Abstract
Objective
Cell phone text messaging reminders offers the promise of an efficient technology for the management of chronic diseases, such as asthma. This review aims to evaluate the effectiveness of text message reminders in improving medication adherence for asthma compared to usual care.
Methods
Randomized controlled trials assessing the effect of text message reminders on adherence to asthma medication were identified from PubMed, Medline, Web of Knowledge EBSCOhost, OvidSP, PsycINFO, and Cochrane Central Register of Controlled Trials and Cochran Health Technology Assessment databases. Literature searches were restricted to the English language, and no restrictions were imposed on the year and country of publication.
Results
Five studies that were deemed relevant to the systematic review were identified from the literature search. Findings on whether text message reminders improve medication adherence were mixed. However, the review indicates that text-messaging interventions were effective as a means of addressing forgetfulness by reminding patients to take their medications.
Conclusion
This review adds to the body of literature reviewing the effectiveness of emerging technologies in the management of diseases. Despite the fact there is limited evidence across the population of studies to support the effectiveness of text message reminders, such technology represents an important tool to achieve optimal medication adherence among asthmatics.
Keywords: Text messaging, short message service, medication adherence, asthma, systematic review
INTRODUCTION
The number of people with asthma continues to grow worldwide.1 According to the Centers for Disease Control and Prevention, 1 in 13 people has asthma.2 Each day, ten Americans die from asthma, and in 2015, 3,615 people died from asthma. Many of these deaths are avoidable with proper treatment and care.2, 3 Medical and absenteeism costs of asthma represent a significant economic burden for states, and these costs are expected to rise.4, 5 The annual economic cost of asthma is more than $81.9 billion in the U.S. – including medical costs and loss of work and school days in 2013.6 Treatment of asthma is achieved through medications that can be administered using different delivery devices, with diverse therapeutic mechanisms of action.
The World Health Organization defines adherence as “the extent to which the person's behavior (including medication-taking) corresponds with agreed recommendations from a healthcare provider.”7 Medication adherence includes the initiation of the treatment, implementation of the prescribed regimen, and discontinuation of the pharmacotherapy.8 Assessments of adherence rates to asthma medications show variable results due to the wider variations in methods used. However, there is a broad agreement that poor medication adherence is a common occurrence among adults and children with asthma.9 Poor adherence to asthma medication has also been linked to successive hospitalizations, as well as increased morbidity and mortality.10 Despite the controversy regarding the exact number, the reported rates of non-adherence range from 30 to 70 percent,11 and about 50 percent of the time asthma patients receiving long-term therapy fail to take their medication as prescribed.7
Several theories have been suggested to explain the reason some individuals with asthma may be non-adherent to their medication regimen. Adherence to asthma medication is influenced by complex socioecological and psychological factors,12 and non-adherence may be intentional or unintentional.13 Intentional non-adherence can be attributed to beliefs, emotions, and preferences.14 For instance, if patients perceive the cost/burden of taking medicine to outweigh the benefit, the patient may hesitate to continue taking medications as prescribed.15 Unintentional non-adherence is linked to limitations in capacity, forgetfulness, or resource constraints.14 For instance, if patients perceive the cost/burden of taking medicine to outweigh the benefit, they may intentionally not adhere to medication prescribed.15 Healthcare professionals have found the importance of learning about the individual's behavior, cultural beliefs, financial ability to purchase medication, and knowledge of asthma when trying to improve adherence.16 While cultural factors and individual characteristics play a role in adherence, forgetfulness is one factor that can be easily influenced.17 Thus, a means to remind patients to take their medicine and to refill their prescription may be an effective way to overcome the obstacles of “forgetfulness.”18, 19
Asthma is a condition for which effective self-management has been shown to improve the patient's quality-of-life and also reduce the persistence and progression of the disease.20 The behavioral strategy of self-management component directly uses techniques such as reminders, contracting, and reinforcement.21 The reminder techniques are found to be significant in increasing medication adherence.22 In recent years, text messages, also known as Short Messaging Services (SMS) based interventions have emerged as a strategy to improve health outcomes and individual health behaviors.23, 24 The increase in cellular phone usage drives the suitability of text messages reminders, with 95% of the American population owning a cellular phone of some kind.25 Typically, text messages are delivered to the individual's cellular phone either once a day or multiple times per day to remind them to take their medication at the prescribed time. The text message might prompt the user for a response, as this has been shown to improve compliance with medications in several chronic conditions.
Text message reminders are reported to be innovative, less costly and effective methods for improving medication adherence. The effectiveness of text message reminders in increasing medication adherence was shown in studies for HIV,26 malaria,27 oral contraceptive use,28 and sunscreen application.29 Evaluating the effectiveness of text message reminders for medication use as an intervention could provide insight to providers as to whether this method is worth adopting. Furthermore, reminders may help increase medication adherence, improve health outcomes, and decrease healthcare costs. The objective of this systematic review is to evaluate the impact of text message reminders on medication adherence among patients with asthma.
METHODS
Search Strategy
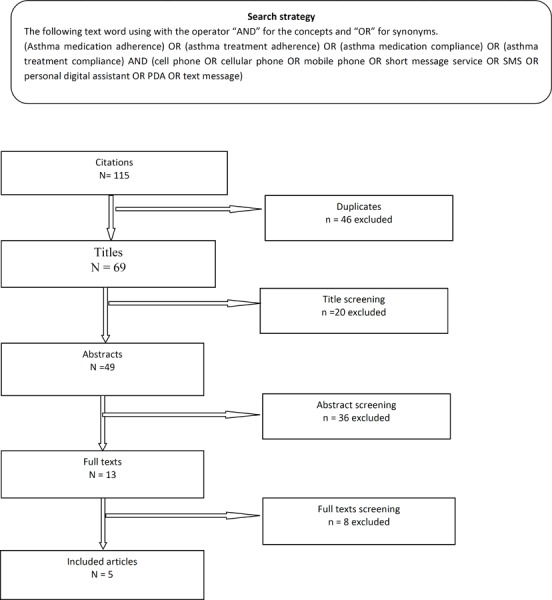
To identify text messages reminders and asthma medication adherence studies, the following electronic databases were searched without considering dates of publication: PubMed, Medline, Web of Knowledge EBSCOhost, OvidSP, PsycINFO, and Cochrane Central Register of Controlled Trials and Cochran Health Technology Assessment databases. Electronic database search was supplemented by manually searching the reference lists of articles that were retrieved electronically to identify additional studies. The keywords used to identify the relevant articles are listed in Figure 1. The authors evaluated each of the articles independently for inclusion based on the preset criteria and they resolved disagreements by discussion.
Figure 1. Article selection process.
Inclusion Criteria
Randomized studies and before-and-after studies on text message reminders for asthma medication adherence were included. The text message reminders were to be sent to the patient by means of integrated automated services or directly by health professionals. No study was excluded based on date and country of publication. Only studies that were published in English were considered. Studies must have reported the impact of text message reminders on asthma medication adherence compared to other interventions such as usual care, counseling, phone call reminders, etc. The primary outcome measured by the study had to be medication adherence. Medication adherence could be assessed either as direct or indirect measures. The direct medication adherence includes measurement of the level of medication or metabolite in the blood and measurement of the biological marker in the blood.30 The indirect medication adherence includes patient self-reported, pill count, rates of prescription refill, patients' diaries, clinical response, and others.30 This review included people of all ages that were clinically diagnosed with asthma.
Data and Analysis
First, the title and abstract of retrieved studies were screened for relevance. Second, full-text papers were examined to assess fulfillment of the inclusion criteria. Figure 1 provides detailed information about the numbers of studies identified, included and excluded and the reasons for exclusion.
RESULTS
Study Characteristics
A total of 115 articles was initially retrieved from the literature search. Of the 115 titles reviewed, 5 were deemed relevant for full-text screening. The characteristics of selected studies are presented in Table 1.
Table 1. Overview of Included Studies.
| Study | Purpose | Study population | Study design | Outcome measures | Result |
|---|---|---|---|---|---|
| Britto, et al. 2012 | To assess the feasibility, acceptability, and utility of a text messaging system that allowed teenagers with asthma to generate and control medical reminders sent to their mobile phones. | N = 19 older than 12 years old teens who were diagnosed with asthma. SMS group (N=12) and control group (N=7) |
◯ X ◯ ◯ ◯ |
Feasibility, acceptability, and utility of the text messaging system. Clinical measure of asthma symptom control | The study group rated the usefulness (remembering to take medication) of the text reminders very highly and expressed high level of satisfaction No conclusion if the text message improved adherence |
| MacDonell et al., (2016) | To conduct a randomized controlled pilot of a multicomponent, technology-based intervention promoting adherence to controller medication in African-American emerging adults with asthma. | Participants (N = 49) were 18-29 years old, African-American, with persistent asthma requiring controller medication. | X ◯ | Ecological Momentary Assessment via two-way text messaging was also used to collect “real-time” data on medication use and asthma control. | The intervention is feasible and effective. However, findings are preliminary and should be replicated with a larger sample and more sophisticated data analyses. |
| Ostjic V, et al., (2005) | This study examined the Global System for Mobile Communications (GSM) short-message service (SMS) as a means of telemedicine in peak expiratory flow (PEF) measurement. | 16 patients, SMS group (N = 8) and control group (N = 8) | R O X O R O O |
Asthma cough, night symptoms FEV daily dose ICS, and FEV daily does lab |
No significant difference between groups in medication compliance/adherence |
| Petrie et al. (2012) |
To investigate if a text message reminder targeted at changing a patients' illness and medication beliefs would improve adherence in young patients with asthma. | Patients aged between 16 and 45 years. Text message intervention (N= 73) and control group (n=74) |
R ◯ X ◯ R ◯ ◯ |
Self-reported adherence Medication belief and asthma control belief | Improved adherence for the follow-up period compared to the control group. Showed improvement in medication and asthma control belief. |
| Strandbygaard et al. (2009) | Examined the impact of receiving a daily text message reminder on one's cell phone on adherence to asthma treatment. | Patients aged between 18 to 45. SMS reminder intervention group (n= 12) and control group (n=14) | R ◯ X ◯ R ◯ ◯ |
Adherence rate to asthma treatment. Reimbursement of asthma medication. Change in exhaled nitric oxide levels, lung function and airway responsiveness |
Improve asthma medication usage, but no change was observed between intervention and control group in reimbursement of asthma medication, change in exhaled nitric oxide levels, lung function and airway responsiveness |
Caption: R O is randomized control trial and O is non-randomized control trial
FVE is forced expiratory volume
ICS is inhaled corticosteroids
Study Outcomes
Britto et al., 2012 examined the feasibility, acceptability, and utility of a text messaging system for teenagers with asthma.31 This text message system was used as means to allow teenagers to control and generate their own medication reminders sent through mobile phones. All 23 eligible patients were assigned to either the intervention or the control group, with 19 of the 23 participants completing the study. The method employed by this study placed 12 teenagers into a study group where the teenagers were able to create and control the text messages. The study did not conclude on whether or not the text messages improved adherence to the asthma medication.
Ostojic et al., 2005 assessed the used of text message reminders as a novel means of telemedicine in peak expiratory flow (PEF) monitoring.32 In their study, 16 asthma patients were randomly assigned to either the SMS group (N = 8) or the control group (N = 8). After a 16-week follow-up period, the study concluded that the study group (receiving SMS) better controlled their asthma. Although patients were compliant in reporting daily PEF, the daily medication adherence was poor. There was no significant difference between the SMS group and the control group in medication adherence. In the SMS group, the value of forced expiratory volume in one second (FEV1), increased (81.25±17.31 vs. 77.63±14.08, p = 0.014) whereas, the control group showed no change. No significant pre-treatment or post-treatment difference was observed between the group receiving text messages and the control group in the mean FEV1. In comparison to the group receiving text message, the control group had higher symptom scores but not for wheezing or limitation of activity.
Strandbygaard, et al., 2009 assessed the impact of receiving daily cell phone text reminders on adherence to asthma treatment.33 In their study, participants were recruited using a local newspaper, and 54 participants responded to the advertisement. The inclusion criteria included a diagnosis of asthma based on clinical history and daily symptoms, ranging from ages of 18 to 45, and positive methacholine challenges test with PD20 ≤ 4µmol. Participants with other comorbidities and smoking history more than 10 years were excluded from participating in the study. After the exclusions, 30 participants met the inclusion criteria and were enrolled in the 3 months follow-up study. The study group consisted of 26 patients between the ages of 18 and 45 years of age, who received daily text messages. The investigator monitored the patients with 3 clinical examinations at week 0, 4, and 12. At week 0, all patients received 1 dose twice daily of the following treatments: inhaled corticosteroids (ICS), and long-acting β2 – agonist (LABA), in combination. All participants received education on the necessity of treatment, knowledge of the disease's mechanisms, and correct inhaler technique. At week 4, the patients were randomly assigned to either the intervention group [receiving SMS every day at 10 a.m until week 8 (N= 12)] or the control group [i.e., not receiving SMS (N= 14)]. Each group had 2 participants who did not complete the study. At week 4, all participants received a prescription for their treatment. Between weeks 8 and 12, the participants were asked to bring their asthma medication for dose count (i.e., to measure adherence). The visits also included an interview by the author, a measurement of nitric oxide, lung function, and airway responsiveness to inhaled methacholine. Adherence rates in the text message group increased from 77.9% in week 4 to 81.5% in week 12. This is in contrast to the control group, in which a decrease in adherence was observed (e.g., 84% to 70%) during the same time frame. The authors indicated that the text message reminders might lead the participants to have a higher awareness of asthma control by implementing the awareness in their daily routine. The study was limited by a small sample size and a short follow up period. A longer follow up period may be required before any unambiguous conclusions.
Petrie et al., 2011 investigated whether text message reminders targeted at changing patients' illness and medication beliefs would improve adherence in young asthma patients by.34 The study focused on 216 patients between the ages of 16 and 45 who responded to an advertisement. However, only 147 patients were eligible and received the consent form and baseline questionnaire. Eligible patients were randomly assigned to either the study group (SMS group) or the control group (usual care). The study group received text messages for a total of 18 weeks. At the 18-week follow up, the SMS group showed improvement in adherence, as well as asthma-control belief compared to the control group. Improved adherence for the follow-up period compared to the control group showed an improvement in medication adherence and asthma control belief.
MacDonell et al., 2016 conducted a pilot study of a multicomponent, technology-based intervention promoting medication adherence in African-American emerging adults.35 The program studied clinically significant differences in adherence of patients with personalized adherence text messages received by the intervention group verses generic text messages received by the control group. Patients from the age of 18 to 29 years of age, African American, clinically diagnosed asthma with prescribed asthma controller medication, cellphone with texting, <80% adherence in the past 30 days, and Asthma Control Test score of score >19 were included in the study. Exclusion criteria included pregnancy, inability to understand written or spoken English, having another serious medical condition requiring regular medication, and/or an active psychiatric disorder that would interfere with study participation. A total of 49 patients were randomized into control group (N=24) and intervention group (N=25). The study found that changes in medication adherence and asthma control from pre- to post intervention favored the intervention, particularly for decrease in asthma symptoms, t (42) = 2.22, p < .05 (Cohen's d = .071). The authors also highlighted that the study is a pilot, and the outcomes may change should it be replicated with a larger sample size, and an advanced analytical approach.
Discussion
The purpose of this systematic review was to evaluate the effectiveness of text message reminders on medication adherence among patients with asthma subscribed to text messages compared to those not subscribed. In the reviewed studies, the intervention group received a text message reminder on daily prompting to take medication as prescribed. Findings from this systematic review indicate that there are limited data on the effectiveness of text message reminders for improving patients' adherence to asthma medication. Despite limited data, evidence to date suggests that text message reminders are an important tool to achieve optimal medication adherence among asthmatics.
The findings are also supported by another review.36 While both systematic reviews are similar with coinciding conclusions, there are differences to be noted. Tran et al. focused their analysis on several forms of telemedicine reminders such as pagers, text messages, and telephone calls; whereas, our study focused on just the impact of text message reminders.36 The primary endpoint for both systematic reviews was medication adherence; however, Tran et al. also evaluated long-term outcomes such as quality of life, symptom control, pulmonary function, and perceptions of illness. While Tran et al. concluded no benefits in improving quality of life, symptom control, or pulmonary function with telemedicine reminders, both systematic reviews are in agreement that adherence of asthma medications can be improved with the use of text message reminders.
The use of text message reminders to increase medication adherence, self-management of disease, and behavioral change is becoming an essential part of patient care. The effectiveness of text message reminders in improving medication adherence was exhibited in other clinical disease states and medical conditions including diabetes,37 severe mental illness,38 acute coronary syndromes,39 and HIV.26
Inherent in all systematic reviews, our study has some limitations. First, studies included in this review did not report reliability and validity. Second, the studies had short follow-up periods (4 weeks to 9 months). Short follow-up periods may conceal the true effect of the text message reminds on medication adherence. Thirdly, the results of the studies included may not be generalizable to the entire population of asthmatics mainly because these studies only included persons under the age of 45 years without consideration of older populations.32, 34 Also, sample sizes were small, with one study having an intervention group size of only 8 participants.32–34 Strandbygaard et al. pointed out that the intervention groups that received the text messages could have also received additional care that as a result led to the increase in adherence, not text messages alone.33 Direct comparison of different interventions aiming at improving medication adherence may have been more beneficial. Such intervention may include of one-way text messaging (sending text message reminders only) compared with two-way text messaging (sending reminders and receiving replies confirming whether the medication has been taken). Notwithstanding the limitations, there is a reason to expect that the evidence provided in this review would support the effectiveness of text message reminders on medication adherence among asthmatics in future trials.
CONCLUSION
Text message reminders can be important in ambulatory care settings and easily implemented in routine clinical practice without much additional time or resources to help patients take their medications as prescribed. Further research is needed to provide evidence regarding the effectiveness of text message reminders as a potential method for improving medication adherence. Specifically, studies with larger sample sizes, different age groups, and comparable intervention methods may provide a precise measure of the effectiveness of text message reminders on enhancing medication adherence. Moreover, future studies aiming at different sociodemographic groups would be more insightful to identify any sources of socioeconomic and demographic variation. Finally, the knowledge from this seminal systematic review is highly important to the practice of pharmacy and provides an opportunity to recognize the profound impact of pharmacy services on public health.
Conflicts of Interest
None
Funding/Support
The author (s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Pawankar R. Allergic diseases and asthma: a global public health concern and a call to action. BioMed Central; 2014. [DOI] [PMC free article] [PubMed]
- 2.https://www.cdc.gov/asthma/default.htm. Prevention CfDCa. Asthma. 2018 Jan 10; 2018. (accessed March 16 2018)
- 3.FitzGerald JM, Tavakoli H, Lynd LD, Al Efraij K, Sadatsafavi M. The impact of inappropriate use of short acting beta agonists in asthma. Respiratory medicine. 2017;131:135–40. doi: 10.1016/j.rmed.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Nurmagambetov T, Khavjou O, Murphy L, Orenstein D. State-level medical and absenteeism cost of asthma in the United States. Journal of Asthma. 2017;54(4):357–70. doi: 10.1080/02770903.2016.1218013. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan PW, Ghushchyan V, Navaratnam P, et al. The national cost of asthma among school-aged children in the United States. Annals of allergy, asthma & immunology. 2017;119(3):246–52. doi: 10.1016/j.anai.2017.07.002. e1. [DOI] [PubMed] [Google Scholar]
- 6.Nurmagambetov T, Kuwahara R, Garbe P. The Economic Burden of Asthma in the United States, 2008-2013. Annals of the American Thoracic Society. 2018. (ja). [DOI] [PubMed]
- 7.Sabaté E. Adherence to long-term therapies: evidence for action: World Health Organization. 2003. [PubMed]
- 8.Vrijens B, De Geest S, Hughes DA et al. A new taxonomy for describing and defining adherence to medications. British journal of clinical pharmacology. 2012;73(5):691–705. doi: 10.1111/j.1365-2125.2012.04167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MC, Verhamme KM. Medication adherence and the risk of severe asthma exacerbations: a systematic review. European Respiratory Journal. 2015;45(2):396–407. doi: 10.1183/09031936.00075614. [DOI] [PubMed] [Google Scholar]
- 10.Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. New England Journal of Medicine. 2000;343(5):332–6. doi: 10.1056/NEJM200008033430504. [DOI] [PubMed] [Google Scholar]
- 11.Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: responses to interviews, focus groups, and questionnaires. Immunology and Allergy Clinics. 2005;25(1):107–30. doi: 10.1016/j.iac.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Saito N, Kamata A, Itoga M, Tamaki M, Kayaba H, Ritz T. Assessment of biological, psychological and adherence factors in the prediction of step-down treatment for patients with well-controlled asthma. Clinical & Experimental Allergy. 2017;47(4):467–78. doi: 10.1111/cea.12888. [DOI] [PubMed] [Google Scholar]
- 13.Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: application of the necessity–concerns framework. Journal of psychosomatic research. 2008;64(1):41–6. doi: 10.1016/j.jpsychores.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Heaney LG, Horne R. Non-adherence in difficult asthma: time to take it seriously. Thorax. 2012;67(3):268–70. doi: 10.1136/thoraxjnl-2011-200257. [DOI] [PubMed] [Google Scholar]
- 15.Goeman DP, Douglass JA. Optimal management of asthma in elderly patients. Drugs & aging. 2007;24(5):381–94. doi: 10.2165/00002512-200724050-00003. [DOI] [PubMed] [Google Scholar]
- 16.Divertie V. Strategies to promote medication adherence in children with asthma. MCN: The American Journal of Maternal/Child Nursing. 2002;27(1):10–8. doi: 10.1097/00005721-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Park J, Jackson J, Skinner E, Ranghell K, Saiers J, Cherney B. Impact of an adherence intervention program on medication adherence barriers, asthma control, and productivity/daily activities in patients with asthma. Journal of Asthma. 2010;47(10):1072–7. doi: 10.3109/02770903.2010.485660. [DOI] [PubMed] [Google Scholar]
- 18.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a textmessaging system to support young people with diabetes. Diabetic Medicine. 2006;23(12):1332–8. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 19.Neville R, Charnock Greene A, McLeod J, Tracey A, Surie J. Mobile phone text messaging can help young people with asthma. British Medical Journal. 2002. [DOI] [PMC free article] [PubMed]
- 20.Jones K, Mullee M, Middleton M, Chapman E, Holgate S. Peak flow based asthma self-management: a randomised controlled study in general practice. British Thoracic Society Research Committee. Thorax. 1995;50(8):851–7. doi: 10.1136/thx.50.8.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunbar JM, Marshall GD, Hovell MF. Behavioral strategies for improving compliance. Compliance in health care. 1979. pp. 174–90.
- 22.Weinstein AG. Clinical management strategies to maintain drug compliance in asthmatic children. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology. 1995;74(4):304–10. [PubMed] [Google Scholar]
- 23.DeKoekkoek T, Given B, Given CW, Ridenour K, Schueller M, Spoelstra SL. mHealth SMS text messaging interventions and to promote medication adherence: an integrative review. Journal of clinical nursing. 2015;24(19–20):2722–35. doi: 10.1111/jocn.12918. [DOI] [PubMed] [Google Scholar]
- 24.Thakkar J, Kurup R, Laba T-L, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA internal medicine. 2016;176(3):340–9. doi: 10.1001/jamainternmed.2015.7667. [DOI] [PubMed] [Google Scholar]
- 25.Center PR. http://www.pewinternet.org/fact-sheet/mobile/ [accessed Apr 11;2018 ];Mobile Fact Sheet. Mobile Fact Sheet 2018.
- 26.Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. The Lancet. 2010;376(9755):1838–45. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 27.Zurovac D, Sudoi RK, Akhwale WS, et al. The effect of mobile phone text-message reminders on Kenyan health workers' adherence to malaria treatment guidelines: a cluster randomised trial. The Lancet. 2011;378(9793):795–803. doi: 10.1016/S0140-6736(11)60783-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castaño PM, Bynum JY, Andrés R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstetrics & Gynecology. 2012;119(1):14–20. doi: 10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 29.Armstrong AW, Watson AJ, Makredes M, Frangos JE, Kimball AB, Kvedar JC. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Archives of dermatology. 2009;145(11):1230–6. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- 30.Osterberg L, Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 31.Britto MT, Munafo JK, Schoettker PJ, Vockell A-LB, Wimberg JA, Yi MS. Pilot and feasibility test of adolescent-controlled text messaging reminders. Clinical pediatrics. 2012;51(2):114–21. doi: 10.1177/0009922811412950. [DOI] [PubMed] [Google Scholar]
- 32.Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, Stipic-Markovic A, Tudjman Z. Improving asthma control through telemedicine: a study of short-message service. Telemedicine Journal & E-Health. 2005;11(1):28–35. doi: 10.1089/tmj.2005.11.28. [DOI] [PubMed] [Google Scholar]
- 33.Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respiratory medicine. 2010;104(2):166–71. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Petrie KJ, Perry K, Broadbent E, Weinman J. A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. British journal of health psychology. 2012;17(1):74–84. doi: 10.1111/j.2044-8287.2011.02033.x. [DOI] [PubMed] [Google Scholar]
- 35.MacDonell KK, Naar S, Gibson-Scipio W, Lam P, Secord E. The Detroit Young Adult Asthma Project: pilot of a technology-based medication adherence intervention for African-American emerging adults. Journal of Adolescent Health. 2016;59(4):465–71. doi: 10.1016/j.jadohealth.2016.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tran N, Coffman JM, Sumino K, Cabana MD. Patient reminder systems and asthma medication adherence: a systematic review. Journal of Asthma. 2014;51(5):536–43. doi: 10.3109/02770903.2014.888572. [DOI] [PubMed] [Google Scholar]
- 37.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. Journal of diabetes science and technology. 2008;2(3):509–17. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bright CE. Integrative Review of Mobile Phone Contacts and Medication Adherence in Severe Mental Illness. Journal of the American Psychiatric Nurses Association. 2018 doi: 10.1177/1078390318754986. 1078390318754986. [DOI] [PubMed] [Google Scholar]
- 39.Khonsari S, Subramanian P, Chinna K, Latif LA, Ling LW, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. European Journal of Cardiovascular Nursing. 2015;14(2):170–9. doi: 10.1177/1474515114521910. [DOI] [PubMed] [Google Scholar]


