Abstract
Background and objectives
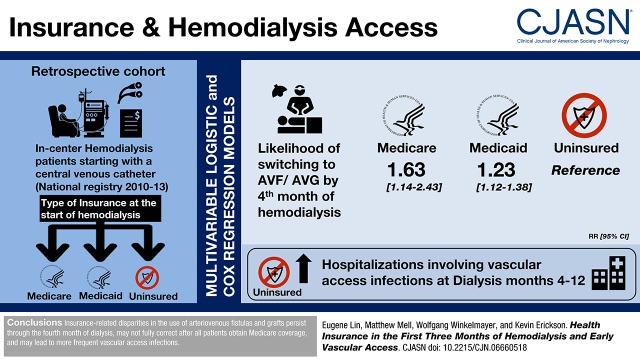
Patients without Medicare who develop ESKD in the United States become Medicare eligible by their fourth dialysis month. Patients without insurance may experience delays in obtaining arteriovenous fistulas or grafts before obtaining Medicare coverage.
Design, setting, participants, & measurements
In this retrospective cohort study, we used a national registry to compare uninsured patients starting in-center hemodialysis with a central venous catheter between 2010 and 2013 with similar patients with Medicare or Medicaid. We evaluated whether insurance status at dialysis start influenced the likelihoods of switching to dialysis through an arteriovenous fistula or graft and hospitalizations involving a vascular access infection. We used multivariable logistic and Cox regression models and transformed odds ratios to relative risks using marginal effects.
Results
Patients with Medicare or Medicaid were more likely to switch to an arteriovenous fistula or graft by their fourth dialysis month versus uninsured patients (Medicare hazard ratio, 1.63; 95% confidence interval, 1.14 to 2.43; Medicaid hazard ratio, 1.23; 95% confidence interval, 1.12 to 1.38). There were no differences in rates of switching to arteriovenous fistulas or grafts after all patients obtained Medicare in their fourth dialysis month (Medicare hazard ratio, 1.17; 95% confidence interval, 0.97 to 1.42; Medicaid hazard ratio, 1.01; 95% confidence interval, 0.96 to 1.06). Patients with Medicare at dialysis start had fewer hospitalizations involving vascular access infection in dialysis months 4–12 (hazard ratio, 0.60; 95% confidence interval, 0.37 to 0.97).
Conclusions
Insurance-related disparities in the use of arteriovenous fistulas and grafts persist through the fourth month of dialysis, may not fully correct after all patients obtain Medicare coverage, and may lead to more frequent vascular access infections.
Keywords: clinical epidemiology; Economic Impact; hemodialysis access; United States Renal Data System; renal dialysis; Medicaid; Central Venous Catheters; Odds Ratio; Medically Uninsured; Risk; Retrospective Studies; Kidney Failure, Chronic; Medicare; Insurance Coverage; Insurance, Health; arteriovenous fistula; hospitalization; Registries
Visual Abstract
Introduction
More than 700,000 adults in the United States have ESKD, which is associated with high morbidity, mortality, and health care costs (1). Most patients with ESKD receive hemodialysis, which can be administered through an arteriovenous fistula (AVF), an arteriovenous graft (AVG), or a central venous catheter. Patients using an AVF or AVG are substantially less likely to be hospitalized for life-threatening infections (2–5) and experience improved survival compared with those using a central venous catheter (6–12).
National efforts to increase AVF use, including the Fistula First Initiative (13,14), led to substantial increases in AVF use. By 2014, >60% of United States patients on prevalent hemodialysis received dialysis through an AVF (15), a rate comparable with that in other developed countries (16). However, only 20% of United States patients initiate dialysis with an AVF or AVG, a lower proportion than in other developed countries (16,17). Lack of health insurance is an important barrier to early AVF or AVG use. Between 12% and 20% of United States adults <65 years old at the onset of ESKD are uninsured, and these patients are less likely to initiate dialysis with an AVF or AVG (1,17).
Patients without Medicare at the start of ESKD must wait 3 months before they become eligible for Medicare on the basis of having ESKD. Because nearly all United States patients qualify for Medicare by the first day of their fourth dialysis month regardless of age (18), most patients can receive outpatient dialysis, regardless of their health insurance, before developing ESKD. However, it is unknown whether this 3-month delay prolongs insurance-related disparities in AVF and AVG use. We examine whether uninsured patients at the start of dialysis experience persistent delays in AVF and AVG use.
Materials and Methods
Data Sources and Patient Selection
Data came from the US Renal Data System, a registry of all patients with Medicare Parts A and B and ESKD, the 2010 Census, and the 2012 American Community Survey.
We selected patients starting in-center hemodialysis with a central venous catheter between July 1, 2010 and July 30, 2013. We limited our analysis to patients with Medicare Parts A and B by the fourth month of dialysis, because we relied on Medicare claims to identify outcomes. We excluded patients who died, recovered kidney function, changed to home dialysis, or received a kidney transplant in the first 120 days of dialysis.
Patients’ health insurance before dialysis can affect their access to pre-ESKD nephrology care (19), which may increase the early placement of AVFs and AVGs. The focus of our study was on the effect that insurance has on AVF and AVG use after ESKD onset. Consequently, we excluded from our primary analyses patients with pre-ESKD nephrology care, for whom it is impossible to determine whether differences in early vascular access use reflect the effect of insurance before or after the onset of ESKD.
Comparison Groups and Study Exposure
We estimated the effect of insurance in the first 3 months of hemodialysis on the likelihood of switching to AVFs and AVGs by identifying two control groups that were similar to uninsured patients at ESKD onset (Figure 1). We first compared uninsured patients with patients with Medicare at dialysis start. Patients who have Medicare coverage at dialysis initiation are usually 65 years of age or older. To reduce bias due to age differences, we required that patients with Medicare were 65–69 years old and that uninsured patients were 60–64 years old.
Figure 1.
Cohort selection from the United States Renal Data System. AVF, arteriovenous fistula; AVG, arteriovenous grant; HD, hemodialysis; US, United States.
A second analysis compared uninsured adults with those with Medicaid only at dialysis initiation. We excluded adults >65 years old, because <1% of patients in these groups were 65 years old or older. An advantage of this comparison is that patients were similar socioeconomically.
Study Outcomes
We had two primary outcomes. First, we studied the likelihood of AVF or AVG use using V codes on claims (20) (Supplemental Material) by the end of a patient’s fourth month of hemodialysis, which is when Medicare claims appear for all patients in the cohort. Second, in patients still using a central venous catheter at the end of the fourth month, we examined the time to AVF or AVG use in the first year of dialysis.
We had three secondary outcomes. First, we examined time to first hospitalization involving a vascular access infection beginning in patients’ fourth dialysis month, when all patients generated Medicare claims. Second, as a negative control, we analyzed time to first hospitalization with any infection (Supplemental Material). We used a previously described algorithm to isolate inpatient stays (21). Third, we examined the likelihood of using an AVF or AVG in the first year of dialysis.
Covariates
We controlled for sex, race, ethnicity, employment status, comorbid conditions, body mass index, albumin, and hemoglobin at dialysis start; dialysis facility characteristics; calendar year; season of dialysis start; population density; and local socioeconomics (listed in Tables 1 and 2). We used chained equations (ten imputations) to multiply impute missing values for serum albumin, hemoglobin, and body mass index (Supplemental Material has technical details, Tables 1 and 2 show the extent of missing data) (22).
Table 1.
Baseline characteristics of patients with Medicare versus no insurance at the start of dialysis ages 60–69 years old
| Characteristic | No Insurance at Day 1, n=907 | Medicare at Day 1, n=4388 | ||
|---|---|---|---|---|
| N or Mean | Percent or SD | N or Mean | Percent or SD | |
| Age, yra | 62 | 1.4 | 67 | 1.4 |
| Sex | ||||
| Women | 420 | 46% | 2037 | 46% |
| Men | 487 | 54% | 2351 | 54% |
| Race | ||||
| White | 611 | 67% | 3090 | 70% |
| Black | 249 | 28% | 1126 | 26% |
| Otherb | 47 | 5% | 172 | 4% |
| Ethnicity | ||||
| Hispanica,c | 237 | 26% | 598 | 14% |
| Employeda,d | 74 | 8% | 165 | 4% |
| Dual eligible | 0 | 0% | 1225 | 28% |
| BMI, kg/m2a,e | ||||
| <18.5 | 31 | 3% | 167 | 4% |
| 18.5 to <30 | 562 | 62% | 2368 | 54% |
| 30 to <40 | 243 | 27% | 1321 | 30% |
| ≥40 | 65 | 7% | 499 | 12% |
| Albumin, g/dle | ||||
| <2.5 | 153 | 23% | 665 | 21% |
| 2.5 to <3 | 163 | 25% | 832 | 26% |
| 3 to <3.5 | 172 | 26% | 871 | 28% |
| ≥3.5 | 167 | 26% | 787 | 25% |
| Hemoglobin category, g/dla,e | ||||
| <8 | 170 | 22% | 568 | 15% |
| 8 to <9 | 205 | 26% | 912 | 24% |
| 9 to <11 | 296 | 37% | 1793 | 47% |
| ≥11 | 120 | 15% | 575 | 15% |
| Comorbidities | ||||
| Coronary artery diseasea | 109 | 12% | 988 | 23% |
| Congestive heart failurea | 233 | 26% | 1614 | 37% |
| Cancera | 34 | 4% | 418 | 10% |
| Hypertension | 803 | 89% | 3805 | 87% |
| Chronic obstructive pulmonary diseasea | 65 | 7% | 664 | 15% |
| Diabetes mellitusf | 500 | 55% | 2688 | 61% |
| Peripheral vascular diseasea | 76 | 8% | 701 | 16% |
| Prior strokea | 69 | 8% | 535 | 12% |
| Drug dependence | 31 | 3% | 104 | 2% |
| Smokerf | 91 | 10% | 328 | 8% |
| Patient institutionalizeda | 26 | 3% | 583 | 13% |
| Needs assistance with ADLs and/or inability to transfera | 77 | 9% | 875 | 20% |
| Facility characteristics | ||||
| Large dialysis organizationf | 560 | 62% | 2865 | 65% |
| Facility is for profitf | 737 | 81% | 3716 | 85% |
| Facility is hospital basedf | 105 | 12% | 392 | 9% |
| Total facility patients per yearf | ||||
| 0–50 | 163 | 18% | 926 | 21% |
| 51–100 | 387 | 43% | 1949 | 44% |
| 101–150 | 216 | 24% | 945 | 22% |
| >150 | 141 | 16% | 568 | 13% |
| Full-time patient-to-nurse/technician ratio | ||||
| <7 | 473 | 52% | 2396 | 55% |
| ≥7 | 434 | 48% | 1992 | 45% |
| Residence characteristics | ||||
| Urbana | 675 | 74% | 2948 | 67% |
| Poverty in zip code,f % | ||||
| <15 | 339 | 37% | 1910 | 44% |
| 15 to <25 | 314 | 35% | 1451 | 33% |
| ≥25 | 254 | 28% | 1027 | 23% |
| Less than high school education in zip code,a % | ||||
| <15 | 346 | 38% | 2016 | 46% |
| 15 to <30 | 391 | 43% | 1808 | 41% |
| ≥30 | 170 | 19% | 564 | 13% |
| Year of dialysis start | ||||
| 2010 | 162 | 18% | 737 | 17% |
| 2011 | 301 | 33% | 1475 | 34% |
| 2012 | 290 | 32% | 1395 | 32% |
| 2013 | 154 | 17% | 781 | 18% |
| Season of dialysis start | ||||
| Winter | 256 | 28% | 1175 | 27% |
| Spring | 210 | 23% | 1027 | 23% |
| Summer | 235 | 26% | 1174 | 27% |
| Fall | 206 | 23% | 1012 | 23% |
BMI, body mass index; ADL, Activities of Daily Living.
P<0.001.
Other race includes Asian, Native American, Pacific Islander, and people with unknown or missing race.
Hispanic ethnicity was determined using the Centers for Medicare and Medicaid Services-2728 (CMS-2728) form.
Employment status was determined using the CMS-2728 form, and it included full-time and part-time employment. Patients who were retired, students, and homemakers were categorized as not employed.
The following variables had missing values: body mass index (n=39, 1% missing), serum albumin (n=1485, 28% missing), and hemoglobin concentration (n=656, 12% missing).
P<0.05.
Table 2.
Baseline characteristics of patients with Medicaid versus no insurance at the start of dialysis
| Characteristic | No Insurance at Day 1, n=6358 | Medicaid at Day 1, n=4322 | ||
|---|---|---|---|---|
| N or Mean | Percent or SD | N or Mean | Percent or SD | |
| Age, yra | 48 | 11 | 48 | 11 |
| Sexb | ||||
| Women | 2105 | 33% | 1878 | 44% |
| Men | 4253 | 67% | 2444 | 57% |
| Raceb | ||||
| White | 3571 | 56% | 2396 | 55% |
| Black | 2518 | 40% | 1649 | 38% |
| Otherc | 269 | 4% | 277 | 6% |
| Ethnicity | ||||
| Hispanicd | 1521 | 24% | 1039 | 24% |
| Employedb,e | 1021 | 16% | 374 | 9% |
| BMI, kg/m2f | ||||
| <18.5 | 189 | 3% | 126 | 3% |
| 18.5 to <30 | 3607 | 57% | 2410 | 56% |
| 30 to <40 | 1831 | 29% | 1222 | 29% |
| ≥40 | 677 | 11% | 523 | 12% |
| Albumin, g/dla,f | ||||
| <2.5 | 1072 | 23% | 797 | 26% |
| 2.5 to <3 | 1170 | 26% | 761 | 25% |
| 3 to <3.5 | 1202 | 26% | 724 | 23% |
| ≥3.5 | 1133 | 25% | 807 | 26% |
| Hemoglobin category, g/dlb,f | ||||
| <8 | 1363 | 25% | 769 | 20% |
| 8 to <9 | 1356 | 24% | 874 | 23% |
| 9 to <11 | 2086 | 38% | 1598 | 42% |
| ≥11 | 744 | 13% | 548 | 15% |
| Comorbidities | ||||
| Coronary artery diseaseb | 424 | 7% | 420 | 10% |
| Congestive heart failureb | 1280 | 20% | 1107 | 26% |
| Cancerb | 121 | 2% | 132 | 3% |
| Hypertensiona | 5614 | 88% | 3721 | 86% |
| Chronic obstructive pulmonary diseaseb | 231 | 4% | 286 | 7% |
| Diabetes mellitusb | 2894 | 46% | 2366 | 55% |
| Peripheral vascular diseaseb | 323 | 5% | 382 | 9% |
| Prior strokeb | 277 | 4% | 308 | 7% |
| Drug dependencea | 401 | 6% | 340 | 8% |
| Smoker | 785 | 12% | 510 | 12% |
| Patient institutionalizedb | 95 | 2% | 246 | 6% |
| Needs assistance with ADLs and/or inability to transferb | 303 | 5% | 483 | 11% |
| Facility characteristics | ||||
| Large dialysis organization | 4172 | 66% | 2869 | 66% |
| Facility is for profita | 5331 | 84% | 3693 | 85% |
| Facility is hospital basedb | 625 | 10% | 291 | 7% |
| Total facility patients per yearb | ||||
| 0–50 | 1114 | 18% | 693 | 16% |
| 51–100 | 2726 | 43% | 1708 | 40% |
| 101–150 | 1509 | 24% | 1124 | 26% |
| >150 | 1009 | 16% | 797 | 18% |
| Full-time patient-to-nurse/technician ratiob | ||||
| <7 | 3368 | 53% | 2089 | 48% |
| ≥7 | 2990 | 47% | 2233 | 52% |
| Residence characteristics | ||||
| Urban | 4762 | 75% | 3234 | 75% |
| Poverty in zip code,b % | ||||
| <15 | 2143 | 34% | 1274 | 30% |
| 15 to <25 | 2244 | 35% | 1603 | 37% |
| ≥25 | 1971 | 31% | 1445 | 33% |
| Less than high school education in zip code,b % | ||||
| <15 | 2354 | 37% | 1450 | 34% |
| 15 to <30 | 2869 | 45% | 1985 | 46% |
| ≥30 | 1135 | 18% | 887 | 21% |
| Year of dialysis start | ||||
| 2010 | 1127 | 18% | 770 | 18% |
| 2011 | 2223 | 35% | 1430 | 33% |
| 2012 | 1852 | 29% | 1358 | 31% |
| 2013 | 1156 | 18% | 764 | 18% |
| Season of dialysis starta | ||||
| Winter | 1773 | 28% | 1126 | 26% |
| Spring | 1511 | 24% | 1132 | 26% |
| Summer | 1532 | 24% | 1033 | 24% |
| Fall | 1542 | 24% | 1031 | 24% |
BMI, body mass index; ADL, Activities of Daily Living.
P<0.05.
P<0.001.
Other race includes Asian, Native American, Pacific Islander, and people with unknown or missing race.
Hispanic ethnicity was determined using the Centers for Medicare and Medicaid Services-2728 (CMS-2728) form.
Employment status was determined using the CMS-2728 form and included full-time and part-time employment. Patients who were retired, students, and homemakers were categorized as not employed.
The following variables had missing values: body mass index (n=95, 1% missing), serum albumin (n=3014, 28% missing), and hemoglobin concentration (n=1342, 13% missing).
Statistical Analyses
We used multivariable logistic regression to examine the associations between insurance and vascular access use at the end of dialysis month 4. To estimate the relative risk (RR) of AVF/AVG use associated with insurance, we calculated predicted probabilities from regression results with nonparametric bootstrapped 95% confidence intervals (95% CIs) (Supplemental Material has technical details).
We used multivariable Cox regression to study the association between insurance and time to the following events in dialysis months 4–12: switching to AVF or AVG use among patients using a catheter at month 4, hospitalization involving a vascular access infection, and hospitalization for any infection. We censored patients for death, change in dialysis modality, transplantation, loss of Medicare, or 3 consecutive months with no reported vascular access on claims. In the Medicare versus uninsured population, we censored 42% and 41% of patients, respectively. In the Medicaid versus uninsured population, we censored 37% and 35% of patients, respectively.
We combined the above logistic regression model with an exponential survival model to examine differences in AVF/AVG use through the first year of dialysis. This involved calculating the conditional probabilities of using a catheter at months 4 and 12 and multiplying the probabilities to estimate the 12-month probability of using a catheter. We used nonparametric bootstrapped 95% CIs. In all multivariable analyses, we controlled for the covariates described above (listed in Tables 1 and 2).
In sensitivity analyses, we tested the robustness of our primary results to a complete patient analysis, treating death as a competing risk (as opposed to a censoring event), including the likelihood of using an AVF/AVG at 6 months instead of 4 months (to account for longer AVF maturation times), and including patients with pre-ESKD nephrology care.
Results
Baseline Characteristics
The analysis comparing patients 65–69 years old with Medicare with uninsured patients 60–64 years old contained 5295 patients. The analysis comparing patients <65 years old with Medicaid with uninsured patients included 10,680 patients (Figure 1).
Tables 1 and 2 illustrate the baseline characteristics stratified by insurance. Compared with uninsured patients 60–64 years old, patients 65–69 years old with Medicare were less likely to be Hispanic and more likely to have higher hemoglobin, be unemployed, live in more affluent counties, and have more comorbidities.
Compared with uninsured patients <65 years old, patients with Medicaid were more likely to be women, be unemployed, live in poorer counties, have higher starting hemoglobin, have lower serum albumin, and have more comorbidities (Supplemental Tables 1 and 2).
Primary Outcomes
Medicare Versus Uninsured.
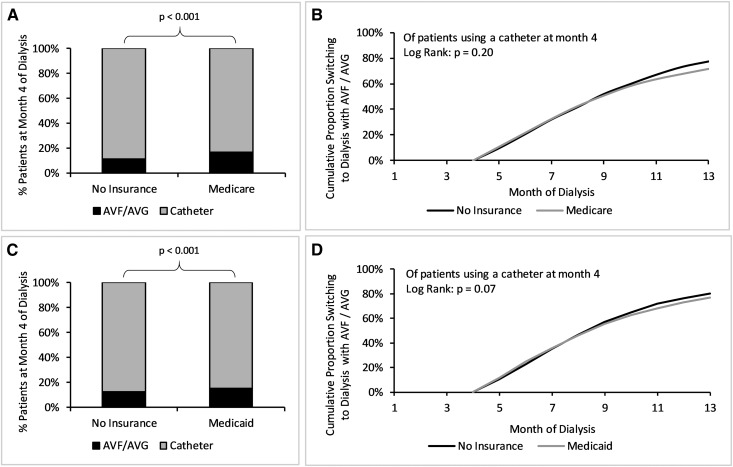
In unadjusted analysis, patients 65–69 years old with Medicare who initiated dialysis using a central venous catheter were more likely to use an AVF or AVG by their fourth dialysis month than uninsured patients 60–64 years old: 16% versus 11%, respectively (P<0.001) (Figure 2a, Table 3). When we adjusted for covariates (all coefficients are in Supplemental Table 3), patients with Medicare had a 63% higher RR (95% CI, 14% to 143%) of AVF or AVG use at month 4 (Figure 3).
Figure 2.
Greater unadjusted arteriovenous fistula (AVF) or arteriovenous graft (AVG) use at month 4 by patients with Medicare and Medicaid with no difference in cumulative incidence afterward. In unadjusted analysis (unpaired t test), patients with Medicare (A) and Medicaid (C) were significantly more likely to use an AVF or AVG than patients with no insurance. When examining patients still using a catheter at month 4, there was no significant difference in the likelihood of obtaining an AVF or AVG in the Medicare versus no insurance (B) or the Medicaid versus no insurance (D) comparisons. Cumulative incidence was derived using the Kaplan–Meier method. (A and C) In the comparison of patients with Medicare versus no insurance, a total of 42% of patients were censored from the Medicare population (9.9% censored for death). The uninsured population had a total of 41% of patients censored (4.5% censored for death). (B and D) In the comparison of patients with Medicaid versus no insurance, a total of 37% of patients were censored from the Medicaid population (3.9% for death). The uninsured population had a total of 35% of patients censored (2.4% for death).
Table 3.
Unadjusted numbers of arteriovenous fistulas and grafts placed over time
| Vascular Access by Population | Month 4 | Month 8 | Month 12 |
|---|---|---|---|
| Medicare versus uninsured | |||
| Medicare | |||
| AVF | 481 | 1521 | 1958 |
| AVG | 239 | 470 | 566 |
| Permanent accesses that are AVFs, % | 67 | 76 | 78 |
| Uninsured | |||
| AVF | 72 | 309 | 458 |
| AVG | 29 | 81 | 101 |
| Permanent accesses that are AVFs, % | 71 | 79 | 82 |
| Medicaid versus uninsured | |||
| Medicaid | |||
| AVF | 478 | 1768 | 2371 |
| AVG | 171 | 421 | 525 |
| Permanent accesses that are AVFs, % | 74 | 81 | 82 |
| Uninsured | |||
| AVF | 626 | 2652 | 3698 |
| AVG | 168 | 465 | 581 |
| Permanent accesses that are AVFs, % | 79 | 85 | 86 |
AVF, arteriovenous fistula; AVG, arteriovenous graft.
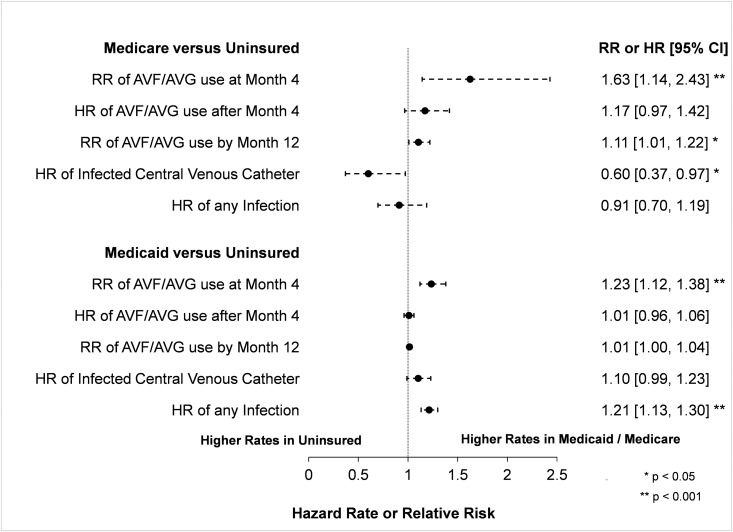
Figure 3.
Greater arteriovenous fistula (AVF) or arteriovenous graft (AVG) use by patients Medicare and Medicaid, with fewer catheter-associated infections in Medicaid patients. Results from multivariable regression models. The reference in all comparisons is the uninsured group. We show the relative risk (RR) of arteriovenous fistula (AVF) or arteriovenous graft (AVG) use at month 4 of dialysis in the entire population estimated from multivariable logistic regression. After excluding patients who were already using an AVF/AVG at month 4, we estimated the hazard ratio (HR) of AVF/AVG use in patients using a central venous catheter after month 4 using multivariable Cox proportional hazard models. We estimated the HR of infections using multivariable Cox proportional hazard models in the entire population. RR of AVF/AVG use at month 13 was determined using a parametric survival model assuming an exponential survival function in the entire population. All models were adjusted for age, sex, race, ethnicity, employment, dual eligibility if applicable, body mass index, albumin, hemoglobin, comorbidities, facility type, number of patients in facility, patient-to-nurse/technician ratio, census characteristics, and year and season of dialysis start (Supplemental Tables 3–10 have coefficients from regressions). 95% CI, 95% confidence interval.
Among patients still receiving dialysis through a central venous catheter at the end of their fourth dialysis month, there was no significant difference in the unadjusted time to switching to an AVF or AVG, with 72% of patients with Medicare and 77% of uninsured patients switching (two-sided log rank test, P=0.20) (Figure 2b). This finding did not change after covariate adjustment, with a hazard ratio (HR) for Medicare versus no insurance of 1.17 (95% CI, 0.97 to 1.42) (Figure 3, Supplemental Table 5).
Medicaid Versus No Insurance.
In unadjusted analyses of patients <65 years old, those with Medicaid who initiated dialysis using a central venous catheter were more likely to use an AVF or AVG by their fourth month of dialysis than uninsured patients: 15% versus 13%, respectively (P<0.001) (Figure 2c, Table 3). After we adjusted for covariates (coefficients are in Supplemental Table 4), patients with Medicaid had a 23% higher RR (95% CI, 12% to 38%) of AVF or AVG use at month 4 (Figure 3).
Among patients still receiving dialysis through a central venous catheter at the end of their fourth dialysis month, there was no significant difference in the unadjusted time to switching to an AVF or AVG, with 77% of patients with Medicaid and 80% of uninsured patients switching (two-sided log rank test, P=0.07) (Figure 2d). Adjusting for covariates did not change this result, with an HR for Medicaid versus no insurance of 1.01 (95% CI, 0.96 to 1.06) (Figure 3, Supplemental Table 6).
Secondary Outcomes
Compared with patients who were uninsured at the start of dialysis, patients with Medicare experienced a lower likelihood of hospitalization involving a vascular access infection between dialysis months 4 and 12 (HR, 0.60; 95% CI, 0.37 to 0.97; P=0.04). In contrast, there was no statistically significant difference in likelihood of hospitalization with any infection between the groups (HR, 0.91; 95% CI, 0.70 to 1.19; P=0.49) (Figure 3, Supplemental Tables 7 and 9). Our comparison of patients with Medicaid with uninsured patients did not find a statistically significant difference in likelihood of hospitalization involving a vascular access infection (HR, 1.10; 95% CI, 0.99 to 1.23; P=0.08). However, patients with Medicaid were significantly more likely to be hospitalized with any infection than uninsured patients (HR, 1.21; 95% CI, 1.13 to 1.30; P<0.001).
Patients with Medicare at the start of dialysis had a higher probability of using an AVF or AVG by the end of month 12 than uninsured patients (RR, 1.11; 95% CI, 1.01 to 1.22; P=0.04). Conversely, there was no significant difference between patients with Medicaid at the start of dialysis and uninsured patients (RR, 1.01; 95% CI, 1.00 to 1.04; P=0.20) (Figure 3, Supplemental Tables 8 and 10).
Sensitivity Analyses
In sensitivity analysis, we found that patients with insurance were also more likely to use an AVF or AVG at the end of month 6 (Medicare RR, 1.54; 95% CI, 1.10 to 2.18; Medicaid RR, 1.24; 95% CI, 1.13 to 1.35), suggesting that longer AVF maturation times did not influence our results (Supplemental Table 11).
We tested the sensitivity of excluding patients with pre-ESKD care by including these patients in our primary models along with a covariate denoting pre-ESKD care in the multivariable regression analyses. Our findings were robust to this sensitivity analysis, with one exception: the Medicaid population had a 5% higher probability of using an AVF or AVG by the end of month 12 than uninsured patients (95% CI, 3% to 7%; P<0.001).
We found no material change in our results on complete patient analysis or when treating death as a competing risk.
Discussion
We found that insurance-related barriers to AVF or AVG use persist into the early dialysis period. In patients initiating dialysis with a central venous catheter, health insurance during the first 3 months of dialysis was associated with greater AVF or AVG use by the end of month 4. The relative magnitude of this difference was substantial. Patients with Medicare or Medicaid at the start of dialysis had 60% and 20%, respectively, higher likelihoods of switching to AVF or AVG use compared with uninsured patients. Although the absolute differences in early AVF and AVG use were modest (5% and 2% unadjusted in the Medicare and Medicaid comparisons, respectively), the relative increases could translate into more substantial gains in younger populations more likely to receive AVF and AVGs.
We also found that insurance-related differences in vascular access use are not necessarily short lived. After obtaining Medicare coverage in the fourth month of dialysis, uninsured patients at the start of dialysis had the same likelihood of switching from a central venous catheter to an AVF or AVG as those with Medicare or Medicaid at dialysis start. Consequently, patients starting dialysis on Medicare were still significantly more likely to use an AVF or AVG by their 12th month than uninsured patients. Our findings are consistent with prior literature showing that patients without health insurance experience substantial barriers to chronic disease care and suggest that this may contribute to long-term disparities in vascular access.
The persistence of insurance-related disparities in vascular access use may be related to inertia. Patients receiving dialysis through a central venous catheter for longer periods of time are less likely to transition to an AVF or AVG, perhaps due to comfort with a catheter (23–25). Additionally, prolonged catheter use is associated with a higher risk for central vein stenosis, complicating future AVF or AVG placement (26). It is unlikely that differences in surgical candidacy explain this disparity, because patients with Medicare or Medicaid at the start of dialysis appeared less healthy, likely making them worse surgical candidates (Tables 1 and 2). Furthermore, patients with Medicaid were more likely than uninsured patients to use an AVF or AVG by month 4, despite being comparable socioeconomically, suggesting that socioeconomic differences do not fully explain differences in vascular access use.
Patients with Medicare experienced fewer hospitalizations involving vascular access infections between dialysis months 4–12. Delayed AVF and AVG use in uninsured patients might explain the relatively higher risk for hospitalizations, consistent with a large body of evidence showing improved health outcomes and lower costs associated with AVF and AVG use compared with catheters (2–11). Although we did not observe a similar difference in hospitalizations involving vascular access infections when comparing patients with Medicaid with uninsured patients, this comparison may also have been confounded by differences in the underlying health of the two populations. Despite our efforts to identify comparison groups as similar as possible, a comparison of observed comorbidities suggests that both the Medicare and Medicaid populations were sicker than the uninsured populations. When comparing patients with Medicare with those without insurance, these differences in underlying health may have led us to underestimate the true association between insurance and hospitalization involving vascular access infections. Because the magnitude of the observed difference in AVF or AVG use among patients with Medicaid versus the uninsured after 3 dialysis months was smaller, it is possible that relative increases in hospitalizations due to prolonged central venous catheter in uninsured patients were too small to offset lower baseline rates of hospitalization resulting from differences in underlying health.
Helping uninsured patients obtain an AVF or AVG earlier could yield substantial gains in health and health care savings and improve systemic disparities faced by uninsured patients. One way to address this opportunity for improvement is to extend Medicare eligibility to the first day of in-center hemodialysis (27). Although this solution would likely face fierce political opposition if it were viewed as an expansion of a federal entitlement program, a similar policy is already in place for patients undergoing home dialysis. Extending Medicare eligibility for vascular access care to the first day of in-center hemodialysis may be more appropriately viewed as a refinement to Medicare’s existing ESKD program. Although such a policy might increase initial upstream costs, it could yield downstream Medicare savings by preventing complications associated with central venous catheters. The Affordable Care Act may have partially addressed this issue through expanding Medicaid, making insurance accessible for many uninsured patients. However, many states have opted out of Medicaid expansion, leaving their patients vulnerable.
Earlier AVF or AVG placements could also reduce undue financial pressure exerted by the Quality Incentive Program (QIP) on providers that care for a large share of uninsured patients. The QIP penalizes dialysis facilities with high proportions of patients using central venous catheters after the first 90 days of dialysis. Although this 90-day grace period gives providers time to help patients obtain an AVF or AVG, our findings suggest that insurance status in the first 3 months of dialysis may contribute to long-term differences in catheter use with associated financial ramifications for dialysis facilities. Additionally, we found that a nontrivial proportion of uninsured patients used an AVF or AVG at month 4 of dialysis, suggesting that providers likely subsidized access placements, either directly through donated care or indirectly through charity, taxes, and government assistance. A policy extending insurance coverage could alleviate financial pressure on these providers.
Our study had some limitations. A relatively small sample size limited statistical power. Data on vascular access use were only available at the monthly level, and we could not compare changes in vascular access type in the first 3 months of dialysis. Additionally, the Medicare population was categorically older than the uninsured population. Although we restricted the Medicare population to 65–69 years of age and the uninsured group to 60–64 years of age, it is possible that small age-related biases persisted. Our results may have also been confounded by unobserved characteristics given the observational nature of our study. Patients without insurance had fewer comorbidities at hemodialysis start, which could reflect an under-reporting of known conditions and may have affected our multivariable regression analyses. We attempted to mitigate some of these concerns by excluding patients with access to pre-ESKD care. However, this exclusion may have led to the selection of a sicker patients in the Medicare and Medicaid cohorts who had access to but did not use pre-ESKD care before starting dialysis.
In summary, insurance-related barriers to AVF or AVG use persist after patients start dialysis and do not seem to correct through the first year of dialysis. These barriers may translate into a higher likelihood of hospitalizations involving vascular access infections in some patients. Coverage for vascular access care among the uninsured population before the fourth month of dialysis could yield increased AVF and AVG use and lead to improvements in patient health and health care costs.
This study was approved by the institutional review boards at Baylor College of Medicine and Stanford University School of Medicine.
Disclosures
None.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Kyle Buika and Sasha Kapralov for their assistance in performing preliminary analyses for this study.
This work was supported by grants F32DK107123 (to E.L.) and K23DK101693 (to K.F.E.) from the National Institute of Diabetes and Digestive and Kidney Diseases. W.C.W. receives research and salary support through the endowed Gordon A. Cain Chair in Nephrology at Baylor College of Medicine.
This work was conducted under data use agreements between W.C.W. (Baylor College of Medicine), Dr. Tara Chang (Stanford University School of Medicine), and the National Institutes for Diabetes and Digestive and Kidney Diseases (NIDDK). An NIDDK officer reviewed the manuscript and approved it for submission. The data reported here have been supplied by the US Renal Data Systems. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.06660518/-/DCSupplemental.
References
- 1.United States Renal Data System : 2017 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2017 [Google Scholar]
- 2.Dalrymple LS, Mu Y, Romano PS, Nguyen DV, Chertow GM, Delgado C, Grimes B, Kaysen GA, Johansen KL: Outcomes of infection-related hospitalization in Medicare beneficiaries receiving in-center hemodialysis. Am J Kidney Dis 65: 754–762, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metcalfe W, Khan IH, Prescott GJ, Simpson K, Macleod AM: Hospitalization in the first year of renal replacement therapy for end-stage renal disease. QJM 96: 899–909, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Rayner HC, Pisoni RL, Bommer J, Canaud B, Hecking E, Locatelli F, Piera L, Bragg-Gresham JL, Feldman HI, Goodkin DA, Gillespie B, Wolfe RA, Held PJ, Port FK: Mortality and hospitalization in haemodialysis patients in five European countries: Results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 19: 108–120, 2004 [DOI] [PubMed] [Google Scholar]
- 5.O’Connor AS, Wish JB, Sehgal AR: The morbidity and cost implications of hemodialysis clinical performance measures. Hemodial Int 9: 349–361, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Dixon BS, Novak L, Fangman J: Hemodialysis vascular access survival: Upper-arm native arteriovenous fistula. Am J Kidney Dis 39: 92–101, 2002 [DOI] [PubMed] [Google Scholar]
- 7.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J; CHOICE Study : Type of vascular access and survival among incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 16: 1449–1455, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK: Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 60: 1443–1451, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Pastan S, Soucie JM, McClellan WM: Vascular access and increased risk of death among hemodialysis patients. Kidney Int 62: 620–626, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Pisoni RL, Arrington CJ, Albert JM, Ethier J, Kimata N, Krishnan M, Rayner HC, Saito A, Sands JJ, Saran R, Gillespie B, Wolfe RA, Port FK: Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: An instrumental variable analysis. Am J Kidney Dis 53: 475–491, 2009 [DOI] [PubMed] [Google Scholar]
- 11.Polkinghorne KR, McDonald SP, Atkins RC, Kerr PG: Vascular access and all-cause mortality: A propensity score analysis. J Am Soc Nephrol 15: 477–486, 2004 [DOI] [PubMed] [Google Scholar]
- 12.Quinn RR, Oliver MJ, Devoe D, Poinen K, Kabani R, Kamar F, Mysore P, Lewin AM, Hiremath S, MacRae J, James MT, Miller L, Hemmelgarn BR, Moist LM, Garg AX, Chowdhury TT, Ravani P: The effect of predialysis fistula attempt on risk of all-cause and access-related death. J Am Soc Nephrol 28: 613–620, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peters VJ, Clemons G, Augustine B: “Fistula First” as a CMS breakthrough initiative: Improving vascular access through collaboration. Nephrol Nurs J 32: 686–687, 2005 [PubMed] [Google Scholar]
- 14.National Kidney Foundation-Dialysis Outcomes Quality Initiative : NKF-DOQI clinical practice guidelines for vascular access. Am J Kidney Dis 30[Suppl 3]: S150–S191, 1997 [PubMed] [Google Scholar]
- 15.Monitor DP: Vascular Access in Use: National Sample, Ann Arbor, MI, Arbor Research Collaborative for Health, 2015 [Google Scholar]
- 16.Pisoni RL, Zepel L, Port FK, Robinson BM: Trends in US vascular access use, patient preferences, and related practices: An update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis 65: 905–915, 2015 [DOI] [PubMed] [Google Scholar]
- 17.Zarkowsky DS, Arhuidese IJ, Hicks CW, Canner JK, Qazi U, Obeid T, Schneider E, Abularrage CJ, Freischlag JA, Malas MB: Racial/ethnic disparities associated with initial hemodialysis access. JAMA Surg 150: 529–536, 2015 [DOI] [PubMed] [Google Scholar]
- 18.92nd Congress: Social Security Amendments of 1972. 1972. United States Code, Public Law 92-603. 86 Stat 1329–1491. Available at: https://www.gpo.gov/fdsys/pkg/STATUTE-86/pdf/STATUTE-86-Pg1329.pdf. Accessed September 17, 2018.
- 19.Gillespie BW, Morgenstern H, Hedgeman E, Tilea A, Scholz N, Shearon T, Burrows NR, Shahinian VB, Yee J, Plantinga L, Powe NR, McClellan W, Robinson B, Williams DE, Saran R: Nephrology care prior to end-stage renal disease and outcomes among new ESRD patients in the USA. Clin Kidney J 8: 772–780, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noridian Healthcare Solutions : Modifiers, Fargo, ND, Noridian Healthcare Solutions, 2018 [Google Scholar]
- 21.Lin E, Kurella Tamura M, Montez-Rath ME, Chertow GM: Re-evaluation of re-hospitalization and rehabilitation in renal research. Hemodial Int 21: 422–429, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WWAMI : Rural-Urban Commuting Area Codes (RUCA), Grand Forks, ND, WWAMI Rural Health Research Center, 2005 [Google Scholar]
- 23.Lee T, Barker J, Allon M: Tunneled catheters in hemodialysis patients: Reasons and subsequent outcomes. Am J Kidney Dis 46: 501–508, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Asif A, Cherla G, Merrill D, Cipleu CD, Briones P, Pennell P: Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int 67: 2399–2406, 2005 [DOI] [PubMed] [Google Scholar]
- 25.Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, Coresh J: Timing of nephrologist referral and arteriovenous access use: The CHOICE Study. Am J Kidney Dis 38: 494–501, 2001 [DOI] [PubMed] [Google Scholar]
- 26.MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M: Central vein stenosis: A common problem in patients on hemodialysis. ASAIO J 51: 77–81, 2005 [DOI] [PubMed] [Google Scholar]
- 27.Allon M, Dinwiddie L, Lacson E Jr., Latos DL, Lok CE, Steinman T, Weiner DE: Medicare reimbursement policies and hemodialysis vascular access outcomes: A need for change. J Am Soc Nephrol 22: 426–430, 2011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.