Abstract
Background
Digital health is increasingly recognized as a cost-effective means to support patient self-care. However, there are concerns about whether the “digital divide,” defined as the gap between those who do and do not make regular use of digital technologies, will lead to increased health inequalities. Access to the internet, computer literacy, motivation to use digital health interventions, and fears about internet security are barriers to use of digital health interventions. Some of these barriers disproportionately affect people of older age, black or minority ethnic background, and low socioeconomic status. HeLP-Diabetes (Healthy Living for People with type 2 Diabetes), a theoretically informed online self-management program for adults with type 2 diabetes, was developed to meet the needs of people from a broad demographic background.
Objective
This study aimed to determine whether there was evidence of a digital divide when HeLP-Diabetes was integrated into routine care. This was achieved by (1) comparing the characteristics of people who registered for the program against the target population (people with type 2 diabetes in inner London), (2) comparing the characteristics of people who registered for the program and used it with those who did not use it, and (3) comparing sections of the website visited by different demographic groups.
Methods
A retrospective analysis of data on the use of HeLP-Diabetes in routine clinical practice in 4 inner London clinical commissioning groups was undertaken. Data were collected from patients who registered for the program as part of routine health services.. Data on gender, age, ethnicity, and educational attainment were collected at registration, and data on webpage visits (user identification number, date, time, and page visited) were collected automatically by software on the server side of the website.
Results
The characteristics of people who registered for the program were found to reflect those of the target population. The mean age was 58.4 years (SD=28.0), over 50.0% were from black and minority ethnic backgrounds, and nearly a third (29.8%) had no qualifications beyond school leaving age. There was no association between demographic characteristics and use of the program, apart from weak evidence of less use by the mixed ethnicity group. There was no evidence of the differential use of the program by any demographic group, apart from weak evidence for people with degrees and school leavers being more likely to use the “Living and working with diabetes” (P=.03) and “Treating diabetes” (P=.04) sections of the website.
Conclusions
This study is one of the first to provide evidence that a digital health intervention can be integrated into routine health services without widening health inequalities. The relative success of the intervention may be attributed to integration into routine health care, and careful design with extensive user input and consideration of literacy levels. Developers of digital health interventions need to acknowledge barriers to access and use, and collect data on the demographic profile of users, to address inequalities.
Keywords: type 2 diabetes mellitus, self-management, patient education, internet, digital divide, social class, health literacy, computer literacy
Introduction
Background
Health systems internationally are struggling with the challenges posed by rising demand and increasing costs of health care due to an aging population, the increase in the prevalence of long-term conditions, and changing patient expectations [1-3]. This challenge has been clearly articulated in the English National Health Service (NHS), with an explicit commitment to improving the quality and efficiency of care delivered by the NHS, within a tightly controlled budget [4]. Two strategies which have been identified are increasing provision of digital health and promoting self-care by patients [5-9]. The expectation is that, where health care can be effectively delivered through digital means, it will be more cost-effective than face-to-face health care delivery, because of the scalability and low marginal costs per additional user of digital health interventions. There is also an expectation that improving patients’ ability to self-care will reduce health care costs and improve health outcomes.
Although there are some data to support both these contentions [4,10-12], there are also anxieties about the extent to which such policies will widen health inequalities [13]. There are concerns about the “digital divide,” defined as the divide between those who do and do not make regular use of digital technologies and the internet [14,15]. Overall, internet use is high in the United Kingdom (UK), with 90% of the population having access in 2017, and one of the most common reasons for using the internet is to access health-related information or services [16]. However, there are still 4 million households without internet access, and those without access are often those who are most in need of health care, including older people, people with disability, and people with lower socioeconomic status (SES) [17]. Data from the Office for National Statistics show that adults aged over 75 years are the lowest users of the internet [16], and the proportion of adults who are recent internet users is lower for disabled people than it is for able-bodied people [18]. Buying and accessing computer equipment is costly, which presents a barrier to access for people with lower SES.
The digital divide is about more than just access. The 2014 Government Digital Inclusion Strategy identified 3 additional challenges, which were (1) not having the skills or capacity to use the internet (computer literacy), (2) not having the motivation to go online, and (3) lack of trust in internet security [19]. Thus the “digital divide” is closely related to general literacy and health literacy. Health literacy has been defined as “the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health” [20]. People with low health literacy are less able to access and use health information effectively and have poorer health outcomes [21,22].
Similarly, there are concerns that programs which aim to promote self-care by patients, such as the expert patient program, may widen health inequalities as people with higher levels of self-efficacy, and better access to social, economic, and practical resources, may be better able to engage with such programs and adopt the behaviors required for effective self-management [23,24].
In this paper, we present registration and usage data from a digital program designed to support self-management of type 2 diabetes mellitus (T2DM), known as Healthy Living for People with type 2 Diabetes (HeLP-Diabetes). We collected data on age, gender, ethnicity, and educational attainment. Educational attainment was used as a marker of SES, as is common in epidemiological research [25,26], and also digital and health literacy. Low health literacy has been found to be more common among older people, people from black and minority ethnic (BAME) backgrounds, people with lower incomes, and people with lower educational attainment [27-29]. Lower digital literacy has also been found to be associated with lower educational attainment [30].
Data on ethnicity were collected due to the higher prevalence of low health literacy, and the concern about health inequalities, among BAME groups. Inequalities in health have been documented across ethnic groups in the United States and the United Kingdom, with Bangladeshi and Pakistani people reporting the poorest health, followed by Caribbean, Chinese, and Indian people [31,32]. White people have the best health [31,32]. Factors underlying these differences include SES, genetic, and cultural factors [33].
Considerable effort was invested during the development of HeLP-Diabetes to ensure that the program was accessible, relevant to, and met the needs of, people from a wide range of demographic backgrounds. The development of HeLP-Diabetes is described in more detail elsewhere [34]. It is a theoretically- informed, evidence-based online program developed using participatory design techniques and extensive user input, which has demonstrated efficacy in improving glycemic control [34,35].
The text for HeLP-Diabetes was written for people with a reading age of 12 (80% of UK population achieve this) [36]. All essential information was provided in a video as well as text, and personal stories were included, as people with low literacy prefer this method of learning [37-39].
HeLP-Diabetes was commissioned by 4 inner London clinical commissioning groups (CCGs) during the data collection period and offered to patients with T2DM as part of routine care. Hence there was a unique opportunity to gather real-world data on whether this intervention was being used across the digital divide. As the use of the program was a necessary prerequisite for patients obtaining health benefits [34], it was a relevant outcome for exploring whether the program was reaching the target audience.
Aims
The overall aim of the study was to determine whether there was evidence of a digital divide when a Web-based self-management program for T2DM was integrated into routine care. Specific objectives were to determine:
Whether the demographic characteristics of people who registered to use the program differed from the target population, and if so how
Whether once registered, specific demographic groups were more likely to use the program
Whether there were different patterns of use by specified demographic characteristics
Methods
Design
A retrospective analysis of data on the use of HeLP-Diabetes in routine clinical practice in 4 inner London CCGs was undertaken.
Setting
General Population of Study Setting
HeLP-Diabetes was commissioned by 4 inner London CCGs (CCG 1, 2, 3 and 4). All 4 CCGs have young, multicultural communities. They are densely populated and have relatively high levels of deprivation [40]. The educational attainment in the 4 CCGs is polarized. The proportion with degree level or above education attainment is higher than the national average. In contrast, 34%-42% of 19-year-old individuals do not have A-level qualifications (postsecondary nontertiary education) [41,42].
Diabetes Population of Study Setting
The target population of the HeLP-Diabetes program was adults with T2DM (see Table 1). There is a higher percentage of people in the 40-64 age group with T2DM in England (42.8%) and all 4 CGGs (range 49.3%-54.4%), than any other age group. More than 48% (range 48.3%-62.6%) of people with T2DM in the 4 participating CCGs are of BAME origin, reflecting the ethnic diversity of these areas [43].
Table 1.
Diabetes population of the clinical commissioning groups compared with England (prevalence is given as a percentage, because the numbers are not publicly available).
| Population demographic characteristic | England | CCGa 1 | CCG 2 | CCG 3 | CCG 4 | ||
| QoFb total type 1 and type 2 diabetes prevalence, n (%) | 3,116,399 (6.7) | 15,213 (6.2) | 10,368 (5.0) | 18,274 (5.5) | 16,663 (6.5) | ||
| T2DMc prevalence, (%) |
|
|
|
|
|
||
|
|
Age (years) |
|
|
|
|
|
|
|
|
|
<40 | 3.9 | 4.6 | 4.8 | 4.9 | 4.8 |
|
|
|
40-64 | 42.8 | 50.4 | 49.3 | 54.4 | 51.4 |
|
|
|
65-79 | 38.0 | 32.8 | 32.2 | 29.2 | 31.0 |
|
|
|
>80 | 13.8 | 10.0 | 10.6 | 9.6 | 11.0 |
|
|
Gender |
|
|
|
|
|
|
|
|
|
Male | 55.8 | 51.9 | 52.5 | 52.5 | 51.7 |
|
|
|
Female | 48.1 | 44.2 | 47.5 | 47.5 | 48.3 |
|
|
Race |
|
|
|
|
|
|
|
|
|
White | 64.4 | 33.8 | 49.2 | 31.3 | 41.4 |
|
|
|
BAMEd | 19.3 | 60.5 | 48.3 | 62.6 | 55.8 |
aCCG: clinical commissioning groups.
bQoF: quality and outcomes framework in population >17 years of age.
cT2DM: type 2 diabetes mellitus.
dBAME: black and minority ethnic.
Intervention
HeLP-Diabetes is described in detail elsewhere [34]. It is an evidence-based, theoretically informed online self-management program for adults with T2DM. Content is based on the Corbin and Strauss [44] theory for living with long-term conditions which takes a holistic approach to diabetes management, incorporating the disease process (adopting healthy behaviors, working with health professionals, and taking medicines), the emotional consequences (the negative emotions associated with being diagnosed with a long-term condition), and the changes that occur in daily life (including the impact of a diagnosis on relationships with friends, family, and colleagues). Information is divided into 8 sections (see Table 2). Patients with T2DM were referred to the program by health care professionals, or made aware through flyers in waiting areas and texting from practices.
Table 2.
Healthy Living for People with type 2 Diabetes (HeLP-Diabetes) website sections.
| Section | Content |
| Understanding diabetes |
|
| Staying healthy |
|
| Treating diabetes |
|
| Living and working with diabetes |
|
| Managing my feelings |
|
| My health record |
|
| News and research |
|
| Forum and help |
|
The intervention was offered to patients with T2DM as a routine service in clinical practice. Practices placed flyers and posters in waiting areas informing patients about the program. Health care professionals were able to offer it to patients in consultations, and some practices wrote or sent texts to patients inviting them to register. Data were not recorded on how many patients were offered the program by health care professionals, and so this was not included in the analysis.
Ethics and Privacy
Details of the people who used the HeLP-Diabetes website were automatically pseudoanonymized with a user identification. Pseudoanonymized data were collected by the server side of the website and subsequently exported by the research team to Microsoft Excel and then Tableau reader for analysis. Secondary analysis of information collected for service evaluation is excluded from an ethics committee review by the NHS Research Ethics Committees (RECs), as long as patients were not identifiable [45]. Formal ethical approval was therefore not needed.
Data Collection
The demographic characteristics of everyone who registered to use the program were collected at the point of registration. Initially, people were registered and given access to the website by a member of the HeLP-Diabetes administrative team, and later a self-registration page was added to the website to allow people to register themselves. The demographic data collected at registration included gender, age, ethnicity, and education level. Education level was categorized using UK and US qualifications, and the International Standard Classification of Education [42].
The server side of the website automatically collected data on visits to the HeLP-Diabetes website. The data collected were: user ID, date and time of login, and page visited. These data were chosen as measures of use following best practice [46]. Alternative measures such as time can be prone to error as people may leave browsers on while engaged in alternative activities. The data presented here were collected between November 2015 and January 2017. During this time, 343 people registered to use the website, but not everyone who registered gave complete data on gender, ethnicity, education level and age. Therefore, the numbers provided in the results (n) are the numbers of people providing data for each demographic factor, and the totals are less than 343.
Analysis
For the analysis, web page visits were grouped into 11 sections. Eight of these are the sections of the website (see Table 2), and the remaining 3 are other web pages that the user may have visited outside the 8 information sections of the HeLP-Diabetes website. These comprise of (1) the homepage, (2) miscellaneous articles, and (3) HeLP-Diabetes: Starting Out (a structured program for people newly diagnosed with T2DM based on the content of HeLP-Diabetes). The profile, administration, logout, and registration pages were excluded from the analysis. Statistical analysis was carried out using Stata (version 14.1) [47].
The analysis addressed each of the 3 research questions listed under the aims.
Question 1: Did the Demographic Characteristics of People Who Registered to Use the Program Differ From the Target Population, and If so How?
The percentage of people who registered to use HeLP-Diabetes from each gender, ethnic, education, and age group was calculated to address this question. The target population was examined using the Public Health England data (see Table 1). A statistical analysis to compare the characteristics of the user population and the target population could not be carried out as the data were categorized differently. Instead of carrying out statistical analyses, we described the demographic characteristics of the registered users by stating the percentage of registered users in specified gender, ethnicity, education level and age groups. We have compared the percentage of male and female registered users with the percentage of males and females with T2DM in the 4 CCGs and compared the percentage of BAME registered users with the proportion of BAME people with T2DM in the 4 CCGs narratively. We were able to comment on which age group had the highest proportion of registered users.
Question 2: Was There Evidence of the Digital Divide in Overall Use?
The term “use” was defined as logging in to the HeLP-Diabetes website at least twice. This was in order to determine who returned to the website, rather than just visiting once. The percentage of people who visited the website at least twice was calculated for each demographic group. Logistic regression analyses were performed to look for evidence of an association between the binary dependent variable (use/nonuse) and each of the covariates (gender, ethnicity, education level, and age group).
Question 3: Was There Evidence of Differential Use by Demographic Characteristic?
The number of users who visited each of the 11 sections of the website and the number of visits to each section were categorized by demographic group. The Wilcoxon signed rank test was used to determine if there was an association between age and the number of visits to each section of the website. The Kruskal-Wallis equality of populations rank test was used to determine if there was an association between ethnicity, education, and the number of web page visits per user to each section of the website.
Results
Question 1: Was There Evidence of the Digital Divide in People Registered to Use the Program?
The mean age (see Table 3) was 58.4 years (SD 28.0). The age group with the highest proportion of people registered to use HeLP-Diabetes is the 51-60-year-olds (101/334, 30.2%), followed by the 61-70-year-olds (80/334, 24.0%), and 71-80-year-olds (56/334, 16.8%). Of the people with T2DM in the general population of the 4 CCGs (see Table 1), the highest proportion (range 49.3%-54.4%) of people was in the 40-64-year-old age group. This suggests that the age of the registered users reflected the target population. The most common education level was a bachelor’s degree or equivalent (102/299, 34.1%), followed by a general certificate of secondary education (GCSE)/high school diploma (89/299, 29.8%).
Table 3.
Demographic characteristics of people who registered at clinical commissioning group 1 (n=97), 2 (n=51), 3 (n=154), and 4 (n=41) to use Healthy Living for People with type 2 Diabetes (HeLP-Diabetes).
| Demographic characteristic | n (%) | |
| Gender (n=317) |
|
|
|
|
Male | 176 (55.5) |
|
|
Female | 141 (44.5) |
| Ethnicity (n=330) |
|
|
|
|
White | 150 (45.5) |
|
|
Black | 117 (35.5) |
|
|
Asian | 46 (13.9) |
|
|
Mixed | 17 (5.2) |
| Education level (n=299) |
|
|
|
|
GCSEa/high school | 89 (29.8) |
|
|
A-level/postsecondary | 64 (21.4) |
|
|
Bachelor’s degree or equivalent | 102 (34.1) |
|
|
Master’s or doctoral degree or equivalent | 44 (14.7) |
| Age group (n=334) |
|
|
|
|
18-30 | 6 (1.7) |
|
|
31-40 | 20 (6.0) |
|
|
41-50 | 55 (16.5) |
|
|
51-60 | 101 (30.2) |
|
|
61-70 | 80 (24.0) |
|
|
71-80 | 56 (16.8) |
|
|
81-90 | 13 (3.9) |
|
|
≥91 | 3 (0.8) |
aGCSE: general certificate of secondary education.
Males represented 55.5% (176/317) of registered users. Public Health data on the 4 CCGs the program was offered in, shows 51%-53% of people with T2DM in these areas are male. A total of 180/330 (54.5%) of the registered users were BAME, and 48%-60% of people with T2DM in the 4 CCGs are BAME. This suggested that the gender and ethnicity of people who registered to use the program reflected the target population in the 4 CCGs.
Q2. Was There Evidence of the Digital Divide in Overall Use?“
Ninety-two of 150 (61.3%) white, 70/117 (59.8%) black, and 28/46 (60.9%) of Asians who registered to use HeLP-Diabetes, visited the website at least twice (see Table 4). This was lower in the mixed group (5/17 (29.4%), odds ratio (OR)=0.26, 95% CI=0.09-0.78). The median age of people who visited the website at least twice was 59 years (lower quartile=50, upper quartile=70), and age groups were categorized into quartiles for this analysis. Visits to the website by the different age groups ranged from 46.7% (50/107) in those aged 60-69 years to 55.9% (62/111) in those aged 51-59 years. There was no significant difference in usage for gender, education level or age.
Table 4.
Proportion of people registered to use HeLP-Diabetes who visited at least twice.
| Demographic characteristics | n/Na (%) | Odds ratio (95% CI) | P value | |
| Gender (n=317) |
|
|
|
|
|
|
Female | 77/141 (54.6) | 1.00 | .19 |
|
|
Male | 109/176 (61.9) | 1.35 (0.86-2.12) | |
| Ethnicity (n=335) |
|
|
|
|
|
|
White | 92/150 (61.3) | 1.00 | .12 |
|
|
Black | 70/117 (59.8) | 0.94 (0.57-1.54) | |
|
|
Asian | 28/46 (60.9) | 0.98 (0.50-1.93) | |
|
|
Mixed | 5/17 (29.4) | 0.26 (0.09-0.78) | |
| Education level (n=299) |
|
|
|
|
|
|
GCSEb/high school | 53/89 (59.6) | 1.00 | .95 |
|
|
A-level/postsecondary | 36/64 (56.3) | 0.87 (0.46-1.67) | |
|
|
Bachelor’s degree or equivalent | 61/102 (59.8) | 1.06 (0.59-1.90) | |
|
|
Master’s degree, doctoral degree or equivalent | 26/44 (59.1) | 0.98 (0.47-2.05) | |
| Age group (n=334) |
|
|
|
|
|
|
22-50 | 49/96 (51.0) | 1.00 | .54 |
|
|
51-59 | 62/111 (55.9) | 1.21 (0.70-2.10) | |
|
|
60-69 | 50/107 (46.7) | 0.84 (0.49-1.46) | |
|
|
70-93 | 44/80 (55.0) | 1.17 (0.65-2.13) | |
aThe proportion who visited the website at least twice (n)/everyone in this demographic group who registered (N).
bGCSE: general certificate of secondary education.
Q3. Were There Different Patterns of Use by Demographic Characteristics?
Overall, the 2 sections of the website that were most visited were (1) My health records and (2) Staying healthy. There was no evidence of differential use of the program by any demographic group, apart from education level, where there was weak evidence of an association between education level and visits to the “Living and working with diabetes” section with P=.03 (Figure 1), and the “Treating diabetes” section with P=.04 (Figure 2). The difference between visits by people with high school diplomas and a tertiary education level was small, as 34.3% (24/70) of visits to the “Living and working with diabetes” were by users with a bachelor’s degree or equivalent, while 32.9% (23/70) of visits were by users with high school diplomas. Also, 34.9% (22/63) of visits to the “Treating diabetes” section were by users with a bachelor’s degree or equivalent, compared to 33.3% (21/63) of visits by users with high school diplomas. The proportion of users who visited both sections with postsecondary nontertiary education level or master’s or doctoral degrees or equivalent was much lower (see Multimedia Appendices 1-4 for details).
Figure 1.
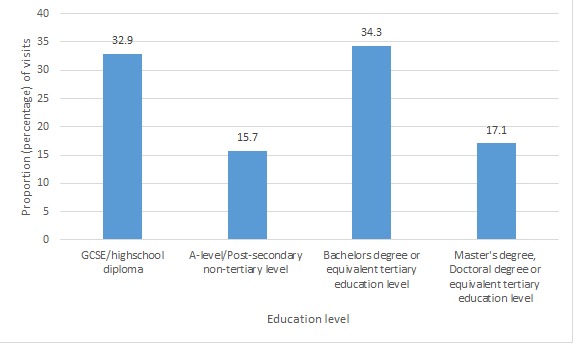
Proportion of visits to the "Living and working with diabetes" section of the website. GCSE: general certificate of secondary education.
Figure 2.
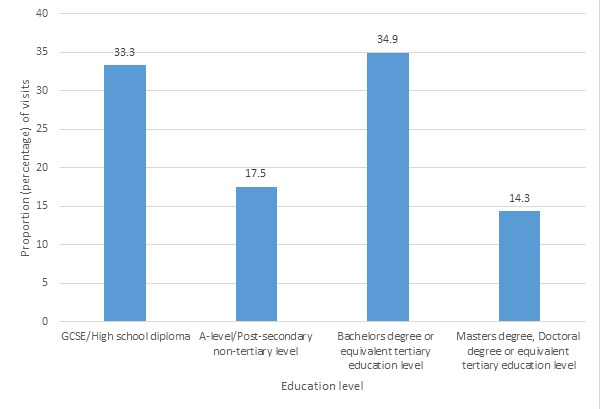
Proportion of visits to the "Treating Diabetes" section of the website. GCSE: general certificate of secondary education.
Discussion
Principal Results
This study is one of the first to explore whether there is evidence of a digital divide in the use of a digital health intervention integrated into routine health care. As such it makes a substantial addition to the literature on whether digital health is likely to increase or decrease health inequalities. Reassuringly, we found no strong evidence of differential patterns of registration, or patterns of use by age, gender, educational attainment or ethnicity. There was weak evidence that people from the mixed ethnicity group were less likely to use the program than the white group (OR=0.26, 95% CI=0.09-0.78, P=.12). There was also weak evidence of differences in visits to the “Living and working with diabetes” (P=.03) and “Treating diabetes” (P=.04) sections of the website by education level. The highest proportion of users who visited these sections of the website were those with a bachelor’s degree or equivalent, but people with high school diplomas closely followed.
Comparison With Prior Work
These findings make a significant contribution because the literature on the use of digital health interventions suggests higher use among younger, well-educated, higher income, nonBAME individuals, which is a pattern that is likely to increase health inequalities. For example, a systematic review of electronic portal (an online electronic health records system) usage among patients with diabetes found that higher education, younger age, higher income, and nonHispanic, nonblack race were associated with higher portal utilization [48].
A second systematic review of patterns of user engagement with mobile and Web-based self-care interventions for adults with T2DM [49], also found that use was higher among younger people. However, 1 study included in the review showed that use of a mobile Health medication adherence promotion intervention for low-income adults with T2DM increased from 25 to 50 years of age, then decreased as age increased [50].
Our findings are also in keeping with a qualitative study of people with high and low levels of health literacy about a digital intervention to promote physical activity for diabetes in 5 countries [51]. Participants in that study were from areas with high levels of deprivation and had a mean age of 62 years and most found the design of the intervention was acceptable and engaging. Findings from both our study and this qualitative study suggest that it is possible to design digital health interventions that appeal to a diverse population, including people with low literacy and health literacy levels.
Strengths and Limitations
A strength of the research is that individuals were offered HeLP-Diabetes as an NHS service, and not as a research study. This provides us with data on “real world” use of the program and not data generated from a highly controlled research setting. Actual website visits were automatically measured rather than using self-reported use of the program, which relies on memory and may result in bias from social desirability. A variety of engagement measures were analyzed including numbers who registered, the proportion who actively used the program, and the number of page visits. There are other measures of engagement including the duration of time spent using the website per visit, and the duration of time between visits to the website. The number of visits was considered to be a more reliable measure of engagement.
A limitation of the research is the total number of participants (n=343). This may limit the power of the study to detect significant differences between demographic groups. The 95% CI was provided in addition to P values in recognition of the fact that a P value by itself provides limited information [52]. Where the P value and 95% CI do not agree, this has been stated.
Implications
The findings of this study suggest that digital health interventions can be designed to be used by people of different demographic backgrounds. This is important to enable equitable access to health information and support, and to prevent worsening health inequalities.
Developers of digital health interventions should be mindful of the needs of different demographic groups in their design process and involve users of different backgrounds at each stage of development. Research on the evaluation of digital health interventions should include the collection of data on the demographic profile of users, and the use (or other engagement measure) of the intervention by different demographic groups.
Developers also need to acknowledge and address barriers to the use of digital health interventions such as low health literacy and poor computer literacy. The 2014 Government Digital Inclusion Strategy has identified lack of computer skills, not having the motivation to go online, and lack of trust in internet security as additional challenges to internet use, in addition to lack of access [19]. Possible reasons for our relative success in crossing the digital divide are twofold. First, full integration into routine health care, with a recommendation for use from health care professionals. This improved motivation to go online and use the intervention, and trust in the security of the intervention [53]. Second, careful design of the intervention to make it fully accessible to a wide range of people. HeLP-Diabetes was designed using participatory design techniques, extensive user input, and consideration of literacy levels and use of audio-visual media [34]. These techniques make the program more accessible to people with lower health literacy and computer literacy.
Conclusion
This study is one of the first to provide evidence that health inequalities are not necessarily widened when a digital health intervention was integrated into routine health care. Weak evidence of a difference in overall use was identified for ethnicity (less use by the mixed-race ethnic group). here was also weak evidence of differences in the use of the “Living and working with diabetes” and “Treating diabetes” sections of the website (the highest proportion of visits were by people with a bachelor’s degree) but the proportion of visits by people with high school diplomas was very similar). The relative success of the intervention may be attributed to integration into routine health care, and recommendation from health care professionals, but also careful design with extensive user input and consideration of literacy levels. Developers of digital health interventions need to acknowledge barriers to access and use including health literacy, computer literacy, motivation and concerns about internet security if they are to navigate and reduce health inequalities successfully.
Acknowledgments
Funding for a percentage of staff time, travel to practices, printing, and postage of registration packs, posters about the program for practices, website development and a percentage of hosting and maintenance of the website was provided by a National Institute for Health Research School for Primary Care Research FR9 grant (Project Ref. 280).
Abbreviations
- BAME
black and minority ethnic
- CCG
clinical commissioning group
- GCSE
general certificate of secondary education
- HeLP-Diabetes
Healthy Living for People with type 2 Diabetes
- NHS
National Health Service
- SES
socioeconomic status
- T2DM
type 2 diabetes mellitus
Total number of visits to each section of the HeLP-Diabetes website by female and male users.
Total number of visits to each section of the HeLP-Diabetes website by users of different education levels.
Total number of visits to each section of the HeLP-Diabetes website by users of different age groups.
Total number of visits to each section of the HeLP-Diabetes website by users of different ethnic groups.
Footnotes
Conflicts of Interest: Elizabeth Murray is Managing Director of HeLP-Digital, a not-for-profit Community Interest Company that exists to disseminate digital interventions, including HeLP-Diabetes and HeLP-Diabetes Starting Out to the NHS. She has not, does not, and will not take any remuneration for this work.
References
- 1.World Health Organization. 2015. [2018-11-09]. World report on ageing and health http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=403903126B3625BD559DBA8579FD4450?sequence=1 . [DOI] [PubMed]
- 2.The Lancet Disease, disability, and demography—a world in transition. The Lancet. 2015 Aug;386(9995):718. doi: 10.1016/S0140-6736(15)61524-0. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)61524-0/fulltext . [DOI] [PubMed] [Google Scholar]
- 3.Vos T, for Global Burden of Disease Study 2013 Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2015 Aug 22;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS England. 2014. [2018-10-17]. Five Year Forward View https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf .
- 5.Honeyman M, Dunn P, McKenna H. The King's Fund. 2016. [2018-10-17]. A digital NHS? An introduction to the digital agenda and plans for implementation https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/A_digital_NHS_Kings_Fund_Sep_2016.pdf .
- 6.National Information Board. 2014. [2018-10-17]. Personalised Health and Care 2020 https://www.digitalhealth.net/includes/images/news0254/PDF/0172_NHS_England_NIB_Report_WITH_ADDITIONAL_MATERIAL_S8.pdf .
- 7.NHS England. 2015. [2018-11-09]. Delivering the Forward View: NHS planning guidance 2016/17-2020/21 https://www.england.nhs.uk/wp-content/uploads/2015/12/planning-guid-16-17-20-21.pdf .
- 8.Wachter Robert M National Advisory Group on Health Information Technology in England. 2016. [2018-10-17]. Making IT work: harnessing the power of health information technology to improve care in England https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/550866/Wachter_Review_Accessible.pdf .
- 9.NHS England and NHS Improvement. 2017. [2018-10-17]. NHS Operational Planning and Contracting Guidance 2017-2019 https://www.england.nhs.uk/wp-content/uploads/2016/09/NHS-operational-planning-guidance-201617-201819.pdf .
- 10.Donker T, Blankers M, Hedman E, Ljótsson B, Petrie K, Christensen H. Economic evaluations of Internet interventions for mental health: a systematic review. Psychol Med. 2015 Dec;45(16):3357–76. doi: 10.1017/S0033291715001427.S0033291715001427 [DOI] [PubMed] [Google Scholar]
- 11.London T, Dash P. McKinsey & Company. London: 2016. [2018-10-17]. Health systems: Improving and sustaining quality through digital transformation https://www.mckinsey.com/business-functions/digital-mckinsey/our-insights/health-systems-improving-and-sustaining-quality-through-digital-transformation . [Google Scholar]
- 12.Diabetes UK. 2015. [2018-10-17]. Diabetes education: the big missed opportunity in diabetes care https://diabetes-resources-production.s3-eu-west-1.amazonaws.com/diabetes-storage/migration/pdf/Diabetes%2520UK_Diabetes%2520education%2520-%2520the%2520big%2520missed%2520opportunity_updated%2520June%25202016.pdf .
- 13.McAuley A. Digital health interventions: widening access or widening inequalities? Public Health. 2014 Dec;128(12):1118–20. doi: 10.1016/j.puhe.2014.10.008.S0033-3506(14)00270-4 [DOI] [PubMed] [Google Scholar]
- 14.Viswanath K, Kreuter Matthew W. Health disparities, communication inequalities, and eHealth. Am J Prev Med. 2007 May;32(5 Suppl):S131–3. doi: 10.1016/j.amepre.2007.02.012. http://europepmc.org/abstract/MED/17466818 .S0749-3797(07)00100-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eng T, Maxfield A, Patrick K, Deering M, Ratzan S, Gustafson Dh. Access to Health Information and Support. JAMA. 1998 Oct 21;280(15):1371. doi: 10.1001/jama.280.15.1371. [DOI] [PubMed] [Google Scholar]
- 16.Office for National Statistics. 2016. Internet access - households and individuals https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/bulletins/internetaccesshouseholdsandindividuals/2016#main-points .
- 17.Chang B, Bakken S, Brown S, Houston Thomas K, Kreps Gary L, Kukafka Rita, Safran Charles, Stavri P Zoe. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc. 2004;11(6):448–57. doi: 10.1197/jamia.M1535. http://europepmc.org/abstract/MED/15299002 .M1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office for National Statistics. 2017. [2018-11-09]. Internet users in the UK: 2017 https://www.ons.gov.uk/businessindustryandtrade/itandinternetindustry/bulletins/internetusers/2017 .
- 19.Department for Digital, Culture Media & Sport. 2017. [2018-10-17]. Digital skills and inclusion - giving everyone access to the digital skills they need https://www.gov.uk/government/publications/uk-digital-strategy/2-digital-skills-and-inclusion-giving-everyone-access-to-the-digital-skills-they-need .
- 20.Kickbusch I, Nutbeam D. World Health Organization. Geneva: 1998. [2018-11-09]. The Health Promotion Glossary http://www.bvsde.ops-oms.org/bvsast/e/fulltext/relcosta/anexo7.html . [Google Scholar]
- 21.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education communication strategies into the 21st century. Health Promotion International. 2000;15(3) doi: 10.1093/heapro/15.3.259. [DOI] [Google Scholar]
- 22.Berkman N, Sheridan S, Donahue K, Halpern D, Crotty Karen. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 Jul 19;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005.155/2/97 [DOI] [PubMed] [Google Scholar]
- 23.Rogers A, Kennedy A, Bower P, Gardner Caroline, Gately Claire, Lee Victoria, Reeves David, Richardson Gerry. The United Kingdom Expert Patients Programme: results and implications from a national evaluation. Med J Aust. 2008 Nov 17;189(10 Suppl):S21–4. doi: 10.5694/j.1326-5377.2008.tb02205.x.rog10822_fm [DOI] [PubMed] [Google Scholar]
- 24.Kennedy A, Rogers A, Gately C. Assessing the introduction of the expert patients programme into the NHS: a realistic evaluation of recruitment to a national lay-led self-care initiative. prim health care res dev. 2005 Apr 01;6(2):137–148. doi: 10.1191/1463423605pc241oa. [DOI] [Google Scholar]
- 25.Grundy E, Holt G. The socioeconomic status of older adults: how should we measure it in studies of health inequalities? J Epidemiol Community Health. 2001 Dec;55(12):895–904. doi: 10.1136/jech.55.12.895. http://jech.bmj.com/cgi/pmidlookup?view=long&pmid=11707484 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moody A, Cowley G, Ng FL, Mindell Jennifer S. Social inequalities in prevalence of diagnosed and undiagnosed diabetes and impaired glucose regulation in participants in the Health Surveys for England series. BMJ Open. 2016 Feb 08;6(2):e010155. doi: 10.1136/bmjopen-2015-010155. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=26857106 .bmjopen-2015-010155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kutner M, Greenberg E, Jin Y, Paulsen C. The National Center for Education Statistics. Washington, DC U. S: Department of Education; 2006. [2018-10-17]. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy https://nces.ed.gov/pubs2006/2006483.pdf . [Google Scholar]
- 28.Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association Health literacy: report of the Council on Scientific Affairs. JAMA. 1999 Feb 10;281(6):552–7.jcn80003 [PubMed] [Google Scholar]
- 29.von Wagner Christian, Knight K, Steptoe A, Wardle Jane. Functional health literacy and health-promoting behaviour in a national sample of British adults. J Epidemiol Community Health. 2007 Dec;61(12):1086–90. doi: 10.1136/jech.2006.053967. http://europepmc.org/abstract/MED/18000132 .61/12/1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Deursen A, van Dijk J. Internet skills and the digital divide. New Media & Society. 2010 Dec 06;13(6):893–911. doi: 10.1177/1461444810386774. [DOI] [Google Scholar]
- 31.Nazroo J. The Structuring of Ethnic Inequalities in Health: Economic Position, Racial Discrimination, and Racism. Am J Public Health. 2003 Feb;93(2):277–284. doi: 10.2105/AJPH.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Acheson D. Department of Health and Social Care. 1998. [2018-10-17]. Independent Inquiry into Inequalities in Health Report https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/265503/ih.pdf .
- 33.Nazroo J. Sociology of Health & Illness; 1998;20(5) Sociol Health & Illness. 1998 Sep;20(5):710–730. doi: 10.1111/1467-9566.00126. [DOI] [Google Scholar]
- 34.Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M, Li J, Ross J, Alkhaldi G, Barnard M, Farmer A, Michie S, Yardley L, May C, Parrott S, Stevenson F, Knox M, Patterson D. Web-based self-management support for people with type 2 diabetes (HeLP-Diabetes): randomised controlled trial in English primary care. BMJ Open. 2017 Sep 27;7(9):e016009. doi: 10.1136/bmjopen-2017-016009. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28954789 .bmjopen-2017-016009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dack C. Integrating theory, qualitative dataparticipatory design to develop HeLP-Diabetes: an internet self-management intervention for people with type 2 diabetes. International Society for Research on Internet Interventions; 2013; Chicago, USA. 2013. [Google Scholar]
- 36.National Literacy Trust. 2017. [2018-04-27]. Adult Literacy https://literacytrust.org.uk/parents-and-families/adult-literacy/
- 37.Bekker H, Winterbottom A, Butow P, Dillard Amanda J, Feldman-Stewart Deb, Fowler Floyd J, Jibaja-Weiss Maria L, Shaffer Victoria A, Volk Robert J. Do personal stories make patient decision aids more effective? A critical review of theory and evidence. BMC Med Inform Decis Mak. 2013;13 Suppl 2(2):S9–6947. doi: 10.1186/1472-6947-13-S2-S9. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-13-S2-S9 .1472-6947-13-S2-S9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jibaja-Weiss M, Volk R, Granchi T, Neff Nancy E, Robinson Emily K, Spann Stephen J, Aoki Noriaki, Friedman Lois C, Beck J Robert. Entertainment education for breast cancer surgery decisions: a randomized trial among patients with low health literacy. Patient Educ Couns. 2011 Jul;84(1):41–8. doi: 10.1016/j.pec.2010.06.009. doi: 10.1016/j.pec.2010.06.009.S0738-3991(10)00368-X [DOI] [PubMed] [Google Scholar]
- 39.Volk R, Jibaja-Weiss M, Hawley S, Kneuper Suzanne, Spann Stephen J, Miles Brian J, Hyman David J. Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns. 2008 Dec;73(3):482–9. doi: 10.1016/j.pec.2008.07.033. http://europepmc.org/abstract/MED/18760888 .S0738-3991(08)00390-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.London Data store. 2015. [2018-04-27]. Indices of Deprivation https://data.london.gov.uk/dataset/indices-of-deprivation-2015 .
- 41.Poverty and inequality data for Lewisham. 2018. [2018-10-17]. Trust for London https://www.trustforlondon.org.uk/data/boroughs/lewisham-poverty-and-inequality-indicators/
- 42.United Nations Educational, Scientific and Cultural Organization. [2018-11-09]. International Standard Classification of Education http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf .
- 43.Public Health England. 2017. [2018-04-27]. National General Practice Profiles: Diabetes https://fingertips.phe.org.uk/profile/general-practice/data .
- 44.Corbin J, Strauss A. Unending work and care. San Francisco: Jossey-Bass Inc; 1988. Managing chronic illness at home. [Google Scholar]
- 45.NHS Health Research Authority. 2016. [2018-11-09]. Research requiring NHS review but not ethical review http://www.hra.nhs.uk/resources/before-you-apply/research-requiring-nhs-rd-review-but-not-ethical-review/
- 46.Danaher BG, Boles SM, Akers L, Gordon JS, Severson HH. Defining participant exposure measures in Web-based health behavior change programs. J Med Internet Res. 2006 Aug 30;8(3):e15. doi: 10.2196/jmir.8.3.e15. http://www.jmir.org/2006/3/e15/ v8i3e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.StataCorp. College Station, TX: Stata Statistical Software; 2017. [2018-11-09]. Stata Statistical Software: Release 15 https://www.stata.com/ [Google Scholar]
- 48.Amante D, Hogan T, Pagoto S, English Thomas M. A systematic review of electronic portal usage among patients with diabetes. Diabetes Technol Ther. 2014 Nov;16(11):784–93. doi: 10.1089/dia.2014.0078. [DOI] [PubMed] [Google Scholar]
- 49.Nelson L, Coston T, Cherrington A, Osborn Chandra Y. Patterns of User Engagement with Mobile- and Web-Delivered Self-Care Interventions for Adults with T2DM: A Review of the Literature. Curr Diab Rep. 2016 Dec;16(7):66–016. doi: 10.1007/s11892-016-0755-1. http://europepmc.org/abstract/MED/27255269 .10.1007/s11892-016-0755-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nelson L, Mulvaney S, Gebretsadik T, Ho Y, Johnson K, Osborn Chandra Y. Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J Am Med Inform Assoc. 2016 Jan;23(1):12–8. doi: 10.1093/jamia/ocv082. http://europepmc.org/abstract/MED/26186935 .ocv082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rowsell A, Muller I, Murray E, Little Paul, Byrne Christopher D, Ganahl Kristin, Müller Gabriele, Gibney Sarah, Lyles Courtney R, Lucas Antonia, Nutbeam Don, Yardley Lucy. Views of People With High and Low Levels of Health Literacy About a Digital Intervention to Promote Physical Activity for Diabetes: A Qualitative Study in Five Countries. J Med Internet Res. 2015 Oct 12;17(10):e230. doi: 10.2196/jmir.4999. http://www.jmir.org/2015/10/e230/ v17i10e230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wasserstein R, Lazar Na. The ASA's Statement on -Values: Context, Process, and Purpose. The American Statistician. 2016 Jun 09;70(2):129–133. doi: 10.1080/00031305.2016.1154108. [DOI] [Google Scholar]
- 53.Murray E, Ross J, Pal K, Li Jinshuo, Dack C, Stevenson F, Sweeting M, Parrott S, Barnard M, Yardley L, Michie S, May C, Patterson D, Alkhaldi G, Fisher B, Farmer A, O'Donnell O. Development, evaluation (including randomised controlled trial and economic evaluation) and implementation of a web-based self-management programme for people with type 2 diabetes (HeLP-Diabetes) NIHR Journals Library. 2017 doi: 10.17863/CAM.11837. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Total number of visits to each section of the HeLP-Diabetes website by female and male users.
Total number of visits to each section of the HeLP-Diabetes website by users of different education levels.
Total number of visits to each section of the HeLP-Diabetes website by users of different age groups.
Total number of visits to each section of the HeLP-Diabetes website by users of different ethnic groups.


