Abstract
Fecal microbiota transplantation (FMT) has evolved into a robust and efficient means for treating recurrent Clostridium difficile infection (CDI). Our narrative review looks at the donor selection, preparation, delivery techniques and cost-effectiveness of FMT. We searched electronic databases, including PubMed, MEDLINE, Google Scholar, and Cochrane Databases, for studies that compared the biological effects of donor selection, fresh or frozen fecal preparation, and various delivery techniques. We also evaluated the cost-effectiveness and manually searched references to identify additional relevant studies. Overall, there is a paucity of studies that directly compare outcomes associated with related and non-related stool donors. However, inferences from prior studies indicate that the success of FMT does not depend on the donor-patient relationship. Over time, the use of unrelated donors has increased because of the formation of stool banks and the need to save processing time and capital. However, longitudinal studies are needed to clarify the optimal freezing time before microbial function declines. Several FMT techniques have been developed, such as colonoscopy, enema, nasogastric or nasojejunal tubes, and capsules. The comparable and high efficacy of FMT capsules, combined with their convenience, safety and aesthetically tolerable mode of delivery, makes it an attractive option for many patients. Cost-effective models comparing these various approaches support the use of FMT via colonoscopy as being the best strategy for the treatment of recurrent CDI.
Keywords: Clostridium difficile, fecal microbiota transplantation, donor selection, capsule, colonoscopy, enema
Introduction
Clostridium difficile infection (CDI) represents a major clinical and economic burden on healthcare systems [1]. The management of treatment failure and recurrent CDI poses a significant challenge, which drives the cost of healthcare because of their associated morbidity and mortality [2]. Recurrent CDI is reported in 10-30% of patients after initial treatment, with recurrence approaching 60% after the third episode of CDI [3]. Restoration of gut diversity through fecal microbiota transplantation (FMT) has emerged as an effective treatment for CDI-associated diarrhea in patients with recurrent disease after initial antibiotic therapy [4]. A variety of approaches to FMT have been studied, including outcomes associated with donor selection, fecal samples and various delivery techniques, including upper or lower gastrointestinal routes [5]. We herein review current knowledge on FMT and in particular its relationship to donor selection, use of frozen or fresh fecal samples, and delivery systems. We also review the cost-effectiveness of FMT by various delivery systems.
Materials and methods
In this narrative review, studies were searched in electronic databases according to article titles, abstract contents, and relevance in the field of FMT through the end of April 2018. The databases used in this review included PubMed, MEDLINE, Google Scholar, and Cochrane Databases. The main terms applied were Clostridium difficile, Clostridium difficile infection, fecal microbiota transplantation, fecal transplantation, fecal bacteriotherapy, intestinal microbiota transplantation, floral reconstitution, infectious diarrhea, donor selection, related donor, fresh stool, frozen stool, capsules, colonoscopy, enema, and management. We also manually searched references to identify additional relevant studies. Articles published in languages other than English were excluded.
Related versus unrelated donors
Early FMT practices offered patients the opportunity to select relatives as a source of stool for transplantation [6,7]. In the event the patient could not identify a donor, a healthy volunteer was chosen. The selected volunteers were often other hospital patients, medical students, or residents [6-9]. Early reviews noted the preference for related donors [10-12] due to their genetic similarity and shared environment, both of which are known to influence gut diversity [13]. A shared environment also reduced the risk of transferring infectious agents to the patient [10,14,15]. However, it was noted that there was no rationale for excluding healthy volunteers [16], and subsequent systematic reviews [4,17] and meta-analysis [18] did not report a statistically significant difference in outcomes based on donor selection. Recently, with the use of stool banks, the use of unrelated donors has increased significantly [19,20].
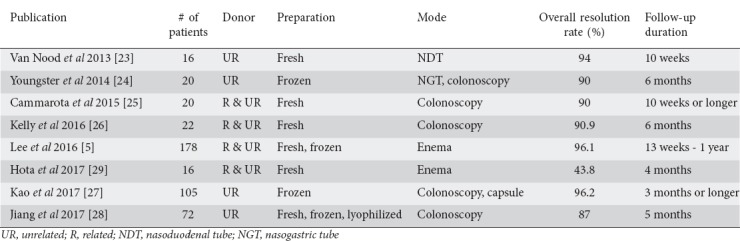
There are limited data on direct comparisons of related and unrelated donors. Inferences from randomized controlled trials (RCTs) are also limited, as those trials were not structured to investigate the donor-patient relationship and their outcomes (Table 1) [5,23-29]. Retrospective studies from the United States [21] and Finland [22] were limited by small sample sizes and found no significant difference in outcomes after eight weeks and one year, respectively (100% vs. 78.6% resolution; 70% vs. 92% resolution, related and unrelated donors respectively). Six RCTs used exclusively unrelated or related donors, or a mixture [5,23,24,26-28], while two RCTs used almost exclusively related donors [25,29]. The rate of resolution in 7 of 8 RCTs ranged from 87-96.2%; one study that utilized a single enema infusion reported a resolution of 43.8%. When compared to the resolution rate of other studies that utilized a single enema infusion, it did not appear to be an outlier (47.9% [30] and 51.6% [31]). Overall, current evidence indicates that the success of FMT does not depend on the donor-patient relationship; however, larger studies should be designed to explore this area in greater detail.
Table 1.
Summary of randomized controlled trials of fecal microbiota transplantation for recurrent Clostridium difficile infection
The advantages of using unrelated donors stem from their easy access and availability from stool banks. It can take weeks to screen a donor [4], thus time and capital are saved by treating patients with donations from an established source. Furthermore, accessibility to FMT is increased by removing the burden of donor screening and processing from healthcare providers [21,32,33]. However, ethical concerns regarding the privacy and ownership of stool have been raised [34,35]. It is unclear how these issues affect patients or stool banks.
Additional benefits of using unrelated donors include the avoidance of unpleasing or difficult conversations with related donors [36,38,39]. A survey of 183 FMT-naïve patients found that 28% of patients found selecting their own donor too unappealing to consider FMT as a treatment [37]. On the other hand, experience from another institution found that, when given a choice after switching to using frozen stool from unrelated donors, all patients preferred the unrelated donor option [21]. These data suggests that some patients struggle with discussing FMT with related donors and may prefer using unrelated donors.
A third option, the autologous donor, involves stool taken from an individual when their disease is in remission [40,41]. Stool can be used as treatment for that individual when the disease relapses. Although implementing this form of personalized medicine has been made easier by the creation of stool banks, its practicality and effectiveness have yet to be evaluated. Regardless of the donor utilized, the recommendation from consensus and working groups around the world emphasizes that every donor should be carefully and thoroughly screened before FMT is performed [42-46].
Frozen versus fresh fecal preparation
Another significant evolution in the practice of fecal transplantation has been the use of frozen fecal matter. The earliest records can be traced to a report in 1998 by a group in Norway [47,48]. Frozen cultures had been used 9 years previously by Tvede and Rask-Maden to treat 5 patients, but their transplant material was referred to as “synthetic stool” as it was a limited combination of cultured bacterial strains [49]. The overall efficacy of the studies performed in Norway ranged from 83-100% [17,47,48].
Since then, most studies involving frozen fecal matter have reported an overall CDI cure rate between 81-100% [5,21,22,24,28,31,50-54] (Table 2). Two retrospective analyses [21,22] and three RCTs [5,24,28] directly compared fresh and frozen stool. All five studies reported primary outcomes that did not differ between fresh and frozen stool. No significant differences were noted, despite the range in the storage time of frozen fecal matter (1 week to 6 months). One small case series involving 3 patients [55] and a pilot clinical trial involving 7 patients who received frozen stool [56] reported lower resolution rates (67% and 71.4% respectively). Besides the significant limitation of small sample sizes, the case series involved patients suffering from severe CDI, one who refused a second transplant and ultimately passed away from fulminant disease [55]. The pilot trial treated patients suffering an initial episode of CDI, some of whom were concomitantly or recently on antibiotics for other indications, with a protocol that did not include a bowel lavage [56]. These differences may have contributed to a lower resolution rate. Regardless, current evidence appears to indicate similar efficacy among frozen and fresh fecal preparations.
Table 2.
Summary of studies of fecal microbiota transplant utilizing frozen stool
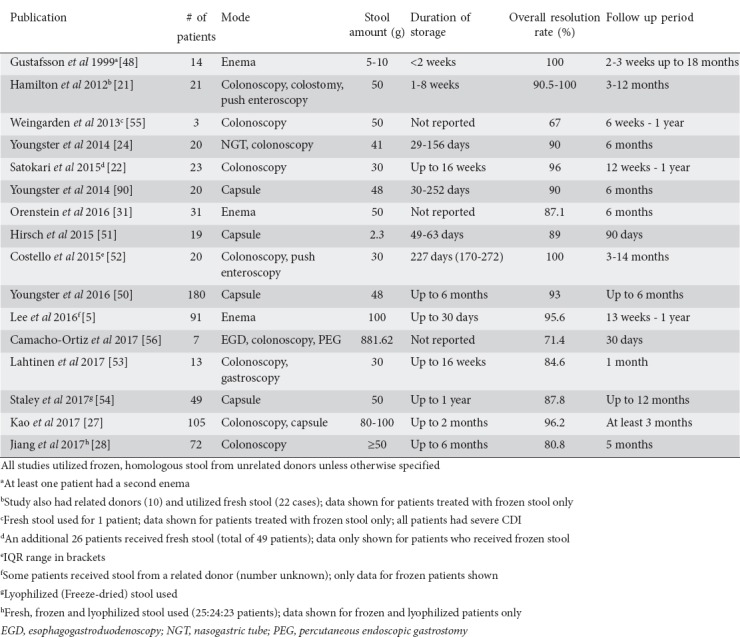
A central question related to the use of frozen stool is the viability of the microbiome over time. Costello et al tested bacterial viability after six months of storage [52]. The study showed that the microbiome remained largely unchanged after six months. CDI resolution has been achieved following 10 months of storage, while other studies have reported successful outcomes of FMT after six months [28,50] and up to 1 year of storage [54]. Similar results have been reported in mice models, though a decline in quantity and diversity was observed after seven months of storage [57]. Given the benefits of frozen fecal transplant material and evidence to support its durability, clinicians trained in the use of FMT may be more inclined to use frozen preparations.
In 2015, an innovation in fecal preparation involved the use of freeze-dried stool [59]. Also known as lyophilized stool, a fresh suspension is transferred to a vacuum drier that produces a powdered product, which is then encapsulated. The motivation behind the creation of lyophilized stool was to develop a more concentrated and conveniently stored product with the hope that patients could utilize it at home. Various studies, including a case report [59], a retrospective study [60], pragmatic cohort study [54] and an RCT [28], have reported on the use of lyophilized stool with resolution rates ranging from 78-100%. The RCT by Jiang et al found lyophilized stool to be statistically less effective than fresh stool (78% vs. 100%, P=0.022) but equally effective as frozen stool (78% vs. 83%, P=0.255) in resolving recurrent CDI [28]. Further studies are needed to determine the efficacy and safety of lyophilized stool.
Delivery methods
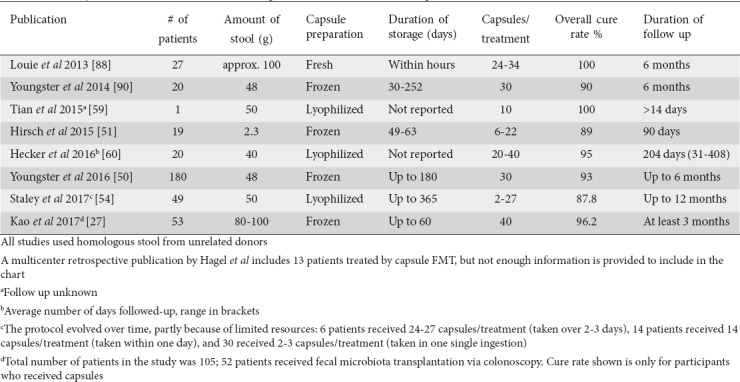
Until 1990, enema was the method of choice for fecal transplant. Since then, various routes have been tested; however, the most optimal route of administration remains unclear. Delivery can be broadly classified into upper and lower gastrointestinal routes. Common upper gastrointestinal routes include esophagogastroduodenoscopy via enteric tubes (nasogastric, nasoduodenal, and nasojejunal tubes), and oral capsules [32,52,61-64]. Common lower gastrointestinal methods include colonoscopy and enemas [21,65-67]. There are benefits and pitfalls for each modality and physicians often choose one that best fits a combination of their patients’ needs, their expertise and availability (Table 3).
Table 3.
Summary of studies of fecal microbiota transplantation delivered via oral capsules
The major advantage that colonoscopy offers over other modalities is the ability to visualize the entire colon [40,68-72]. It also enables reliable delivery of stool to affected segments of the bowel [71,73,74] and possibly better retention of stool [73]. This can be particularly important, since it has been observed that the proximal colon has more severe pseudomembranous changes [75]. Furthermore, colonoscopy can deliver larger amounts of stool per transplant procedure [40,71,74,76], associated with higher success rates [17]. Bowel preparation before the procedure is suggested to increase the likelihood of resolution of CDI by decreasing the number of spores and residual organisms [74]. However, there is a risk of bowel perforation, and those who are severely ill may not tolerate the procedure or anesthesia [69,77,78,79].
Enemas are less invasive, easier to perform, and relatively less expensive [80]. The ease and simplicity of an enema allows it to be used in the hospital, ambulatory offices, and even at home [81,82]. However, there are greater concerns regarding retention of stool, as well as the risk that stool would not reach beyond the splenic flexure [72], which may require multiple infusions to achieve efficacy [83]. Greater facility time and personnel are sometimes required to maintain and rotate the patient between various positions to compensate for poor retention [70]. Additionally, patients with poor sphincter tone or issues with incontinence may augment concerns about retention [80].
Upper gastrointestinal routes are typically faster, less expensive and better tolerated compared to colonoscopy, though not as esthetically pleasing to some patients [12,15,16,61,68,70]. Typically, less stool sample is used when upper gastrointestinal routes are used, possibly to avoid regurgitation as well as better retention rates [61,84]. On the other hand, this has also been suggested as a reason why some transplants fail [17]. Common concerns include degradation by the gastric milieu, aspiration, hemorrhage and perforation of the upper gastrointestinal system [68,85-87]. This was supported by Wang et al who demonstrated in a systematic review that the rate of adverse events was more common when upper compared to lower gastrointestinal routes were used (43.6% vs. 17.7%) [58].
The most recently developed mode of stool delivery is in the form of oral capsules [88,89]. It involves the delivery of stool mixed with a cryoprotectant, most commonly glycerol, and double- or triple-encapsulated to protect the stool from stomach acidity. Capsules are minimally invasive, convenient, and eliminate the risk of perforation by endoscopic procedures. Additionally, capsules are more esthetically pleasing, as patients have shown a preference for this mode of delivery over others [27,37].
Studies comparing the different routes of FMT have had mixed results, most likely due to sample size and research design [92]. Postigo et al compared the efficacy of upper and lower routes of delivery. Using a pooled analysis of 182 patients, the study did not show a significant difference between lower gastrointestinal and upper gastrointestinal delivery of FMT 95% (95% confidence interval [CI] 92-97%) vs. 88% (95%CI 82-94%), respectively (P=0.162) [93]. An observational follow-up study by Gundacker et al found that FMT by nasogastric tube (NGT) was less effective than colonoscopy [65]. Subgroup analysis revealed that NGT was equally effective for patients who were severely ill (Charleston comorbidity index [CCI]>5) or moderately ill (CCI<5), although there was a trend towards increasing effectiveness with colonoscopy for severely ill patients. However, a small randomized study of 20 patients by Youngster et al found colonoscopy and NGT to be equally successful [24]. A larger study by Kao et al involving 116 patients (57 patients randomized to the capsule group and 59 to the colonoscopy group) found that the use of capsules was non-inferior to colonoscopy [27]. The study showed that 96.2% of patients achieved prevention of recurrent CDI after a single treatment in both groups (capsule=51/53, colonoscopy=50/52; difference 0%; 1-sided 95%CI -6.1% to infinity; P<0.001). Evidence from these comparisons largely indicates that upper gastrointestinal methods of delivery can be equally effective as lower gastrointestinal methods. Furthermore, the high efficacy of FMT capsules, combined with their convenience, safety and esthetics, make them an attractive option for many patients.
Cost-effectiveness of FMT
CDI places a large burden on the healthcare system and makes it imperative to develop guidelines that emphasize cost-effective therapies [93-97]. A meta-analysis estimated the total financial burden of inpatient management of CDI in the United States to be $6.3 billion in 2015 [94]. In Europe, the economic burden of CDI was estimated to be roughly €3 billion [98], with costs per episode ranging between €5798 and €11,202 [97]. Given the effectiveness of FMT in the management of recurrent CDI, several studies have evaluated its cost-effectiveness [99-104].
The first cost-effective analysis compared three types of FMT (colonoscopy, duodenal infusion, and enema) and standard antibiotic therapy in the US. The analysis began with the first episode of recurrence and utilized contemporary guidelines to model two additional episodes of recurrence. At a willingness-to-pay threshold of $50,000/quality-adjusted life year (QALY), they found that FMT via colonoscopy was cost-effective compared to vancomycin and dominant (both cheaper and more effective) compared to the other therapies [99]. Of the several assumptions that went into the model, the choice to model FMT with only a single infusion of stool per treatment should be noted. If multiple infusions were permitted, the resolution rates for FMT via enema or duodenal infusion might have been higher (0.813 vs. 0.926 and 0.815 vs. 0.94, respectively), which may have significantly altered the conclusions of the study.
Two other cost-effectiveness analyses have led to mixed conclusions. A decision-analytic model involving Markov processes compared colonoscopy, enema, NGT and standard antibiotic therapy, beginning with the first recurrence of CDI. The analysis, from the perspective of the ministry of health in Ontario, Canada, concluded that FMT via colonoscopy dominated all other strategies. Sensitivity analysis revealed it to be dominant in 87% of simulations. FMT via enema was preferred if colonoscopy was not available [100]. Another decision-analytic model, from France, compared various methods of FMT (colonoscopy, duodenal infusion, enema), vancomycin and fidaxomicin, for the second recurrence of CDI. Using the WHO’s commission on macroeconomics and health to set the willingness-to-pay threshold at $32,000, they found FMT via enema to be highly cost-effective (incremental cost-effectiveness ratio [ICER] $18,092/QALY) compared to vancomycin. Although FMT via colonoscopy was still cost-effective according to WHO guidelines, it was not as cost-effective as FMT via enema (ICER $73,653/QALY) [101].
Other cost-effectiveness studies for recurrent CDI have limited their scope to comparing specific methods. One study compared FMT via colonoscopy to vancomycin for the third recurrence of CDI. They found that FMT dominated vancomycin unless the cure rate with vancomycin was greater than 90% or the costs of FMT exceeded $3,205 (2011 USD) [102]. Another study used Markov’s model to compare two methods of FMT (nasoduodenal infusion and colonoscopy) and vancomycin for the first recurrence of CDI. From the perspective of the healthcare system in Australia, the study found both methods of FMT to be dominant over vancomycin, with an estimated savings of over AU$1.37 million (2015 Australian dollars) per year. While no significant differences were reported between the various methods of FMT, the study did not incorporate the risks associated with nasoduodenal infusion into their model [103].
Additionally, a decision-analytic model by Varier et al compared FMT via colonoscopy to metronidazole and vancomycin, from the perspective of a third-party payer. Given the lack of published data on the effectiveness of FMT for initial CDI, the authors assumed that the procedure was as effective as it was for recurrent CDI [104]. At a willingness-to-pay threshold of $100,000 (2011 US dollars), the base case of FMT was not cost-effective when compared to metronidazole (ICER $124,964/QALY) but was dominant over vancomycin. FMT would have dominated metronidazole if the cost of the procedure was less than $584, the cost of metronidazole was over $559, or the cure rate with metronidazole was less than 71% [104]. Recently, a small RCT in Norway showed that, when FMT was used as primary therapy for CDI, overall response to treatment was achieved in 7 (n=9) patients in the FMT group (78%; 95%CI 40-97), compared with 5 (n=11) in the metronidazole group (45%; 95%CI 17-77) (P=0.20) [105]. However, the study did not show statistical significance. Longitudinal studies are needed to define the role of FMT in the management of primary CDI. Currently, it appears that FMT may not be a cost-effective strategy for initial cases of CDI.
Concluding remarks
FMT is an effective and robust strategy for treating recurrent CDI. Our narrative review has shown that the success of FMT does not depend on the donor-patient relationship. To this end, the use of unrelated donor stool is becoming widely accepted with the creation of stool banks. However, further studies are needed to clarify storage requirements and the optimal freezing time before declining microbial function and diversity. Furthermore, several FMT techniques are used in the process of fecal transplantation. Based upon current data, we believe colonoscopy to be the most effective strategy. However, capsule FMT offers patients a more convenient and esthetically pleasing option. Cost-effectiveness models comparing these various approaches support the use of fecal transplant using colonoscopy over antibiotic therapy for treating recurrent CDI. However, there remains a knowledge gap regarding the cost-effectiveness of capsule FMT.
Biography
The Brooklyn Hospital Center, Academic Affiliate of The Icahn School of Medicine at Mount Sinai, Clinical Affiliate of The Mount Sinai Hospital, Brooklyn; Elmhurst Medical Center, New York, USA
Footnotes
Conflict of Interest: None.
Financial Support: Supported by NIH 5 T32 DK 7356-37 (BN)
Funding: This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
References
- 1.Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections:a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173:2039–2046. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 2.Olsen MA, Yan Y, Reske KA, Zilberberg MD, Dubberke ER. Recurrent Clostridium difficile infection is associated with increased mortality. Clin Microbiol Infect. 2015;21:164–170. doi: 10.1016/j.cmi.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 3.Cohen SH, Gerding DN, Johnson S, et al. Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults:2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31:431–455. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 4.Kassam Z, Lee CH, Yuan Y, Hunt RH. Fecal microbiota transplantation for Clostridium difficile infection:systematic review and meta-analysis. Am J Gastroenterol. 2013;108:500–508. doi: 10.1038/ajg.2013.59. [DOI] [PubMed] [Google Scholar]
- 5.Lee CH, Steiner T, Petrof EO, et al. Frozen vs fresh fecal microbiota transplantation and clinical resolution of diarrhea in patients with recurrent Clostridium difficile infection:a randomized clinical trial. JAMA. 2016;315:142–149. doi: 10.1001/jama.2015.18098. [DOI] [PubMed] [Google Scholar]
- 6.Kernsten HH. Intentional replacement of bacteria following antibiotic therapy. J Iowa State Med Soc. 1958;48:240–243. [PubMed] [Google Scholar]
- 7.Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958;44:854–859. [PubMed] [Google Scholar]
- 8.Cutolo LC, Kleppel NH, Freund HR, Holker J. Fecal feedings as therapy in staphylococcus enterocolitis. N Y State J Med. 1959;59:3831–3833. [PubMed] [Google Scholar]
- 9.Bowden TA, Jr, Mansberger AR, Jr, Lykins LE. Pseudomembraneous enterocolitis:mechanism for restoring floral homeostasis. Am Surg. 1981;47:178–183. [PubMed] [Google Scholar]
- 10.Borody TJ. “Flora Power”—fecal bacteria cure chronic C. difficile diarrhea. Am J Gastroenterol. 2000;95:3028–3029. doi: 10.1111/j.1572-0241.2000.03277.x. [DOI] [PubMed] [Google Scholar]
- 11.Borody TJ, Warren EF, Leis SM, Surace R, Ashman O, Siarakas S. Bacteriotherapy using fecal flora:toying with human motions. J Clin Gastroenterol. 2004;38:475–483. doi: 10.1097/01.mcg.0000128988.13808.dc. [DOI] [PubMed] [Google Scholar]
- 12.Bakken JS. Fecal bacteriotherapy for recurrent Clostridium difficile infection. Anaerobe. 2009;15:285–289. doi: 10.1016/j.anaerobe.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Tasnim N, Abulizi N, Pither J, Hart MM, Gibson DL. Linking the gut microbial ecosystem with the environment:does gut health depend on where we live? Front Microbiol. 2017;8:1935. doi: 10.3389/fmicb.2017.01935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aas J, Gessert CE, Bakken JS. Recurrent Clostridium difficile colitis:case series involving 18 patients treated with donor stool administered via a nasogastric tube. Clin Infect Dis. 2003;36:580–585. doi: 10.1086/367657. [DOI] [PubMed] [Google Scholar]
- 15.Garborg K, Waagsbø B, Stallemo A, Matre J, Sundøy A. Results of faecal donor instillation therapy for recurrent Clostridium difficile-associated diarrhoea. Scand J Infect Dis. 2010;42:857–861. doi: 10.3109/00365548.2010.499541. [DOI] [PubMed] [Google Scholar]
- 16.van Nood E, Speelman P, Kuijper EJ, Keller JJ. Struggling with recurrent Clostridium difficile infections:is donor faeces the solution? Euro Surveill. 2009:14. doi: 10.2807/ese.14.34.19316-en. [DOI] [PubMed] [Google Scholar]
- 17.Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis. 2011;53:994–1002. doi: 10.1093/cid/cir632. [DOI] [PubMed] [Google Scholar]
- 18.Li YT, Cai HF, Wang ZH, Xu J, Fang JY. Systematic review with meta-analysis:long-term outcomes of faecal microbiota transplantation for Clostridium difficile infection. Aliment Pharmacol Ther. 2016;43:445–457. doi: 10.1111/apt.13492. [DOI] [PubMed] [Google Scholar]
- 19.Shin JH, Chaves-Olarte E, Warren CA. Clostridium difficile infection. Microbiol Spectr. 2016;4 doi: 10.1128/microbiolspec.EI10-0007-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terveer EM, van Beurden YH, Goorhuis A, et al. How to:Establish and run a stool bank. Clin Microbiol Infect. 2017;23:924–930. doi: 10.1016/j.cmi.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107:761–767. doi: 10.1038/ajg.2011.482. [DOI] [PubMed] [Google Scholar]
- 22.Satokari R, Mattila E, Kainulainen V, Arkkila PE. Simple faecal preparation and efficacy of frozen inoculum in faecal microbiota transplantation for recurrent Clostridium difficile infection—an observational cohort study. Aliment Pharmacol Ther. 2015;41:46–53. doi: 10.1111/apt.13009. [DOI] [PubMed] [Google Scholar]
- 23.van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 24.Youngster I, Sauk J, Pindar C, et al. Fecal microbiota transplant for relapsing Clostridium difficile infection using a frozen inoculum from unrelated donors:a randomized, open-label, controlled pilot study. Clin Infect Dis. 2014;58:1515–1522. doi: 10.1093/cid/ciu135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cammarota G, Masucci L, Ianiro G, et al. Randomised clinical trial:faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41:835–843. doi: 10.1111/apt.13144. [DOI] [PubMed] [Google Scholar]
- 26.Kelly CR, Khoruts A, Staley C, et al. Effect of fecal microbiota transplantation on recurrence in multiply recurrent Clostridium difficile infection:a randomized trial. Ann Intern Med. 2016;165:609–616. doi: 10.7326/M16-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kao D, Roach B, Silva M, et al. Effect of oral capsule- vs colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection:a randomized clinical trial. JAMA. 2017;318:1985–1993. doi: 10.1001/jama.2017.17077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang ZD, Ajami NJ, Petrosino JF, et al. Randomised clinical trial:faecal microbiota transplantation for recurrent Clostridium difficile infection fresh, or frozen, or lyophilised microbiota from a small pool of healthy donors delivered by colonoscopy. Aliment Pharmacol Ther. 2017;45:899–908. doi: 10.1111/apt.13969. [DOI] [PubMed] [Google Scholar]
- 29.Hota SS, Sales V, Tomlinson G, et al. Oral vancomycin followed by fecal transplantation versus tapering oral vancomycin treatment for recurrent Clostridium difficile infection:an open-label, randomized controlled trial. Clin Infect Dis. 2017;64:265–271. doi: 10.1093/cid/ciw731. [DOI] [PubMed] [Google Scholar]
- 30.Lee CH, Belanger JE, Kassam Z, et al. The outcome and long-term follow-up of 94 patients with recurrent and refractory Clostridium difficile infection using single to multiple fecal microbiota transplantation via retention enema. Eur J Clin Microbiol Infect Dis. 2014;33:1425–1428. doi: 10.1007/s10096-014-2088-9. [DOI] [PubMed] [Google Scholar]
- 31.Orenstein R, Dubberke E, Hardi R, et al. PUNCH CD Investigators. Safety and durability of RBX2660 (microbiota suspension) for recurrent Clostridium difficile infection:results of the PUNCH CD Study. Clin Infect Dis. 2016;62:596–602. doi: 10.1093/cid/civ938. [DOI] [PubMed] [Google Scholar]
- 32.Rubin TA, Gessert CE, Aas J, Bakken JS. Fecal microbiome transplantation for recurrent Clostridium difficile infection:report on a case series. Anaerobe. 2013;19:22–26. doi: 10.1016/j.anaerobe.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 33.Kelly CP. Fecal microbiota transplantation—an old therapy comes of age. N Engl J Med. 2013;368:474–475. doi: 10.1056/NEJMe1214816. [DOI] [PubMed] [Google Scholar]
- 34.Daloiso V, Minacori R, Refolo P, et al. Ethical aspects of fecal microbiota transplantation (FMT) Eur Rev Med Pharmacol Sci. 2015;19:3173–3180. [PubMed] [Google Scholar]
- 35.Hawkins AK, O'Doherty KC. “Who owns your poop?”:insights regarding the intersection of human microbiome research and the ELSI aspects of biobanking and related studies. BMC Med Genomics. 2011;4:72. doi: 10.1186/1755-8794-4-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zellmer C, De Wolfe TJ, Van Hoof S, Blakney R, Safdar N. Patient perspectives on fecal microbiota transplantation for Clostridium difficile infection. Infect Dis Ther. 2016;5:155–164. doi: 10.1007/s40121-016-0106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zipursky JS, Sidorsky TI, Freedman CA, Sidorsky MN, Kirkland KB. Patient attitudes toward the use of fecal microbiota transplantation in the treatment of recurrent Clostridium difficile infection. Clin Infect Dis. 2012;55:1652–1658. doi: 10.1093/cid/cis809. [DOI] [PubMed] [Google Scholar]
- 38.Park L, Mone A, Price JC, et al. Perceptions of fecal microbiota transplantation for Clostridium difficile infection:factors that predict acceptance. Ann Gastroenterol. 2017;30:83–88. doi: 10.20524/aog.2016.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pakyz AL, Moczygemba LR, VanderWielen LM, Edmond MB. Fecal microbiota transplantation for recurrent Clostridium difficile infection:The patient experience. Am J Infect Control. 2016;44:554–559. doi: 10.1016/j.ajic.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 40.Duplessis CA, You D, Johnson M, Speziale A. Efficacious outcome employing fecal bacteriotherapy in severe Crohn's colitis complicated by refractory Clostridium difficile infection. Infection. 2012;40:469–472. doi: 10.1007/s15010-011-0226-1. [DOI] [PubMed] [Google Scholar]
- 41.Wang ZK, Yang YS, Chen Y, Yuan J, Sun G, Peng LH. Intestinal microbiota pathogenesis and fecal microbiota transplantation for inflammatory bowel disease. World J Gastroenterol. 2014;20:14805–14820. doi: 10.3748/wjg.v20.i40.14805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cammarota G, Ianiro G, Tilg H, et al. European FMT Working Group. European consensus conference on faecal microbiota transplantation in clinical practice. Gut. 2017;66:569–580. doi: 10.1136/gutjnl-2016-313017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moayyedi P, Marshall JK, Yuan Y, Hunt R. Canadian Association of Gastroenterology position statement:fecal microbiota transplant therapy. Can J Gastroenterol Hepatol. 2014;28:66–68. doi: 10.1155/2014/346590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allen-Vercoe E, Reid G, Viner N, et al. A Canadian Working Group report on fecal microbial therapy:microbial ecosystems therapeutics. Can J Gastroenterol. 2012;26:457–462. doi: 10.1155/2012/213828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kelly CR, Kahn S, Kashyap P, et al. Update on fecal microbiota transplantation 2015:indications, methodologies, mechanisms, and outlook. Gastroenterology. 2015;149:223–237. doi: 10.1053/j.gastro.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Position Statement On Faecal Microbiota Transplant (FMT) [[Accessed May 19, 2018]]. http://www.gesa.org.au/public/13/files/GESA%20position%20statement%20FMT%20FAM%20JMA%20SPC%2020170426.pdf .
- 47.Gustafsson A, Lund-Tønnesen S, Berstad A, Midtvedt T, Norin E. Faecal short-chain fatty acids in patients with antibiotic-associated diarrhoea, before and after faecal enema treatment. Scand J Gastroenterol. 1998;33:721–727. doi: 10.1080/00365529850171666. [DOI] [PubMed] [Google Scholar]
- 48.Gustafsson A, Berstad A, Lund-Tønnesen S, Midtvedt T, Norin E. The effect of faecal enema on five microflora-associated characteristics in patients with antibiotic-associated diarrhoea. Scand J Gastroenterol. 1999;34:580–586. doi: 10.1080/003655299750026038. [DOI] [PubMed] [Google Scholar]
- 49.Tvede M, Rask-Madsen J. Bacteriotherapy for chronic relapsing Clostridium difficile diarrhoea in six patients. Lancet. 1989;1:1156–1160. doi: 10.1016/s0140-6736(89)92749-9. [DOI] [PubMed] [Google Scholar]
- 50.Youngster I, Mahabamunuge J, Systrom HK, et al. Oral, frozen fecal microbiota transplant (FMT) capsules for recurrent Clostridium difficile infection. BMC Med. 2016;14:134. doi: 10.1186/s12916-016-0680-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hirsch BE, Saraiya N, Poeth K, Schwartz RM, Epstein ME, Honig G. Effectiveness of fecal-derived microbiota transfer using orally administered capsules for recurrent Clostridium difficile infection. BMC Infect Dis. 2015;15:191. doi: 10.1186/s12879-015-0930-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Costello SP, Conlon MA, Vuaran MS, Roberts-Thomson IC, Andrews JM. Faecal microbiota transplant for recurrent Clostridium difficile infection using long-term frozen stool is effective:clinical efficacy and bacterial viability data. Aliment Pharmacol Ther. 2015;42:1011–1018. doi: 10.1111/apt.13366. [DOI] [PubMed] [Google Scholar]
- 53.Lahtinen P, Mattila E, Anttila VJ, et al. Faecal microbiota transplantation in patients with Clostridium difficile and significant comorbidities as well as in patients with new indications:A case series. World J Gastroenterol. 2017;23:7174–7184. doi: 10.3748/wjg.v23.i39.7174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Staley C, Hamilton MJ, Vaughn BP, et al. Successful resolution of recurrent Clostridium difficile infection using freeze-dried, encapsulated fecal microbiota;pragmatic cohort study. Am J Gastroenterol. 2017;112:940–947. doi: 10.1038/ajg.2017.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weingarden AR, Hamilton MJ, Sadowsky MJ, Khoruts A. Resolution of severe Clostridium difficile infection following sequential fecal microbiota transplantation. Clin Gastroenterol. 2013;47:735–737. doi: 10.1097/MCG.0b013e31829004ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Camacho-Ortiz A, Gutiérrez-Delgado EM, Garcia-Mazcorro JF, et al. Randomized clinical trial to evaluate the effect of fecal microbiota transplant for initial Clostridium difficile infection in intestinal microbiome. PLoS One. 2017;12:e0189768. doi: 10.1371/journal.pone.0189768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jiang ZD, Alexander A, Ke S, et al. Stability and efficacy of frozen and lyophilized fecal microbiota transplant (FMT) product in a mouse model of Clostridium difficile infection (CDI) Anaerobe. 2017;48:110–114. doi: 10.1016/j.anaerobe.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 58.Wang S, Xu M, Wang W, et al. Systematic review:adverse events of fecal microbiota transplantation. PLoS One. 2016;11:e0161174. doi: 10.1371/journal.pone.0161174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tian H, Ding C, Gong J, Wei Y, McFarland LV, Li N. Freeze-dried, capsulized fecal microbiota transplantation for relapsing Clostridium difficile infection. J Clin Gastroenterol. 2015;49:537–538. doi: 10.1097/MCG.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 60.Hecker MT, Obrenovich ME, Cadnum JL, et al. Fecal microbiota transplantation by freeze-dried oral capsules for recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3:ofw091. doi: 10.1093/ofid/ofw091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gweon TG, Kim J, Lim CH, et al. Fecal microbiota transplantation using upper gastrointestinal tract for the treatment of refractory or severe complicated Clostridium difficile infection in elderly patients in poor medical condition:the first study in an Asian country. Gastroenterol Res Pract. 2016;2016:2687605. doi: 10.1155/2016/2687605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bauer MP, van Dissel JT. Alternative strategies for Clostridium difficile infection. Int J Antimicrob Agents. 2009;33(Suppl 1):S51–S56. doi: 10.1016/S0924-8579(09)70018-4. [DOI] [PubMed] [Google Scholar]
- 63.Link A, Lachmund T, Schulz C, Weigt J, Malfertheiner P. Endoscopic peroral jejunal fecal microbiota transplantation. Dig Liver Dis. 2016;48:1336–1339. doi: 10.1016/j.dld.2016.08.110. [DOI] [PubMed] [Google Scholar]
- 64.Trubiano JA, Gardiner B, Kwong JC, Ward P, Testro AG, Charles PG. Faecal microbiota transplantation for severe Clostridium difficile infection in the intensive care unit. Eur J Gastroenterol Hepatol. 2013;25:255–257. doi: 10.1097/MEG.0b013e32835b2da9. [DOI] [PubMed] [Google Scholar]
- 65.Gundacker ND, Tamhane A, Walker JB, Morrow CD, Rodriguez JM. Comparative effectiveness of faecal microbiota transplant by route of administration. J Hosp Infect. 2017;96:349–352. doi: 10.1016/j.jhin.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 66.Louie TJ, Louie MR, Krulicki W, Byrne B, Ward L. Abstracts of the Interscience Conference on Antimicrobial Agents & Chemotherapy (Washington DC) Arlington, Virginia: Infectious Disease Society of America; 2008. Home-based fecal flora infusion to arrest multiply-recurrent Clostridium difficile infection (CDI) [Google Scholar]
- 67.Schneider KM, Wirtz TH, Kroy D, et al. Successful fecal microbiota transplantation in a patient with severe complicated Clostridium difficile infection after liver transplantation. Case Rep Gasroenterol. 2018;12:76–84. doi: 10.1159/000481937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mattila E, Uusitalo-Seppälä R, Wuorela M, et al. Fecal transplantation, through colonoscopy, is effective therapy for recurrent Clostridium difficile infection. Gastroenterology. 2012;142:490–496. doi: 10.1053/j.gastro.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 69.Pathak R, Enuh HA, Patel A, Wickremesinghe P. Treatment of relapsing Clostridium difficile infection using fecal microbiota transplantation. Clin Exp Gastroenterol. 2013;7:1–6. doi: 10.2147/CEG.S53410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cammarota G, Ianiro G, Gasbarrini A. Fecal microbiota transplantation for the treatment of Clostridium difficile infection:a systematic review. J Clin Gastroenterol. 2014;48:693–702. doi: 10.1097/MCG.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 71.Kelly CR, de Leon L, Jasutkar N. Fecal microbiota transplantation for relapsing Clostridium difficile infection in 26 patients:methodology and results. J Clin Gastroenterol. 2012;46:145–149. doi: 10.1097/MCG.0b013e318234570b. [DOI] [PubMed] [Google Scholar]
- 72.Persky SE, Brandt LJ. Treatment of recurrent Clostridium difficile-associated diarrhea by administration of donated stool directly through a colonoscope. Am J Gastroenterol. 2000;95:3283–3285. doi: 10.1111/j.1572-0241.2000.03302.x. [DOI] [PubMed] [Google Scholar]
- 73.Rohlke F, Surawicz CM, Stollman N. Fecal flora reconstitution for recurrent Clostridium difficile infection:results and methodology. J Clin Gastroenterol. 2010;44:567–570. doi: 10.1097/MCG.0b013e3181dadb10. [DOI] [PubMed] [Google Scholar]
- 74.Yoon SS, Brandt LJ. Treatment of refractory/recurrent C. difficile-associated disease by donated stool transplanted via colonoscopy:a case series of 12 patients. J Clin Gastroenterol. 2010;44:562–566. doi: 10.1097/MCG.0b013e3181dac035. [DOI] [PubMed] [Google Scholar]
- 75.Guo B, Harstall C, Louie T, Veldhuyzen van Zanten S, Dieleman LA. Systematic review:faecal transplantation for the treatment of Clostridium difficile-associated disease. Aliment Pharmacol Ther. 2012;35:865–875. doi: 10.1111/j.1365-2036.2012.05033.x. [DOI] [PubMed] [Google Scholar]
- 76.Brandt LJ, Borody TJ, Campbell J. Endoscopic fecal microbiota transplantation:“first-line” treatment for severe Clostridium difficile infection? J Clin Gastroenterol. 2011;45:655–657. doi: 10.1097/MCG.0b013e3182257d4f. [DOI] [PubMed] [Google Scholar]
- 77.Ehlermann P, Dösch AO, Katus HA. Donor fecal transfer for recurrent Clostridium difficile-associated diarrhea in heart transplantation. J Heart Lung Transplant. 2014;33:551–553. doi: 10.1016/j.healun.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 78.Zainah H, Hassan M, Shiekh-Sroujieh L, Hassan S, Alangaden G, Ramesh M. Intestinal microbiota transplantation, a simple and effective treatment for severe and refractory Clostridium difficile infection. Dig Dis Sci. 2015;60:181–185. doi: 10.1007/s10620-014-3296-y. [DOI] [PubMed] [Google Scholar]
- 79.Kelly CR, Ihunnah C, Fischer M, et al. Fecal microbiota transplant for treatment of Clostridium difficile infection in immunocompromised patients. Am J Gastroenterol. 2014;109:1065–1071. doi: 10.1038/ajg.2014.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kassam Z, Hundal R, Marshall JK, Lee CH. Fecal transplant via retention enema for refractory or recurrent Clostridium difficile infection. Arch Intern Med. 2012;172:191–193. doi: 10.1001/archinte.172.2.191. [DOI] [PubMed] [Google Scholar]
- 81.Silverman MS, Davis I, Pillai DR. Success of self-administered home fecal transplantation for chronic Clostridium difficile infection. Clin Gastroenterol Hepatol. 2010;8:471–473. doi: 10.1016/j.cgh.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 82.Duke PS, Fardy J. Recurrent Clostridium difficile infection treated with home fecal transplantation:a case report. J Med Case Rep. 2014;28:393. doi: 10.1186/1752-1947-8-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brandt LJ, Aroniadis OC, Mellow M, et al. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107:1079–1087. doi: 10.1038/ajg.2012.60. [DOI] [PubMed] [Google Scholar]
- 84.Bang BW, Park JS, Kim HK, et al. Fecal microbiota transplantation for refractory and recurrent Clostridium difficile infection:a case series of nine patients. Korean J Gastroenterol. 2017;69:226–231. doi: 10.4166/kjg.2017.69.4.226. [DOI] [PubMed] [Google Scholar]
- 85.Dutta SK, Girotra M, Garg S, et al. Efficacy of combined jejunal and colonic fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol. 2014;12:1572–1576. doi: 10.1016/j.cgh.2013.12.032. [DOI] [PubMed] [Google Scholar]
- 86.Baxter M, Ahmad T, Colville A, Sheridan R. Fatal aspiration pneumonia as a complication of fecal microbiota transplant. Clin Infect Dis. 2015;61:136–137. doi: 10.1093/cid/civ247. [DOI] [PubMed] [Google Scholar]
- 87.Hagel S, Fischer A, Ehlermann P, et al. German Clinical Microbiome Study Group (GCMSG) Fecal microbiota transplant in patients with recurrent Clostridium difficile infection. Dtsch Arztebl Int. 2016;113:583–589. doi: 10.3238/arztebl.2016.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Louie T, Cannon K, O'Grady H, et al. Fecal microbiome transplantation (FMT) via oral fecal microbial capsules for recurrent Clostridium difficile infection (rCDI) ID week. 2013:201389. [Google Scholar]
- 89.Rao K, Young VB, Malani PN. Capsules for fecal microbiota transplantation in recurrent Clostridium difficile infection:the new way forward or a tough pill to swallow? JAMA. 2017;318:1979–1980. doi: 10.1001/jama.2017.17969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Youngster I, Russell GH, Pindar C, Ziv-Baran T, Sauk J, Hohmann EL. Oral, capsulized, frozen fecal microbiota transplantation for relapsing Clostridium difficile infection. JAMA. 2014;312:1772–1778. doi: 10.1001/jama.2014.13875. [DOI] [PubMed] [Google Scholar]
- 91.Quraishi MN, Widlak M, Bhala N, et al. Systematic review with meta-analysis:the efficacy of faecal microbiota transplantation for the treatment of recurrent and refractory Clostridium difficile infection. Aliment Pharmacol Ther. 2017;46:479–493. doi: 10.1111/apt.14201. [DOI] [PubMed] [Google Scholar]
- 92.Postigo R, Kim JH. Colonoscopic versus nasogastric fecal transplantation for the treatment of Clostridium difficile infection:a review and pooled analysis. Infection. 2012;40:643–648. doi: 10.1007/s15010-012-0307-9. [DOI] [PubMed] [Google Scholar]
- 93.Bauer MP, Notermans DW, van Benthem BH, et al. ECDIS Study Group. Clostridium difficile infection in Europe:a hospital-based survey. Lancet. 2011;377:63–73. doi: 10.1016/S0140-6736(10)61266-4. [DOI] [PubMed] [Google Scholar]
- 94.Zhang S, Palazuelos-Munoz S, Balsells EM, Nair H, Chit A, Kyaw MH. Cost of hospital management of Clostridium difficile infection in United States-a meta-analysis and modelling study. BMC Infect Dis. 2016;16:447. doi: 10.1186/s12879-016-1786-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Borren NZ, Ghadermarzi S, Hutfless S, Ananthakrishnan AN. The emergence of Clostridium difficile infection in Asia:A systematic review and meta-analysis of incidence and impact. PLoS One. 2017;12:e0176797. doi: 10.1371/journal.pone.0176797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Roldan GA, Cui AX, Pollock NR. Assessing the burden of Clostridium difficile infection in low- and middle-income countries. J Clin Microbiol. 2018:56. doi: 10.1128/JCM.01747-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Reigadas Ramírez E, Bouza E.S. Economic burden of Clostridium difficile infection in European countries. In: Mastrantonio P, Rupnik M, editors. Updates on Clostridium difficile in Europe. Advances in Experimental Medicine and Biology. Vol. 1050. Cham: Springer; 2018. pp. 1–12. [DOI] [PubMed] [Google Scholar]
- 98.Jones AM, Kuijper EJ, Wilcox MH. Clostridium difficile:a European perspective. J Infect. 2013;66:115–128. doi: 10.1016/j.jinf.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 99.Konijeti GG, Sauk J, Shrime MG, Gupta M, Ananthakrishnan AN. Cost-effectiveness of competing strategies for management of recurrent Clostridium difficile infection:a decision analysis. Clin Infect Dis. 2014;58:1507–1514. doi: 10.1093/cid/ciu128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lapointe-Shaw L, Tran KL, Coyte PC, et al. Cost-effectiveness analysis of six strategies to treat recurrent Clostridium difficile infection. PLoS One. 2016;11:e0149521. doi: 10.1371/journal.pone.0149521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Baro E, Galperine T, Denies F, et al. Cost-effectiveness analysis of five competing strategies for the management of multiple recurrent community-onset Clostridium difficile infection in France. PLoS One. 2017;12:e0170258. doi: 10.1371/journal.pone.0170258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Varier RU, Biltaji E, Smith KJ, et al. Cost-effectiveness analysis of fecal microbiota transplantation for recurrent Clostridium difficile infection. Infect Control Hosp Epidemiol. 2015;36:438–444. doi: 10.1017/ice.2014.80. [DOI] [PubMed] [Google Scholar]
- 103.Merlo G, Graves N, Brain D, Connelly LB. Economic evaluation of fecal microbiota transplantation for the treatment of recurrent Clostridium difficile infection in Australia. J Gastroenterol Hepatol. 2016;31:1927–1932. doi: 10.1111/jgh.13402. [DOI] [PubMed] [Google Scholar]
- 104.Varier RU, Biltaji E, Smith KJ, et al. Cost-effectiveness analysis of treatment strategies for initial Clostridium difficile infection. Clin Microbiol Infect. 2014;20:1343–1351. doi: 10.1111/1469-0691.12805. [DOI] [PubMed] [Google Scholar]
- 105.Juul FE, Garborg K, Bretthauer M, et al. Fecal microbiota transplantation for primary Clostridium difficile infection. N Engl J Med. 2018;378:2535–2536. doi: 10.1056/NEJMc1803103. [DOI] [PubMed] [Google Scholar]


