To the Editor: Eliminating a nidus was deemed to be the key to curing brain arteriovenous malformations (bAVMs). When conducting interventional embolization, it was suggested to superselect the microcatheter close to the nidus before injecting embolic agents. The traditional embolization was conducted via arterial approaches, which required the accessibility of arterial feeders. Difficulties and risks increased in the cases with lesions with narrow calibers, tortuous courses, or “en passage” arterial supplies. Transvenous approaches were proved to be safe and effective accesses in bAVM embolization without the limitations of arteries.[1] The current transvenous approaches were established through femoral and cervical veins. They had to face the essential challenges of the intracranial venous system in superselecting, such as high anatomic variability, extreme angle with tortuosity, and fragility of the vascular wall. A unique transvenous approach, which performed a direct puncture (DP) of the superficial draining vein (SDV) in the operative field, overcame the shortcoming above. It was first reported in an operation on superficial spinal arteriovenous fistula and acted as an emergency remedy for critical bleeding.[2] On the platform of one-stage hybrid operation, interventional and surgical procedures could be combined complementarily which could forestall the difficulties and limitations of each single method. The technique of DP-SDV was planned to establish a transvenous approach in the patients whose regular arterial and venous approaches were inaccessible. In our study, two bAVM patients were cured successfully by one-stage hybrid operations, in which transvenous embolization was implemented with DP-SDV technique. The technique was validated in both of the cases and induced the effective transvenous embolization of their lesions.
From January 2016 to December 2017, 151 cases with bAVMs were involved in a registered prospective cohort study (No. NCT03209804) for one-stage hybrid operation. Among them, two patients received one-stage hybrid operation with transvenous embolization using DP-SDV technique. The study was approved by the Research Ethics Committee of Beijing Tiantan Hospital (No. KY2016-034-02), and the patients gave written informed consent before participating.
Operative plans were decided after considerate discussion among neurosurgeons, endovascular physicians, neuroimaging specialists, and anesthetists. The basic operative indication included a history of hemorrhage or epilepsy caused by the lesion. The technical criterion was that ≥1 SDV could be exposed in the surgery field.
The DP-SDV technique was performed on the basis of one-stage hybrid operation in a hybrid operating theater, which was equipped with a ceiling-mounted monoplane X-ray system (Allura® FD20, Koninklijke Philips N.V., Best, the Netherlands), a neurosurgical operating microscope (Pentero® 900, Carl Zeiss Surgical AG, Oberkochern, Germany), a multifunction table (MAQUET Holding B.V. & Co. KG, Rastatt, Germany), and other basic auxiliary operative equipments. The fluoroscopic system was assisted with a neuroimage workstation (Interventional Workspot R1.4.1.10015, Philips Medical Systems Nederland B.V., Best, the Netherlands) for image processing. The operation was performed in a general endotracheal anesthesia status. A radiolucent carbon-fiber head brace (MAQUET Holding B.V. & Co. KG, Rastatt, Germany) was used for cranial immobilization. The skin incision and approach of neurosurgical operation were designed with a neuronavigation system (Brainlab® Cranial 3.0, Brainlab AG, Munich, Germany) to minimize the invasion. Electrophysiological conditions (somatosensory evoked potentials and motor evoked potentials) were monitored (Nicolet® Endeavor CR™ IOM, Natus Medical Incorporated, Pleasanton, CA, USA) by professionals. The detector of the monoplane was wrapped with a sterile cover during the operation. Rotations of the tube were limited strictly under the height of the operating table to ensure the sterility of the surgery field.
A 6-F femoral sheath (AVANTI® Introducer, Cordis Corporation, Miami Lakes, FL, USA) was used to set up a right femoral arterial approach with the Seldinger technique. A 6-F guiding catheter (Envoy®, Codman division of Johnson and Johnson Medical Ltd., Wokingham, Berkshire, UK) was catheterized into the feeding arteries through the sheath under the introduction of a guidewire (Radifocus® GuideWire M, Terumo Corporation, Tokyo, Japan). A digital subtraction angiography (DSA) was performed to acquire the location of the guiding catheter and the lesion. Heparin saline was dripping continuously into the femoral sheath and the guiding catheter to prevent lumens from thrombosis. To reduce the shifting of catheter tips during the surgical operation, all the exposed parts of instruments were fixated on the skin of the right thigh.
Candidate SDVs were exposed in a craniotomy with the guidance of neuronavigation. The target SDV was confirmed by real-time fluoroscopy, which provided the shortest pathway to the nidus. An 18-gauge indwelling needle (Introcan Safety®, B. Braun Melsungen AG, Melsungen, Germany) was used to puncture on the target SDV as close as possible to the nidus. After the stylet was withdrawn, a transvenous approach was established with the cannula remaining for the following transvenous manipulations. A transcannula DSA was performed manually for the confirmation. If the nidus was in the range of the cannula, liquid embolic agent (Onyx™18/34, eV3 Inc., Minneapolis, Minnesota, USA) was directly injected through it; otherwise, microcatheters were catheterized through the cannula into the nidus for safe embolization. The diffusion of the embolic agent should be noticed during the injection. It caused alarm if the glue diffused to the downstream part of SDV, exceeding the puncture point. Meanwhile, the injection was stopped if there was a risk of causing sinus embolism. An appropriate retrograde embolization of the nidus and feeders could decrease its blood flow volume and make the following surgical resection easier with less intraoperative bleeding. The cannula was temporarily closed with an aneurysmal clip (Aesculap® FT740T, Aesculap AG, Tuttlingen, Germany) and was removed with the lesion together. Before suturing the dura, the intraoperative color Doppler ultrasonography (Flex Focus® 800, BK Medical ApS., Mileparken, Herlev, Denmark) and DSA were performed to prevent any residue of the lesion.
Follow-up DSA and CT angiography (CTA) were systematically conducted in 6 months. Evaluations with the modified Rankin scale (mRS) were implemented at admission, discharge, 3-month follow-up, and 6-month follow-up.
Two male patients aged 6 and 29 years were involved in the study. They were in grade 2 and grade 3 of Spetzler-Martin (S-M) grading system, respectively. Details of the patients were illustrated in the following sections. Both patients received successful transvenous embolization with the DP-SDV technique. With the help of it, both of the patients had their bAVM resected completely with a blood loss ≤500 ml. No neural functional deterioration was induced by the operation. No hemorrhagic or ischemic complication occurred in the postoperative period. Both patients got a 0 score on mRS at discharge.
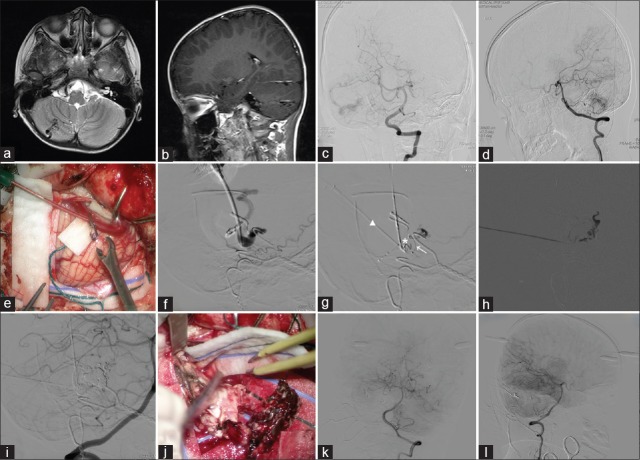
The first patient was a 6-year-old male patient with progressive grand mal epilepsy in the last 4 years. The physical examination did not show any abnormal result. A right cerebellar bAVM was revealed on magnetic resonance imaging (MRI) [Figure 1a and 1b]. According to results of the intraoperative DSA, the lesion was in grade 2 of S-M grading system. A partial embolization before surgery was suggested to reduce its blood flow volume. Considering the perioperative risks of embolization, one-stage hybrid operation was planned.
Figure 1.
The process of transvenous embolization with DP-SDV technique: Illustration of Case 1. (a) The axial view of cranial T2-weighted MRI. An abnormal vessel signal was revealed in the right cerebellar hemisphere. (b) The sagittal view of enhanced T1-weighted MRI. (c) The posteroanterior view of intraoperative DSA before embolization. The bAVM was supplied by branches of the right SCA, AICA, and PICA and was drained into right transverse sinus through dilated cerebellar superficial vein. (d) The lateral view of intraoperative DSA. (e) The target SDV was punctured with an 18-gauge dwelling needle under the microscope. Withdrawing the stylet, the cannula was fixated by an aneurysm clip. (f) A manual DSA through the cannula. The contrast agent diffused rapidly to the downstream part of SDV. (g) An glue embolus (*) formed on the tip of cannula and partially occluded the SDV. A new approach (△) was set up with DP-SDV technique. A microcatheter (↖) was catheterized into the nidus through the cannula. (h) The glue was injected through microcatheter under roadmap. After filling up the majority of nidus, the embolic agent went into the arterial feeders retrogradely. (i) DSA via the guiding catheter reserved in the right vertebral artery. A subtotal embolization was achieved before surgical resection. (j) The microsurgical resection of bAVM. A clear boundary was observed between the lesion and the normal brain tissue. The lesion was stripped off from the parenchyma easily. (k) The posteroanterior view of the final DSA. The bAVM was completely obliterated. (l) The lateral view of the final DSA. MRI: Magnetic resonance image; DSA: Digital subtraction angiography; bAVM: Brain arteriovenous malformation; SCA: Superior cerebellar artery; AICA: Anterior inferior cerebellar artery; PICA: Posterior inferior cerebellar artery; SDV: Superficial draining vein; DP-SDV: Direct puncture of superficial draining vein. *: The glue emboli; △: The new approach established by a cannula with DP-SDV technique; ↖: The microcatheter introduced through the cannula.
The operation was performed under general endotracheal anesthesia. A transarterial approach was established with the Seldinger technique on the right femoral artery. The three-dimension road map was acquired by conducting a 3-dimensional rotating angiography (3D-RA), which clearly revealed a right cerebellar bAVM of 3.1 cm × 3.2 cm × 2.2 cm in size with the feeders from the branches of the right superior cerebellar artery (SCA), anterior inferior cerebellar artery (AICA), and posterior inferior cerebellar artery (PICA). The lesion was drained into the right transverse sinus through SDVs [Figure 1c and 1d]. A 6-F guiding catheter (Envoy®, Codman division of Johnson & Johnson Medical Ltd., Wokingham, Berkshire, UK) was catheterized and reserved in the right cervical vertebral artery. After fixating the interventional instruments, the target SDV was exposed by a craniotomy with a posterior midline approach. An 18-gauge indwelling needle (Introcan Safety®, B. Braun Melsungen AG, Melsungen, Germany) was used for the establishment of the direct transvenous approach. A temporary occlusion clip (Aesculap® FT740T, Aesculap AG, Tuttlingen, Germany) was used to immobilize the cannula [Figure 1e]. Fluoroscopy was performed from both cannula and guiding catheter to verify the relative location between the cannula and the lesion. The contrast agent hardly distributed into the arterial feeders in the fluoroscopy through the cannula [Figure 1f]. A high blood flow volume of the lesion was suggested. We ventured to inject the embolic agent (Onyx™18, eV3 Inc., Minneapolis, Minnesota, USA) through the cannula directly to reduce the volume. However, it deposited around the cannula's tip due to the forward blood flow and formed an embolus partially obliterating the SDV [Figure 1g]. The injection was stopped immediately. Another DP-SDV approach was established in the upstream adjacently. To deliver the embolic agent effectively into the nidus, a microcatheter (Excelsior® SL-10, Stryker® Neurovascular, Fremont, CA, USA) was introduced through the new approach and catheterized into the nidus under the road map [Figure 1g]. Before the embolization, 0.5 ml of dimethyl sulfoxide (DMSO, eV3 Inc., Minneapolis, Minnesota, USA) was used to flush the microcatheter. A total of 3.0 ml of embolic agent (Onyx™18, eV3 Inc., Minneapolis, Minnesota, USA) was injected discontinuously under the roadmap [Figure 1h]. A subtotal embolization of the lesion was revealed in the following fluoroscopy through the guiding catheter [Figure 1i]. After withdrawing interventional instruments, clips were used to close the puncture points. Afterward, microsurgical resection was performed. A clear boundary was observed between the lesion and the normal parenchyma [Figure 1j]. The lesion was stripped off easily from the cerebellum tissue within 46.7 min. No residue of bAVM was found in the following DSA [Figure 1k and 1l]. The operation lasted 5.5 h, with 500 ml of intraoperative hemorrhage. The patient was discharged 6 days after the operation without any neural functional deficit. No complication occurred during hospitalization. The mRS score at discharge was 0.
The second patient was a 29-year-old male patient who presented with a sudden visual impairment 9 years ago. A hematoma was revealed on the right occipital lobe and was evacuated emergently in the local hospital. In the operation, a bAVM was found adjoined to the hematoma and remained. Follow-up MRI revealed a bAVM of 3.0 cm × 2.1 cm × 2.5 cm close to the visual cortex. The lesion rooted from the cortex to the posterior horn of the lateral ventricle. The visual field test showed a homonymous hemianopia on the left. According to results of the intraoperative DSA, the lesion was in grade 3 of S-M grading system.
The hybrid operation was performed under general endotracheal anesthesia. A transarterial approach was established first with the Seldinger technique on the right femoral artery. Through DSA, the bAVM was clearly revealed on the right occipital lobe and fed by branches of the right posterior cerebral artery and right middle cerebral artery. Its nidus was drained into the superior sagittal sinus through two dilated superficial veins. A 6-F guiding catheter (Envoy®, Codman division of Johnson & Johnson Medical Ltd., Wokingham, Berkshire, UK) was catheterized into the right cervical vertebral artery and indwelled with heparin saline instilled continually. A craniotomy was designed and performed with the assistance of neuro-navigation. The SDV was exposed in the operation and punctured with an 18-gauge indwelling needle (Introcan Safety®, B. Braun Melsungen AG, Melsungen, Germany) microscopically. The blood flow of SDV was controlled by an aneurysm clip (Aesculap® FT740T, Aesculap AG, Tuttlingen, Germany) distal to the cannula. The bAVM and its SDV were double-checked by DSAs via both cannula and guiding catheter. As the SDV was found close to the nidus, the cannula was delivered directly into the nidus. After flushing the cannula with 0.1 ml of DMSO (eV3 Inc., Minneapolis, Minnesota, USA), Onyx™18 (eV3 Inc., Minneapolis, Minnesota, USA) was injected into the nidus intermittently under the roadmap. Once the embolic agent was infusing into the arterial feeders, the injection was paused to prevent any implication of normal arteries. The process was repeated until the nidus and abnormal feeders were embolized as much as possible. In total, 1.5 ml of the embolic agent was injected in the procedure. After withdrawing the cannula, the aneurysm clip was replaced on the puncture point to close the approach. Subsequently, the lesion was resected microsurgically within 30 min. The following DSA confirmed the total resection of the bAVM. The operation took 5.6 h, with a blood loss of 400 ml. The patient was discharged 7 days after the operation without any deficit of neurological function, visual acuity, or visual field.
With the rapid development of endovascular interventions, different techniques have been proposed to improve the safety and efficiency. However, traditional approaches have limited its improvement. The long distance between the puncture point and lesion, as well as the tortuosity, made it difficult to superselect the microcatheter into the target artery through femoral and radial approaches. Although the transcarotid approach could shorten the distance, it would increase the risk of related complications.[3] In the first case, although the lesion was fed by the branches of SCA, AICA, and PICA, it was difficult to implement the embolization through any traditional transarterial approaches. The long routing distance of SCA would decrease the controllability of the microcatheter. The caliber of the PICA limits its tolerance of a microcatheter. Moreover, the tortuosity at the initial part of the AICA makes it difficult to both catheterize and manipulate the instruments. The traditional approaches are trapped in this case. By the support of the one-stage hybrid operation, the DP-SDV technique was innovated to solve this problem. The shortcut approach could reduce the difficulties in both catheterizing and manipulating. Meanwhile, as the lesion was already exposed, surgical measures could be taken promptly if any adverse event happened.
Although the procedures were performed satisfactorily as planned, they could be improved for more safety and efficiency. First, specialized instruments should be specifically designed. Adverse events could be caused by any inappropriate manipulation, such as the injury or thrombosis of the vein and damage to the brain parenchyma. A specifically designed sheath and instrument would decrease the incidence of the adverse events above and improve the workflow. Second, cooperating with transarterial manipulations could improve the result of embolization. In cases with high blood flow, a balloon catheter could be dilated in the trunk of the ipsilateral feeding artery to reduce the flow for a safer transvenous embolization.
The cooperation between microsurgical operation and endovascular intervention has existed for decades. Although it achieved some successes in curing the complex bAVMs, the essential risks of such a cooperation should not be neglected, especially bleeding during the intervention and interval periods.[4] As equipment has developed, one-stage hybrid operations have improved our understanding of the complex bAVMs. In the new cooperation mode, the risks and shortcomings of each traditional method could be complemented by combining them. Moreover, novel operative techniques, the DP-SDV, for example, could provide more choices for the treatment of bAVMs.
DP-SDV proved to be practicable in setting up a novel transvenous approach for the embolization of bAVMs in one-stage hybrid operations. By setting up a shorter and direct-viewing approach, the shortcomings of traditional approaches were overcome. With a more thorough understanding of one-stage hybrid operating techniques, innovative methods will be proposed in the treatment of bAVMs.
Declaration of patient consent
The authors certify that they have obtained appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by grants from the Beijing Municipal Science and Technology Project (No. D161100003816005) and the National Key Technologies R&D Program of China (No. 2016YFC1301800).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Iosif C, Mendes GA, Saleme S, Ponomarjova S, Silveira EP, Caire F, et al. Endovascular transvenous cure for ruptured brain arteriovenous malformations in complex cases with high spetzler-martin grades. J Neurosurg. 2015;122:1229–38. doi: 10.3171/2014.9.JNS141714. doi: 10.3171/2014.9.JNS141714. [DOI] [PubMed] [Google Scholar]
- 2.Shin HK, Suh DC, Jeon SR. Intraoperative direct puncture and embolization (IOPE) using a glue material for spinal cord arteriovenous fistula: A case report. Eur Spine J. 2015;24(Suppl 4):S594–9. doi: 10.1007/s00586-015-3773-9. doi: 10.1007/s00586-015-3773-9. [DOI] [PubMed] [Google Scholar]
- 3.Gupta P, Rath GP, Banik S, Mahajan C. Increased airway pressure due to superior mediastinal hematoma during endovascular coiling by transcarotid approach. J Clin Anesth. 2016;30:63–5. doi: 10.1016/j.jclinane.2015.12.039. doi: 10.1016/j.jclinane.2015.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Gruber A, Bavinzski G, Kitz K, Barthelmes S, Mayr M, Knosp E, et al. Multimodality management of cerebral arteriovenous malformations with special reference to AVM-related hemorrhages during ongoing staged treatment. Acta Neurochir Suppl. 2016;123:153–8. doi: 10.1007/978-3-319-29887-0_22. doi: 10.1007/978-3-319-29887-0_22. [DOI] [PubMed] [Google Scholar]