education | |||||||
| Junior high school or below | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| High school | 0.8 (0.6–0.9)‡ | 0.9 (0.8–1.2) | 0.9 (0.7–1.2) | 0.8 (0.6–1.0) | 1.1 (0.7–1.6) | 0.8 (0.7–1.0)∗ | 0.9 (0.7–1.1) |
| College or above | 0.7 (0.5–0.8)† | 0.9 (0.7–1.1) | 1.2 (0.9–1.6) | 0.5 (0.3–0.7)† | 1.2 (0.8–1.9) | 0.6 (0.5–0.8)† | 0.7 (0.5–0.8)‡ |
| Family Income | |||||||
| Quintile 1 (lowest) | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Quintile 2 | 1.1 (0.9–1.2) | 0.9 (0.8–1.1) | 0.7 (0.5–0.8)† | 0.5 (0.4–0.7)† | 0.7 (0.5–0.9)∗ | 0.8 (0.7–1.0)∗ | 0.9 (0.8–1.1) |
| Quintile 3 (highest) | 1.1 (0.9–1.3) | 1.3 (1.1–1.6)‡ | 1.0 (0.8–1.2) | 0.9 (0.7–1.2) | 1.5 (1.1–2.0)‡ | 1.0 (0.9–1.2) | 1.0 (0.8–1.2) |
aOR = adjusted odds ratio; CSA = childhood sexual abuse; HRSBs = high-risk sexual behaviors.
P < .05.
P < .001.
P < .01.
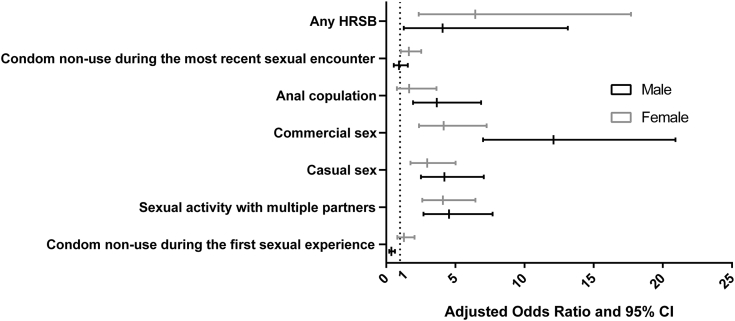
Figure 2 shows the estimated aOR and 95% CI of different types of HRSBs by gender and CSA experience. CSA experience was significantly associated with sexual activity with multiple partners, casual sex, and commercial sex in both the male and female subsamples. In males, compared to youth without CSA experience, the odds of having anal copulation (aOR 3.7, 95% CI 1.9–6.9) was significantly higher among those with CSA experience. Condom non-use during the first sexual experience was significantly less probable among CSA-experienced males (aOR 0.4, 95% CI 0.2–0.6). In females, there were no significant associations between CSA experience and anal copulation. The odds of condom non-use during the most recent sexual encounter was significantly higher among female youth with CSA experience (aOR 1.6, 95% CI 1.1–2.5).
Figure 2.
Adjusted odds ratio and 95% CI of different types of high-risk sexual behaviors (HRSB), by gender and child sexual abuse experience.
Discussion
We investigated the association between CSA experience and HRSBs among Chinese youth aged 15–24 years old based on Youth Access to Reproductive Health in China survey data from 2009. The prevalence of HRSBs in our study was higher comparing with previous studies25 in developed countries possibly due to the changes in social attitudes and inadequate access to sexual and reproductive services among Chinese youth in recent years.26 We observed a strong association between CSA and HRSBs. In addition, the risk of engaging in different types of HRSBs was significantly higher among youth with a CSA history. To the best of our knowledge, this is the first study that has used population-based data from China to examine the relation between CSA experience and HRSBs in youth, and provides evidence to the existing literature in developing nations of a non-Western context.
Consistent with previous studies in other countries,11, 27 a history of CSA was associated with an elevated risk of engaging in any HRSBs among Chinese youth. And the significant associations between CSA and sexual activity with multiple partner, casual sex, commercial sex and anal copulation further demonstrated our conclusion. Although the causal relationship between CSA and HRSBs cannot be demonstrated by our study design, a previous study suggested that CSA might have lasting negative effects on mental and reproductive health during adolescence and adulthood. Several theoretical explanations have been proposed to account for this associations. The Finkelhor28 “trauma-genic dynamics” model suggested that CSA experience may alter a child’s cognitive or emotional orientation to the world and causes trauma by distorting the child’s self-concept, world view, or affective capacities. Building on this theorizing, most of previous studies claimed that CSA history may not only exacerbate the tendency to internalize problems,9 such as post-traumatic stress disorder, depression, low self-esteem, dissociation, and low danger awareness,11 but also operate through externalizing aspects, causing more impulsivity and inattention, meanwhile inhibiting control, planning, and decision-making,29 making victims more vulnerable to HRSBs. Our findings highlight the risk of HRSB among youth with CSA experience and the needs to increase public awareness in China.
Furthermore, we found a gender difference. Consistent with previous studies,30, 31 a significant association between CSA experience and anal copulation was only observed among male youth. 1 Study in the United States32 found that CSA was associated with a greater likelihood of unprotected anal copulation among gay and bisexual men. In females, not using a condom during the most recent sexual encounter was positively correlated with CSA experience. A previous study that conducted path analyses indicated that control and relationship power played mediating roles in HRSBs in females sexually abused as children.33 Future interventions that include counseling CSA victims, publicizing the issue, and educating society about STD prevention using a gender-specific approach may be needed to reduce the risk among youth, especially those with CSA experience, engaging in potentially dangerous HRSBs.
We also found that the risk of condom non-use during the first sexual experience was significantly lower in males with CSA experience, which is inconsistent with our other findings and the results of previous studies.16, 34 However, 1 study35 suggested that males with CSA experience tend to have lower sexual self-esteem, which is correlated with higher contraception use during penetrative sex,36 since sexual intercourse without contraception may be considered as a symbol of masculine power aligned with positive sexual self-concept in males in certain cultures.37 This could potentially explain this surprising finding in our study.
Limitations
This study had several limitations. First, the Youth Access to Reproductive Health in China survey only focused on unmarried youth; the CSA experience and HRSBs of married youth could not be observed. Secondly, any prevalence related to sexual experience is likely to be underreported including HRSB and CSA because these experiences are still a very sensitive topic in China, and worries of shame and embarrassment may lead to underreporting such information. Thirdly, the prevalence of CSA may be underestimated because our estimation was based on some specific questions rather than a standard measurement scale, which tend to elicit higher rates. Additionally, we were unable to examine causal relationships between CSA and HRSBs due to the cross-sectional design, and the possibility that youth who engaged into HRSBs before adulthood are at higher risk of being sexually abused cannot be excluded. Future research using more detailed and in-depth measurements of sexual abuse and HRSBs may shed greater light on this topic.
Conclusion
HRSBs is a serious threat to both the physical and mental health of youth in China, and it is highly associated with CSA. Youth who experience CSA are exposed to a higher risk of HRSBs and consequent reproductive health problems, and the pattern of this association differs by gender. Our results have some implications for public reproductive health practice and research.
In general, for future public adolescent reproductive health interventions, more effort should focus on improving public knowledge about CSA and establishing preventive measures and social assistance systems for sexually abused children in China. In addition, future studies and practices should take gender-specific differences into consideration and explore more efficient interventions for bio-psychosocial risk factors; in particular, more emphasis in terms of public awareness should be placed on male victims, since to date they have generally been neglected compared to females.
Statement of authorship
Category 1
-
(a)Conception and Design
- Ruoxi Ding; Xu Wen
-
(b)Acquisition of Data
- Xiaoying Zheng
-
(c)Analysis and Interpretation of Data
- Ruoxi Ding
Category 2
-
(a)Drafting the Article
- Ruoxi Ding
-
(b)Revising It for Intellectual Content
- Ping He; Chao Guo; Yanan Luo
Category 3
-
(a)Final Approval of the Completed Article
- Xiaoying Zheng; Xinming Song
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Kotchick B.A., Shaffer A., Forehand R. Adolescent sexual risk behavior: a multi-system perspective. Clin Psychol Rev. 2001;21:493–519. doi: 10.1016/s0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- 2.Donahue K.L., Lichtenstein P., Lundström S. Childhood behavior problems and adolescent sexual risk behavior: familial confounding in the Child and Adolescent Twin Study in Sweden (CATSS) J Adolesc Health. 2013;52:606–612. doi: 10.1016/j.jadohealth.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drago F., Ciccarese G., Zangrillo F. A survey of current knowledge on sexually transmitted diseases and sexual behavior in Italian adolescents. Int J Environ Res Public Health. 2016;13:422. doi: 10.3390/ijerph13040422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siracusano S., Silvestri T., Casotto D. Sexually transmitted diseases: epidemiological and clinical aspects in adults. Urologia. 2014;81:200–208. doi: 10.5301/uro.5000101. [DOI] [PubMed] [Google Scholar]
- 5.Joint United Nations Programme on HIV/AIDS (UNAIDS) UNAIDS; Geneva: 2014. World AIDS Day Report: fact sheet. [Google Scholar]
- 6.Ma Q., Masako O.K., Cong L. Sexual behavior and awareness of Chinese university students in transition with implied risk of sexually transmitted diseases and HIV infection: a cross-sectional study. BMC Public Health. 2006;6:232. doi: 10.1186/1471-2458-6-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Ministry of Health in P. R. China. Almanac of China's Health 2009 (2010) Chinese Xiehe Medical University Publishing House. [In Chinese]
- 8.Zhu Q., Gao E., Cheng Y. Child sexual abuse and its relationship with health risk behaviors among adolescents and young adults in Taipei. Asia Pac J Public Health. 2015;27:643–651. doi: 10.1177/1010539515573075. [DOI] [PubMed] [Google Scholar]
- 9.Senn T.E., Carey M.P., Vanable P.A. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grauerholz L. An ecological approach to understanding sexual revictimization: linking personal, interpersonal, and sociocultural factors and processes. Child Maltreat. 2000;5:5–17. doi: 10.1177/1077559500005001002. [DOI] [PubMed] [Google Scholar]
- 11.Lalor K., McElvaney R. Child sexual abuse, links to later sexual exploitation/high-risk sexual behavior, and prevention/treatment programs. Trauma Violence Abuse. 2010;11:159–177. doi: 10.1177/1524838010378299. [DOI] [PubMed] [Google Scholar]
- 12.Abajobir A.A., Kisely S., Maravilla J.C. Gender differences in the association between childhood sexual abuse and risky sexual behaviors: a systematic review and meta-analysis. Child Abuse Neglect. 2016;63:249–260. doi: 10.1016/j.chiabu.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 13.Bensley L.S., Eenwyk J.V., Simmons K.W. Self-reported childhood sexual and physical abuse and adult HIV-risk behaviors and heavy drinking. Am J Prev Med. 2000;18:151–158. doi: 10.1016/s0749-3797(99)00084-7. [DOI] [PubMed] [Google Scholar]
- 14.Wilson H.W., Widom C.S. An examination of risky sexual behavior and HIV in victims of child abuse and neglect: a 30-year follow-up. Health Psychol. 2008;27:149–158. doi: 10.1037/0278-6133.27.2.149. [DOI] [PubMed] [Google Scholar]
- 15.Richter L., Komárek A., Desmond C. Reported physical and sexual abuse in childhood and adult HIV risk behavior in three African countries: findings from Project Accept (HPTN-043) AIDS Behav. 2014;18:381–389. doi: 10.1007/s10461-013-0439-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diiorio C., Hartwell T., Hansen N. Childhood sexual abuse and risk behaviors among men at high risk for HIV infection. Am J Public Health. 2002;92:214–219. doi: 10.2105/ajph.92.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paul J.P., Catania J., Pollack L. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: the Urban Men's Health Study. Child Abuse Negl. 2001;25:557–584. doi: 10.1016/s0145-2134(01)00226-5. [DOI] [PubMed] [Google Scholar]
- 18.Kalichman S.C., Gore-Felton C., Benotsch E. Trauma symptoms, sexual behaviors, and substance abuse: correlates of childhood sexual abuse and HIV risks among men who have sex with men. J Child Sexual Abus. 2004;13:1–15. doi: 10.1300/J070v13n01_01. [DOI] [PubMed] [Google Scholar]
- 19.Haydon A.A., Hussey J.M., Halpern C.T. Childhood abuse and neglect and the risk of STDs in early adulthood. Perspect Sex Reprod Health. 2011;43:16–22. doi: 10.1363/4301611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen J., Dunne M.P., Han P. Child sexual abuse in China: a study of adolescents in four provinces. Child Abuse Negl. 2004;28:1171–1186. doi: 10.1016/j.chiabu.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Luo Y., Parish W.L., Laumann E.O. A population-based study of childhood sexual contact in China: prevalence and long-term consequences. Child Abuse Negl. 2008;32:721–731. doi: 10.1016/j.chiabu.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen J., Dunne M.P., Han P. Child sexual abuse in Henan province, China: associations with sadness, suicidality, and risk behaviors among adolescent girls. J Adolesc Health. 2006;38:544–549. doi: 10.1016/j.jadohealth.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Zheng X., Chen G. Survey of youth access to reproductive health in China [in Chinese] Population Development. 2010;16:2–16. [Google Scholar]
- 24.Goedert J.J. What is safe sex? Suggested standards linked to testing for human immunodeficiency virus. N Engl J Med. 1987;316:1339–1342. doi: 10.1056/NEJM198705213162111. [DOI] [PubMed] [Google Scholar]
- 25.Wellings K., Collumbien M., Slaymaker E. Sexual behavior in context: a global perspective. Lancet. 2006;368:1706–1728. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- 26.Guo C., Zhang L., Wang Z. Prevalence of and disparities in HIV-related sexual risk behaviors among Chinese youth in relation to sexual orientation: a cross-sectional study. Sexual Health. 2016;13:497–499. doi: 10.1071/SH15190. [DOI] [PubMed] [Google Scholar]
- 27.Draucker C.B., Mazurczyk J. Relationships between childhood sexual abuse and substance use and sexual risk behaviors during adolescence: an integrative review. Nurs Outlook. 2013;61:291–310. doi: 10.1016/j.outlook.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Finkelhor D. The trauma of child sexual abuse: two models. J Interpers Violence. 1987;2:348–366. [Google Scholar]
- 29.Crockett L.J., Raffaelli M., Shen Y.L. Linking self-regulation and risk proneness to risky sexual behavior: pathways through peer pressure and early substance use. J Res Adolesc. 2010;16:503–525. [Google Scholar]
- 30.Williams J.K., Wilton L., Magnus M. Relation of childhood sexual abuse, intimate partner violence, and depression to risk factors for HIV among black men who have sex with men in 6 US cities. Am J Public Health. 2015;105:2473–2481. doi: 10.2105/AJPH.2015.302878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mimiaga M.J., Noonan E., Donnell D. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE study. J Acquir Immune Defic Syndr. 2009;51:340–348. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jinich S., Paul J.P., Stall R. Childhood sexual abuse and HIV risk-taking behavior among gay and bisexual men. AIDS Behav. 1998;2:41–51. [Google Scholar]
- 33.Mosack K.E., Randolph M.E., Dicksongomez J. Sexual risk-taking among high-risk urban women with and without histories of childhood sexual abuse: mediating effects of contextual factors. J Child Sexual Abus. 2010;19:43–61. doi: 10.1080/10538710903485591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson H.W., Widom C.S. Sexually transmitted diseases among adults who had been abused and neglected as children: a 30-year prospective study. Am J Public Health. 2009;99:197–203. doi: 10.2105/AJPH.2007.131599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krahé B., Berger A. Gendered pathways from child sexual abuse to sexual aggression victimization and perpetration in adolescence and young adulthood. Child Abuse Negl. 2016;63:261–272. doi: 10.1016/j.chiabu.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Lefkowitz E.S. Sexual esteem in emerging adulthood: associations with sexual behavior, contraception use, and romantic relationships. J Sex Res. 2015;52:795–806. doi: 10.1080/00224499.2014.945112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oudshoorn N. Astronauts in the sperm world: the renegotiation of masculine identities in discourses on male contraceptives. Men Masculinities. 2004;6:349–367. [Google Scholar]