Abstract
Background:
Nowadays, the anterior cruciate ligament (ACL) injury has been one of the most common diseases of the knee joint. The relationships between the ACL injury and the anatomical structures are still controversial. This study aimed to identify the anatomical risk factors of ACL injury by magnetic resonance imaging (MRI) of the knee.
Methods:
This was a retrospective study of 125 patients undergoing primary ACL reconstruction between July 2013 and May 2017. Another 125 patients without any organic knee joint injury were served as controls. The shape of intercondylar notch, the intercondylar notch width index, the intercondylar notch height index, the α angle, the β angle, and the medial and lateral tibial plateau slope were measured with MRI and compared. The data were compared by binary logistic regression to find the risk factors.
Results:
The two groups differed in the proportion of male patients (70.4% vs. 52.0%, χ2 = 8.911, P = 0.003), but gender was excluded as a risk factor for ACL injury with regression analysis (odds ratio = 1.476, 95% confidence interval [CI]: 0.689–3.160, P = 0.317). The injured group was found to have a smaller notch width index (95% CI = 7.960E-23–2.154E-9, P < 0.001), a larger β angle (95% CI = 1.311–1.785, P < 0.001), and a larger lateral tibial plateau slope (95% CI = 1.201–1.683, P < 0.001). The cutoff values of notch width index, β angle, and the lateral tibial plateau slope were 0.252, 38.5°, and 7.5°, respectively.
Conclusions:
In this study, a narrow intercondylar notch (intercondylar notch width index <0.252), a larger lateral tibial slope (>7.5°), and larger β angle (>38.5°) might be the factors associated with ACL injury.
Trial Registration:
ChiCTR-RRC-17014116; http://www.chictr.org.cn/showproj.aspx?proj=24119 .
Keywords: Anatomy, Anterior Cruciate Ligament Injuries, Risk Factors
摘要
背景:
随着时代的发展,前交叉韧带(anterior cruciate ligament, ACL)损伤已成为最为常见的膝关节损伤疾病之一。 各个解剖学因素与ACL损伤之间的关系仍存在争议。本研究旨在通过磁共振研究评估各解剖学因素与ACL损伤之间的关系。
方法:
此研究为一项回顾性研究,纳入2013年7月至2017年5月间行初次ACL重建的125位患者作为损伤组及另外125位无膝 关节损伤病人作为对照组。通过磁共振图像测量和比较各解剖学指标包括髁间窝形态、髁间窝宽度系数、髁间窝高度系 数、a角、β角及内外侧平台后倾角。研究方法采用回归分析确定各因素与ACL损伤之间的关系。
结果:
两组男性患者比例存在明显差异(70.4% vs.52.0%, χ2=8.911, P =0.003),但回归分析显示性别并非导致 ACL 损伤的危险因素(OR = 1.476, 95% CI:0.689–3.160, P=0.317)。损伤组患者相比于对照组有着较小的髁间窝宽度系数 (95% CI =7.960E-23- 2.154E-9,P<0.001)、较大的β角(95% CI =1.311–1.785,P<0.001)和较大外侧胫骨平台后倾角 (95%CI=1.201–1.683, P<0.001),这三者各自的参考临界值为0.252, 38.5º和7.5º。
结论:
本研究显示,较小的髁间窝宽度系数(<0.252)、较大的外侧胫骨平台后倾角(>7.5º) 以及较大的β角(>38.5º)是 导致ACL损伤的危险因素,同时β角可能成为评估ACL损伤最重要的危险因素。
INTRODUCTION
The anterior cruciate ligament (ACL) is one of the major stabilizers of the knee joint. In addition, it is one of the most commonly injured ligaments of the knee joint. Because of the high incidence of sequelae resulting from ACL injuries, including pain, instability, articular cartilage injury, and posttraumatic osteoarthritis,[1,2] various studies have attempted to identify the risk factors of ACL injuries, including sex, femoral intercondylar notch dimension, ACL size, and joint laxity.[3,4,5,6,7]
Magnetic resonance imaging (MRI) is the most efficient and noninvasive method for the diagnosing ACL injuries and observing knee morphology.[8] Recently, an increasing number of studies have used MRI technology to evaluate the various anatomical aspects of the knee joint,[9,10,11,12] such as the increased tibial plateau slope and the intercondylar notch type.[13,14,15,16,17,18]
In the early years of ACL research, many clinical studies and high-quality meta-analyses were conducted to identify the association between the tibial slope and ACL injury, but the results were inconsistent.[13,14,19,20,21,22] Several studies found differences in the anatomic risk factors between men and women.[11,23] In addition, one study suggested that the medial tibial plateau slope and lateral tibial plateau slope should be measured separately due to their opposite effects on ACL injury.[24] Similarly, there have been conflicting reports about the association between the shape of the femoral condyle and ACL injury.[13,18,25,26,27,28,29] In addition, van Eck et al.[18] suggested that ACL injury was associated with the shape of the femoral notch, Al-Saeed et al.[8] found that a Type A femoral notch was a risk factor for ACL injury, while a small femoral notch width index was not a risk factor for ACL injury. Type A was described as a narrow notch that resembled an acute triangle. Moreover, Alentorn-Geli et al.[13] suggested that the intercondylar notch angle may be a better parameter to evaluate notch narrowing and its potential association with ACL injuries than the notch width.
Because of the conflicting opinions about anatomical structures, the purpose of this study was to determine the relationship between anatomic structures and ACL injury and to identify the risk factor which was the most clinically relevant risk factor. The investigated structures include the intercondylar notch index, intercondylar notch height index, α angle (notch angle), β angle (formed by the Blumensaat line and the long axis of the femur), medial tibial plateau slope, and lateral tibial plateau slope.
METHODS
Ethical approval
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University (No. JD-LK-2017-022-01). As a retrospective study and data analysis were performed anonymously, this study was exempt from the informed consent from patients.
Patient selection
This study was a retrospective review of patients who underwent primary ACL reconstruction in our hospital between July 2013 and May 2017. In total, 235 patients underwent primary ACL reconstruction; patients with the following criteria of knee injury were excluded from the study: (1) suspicious ACL rupture; (2) other ligament injuries, such as the posterior cruciate ligament and medial collateral ligament; (3) skeletal dysplasia; (4) knee joint valgus or varus deformity; (5) fracture history of the knee joint; (6) osteoarthritis; (7) history of knee surgery; or (8) no MRI images. Finally, 110 patients (20 patients with medial collateral ligament injury, 58 patients with fracture history, 19 patients with osteoarthritis, and 13 patients without MRI images) were excluded due to the exclusion criteria. Thus, 125 patients with ACL injuries and 125 control patients with an MRI-confirmed absence of an organic knee joint injury (no evidence of ACL injury, meniscus injury, fracture, etc., on MRI images) were included in this study. The diagnosis of the ACL injury was confirmed by arthroscopic examination, which is the gold standard. (The study included eight independent variables, and the number of the study was more than 20 times of the number of the independent variables.)
Patient exclusion criteria
Patients who met the following knee injury criteria were excluded from the study: (1) suspected ACL rupture; (2) other ligament injuries, such as the posterior cruciate ligament and medial collateral ligament; (3) skeletal dysplasia; (4) knee joint valgus or varus deformity; (5) fracture history of the knee joint; (6) osteoarthritis; (7) history of knee surgery; or (8) no MRI images.
Measurement of the anatomical indexes of the knee joint
The MR images were acquired on an Esaote Dedicated MRI 0.25T G-scan (Italy), and we download the images from our institute's Picture Archiving and Communication System. We obtained the axial images on T1-weighted image (T1WI) with a repetition time (TR) of 800 ms, an echo time (TE) of 14 ms, and a 4-mm slice thickness at every 0.4-mm advance. The sagittal images were obtained on T1WI with a TR of 850 ms, an TE of 26 ms, and a 4-mm slice thickness at every 0.4-mm advance and on T2WI with a TR of 2800 ms, an TE of 80 ms, and a 4-mm slice thickness every 0.4-mm advance.
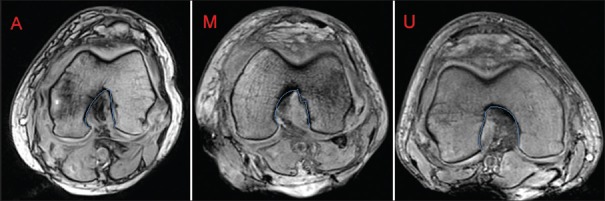
The method used to locate the reference line on the axial plane is shown in Figure 1; the reference line was drawn between the condylar ends across the most distal aspect of the femur. As described by Souryal et al.,[30] the femoral condylar width was measured along a line through the popliteal groove parallel to the reference line [Figure 2]. The height of the femoral condylar was the distance from the peak of the lateral femoral condylar to the reference line [Figure 2]. The intercondylar notch height was equal to the maximum height of the notch (from the peak of the notch to the reference line) [Figure 2]. The intercondylar notch width was measured at the borders of two-thirds of the intercondylar notch height [Figure 2]. The α angle was measured as the inclination of the two lines (from the peak of the notch to the most inferior aspect of the notch at the medial and lateral condyles). We drew a line B parallel to the reference line C, and the line B was the tangent of the notch; the point A was the apex of the notch [Figure 3]. The shape of the intercondylar notch was classified as Type A, Type U, and Type M, according to van Eck et al.[18] Same to the above description, Type A was described as a narrow notch that resembled an acute triangle. In Type U, the apex was wider than that of Type A. Type M had two apices, which distinguished it from the other two types, and was also wider [Figure 4].
Figure 1.
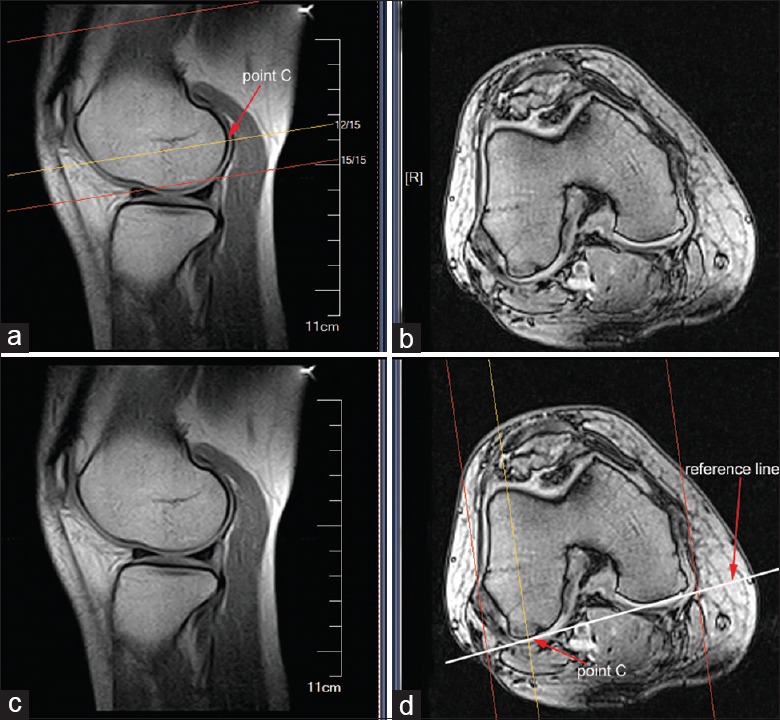
The way to locate the reference line. With the localization function of the imaging system, we could locate the most distal aspect of the lateral femoral condylar as point C; on the axial plane, we could make the tangent to the condylar ends through the point C.
Figure 2.
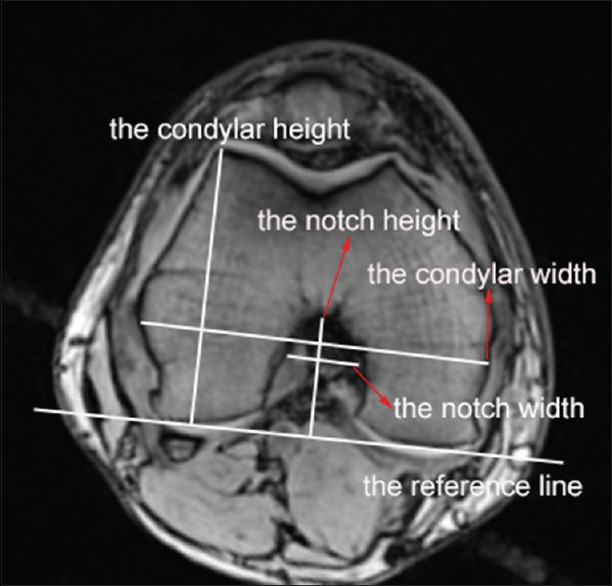
Measurements of the anatomic structures of femoral condylar and intercondylar notch. On the axial magnetic resonance imaging, the measurements of the notch width, notch height, femoral condylar height, and femoral condylar width.
Figure 3.
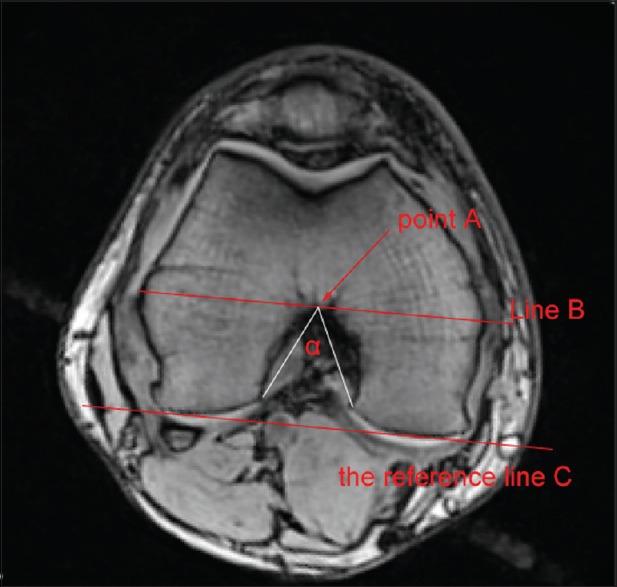
The way to measure notch angle. We drew a line B parallel to the reference line C, and the line B was the tangent of the notch; the point A was the apex of the notch. The α angle was measured as the inclination of the two lines (from the peak of the notch to the most inferior aspect of the notch at the medial and lateral condyles).
Figure 4.
The three shape types of femoral notch. The above pictures showed three types of femoral notch: the left one was Type A, the middle one was Type M, and the right one was Type U.
On the sagittal MRI, in a sagittal section where the entire Blumensaat line was seen, then we drew two circles, one that was tangent to the distal, anterior, and posterior femur edges and another that was tangent to the anterior and posterior femur edges. The line connecting the centers of the two circles was defined as the long axis of the femur [Figure 5]. The β angle was measured as the angle formed by the Blumensaat line and the long axis of the femur [Figure 6].[26] To measure the medial and lateral tibial plateau slopes, we chose the sagittal slice that clearly showed the intercondylar eminence and the attachment of the posterior cruciate ligament. Then, we drew two circles, one that was tangent to the proximal, anterior, and posterior tibial edges and another that was tangent to the anterior and posterior tibial edges. The line connecting the centers of the two circles was defined as the longitudinal tibial axis[31] [Figure 7]. Finally, the inclination of the perpendicular line of the longitudinal tibial axis and tangent to the medial tibial plateau was the medial tibial slope. The lateral tibial slope was measured using a similar method [Figures 8 and 9].
Figure 5.
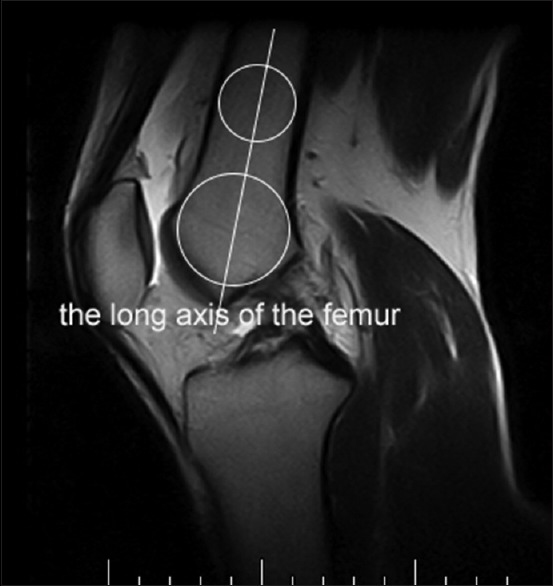
The ways to locate the central axis of the femur.
Figure 6.

Measurement of β angle. On the sagittal magnetic resonance imaging, the β angle was the inclination of the longitudinal femoral axis and the Blumensaat line.
Figure 7.
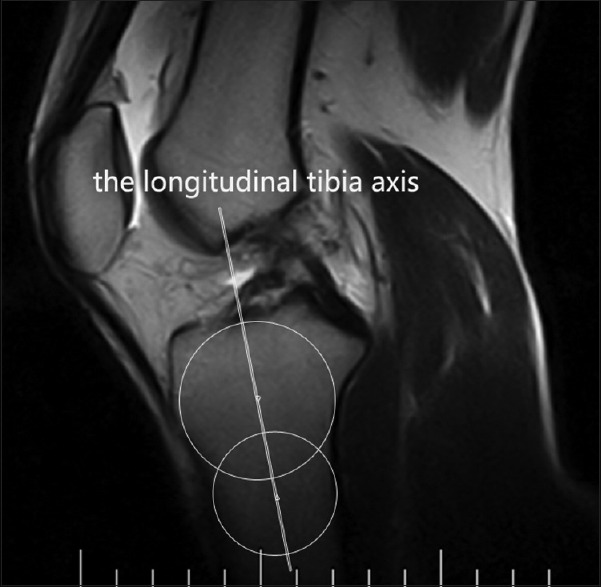
The ways to locate the longitudinal tibial axis. We chose the sagittal slice which clearly showed the intercondylar eminence and the attachment of the posterior cruciate ligament.
Figure 8.
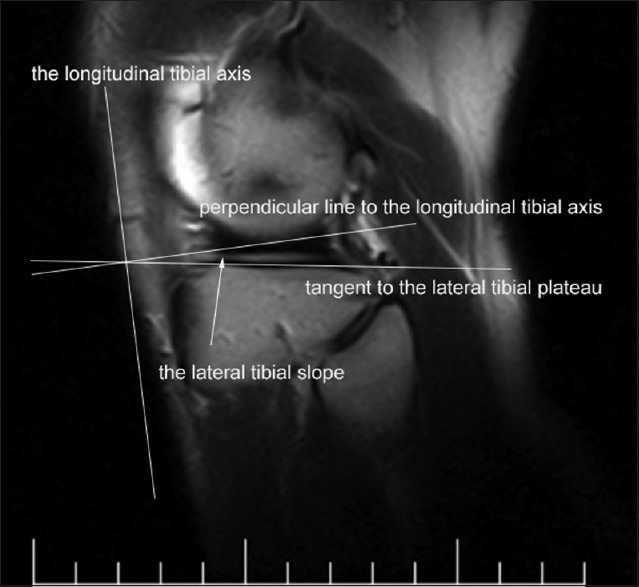
Measurements of the lateral tibial slope.
Figure 9.
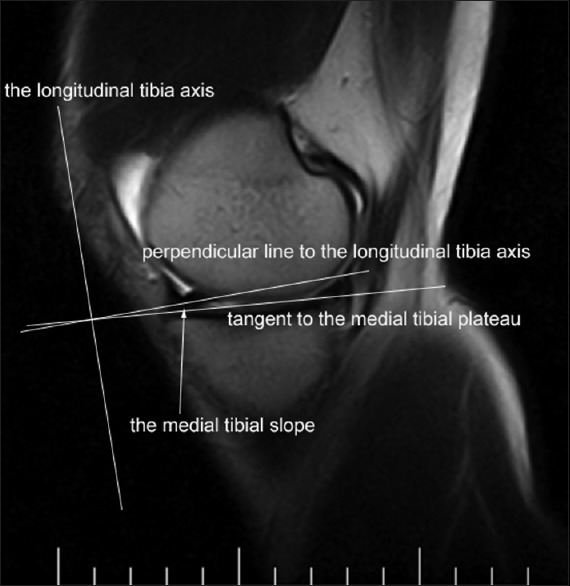
Measurements of the medial tibial slope.
Statistical analysis
The data analysis consisted of descriptive statistics and regression modeling. The differences of the age between two groups were compared by rank-sum test. The differences in the male: female ratio and the number of each type of shape of the intercondylar notch between the two groups were compared by the Chi-square test. Before the logistic analysis, a single factor analysis was conducted to compare the measurements between ACL-injured and noninjured groups. The relationships between ACL injury and potential risk factors including age, sex, notch shape, notch width index, notch height index, α angle, β angle, medial tibial slope, and lateral tibial slope were assessed by binary logistic regression analysis. In that analysis, the dependent variable was defined as ACL status (0 = normal; 1 = injury). The statistical significance of the coefficients in the regression equation was determined with the Wald test. Odds ratios (ORs) and their respective 95% confidence intervals(CIs) were also estimated. Receiver operating characteristic (ROC) curves were prepared from the measured MRI data to determine the cutoff values. All statistical analyses were performed using SPSS 24.0 (SPSS Inc., Chicago, IL, USA), and a value of P < 0.05 was considered statistically significant.
RESULTS
There were 125 ACL injury patients and 125 controls. There was no age difference between the groups (30.8 ± 10.0 vs. 32.4 ± 9.7 years, Z = 1.458, P = 0.145). The demographic data, injury side data, and the notch shape proportions are shown in Table 1. There were more males in the injury group (70.4% vs. 52.0%, χ2 = 8.911, P = 0.003), but the gender was not identified as a risk factor in the logistic regression analysis (odds ratio [OR] = 1.476, 95% confidence interval [CI]: = 0.689–3.160, P = 0.317) [Table 2]. The side of the injury was also not different between the two groups (χ2 = 0.400, P = 0.527). The proportion of Type A intercondylar notches observed in the injured group was larger than that in the control group (54.4% vs. 36.8%, χ2 = 7.804, P = 0.005). The single factor analysis was shown in Table 3. From the table, we found smaller notch width index (0.247 ± 0.032 vs. 0.273 ± 0.024, t = −7.360, P < 0.001), smaller α angle (46.70 ± 7.04 vs. 50.73 ± 7.76, t = −4.293, P < 0.001), larger β angle (41.48 ± 2.22 vs. 38.30 ± 3.16, t = 9.199, P < 0.001), larger medial tibial slope (6.85 ± 2.59 vs. 5.61 ± 1.76, t = 4.424, P < 0.001), and lager lateral tibial slope (8.04 ± 3.32 vs. 5.34 ± 1.83, t = 7.953, P < 0.001) in ACL-injured group compared to the controls. The binary logistic regressions of the factors including the intercondylar notch shape, notch width index, notch height index, α angle, β angle, medial tibial plateau slope, and lateral tibial plateau slope are shown in Table 2. From the table, the notch width index (OR = 4.141E-16, 95% CI = 7.960E-23–2.154E-9, P < 0.001), β angle (OR = 1.530, 95% CI = 1.311–1.785, P < 0.001), and lateral tibial slope (OR = 1.422, 95% CI = 1.201–1.683, P < 0.001) were identified as significant risk factors for ACL injury.
Table 1.
Basic clinical characteristics of the ACL-injured and noninjured group
| Parameters | Injured group (n = 125) | Control group (n = 125) | Statistics | P |
|---|---|---|---|---|
| Age (years) | 30.8 ± 10.0 | 32.4 ± 9.7 | 1.458* | 0.145 |
| Gender | ||||
| Male | 88 (70.4) | 65 (52.0) | 8.911† | 0.003 |
| Female | 37 (29.6) | 60 (48.0) | ||
| Side | ||||
| Left | 62 (49.6) | 67 (53.6) | 0.400† | 0.527 |
| Right | 63 (50.4) | 58 (46.4) | ||
| Notch type | ||||
| A | 68 (54.4) | 46 (36.8) | 7.804† | 0.005 |
| U + M | 57 (45.6) | 79 (63.2) |
Values are presented as mean ± SD and n (%). *Z values; †χ2 values. ACL: Anterior cruciate ligament; A: The A-type notch; U + M: The U-type and M-type notch; SD: Standard deviation.
Table 2.
Binary logistic regression analysis of relationship of the factors with ACL injury (n = 250)
| Variable | Regression coefficient | SD | P | OR | 95% CI |
|---|---|---|---|---|---|
| Age (years) | 0.730 | ||||
| 20–29 | −0.903 | 2.148 | 0.674 | 0.405 | 0.006–27.292 |
| 30–39 | −1.484 | 2.081 | 0.476 | 0.227 | 0.004–13.405 |
| 40–49 | −1.442 | 2.097 | 0.492 | 0.236 | 0.004–14.418 |
| 50–59 | −1.775 | 2.124 | 0.403 | 0.169 | 0.003–10.896 |
| 60–69 | −0.356 | 2.288 | 0.876 | 0.700 | 0.008–62.022 |
| Sex | 0.389 | 0.389 | 0.317 | 1.476 | 0.689–3.160 |
| Notch shape | 0.867 | ||||
| Notch shape M | −0.230 | 0.432 | 0.595 | 0.794 | 0.340–1.854 |
| Notch shape U | −0.110 | 0.745 | 0.883 | 0.896 | 0.208–3.857 |
| Notch width index | −35.42 | 7.890 | <0.001 | 4.141E-16 | 7.960E-23–2.154E-9 |
| Notch height index | 0.882 | 1.006 | 0.380 | 2.416 | 0.337–17.342 |
| α angle (°) | −0.038 | 0.032 | 0.231 | 0.963 | 0.905–1.024 |
| β angle (°) | 0.425 | 0.079 | <0.001 | 1.530 | 1.311–1.785 |
| Medial tibial slope | −0.026 | 0.095 | 0.787 | 0.975 | 0.809–1.175 |
| Lateral tibial slope | 0.352 | 0.086 | <0.001 | 1.422 | 1.201–1.683 |
OR: Odds ratio; CI: Confidence interval; α angle: The notch angle; β angle: The angle formed by the Blumensaat line and the long axis of the femur; n = 250, including 125 injured patients and 125 controls; ACL: Anterior cruciate ligament; SD: Standard deviation.
Table 3.
Single factor analysis comparing the measurements between ACL-injured and noninjured group (n = 250)
| Parameters | Injured group (n = 125) | Control group (n = 125) | t | P |
|---|---|---|---|---|
| Notch width index | 0.247 ± 0.032 | 0.273 ± 0.024 | −7.360 | <0.001 |
| Notch height index | 0.453 ± 0.068 | 0.442 ± 0.186 | 0.585 | 0.559 |
| α angle (°) | 46.70 ± 7.04 | 50.73 ± 7.76 | −4.293 | <0.001 |
| β angle (°) | 41.48 ± 2.22 | 38.30 ± 3.16 | 9.199 | <0.001 |
| Medial tibial slope | 6.85 ± 2.59 | 5.61 ± 1.76 | 4.424 | <0.001 |
| Lateral tibial slope | 8.04 ± 3.32 | 5.34 ± 1.83 | 7.953 | <0.001 |
Values are presented as mean ± SD. ACL: Anterior cruciate ligament; α angle: The notch angle; β angle: The angle formed by the Blumensaat line and the long axis of the femur; SD: Standard deviation.
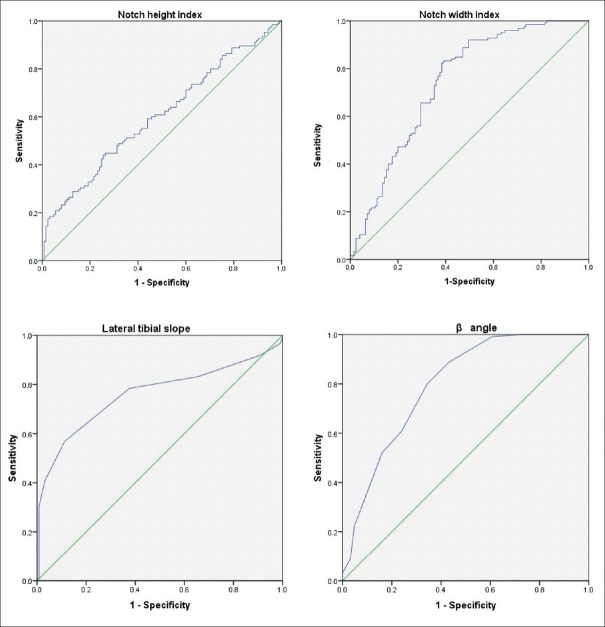
To obtain the cutoff values for the four factors, the ROC curves were generated [Figure 10]. The cutoff values of the notch width index, β angle, and lateral tibial plateau slope were 0.252, 38.5°, and 7.5°, respectively. The sensitivity and specificity were 83.2% and 60.8% for the cutoff value of the notch width index, 88.8% and 56.8% for the cutoff value of the β angle, and 56.8% and 88.8% for the cutoff of the lateral tibial plateau slope, respectively.
Figure 10.
The receiver operating characteristic curves of notch width index (Area Under ROC Curve= 0.739, 95% CI = 0.677–0.801, P < 0.001); notch height index (Area Under ROC Curve= 0.603, 95% CI = 0.533–0.672, P = 0.005); β angle (Area Under ROC Curve= 0.796, 95% CI = 0.740–0.851, P < 0.001) and lateral tibial slope (Area Under ROC Curve= 0.760, 95% CI = 0.698–0.822, P < 0.001). CI: Confidence interval; α angle: The notch angle; β angle: The angle formed by the Blumensaat line and the long axis of the femur; ROC:Receiver operating characteristic curve
DISCUSSION
In this study, we found that a narrower intercondylar notch (< 0.252, sensitivity and specificity were 83.2% and 60.8%, respectively) with a larger β angle (>38.5°, sensitivity and specificity were 88.8% and 56.8%, respectively) and lateral tibial slope (>7.5°, sensitivity and specificity were 56.8% and 88.8%, respectively) were associated with an increased risk of ACL injury. The β angle appeared to be the most important risk factor for predicting ACL injury. The findings of this study agreed with those of previous studies. Zeng et al.[32] conducted a meta-analysis, and the results showed that a smaller notch width index predisposes an individual to ACL injury; the level of evidence was III. A case–control study performed by O’Malley et al.[15] showed a moderate relationship between an increased posterior tibial slope and ACL injury, and the level of evidence was also III. Furthermore, a case-control study performed by Webb et al.[33] showed that an increased tibial slope is associated with increased odds of further ACL injury after ACL reconstruction. In the present study, we further demonstrated that the lateral tibial slope but not the medial tibial slope was associated with ACL injury.
In the present study, we found that the β angle could be the most important risk factor for predicting ACL injury. There have been few studies on the relationship between the β angle and ACL injury. Fernández-Jaén et al.[26] conducted a case-control study and found that ACL injury was associated with a large β angle; they proposed that the risk for ACL injury was multifactorial and that the β angle might not be the sole cause of ACL injury. In this study, we measured the β angle on MRI images and logistic regression analysis showed a clear correlation with ACL injury.
A larger β angle may result in the ACL being more horizontal, therefore causing more ACL impingement against the anterior intercondylar notch, leading to more ACL injury. Similarly, there is less impingement when the β angle is decreased because the ACL is in a more vertical position.[26] However, Bouras et al.[34] did not find a convincing relationship between β angle and ACL injury. Because we could easily measure the β angle on MRI images, we believe that surgeons should pay more attention to patients with larger β angles, and more biomechanical studies on the effects of a larger β angle should be conducted in the future.
There has been extensive discussion regarding the relationship between ACL injury and the tibial slope which remained controversial.[13,14,21] Alentorn-Geli et al.[13] suggested that an increased posterior tibial slope may be associated with ACL injury in male patients, but the association between ACL injury and the angle formed by the Blumensaat line and the anterior tibial slope in male patients requires more investigation. Dare et al.[14] found that the lateral tibial slope was significantly associated with an increased risk of ACL injuries in pediatric and adolescent patients. Some studies have shown a relationship between ACL injury and the tibial slope, but the findings were inconsistent and controversial. The results of a meta-analysis on the topic were also inconclusive[19] although there could be an association in males.[35] From the biomechanical viewpoint, an increased tibial slope may generate greater translational force that could result in increased anterior motion of the tibia. It is known that a major role of the ACL is to prevent anterior tibial motion. Thus, an increased tibial slope may lead to increased tension of the ACL and even ACL rupture.[36] In this study, the lateral tibial slope was identified as an associated risk factor for ACL injury (OR = 1.422, 95% CI = 1.201–1.683, P < 0.001). In addition, the ROC curve showed that the cutoff value was 7.5°, and the sensitivity and specificity for the cutoff value of it were 56.8% and 88.8%, respectively. Although the cutoff value in the study seemed somewhat small, it is important to recognize that multiple factors contribute to ACL injury and that the knee joint acts as a whole in the extension and flexion.
In the study, we found that the intercondylar notch shape did not contribute to ACL injury (P = 0.867), although the proportion of Type A intercondylar notches observed in the injured group was larger than that in the control group (P = 0.005). A Type A intercondylar notch is a narrow intercondylar notch. van Eck et al.[18] classified the type of intercondylar notch into the three types used in this study, namely Type A, Type U, and Type M. The relationship between notch type and ACL injury has been controversial. Osama et al.[8] found that the Type A notch appeared to be a risk factor for ACL injury. Keays et al.[37] found that a Type A notch may also be a contributing factor to ACL injuries in siblings. Because the cause of the ACL injury is multifactorial, while several studies have been conducted to confirm the relationship between notch type and ACL injury, but the results have been conflicting.[38,39,40]
We did not find that the α angle contributed to the increased risk of ACL injury (OR = 0.963, 95% CI = 0.905–1.024, P = 0.231). There have been only a few studies on this relationship, and the results of those studies were also conflicting. Anderson et al.[42,43] found that a notch angle less than or equal to 50° may lead to the ACL injury. To identify the reliability of the notch angle in predicting ACL injury, Stein et al.[41] and Al-Saeed et al.[8] conducted a study and proposed that if the notch resembled “Ω,” then they could confirm that the boom length was small and that the notch width was larger. Therefore, Alentorn-Geli et al.[13] suggested that the notch angle was a better parameter to use to evaluate notch narrowing. In order to remove the age effect on the bone morphology, we divided the patients according to age groups. As shown in Table 2, there was no correlation of age group with ACL injury.
This study had some limitations. First, this was a retrospective study, so we had no chance to use an MRI scans of the patients’ other intact knees as the images of controls. Second, there could exist a selection bias with regard to the difference in gender between the study group and control group. Third, the analysis was not adjusted for many extrinsic and intrinsic factors of the knee joint.
In conclusion, a narrow intercondylar notch (intercondylar notch width index <0.252), a larger β angle (>38.5°), and a larger lateral tibial slope (>7.5°) are risk factors in predicting likelihood for ACL injury. The β angle might be the factor with the strongest prediction for ACL injury.
Financial support and sponsorship
This study was supported by grants from the National Natural Science Foundation of China (No. 81171730) and Postgraduate Research and Practice Innovation Program of Jiangsu Province (No. SJCX17_0658).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Levine JW, Kiapour AM, Quatman CE, Wordeman SC, Goel VK, Hewett TE, et al. Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med. 2013;41:385–95. doi: 10.1177/0363546512465167. doi: 10.1177/0363546512465167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21:696–702. doi: 10.1016/j.arthro.2005.03.010. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC, et al. Risk factors associated with noncontact injury of the anterior cruciate ligament: A prospective four-year evaluation of 859 west point cadets. Am J Sports Med. 2003;31:831–42. doi: 10.1177/03635465030310061801. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 4.Söderman K, Alfredson H, Pietilä T, Werner S. Risk factors for leg injuries in female soccer players: A prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001;9:313–21. doi: 10.1007/s001670100228. doi: 10.1007/s001670100228. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhari AM, Zelman EA, Flanigan DC, Kaeding CC, Nagaraja HN. Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: A magnetic resonance imaging study. Am J Sports Med. 2009;37:1282–7. doi: 10.1177/0363546509332256. doi: 10.1177/0363546509332256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Si HB, Zeng Y, Shen B, Yang J, Zhou ZK, Kang PD, et al. The influence of body mass index on the outcomes of primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:1824–32. doi: 10.1007/s00167-014-3301-1. doi: 10.1007/s00167-014-3301-1. [DOI] [PubMed] [Google Scholar]
- 7.Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lázaro-Haro C, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: A review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859–79. doi: 10.1007/s00167-009-0823-z. doi: 10.1007/s00167-009-0823-z. [DOI] [PubMed] [Google Scholar]
- 8.Al-Saeed O, Brown M, Athyal R, Sheikh M. Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21:678–82. doi: 10.1007/s00167-012-2038-y. doi: 10.1007/s00167-012-2038-y. [DOI] [PubMed] [Google Scholar]
- 9.Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: A case-control study. Arthroscopy. 2010;26:901–6. doi: 10.1016/j.arthro.2009.12.012. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC., Jr Shallow medial tibial plateau and steep medial and lateral tibial slopes: New risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38:54–62. doi: 10.1177/0363546509349055. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 11.Hudek R, Fuchs B, Regenfelder F, Koch PP. Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res. 2011;469:2377–84. doi: 10.1007/s11999-011-1802-5. doi: 10.1007/s11999-011-1802-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467:2066–72. doi: 10.1007/s11999-009-0711-3. doi: 10.1007/s11999-009-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alentorn-Geli E, Pelfort X, Mingo F, Lizano-Díez X, Leal-Blanquet J, Torres-Claramunt R, et al. An evaluation of the association between radiographic intercondylar notch narrowing and anterior cruciate ligament injury in men: The notch angle is a better parameter than notch width. Arthroscopy. 2015;31:2004–13. doi: 10.1016/j.arthro.2015.04.088. doi: 10.1016/j.arthro.2015.04.088. [DOI] [PubMed] [Google Scholar]
- 14.Dare DM, Fabricant PD, McCarthy MM, Rebolledo BJ, Green DW, Cordasco FA, et al. Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: An MRI-based case-control study of 152 patients. Am J Sports Med. 2015;43:1632–9. doi: 10.1177/0363546515579182. doi: 10.1177/0363546515579182. [DOI] [PubMed] [Google Scholar]
- 15.O’Malley MP, Milewski MD, Solomito MJ, Erwteman AS, Nissen CW. The association of tibial slope and anterior cruciate ligament rupture in skeletally immature patients. Arthroscopy. 2015;31:77–82. doi: 10.1016/j.arthro.2014.07.019. doi: 10.1016/j.arthro.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Sun YH, Chen LX, Jiao ZD, Wang L, Zhang RM, Fang J, et al. Age-related changes of posterior tibial slope and its roles in anterior cruciate ligament injury. Int Surg. 2015;101:70–7. doi: 10.9738/INTSURG-D-15-00127.1. doi: 10.9738/INTSURG-D-15-00127.1. [DOI] [PubMed] [Google Scholar]
- 17.Youm YS, Cho SD, Cho HY, Jung SH. Relationship between mucoid degeneration of the anterior cruciate ligament and posterior tibial slope in patients with total knee arthroplasty. Knee Surg Relat Res. 2016;28:34–8. doi: 10.5792/ksrr.2016.28.1.34. doi: 10.5792/ksrr.2016.28.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Eck CF, Martins CA, Vyas SM, Celentano U, van Dijk CN, Fu FH. Femoral intercondylar notch shape and dimensions in ACL-injured patients. Knee Surg Sports Traumatol Arthrosc. 2010;18:1257–62. doi: 10.1007/s00167-010-1135-z. doi: 10.1007/s00167-010-1135-z. [DOI] [PubMed] [Google Scholar]
- 19.Wordeman SC, Quatman CE, Kaeding CC, Hewett TE. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: A systematic review and meta-analysis. Am J Sports Med. 2012;40:1673–81. doi: 10.1177/0363546512442307. doi: 10.1177/0363546512442307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeng C, Cheng L, Wei J, Gao SG, Yang TB, Luo W, et al. The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22:53–65. doi: 10.1007/s00167-012-2277-y. doi: 10.1007/s00167-012-2277-y. [DOI] [PubMed] [Google Scholar]
- 21.Blanke F, Kiapour AM, Haenle M, Fischer J, Majewski M, Vogt S, et al. Risk of noncontact anterior cruciate ligament injuries is not associated with slope and concavity of the tibial plateau in recreational alpine skiers: A Magnetic resonance imaging-based case-control study of 121 patients. Am J Sports Med. 2016;44:1508–14. doi: 10.1177/0363546516632332. doi: 10.1177/0363546516632332. [DOI] [PubMed] [Google Scholar]
- 22.Rahnemai-Azar AA, Yaseen Z, van Eck CF, Irrgang JJ, Fu FH, Musahl V, et al. Increased lateral tibial plateau slope predisposes male college football players to anterior cruciate ligament injury. J Bone Joint Surg Am. 2016;98:1001–6. doi: 10.2106/JBJS.15.01163. doi: 10.2106/JBJS.15.01163. [DOI] [PubMed] [Google Scholar]
- 23.Hohmann E, Bryant A, Reaburn P, Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc. 2011;19(Suppl 1):S109–14. doi: 10.1007/s00167-011-1547-4. doi: 10.1007/s00167-011-1547-4. [DOI] [PubMed] [Google Scholar]
- 24.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16:112–7. doi: 10.1007/s00167-007-0438-1. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 25.Domzalski M, Grzelak P, Gabos P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: Analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop. 2010;34:703–7. doi: 10.1007/s00264-010-0987-7. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernández-Jaén T, López-Alcorocho JM, Rodriguez-Iñigo E, Castellán F, Hernández JC, Guillén-García P. The importance of the intercondylar notch in anterior cruciate ligament tears. Orthop J Sports Med. 2015;3:2325967115597882. doi: 10.1177/2325967115597882. doi: 10.1177/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw KA, Dunoski B, Mardis N, Pacicca D. Knee morphometric risk factors for acute anterior cruciate ligament injury in skeletally immature patients. J Child Orthop. 2015;9:161–8. doi: 10.1007/s11832-015-0652-1. doi: 10.1007/s11832-015-0652-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freychet B, Lakhal W, Daggett M, Bonnard C. Intercondylar notch dysplasia in open-physis anterior cruciate ligament injuries: A case-control study. Orthop Traumatol Surg Res. 2016;102:203–6. doi: 10.1016/j.otsr.2015.11.017. doi: 10.1016/j.otsr.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 29.Lombardo S, Sethi PM, Starkey C. Intercondylar notch stenosis is not a risk factor for anterior cruciate ligament tears in professional male basketball players: An 11-year prospective study. Am J Sports Med. 2005;33:29–34. doi: 10.1177/0363546504266482. doi: 10.1177/0363546504266482. [DOI] [PubMed] [Google Scholar]
- 30.Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: Associated intercondylar notch stenosis. Am J Sports Med. 1988;16:449–54. doi: 10.1177/036354658801600504. doi: 10.1177/036354658801600504. [DOI] [PubMed] [Google Scholar]
- 31.Lipps DB, Wilson AM, Ashton-Miller JA, Wojtys EM. Evaluation of different methods for measuring lateral tibial slope using magnetic resonance imaging. Am J Sports Med. 2012;40:2731–6. doi: 10.1177/0363546512461749. doi: 10.1177/0363546512461749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng C, Gao SG, Wei J, Yang TB, Cheng L, Luo W, et al. The influence of the intercondylar notch dimensions on injury of the anterior cruciate ligament: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:804–15. doi: 10.1007/s00167-012-2166-4. doi: 10.1007/s00167-012-2166-4. [DOI] [PubMed] [Google Scholar]
- 33.Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41:2800–4. doi: 10.1177/0363546513503288. doi: 10.1177/0363546513503288. [DOI] [PubMed] [Google Scholar]
- 34.Bouras T, Fennema P, Burke S, Bosman H. Stenotic intercondylar notch type is correlated with anterior cruciate ligament injury in female patients using magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2018;26:1252–7. doi: 10.1007/s00167-017-4625-4. doi: 10.1007/s00167-017-4625-4. [DOI] [PubMed] [Google Scholar]
- 35.Wang YL, Yang T, Zeng C, Wei J, Xie DX, Yang YH, et al. Association between tibial plateau slopes and anterior cruciate ligament injury: A Meta-analysis. Arthroscopy. 2017;33:1248–59.e4. doi: 10.1016/j.arthro.2017.01.015. doi: 10.1016/j.arthro.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 36.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76:745–9. doi: 10.1302/0301-620x.76b5.8083263. [PubMed] [Google Scholar]
- 37.Keays SL, Keays R, Newcombe PA. Femoral intercondylar notch width size: A comparison between siblings with and without anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24:672–9. doi: 10.1007/s00167-014-3491-6. doi: 10.1007/s00167-014-3491-6. [DOI] [PubMed] [Google Scholar]
- 38.Hoteya K, Kato Y, Motojima S, Ingham SJ, Horaguchi T, Saito A, et al. Association between intercondylar notch narrowing and bilateral anterior cruciate ligament injuries in athletes. Arch Orthop Trauma Surg. 2011;131:371–6. doi: 10.1007/s00402-010-1254-5. doi: 10.1007/s00402-010-1254-5. [DOI] [PubMed] [Google Scholar]
- 39.Ireland ML, Ballantyne BT, Little K, McClay IS. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2001;9:200–5. doi: 10.1007/s001670100197. doi: 10.1007/s001670100197. [DOI] [PubMed] [Google Scholar]
- 40.Dienst M, Schneider G, Altmeyer K, Voelkering K, Georg T, Kramann B, et al. Correlation of intercondylar notch cross sections to the ACL size: A high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127:253–60. doi: 10.1007/s00402-006-0177-7. doi: 10.1007/s00402-006-0177-7. [DOI] [PubMed] [Google Scholar]
- 41.Stein V, Li L, Guermazi A, Zhang Y, Kent Kwoh C, Eaton CB, et al. The relation of femoral notch stenosis to ACL tears in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2010;18:192–9. doi: 10.1016/j.joca.2009.09.006. doi: 10.1016/j.joca.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cha JH, Lee SH, Shin MJ, Choi BK, Bin SI. Relationship between mucoid hypertrophy of the anterior cruciate ligament (ACL) and morphologic change of the intercondylar notch: MRI and arthroscopy correlation. Skeletal Radiol. 2008;37:821–6. doi: 10.1007/s00256-008-0527-3. doi: 10.1007/s00256-008-0527-3. [DOI] [PubMed] [Google Scholar]
- 43.Anderson AF, Lipscomb AB, Liudahl KJ, Addlestone RB. Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15:547–52. doi: 10.1177/036354658701500605. doi: 10.1177/036354658701500605. [DOI] [PubMed] [Google Scholar]