Abstract
Hives is an erythematous and itchy disease that commonly affects the trunk and the organs. Acute urticaria is a common disease and affects about 10%–20% of the population during its lifetime. In patients with chronic urticaria, about 25%–30% of cases, antithyroid peroxidase (TPO) was detected and Hashimoto's disease was diagnosed. This study aimed to evaluate the anti-TPO antibody in patients with chronic urticaria and the effect of treatment of levothyroxine on its recovery. In this study, 72 people with chronic urticaria and positive anti-TPO antibody were randomly divided into two groups. Low-dose antihistamine was administered to both groups, and the first group received levothyroxine at a dose of 50 μg/day. The severity of itching was evaluated according to the visual analog scale before and after therapy. There was no significant difference in the age, sex, thyroid-stimulating hormone (TSH), and anti-TPO between the two groups. Ninety-two patients were female. In this study, all patients took a small dose of loratadine. Relative healing was observed in both the groups. However, in a group of patients taking levothyroxine and loratadine, recovery was faster and patients with no itching were significantly more likely than the other groups. The prevalence of chronic urticaria and anti-TPO antibody in this study was very high and was due to sex hormones. Therefore, in young women with chronic urticaria, especially in refractory cases, they should be monitored for anti-TPO. Anti-TPO and TSH should be evaluated for the diagnosis and treatment of patients with urticaria or chronic angioedema. Levothyroxine therapy in hives and chronic urticaria is beneficial in the treatment of thyroid dysfunction.
Keywords: Anti-TPO antibody, autoimmune thyroiditis, chronic urticaria, levothyroxine, thyroid
INTRODUCTION
Chronic urticaria is one of the most common skin complaints according to the American College of Allergy, Asthma and Immunology; about 20% of people have experienced hives in their lives at least once in their lifetime.[1] Hives, caused by the secretion of antihistamines in the body by the immune system, can affect the quality of life.[2] Urticaria that lasts for more than 6 weeks (continuous or repeated) is called chronic.[2,3] For some people, chronic urticaria is caused by allergies, but for others, there is no diagnostic cause.[2] Chronic urticaria, which has no known cause, is called chronic idiopathic urticaria.[2,4] However, in many cases, there are ways to reduce chronic itching of urticaria. Stress can increase the severity of itching of the skin and can cause the skin to be susceptible to eczema, psoriasis, acne, hives, and other types of rash (skin lesions).[5] Chrousos showed the relationship between the nervous system and skin inflammatory disorders.[6] His research showed that stress results in the release of chemicals from the nerve endings of the skin, which affects how the body responds to important functions. These chemicals lead to inflammation of the skin.[6] One of the causes of chronic urticaria is hyperthyroidism. Hyperthyroidism triggers the activation of kinins and then chronic urticaria.[7] Kinin is a group of substances formed in the body tissue in response to injury. They are polypeptides and cause vasodilation and smooth muscle contraction.[7] In patients with chronic urticaria, about 25%–30% of cases, antithyroid peroxidase (TPO) was detected and Hashimoto's disease was diagnosed.[7,8] Recent research has focused on the role of autoimmune diseases in recent years.[9] The role of autoimmune thyroid disease is more pronounced. The cause of chronic urticaria in autoimmune thyroid is still unknown. Studies have also shown that thyroid hormone is effective in improving hives and/or chronic urticaria with thyroid autoimmunity.[7,9] The association between chronic urticaria and autoimmune thyroid disease has been evaluated with different results.[9,10] This study aimed to evaluate the effect of levothyroxine on the treatment of patients with autoimmune thyroid disease and chronic urticaria.
MATERIALS AND METHODS
In this study, 72 people with chronic urticaria and positive anti-TPO antibody were selected. Patients were randomly divided into two groups. Thyroid-stimulating hormone (TSH) was measured in all the patients. Patients with clear thyroid dysfunction were excluded from the study, and patients were mostly euthyroid or subclinical hypothyroidism. Levothyroxine was administered at a dose of 50 μg/day for 3 months to patients group (36 patients) and placebo was administered to the control group (36 people). All patients were taking low-dose antihistamines, tablet loratadine 10 mg/day. Ethically, we could not stop the antihistamines of patients. The severity of itching was evaluated according to the visual analog scale before and after therapy. The visual analog scale is a measurement tool that can measure different parameters such as itching or pain that cannot be easily measured. It is often used in epidemiologic and clinical research to measure the intensity or frequency of various symptoms. This study was registered at the Iranian Center for Clinical Trials (Iranian Registry of Clinical Trials), No. IRCT2014112613612N3. Statistical analysis was performed using SPSS Statistics for Windows, Version 21 (Armonk, NY: IBM Corp). The data are shown as mean ± standard deviation and 95% confidence interval. Independent t-test was used to check the difference between the means of two groups. Chi-square test was used to determine the statistical difference in qualitative variables. P < 0.05 was considered statistically significant.
RESULTS
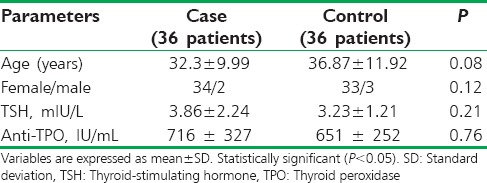
In this study, 72 people with chronic urticaria enrolled and 9 of them refused to continue and were excluded. Patients were randomly divided into two equal groups. Demographic data and laboratory parameters of patients in both the groups are summarized in Table 1. As shown in Table 1, there was no significant difference in the age, sex, TSH, and anti-TPO between the two groups. All patients with clear thyroid dysfunction were excluded, and patients in this study were mostly euthyroid or subclinical hypothyroidism.
Table 1.
Demographic data and laboratory parameters of patients in both the groups
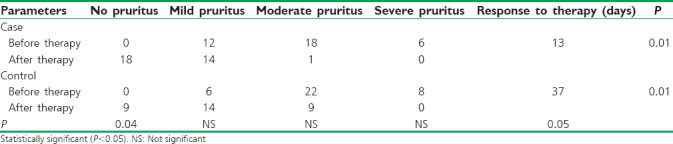
Patients in the case group received levothyroxine and loratadine and patients in the control group received loratadine alone. Three patients in the case group and six patients in the control group were excluded. The severity of itching was evaluated according to the visual analog scale before and after therapy. Itching was divided into three degrees: mild, moderate, and severe. As shown in Table 2, itching in the mild, moderate, and severe degrees was 12, 18, and 6, respectively in the case group, and after treatment, nonitching point was observed in 18 patients. However, in the control group, nonitching point was observed in nine patients (P = 0.04). The response rate to treatment in the case group was significantly higher than the control group, and the recovery time was shorter.
Table 2.
The degree of pruritus before and after treatment in two groups
DISCUSSION
The relationship between chronic urticaria and autoimmune thyroid diseases has been observed since 1983, when the patient with urticaria and thyroiditis was described by Midelfart et al.[11] The prevalence of chronic urticaria in women is twice than that in men.[12] Changes in sex hormone in woman can change the severity of urticaria. Changes in hormones are seen following the onset of menstrual cycle, pregnancy, menopause, and autoimmune thyroid disorders.[12] A hypersensitivity reaction to female sex hormones may stimulate the immune system and cause hives.[12] In this study, the number of women was much higher than men. Number of women in our study is more than men, because we chose women with chronic itching plus positive anti-TPO.
In many studies, it has been reported that the prevalence of anti-TPO in patients with chronic urticaria is higher than the general population.[13] The prevalence of anti-TPO in the general population is 3%–6%, while the incidence in patients with chronic urticaria is reported to be 17.7%–29%[13,14,15,16] Our patients in this study were euthyroid and only had anti-TPO antibody positive. Some of them had subclinical hypothyroidism.
In this study, all patients took a small dose of loratadine. Relative healing was observed in both the groups. However, in a group of patients taking levothyroxine and loratadine, recovery was faster, and patients with no itching were significantly more likely than the other group. On the other hand, in this study, patients who received levothyroxine had a shorter recovery time. In some studies, the positive effect of levothyroxine on chronic urticaria has been reported.[10,17,18] One study indicated that levothyroxine administration in chronic urticaria and anti-TPO positive improved itching.[17] According to this study and other studies, administration of levothyroxine in patients with chronic urticaria leads to faster recovery. A study by Zauli et al. had suggested that patients with chronic urticaria should be measured anti-TPO and TSH levels.[19] Chronic urticaria can be associated with autoimmune thyroid disease. Patients who have not been found to have a cause for chronic urticaria should be required to measure TSH and anti-TPO. The assessment of thyroid function test alone is not enough and anti-TPO should be measured because TSH is usually normal, but anti-TPO may be positive.
CONCLUSION
Anti-TPO and TSH should be evaluated for the diagnosis and treatment of patients with urticaria or chronic angioedema. Levothyroxine therapy in hives and chronic urticaria is beneficial in the treatment of thyroid dysfunction.
Ethical approval
The study protocol was approved by the Ethics Committee of Tabriz University of Medical Sciences, Tabriz, Iran. The current study was performed according to the Institutional Committee for the Protection of Human Subjects, which was adopted by the 18th World Medical Assembly, Helsinki, Finland, and its later amendments.
Financial support and sponsorship
This study was financially supported by Tabriz University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lieberman P, Camargo CA, Jr, Bohlke K, Jick H, Miller RL, Sheikh A, et al. Epidemiology of anaphylaxis: Findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol. 2006;97:596–602. doi: 10.1016/S1081-1206(10)61086-1. [DOI] [PubMed] [Google Scholar]
- 2.Kasperska-Zajac A, Sztylc J, Machura E, Jop G. Plasma IL-6 concentration correlates with clinical disease activity and serum C-reactive protein concentration in chronic urticaria patients. Clin Exp Allergy. 2011;41:1386–91. doi: 10.1111/j.1365-2222.2011.03789.x. [DOI] [PubMed] [Google Scholar]
- 3.Młynek A, Zalewska-Janowska A, Martus P, Staubach P, Zuberbier T, Maurer M, et al. How to assess disease activity in patients with chronic urticaria? Allergy. 2008;63:777–80. doi: 10.1111/j.1398-9995.2008.01726.x. [DOI] [PubMed] [Google Scholar]
- 4.Greaves M. Chronic urticaria. J Allergy Clin Immunol. 2000;105:664–72. doi: 10.1067/mai.2000.105706. [DOI] [PubMed] [Google Scholar]
- 5.Arck P, Paus R. From the brain-skin connection: The neuroendocrine-immune misalliance of stress and itch. Neuroimmunomodulation. 2006;13:347–56. doi: 10.1159/000104863. [DOI] [PubMed] [Google Scholar]
- 6.Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5:374–81. doi: 10.1038/nrendo.2009.106. [DOI] [PubMed] [Google Scholar]
- 7.Verneuil L, Leconte C, Ballet JJ, Coffin C, Laroche D, Izard JP, et al. Association between chronic urticaria and thyroid autoimmunity: A prospective study involving 99 patients. Dermatology. 2004;208:98–103. doi: 10.1159/000076480. [DOI] [PubMed] [Google Scholar]
- 8.Concha LB, Chang CC, Szema AM, Dattwyler RJ, Carlson HE. IgE antithyroid antibodies in patients with Hashimoto's disease and chronic urticaria. Allergy Asthma Proc. 2004;25:293–6. [PubMed] [Google Scholar]
- 9.Yavari A, Najafpoor F, Aliasgarzadeh A, Niafar M, Mobasseri M. Effect of aerobic exercise, resistance training or combined training on glycaemic control and cardiovascular risk factors in patients with type 2 diabetes. Biol Sport. 2012;29:135. [Google Scholar]
- 10.Magen E, Mishal J. The effect of L-thyroxine treatment on chronic idiopathic urticaria and autoimmune thyroiditis. Int J Dermatol. 2012;51:94–7. doi: 10.1111/j.1365-4632.2011.05172.x. [DOI] [PubMed] [Google Scholar]
- 11.Midelfart K, Moseng D, Kavli G, Stenvold SE, Volden G. A case of chronic urticaria and vitiligo, associated with thyroiditis, treated with PUVA. Dermatologica. 1983;167:39–41. doi: 10.1159/000249743. [DOI] [PubMed] [Google Scholar]
- 12.Kasperska-Zajac A, Brzoza Z, Rogala B. Sex hormones and urticaria. J Dermatol Sci. 2008;52:79–86. doi: 10.1016/j.jdermsci.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Czarnecka-Operacz M, Bator-Wegner M, Silny W. Atopy patch test reaction to airborne allergens in the diagnosis of atopic dermatitis. Acta Dermatovenerol Croat. 2005;13:3–16. [PubMed] [Google Scholar]
- 14.Kaplan A, Greaves M. Pathogenesis of chronic urticaria. Clin Exp Allergy. 2009;39:777–87. doi: 10.1111/j.1365-2222.2009.03256.x. [DOI] [PubMed] [Google Scholar]
- 15.Mobasseri M, Yavari A, Najafpoor F, Aliasgarzadeh A, Niafar M. Effect of a long-term regular physical activity on hypertension and body mass index in type 2 diabetes patients. J Sports Med Phys Fitness. 2015;55:84–90. [PubMed] [Google Scholar]
- 16.Turktas I, Gokcora N, Demirsoy S, Cakir N, Onal E. The association of chronic urticaria and angioedema with autoimmune thyroiditis. Int J Dermatol. 1997;36:187–90. doi: 10.1046/j.1365-4362.1997.00187.x. [DOI] [PubMed] [Google Scholar]
- 17.Karaayvaz M, Calişkaner Z, Turan M, Akar A, Oztürk S, Ozangüç N, et al. Levothyroxine versus ketotifen in the treatment of patients with chronic urticaria and thyroid autoimmunity. J Dermatolog Treat. 2002;13:165–72. doi: 10.1080/09546630212345673. [DOI] [PubMed] [Google Scholar]
- 18.Kiyici S, Gul OO, Baskan EB, Hacioglu S, Budak F, Erturk E, et al. Effect of levothyroxine treatment on clinical symptoms and serum cytokine levels in euthyroid patients with chronic idiopathic urticaria and thyroid autoimmunity. Clin Exp Dermatol. 2010;35:603–7. doi: 10.1111/j.1365-2230.2009.03642.x. [DOI] [PubMed] [Google Scholar]
- 19.Zauli D, Grassi A, Ballardini G, Contestabile S, Zucchini S, Bianchi FB, et al. Thyroid autoimmunity in chronic idiopathic urticaria: Implications for therapy. Am J Clin Dermatol. 2002;3:525–8. doi: 10.2165/00128071-200203080-00002. [DOI] [PubMed] [Google Scholar]


