Abstract
OBJECTIVES:
Children with medical complexity (CMC) are commonly assisted by medical devices to support essential body functions, although complications may lead to preventable emergency department (ED) and hospital use. Our objective was to identify predictors of device-complicated ED visits and hospitalizations.
METHODS:
This single-center retrospective cohort study included patients referred to a Pediatric Complex Care Program between April 1, 2014, and April 30, 2016, assisted by at least 1 medical device. Hospitalizations and ED visits in the year before enrollment were rated for likelihood for being due to device complications. Interrater reliability among 3 independent reviewers was assessed. Bivariate followed by multivariate logistic regression clustered by patient helped us identify associations between demographic, clinical, and device characteristics associated with device-complicated ED or hospital encounters.
RESULTS:
Interrater reliability was high (κ = 0.92). Among 98 CMC, device-complicated encounters represented 17% of 258 hospitalizations and 31% of 228 ED visits. Complications of 3 devices (central venous catheters, enteral tubes, and tracheostomy tubes) accounted for 13% of overall hospitalizations and 28% of overall ED visits. Central venous catheter presence (adjusted odds ratio [aOR] 3.2 [95% confidence interval (CI) 1.1–9.5]) was associated with device-complicated ED visits. Gastrojejunostomy/jejunostomy tube presence (aOR 3.3 [95% CI 1.5–7.5]) or tracheostomies with (aOR 8.1 [95% CI 2.3–28.5]) or without (aOR 4.5 [95% CI 1.7–7.5]) ventilator use was associated with device-complicated hospitalizations. Clinical variables were poor predictors of device-complicated encounters.
CONCLUSIONS:
Device-complicated ED visits and hospitalizations comprised a substantial proportion of total hospital and ED use. Developing interventions to prevent device complications may be a promising strategy to reduce overall CMC use.
Children with medical complexity (CMC) account for over one-third of child health spending, most of which is due to hospital care,1,2 and promising targets to lower use are needed. The lifelong chronic health conditions associated with medical complexity are frequently accompanied by need for invasive medical devices, such as gastrostomy and tracheostomy tubes, to support or replace essential body functions.3–6 Although CMC experience high hospital use and disproportionate health care expenditures,6,7 those patients assisted by medical devices are among the highest using subset.1,8,9 Moreover, unexpected complications of these devices (eg, infections or malfunctions) are an important source of health care use,3,10,11 representing 10% of CMC hospitalizations and being the third most common reason for hospitalization in 1 study.3 Little is known, however, about the patient characteristics predicting encounters from device complications, some of which may be avoidable.
Most research on CMC assisted by medical devices has explored caregiver experiences,8,12–14 overall use,9,11 or single devices such as tracheostomy15–19 or home oxygen therapy.20,21 Reliable and valid indicators of device complication encounters are underdeveloped. To identify and decrease device complication hospitalizations, a better understanding of these encounters and the patient and/or device characteristics that predict them is needed.
Our purpose with this study was to reliably identify emergency department (ED) visits and hospitalizations due to medical device complications and then to identify CMC, family, health care, and device characteristics predicting these encounters. We hypothesized that device complications would be common and more likely in patients who require feeding devices or have higher severity of illness.
Methods
Population, Setting, and Study Design
This retrospective cohort study included patients referred to a Pediatric Complex Care Program (PCCP) at a children’s hospital in the Midwestern United States between April 1, 2014 and April 30, 2016 who were assisted by at least 1 medical device to support an essential body function at the time of program enrollment. The PCCP began in 2014 to provide outpatient and inpatient medical comanagement and care coordination for CMC having chronic conditions affecting 3 or more organ systems, ongoing care from 3 or more medical or surgical specialists, and either 5 or more days hospitalized or 10 or more specialty clinic visits in the year before referral. CMC can be referred by any source (providers, families, community members) and retain their pediatric primary care provider. The multidisciplinary PCCP team includes general pediatricians, pediatric advance practice providers, registered nurses, and a social worker. Program activities include an initial 90-minute face-to-face enrollment visit; 60-minute scheduled clinic visits for comprehensive shared care planning every 6 months; as-needed urgent visits for acute issues; ED and inpatient consultation; and non–face-to-face medical management and care coordination. Because we were interested in characterizing general experiences of CMC who are assisted by devices, we analyzed ED visits and hospitalizations due to device complications before the child’s enrollment into PCCP.
Data Collection
Data were abstracted from electronic health records (EHRs) by using a structured protocol and entered into a Research Electronic Data Capture database.22 Although we were limited primarily to data within our health system, we did use the “Care Everywhere” feature within Epic (Epic System Corp, Verona, WI) to review available EHR data from external health systems. All available visits inside and outside of our system were included in analyses.
Definitions of Key Variables
ED or Hospital Use due to Device Complications
ED visits included any visit to the ED with a physician’s history and physical note, regardless of the disposition (ie, home or admitted). Hospitalizations were defined as any inpatient or observation stay with a discharge summary note. We sought to categorize the degree to which each ED visit and hospitalization was due to device complication on the basis of EHR review. We developed a scale describing the likelihood that a medical device was the cause of a given ED visit or hospitalization, with definitions and representative clinical scenarios, after 3 rounds of refinement. Additional detail and example cases are included in Supplemental Fig 2.
Each ED or hospital encounter for a patient was assigned one of the following:
0. Planned encounter for placement of a device not previously in use and not due to device complication, such as a hospitalization to place a baclofen pump
1. Unrelated to device complication in most circumstances
2. Uncertain
3. Related to device complication in most circumstances
Our initial scale was refined by pilot testing with 5 patients. The first 50 randomly selected encounters were reviewed by 3 reviewers: a trained research assistant (A.N.) and 2 physician reviewers each with >10 years of complex care experience, 1 with experience as a hospital medicine division chief and both with experience as medical directors of complex care programs (R.J.C. and M.E.). Reviewers had access to all aspects of the EHR, including history and physical, progress, transfer, ED and discharge summary notes, as well as laboratory data and outpatient encounters. The group evaluated agreement and identified and resolved discrepancies through group discussion and assigned a consensus score to each encounter. The device complication scale definitions were then revised, and this process was repeated after review of a second 50 randomly selected encounters. Because high interrater reliability was achieved, a single reviewer (A.N.) assigned remaining scale scores.
Medical Devices
Medical device use was adapted from Feudtner’s definition of technology dependence23 as “some form of medical technology, including medications or devices; and they would, if the technology were to fail or its use be discontinued, likely suffer a sufficiently adverse health consequence that hospitalization would be required.” For the purposes of this study, we focused on devices (ie, we did not include medications). We included 15 possible devices for this study.
Continuous positive airway pressure (CPAP) and/or bilevel positive airway pressure (BiPAP)
Tracheostomy without ventilator
Tracheostomy with ventilator
Home oxygen (eg, simple face mask, nasal cannula)
Ventricular shunt (eg, ventriculo-peritoneal shunt)
Central venous catheter
Gastrostomy tube
Gastrojejunostomy or Jejunostomy tube
Nasogastric or nasojejunal tube
Baclofen pump
Pacemaker
Dialysis (hemodialysis or peritoneal)
Vagal nerve stimulator
Ileostomy and/or colostomy
Insulin pump
Duration of use of each medical device and total number of devices at the time of enrollment was abstracted from the EHRs. For each ED visit or hospitalization, we determined the devices present at the time of the encounter. Among ED visits or hospitalizations rated as being due to device complications, the involved device was identified.
Predictors of ED Visits or Hospitalizations due to Device Complications
Based on previously published research3,9,24 and multidisciplinary PCCP provider input, we identified predictors of ED visits or hospitalizations from device complications that could be abstracted from the EHR at the time of PCCP enrollment. Child and family characteristics included child demographics, household structure (living in 1 or >1 household; 2-parent, single-parent or foster care; and number of siblings), and passive smoke exposure. Health care characteristics included receiving any routine care external to our institution, distance (miles) from principal residence to the medical center, involvement of therapies (occupational, physical, speech), presence of in-home personal care or respite workers, and receipt of either early intervention services or an individualized education plan. Severity of illness characteristics included number of complex chronic conditions25 and numbers of affected body systems, specialists, hospital, and ED visits in year before complex care program enrollment.
Data Analysis
Interrater reliability for device complication visits between the 3 reviewers was determined from κ statistics after the first 50 and second 50 encounters. Encounters were then dichotomized as being due to device complications when visits scored 3 on the device complication scale.
Descriptive statistics characterized the patient population according to number and type of medical devices, frequencies and durations of device use, as well as the proportions of ED visits and hospitalizations that were due to device complications for each device. Bivariate followed by multivariate logistic regression clustered by patient then identified associations between an ED visit or hospitalization being due to device complications and number of devices present, child and family factors, or severity of illness. Multivariate models were constructed by including covariates having significant bivariate relationships (P < .05). All analyses were completed using Stata (SE version 14.0; Stata Corp, College Station, TX). This study was approved by the Institutional Review Board at the University of Wisconsin.
Results
CMC and Medical Device Characteristics
The study cohort included 98 CMC who were assisted by at least 1 medical device to support an essential body function at the time of enrollment in PCCP. Table 1 summarizes CMC characteristics. The sample had a mean age of 6.5 years and were 49% girls. Most were non-Hispanic white (84%), with half having a primary public payer. The mean travel time from principal residence to the PCCP was 64 minutes (SD 39). On average, enrolled CMC had 4.9 complex chronic conditions, saw 7 subspecialists, took 10 scheduled medications, and spent 24 days in the hospital in the year before enrollment. In-home personal care or respite workers were involved with 35% of CMC.
TABLE 1.
Enrollment Characteristics of Children in a Complex Care Program Assisted by Medical Devices, N = 98
| Characteristic | Quantity |
|---|---|
| No. devices, median (IQR) | 2 (1–2) |
| Age, y, mean (SD) | 6.5 (5.0) |
| Gestational age at birth, wk, mean (SD) | 36.8 (4.2) |
| Girls, n (%) | 48 (49.0) |
| Race and/or ethnicity, n (%) | |
| White, non-Hispanic | 82 (83.7) |
| Black or African American, non-Hispanic | 5 (5.1) |
| Hispanic, any race | 5 (5.1) |
| Other | 6 (6.1) |
| Primary language of guardian, n (%) | |
| English | 94 (95.9) |
| Spanish | 3 (3.1) |
| Parent and/or household status, n (%) | |
| Two-parent | 74 (75.5) |
| Single-parent | 18 (18.4) |
| Foster or guardian | 6 (6.1) |
| Spends time in >1 household, n (%) | 9 (9.2) |
| No. siblings, mean (SD) | 1.9 (2.0) |
| Passive smoke exposure, n (%) | 19 (19.4) |
| Primary payer, n (%) | |
| Public | 49 (50.0) |
| Commercial | 49 (50.0) |
| Distance to hospital, min, mean (SD) | 63.5 (39.3) |
| Complex care program enrollment criteria, past y, mean (SD) | |
| Subspecialists | 7.1 (2.5) |
| Ambulatory clinic visits | 12.6 (8.8) |
| Hospitalizations | 1.7 (1.9) |
| Hospital days | 24.2 (39.8) |
| Complex chronic conditions, mean (SD) | 4.9 (1.7) |
| ED visits, past y, mean (SD) | 2.1 (2.7) |
| Scheduled medications, mean (SD) | 9.8 (6.4) |
| Any care received outside institution, n (%) | 67 (68.4) |
| Additional resources and therapies, n (%) | |
| Occupational therapy | 65 (66.3) |
| Speech therapy | 62 (63.3) |
| Physical therapy | 72 (73.5) |
| Personal care and/or respite worker | 34 (34.7) |
| Early intervention or individualized education plan | 68 (69.4) |
Table 2 illustrates device use among patients on PCCP enrollment. The median number of devices per CMC was 2 (interquartile range [IQR] 1–2). The most commonly used device was gastrostomy tube (79%, Table 2), with 95% using some form of enteral feeding tube. Vagal nerve stimulators were used by 2%, and no patients used pacemakers, dialysis, or insulin pumps. Ventricular shunts represented the type of device that was in place for the longest duration of time when referred to the PCCP (median 78 months, IQR 25.2–120.1).
TABLE 2.
Device Use Combinations on Enrollment to a PCCP
| Patients With Device | Duration of Use | Simultaneous Device Use, n (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Median (IQR), mo | BiPAP and/or CPAP | Home Oxygen | Tracheostomy With Ventilator | Tracheostomy Without Ventilator | Gastrojejunostomy or Jejunostomy Tube | Gastrostomy Tube | Ileostomy and/or Colostomy | Nasogastric or Nasojejunal Tube | Baclofen Pump | Central Venous Catheter | Vagal Nerve Stimulator | Ventricular Shunt | |
| BiPAP and/or CPAP | 10 (10.2) | 12.0 (4.8–51.8) | — | 4 (40)d | 0 (0)a | 1 (9)b | 2 (20)b | 7 (70)d | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a |
| Home oxygen | 23 (23.5) | 8.2 (2.2–15.3) | 4 (17)b | — | 0 (0)a | 4 (17)b | 3 (13)b | 17 (74)d | 1 (4)b | 3 (13)b | 1 (4)b | 1 (4)b | 0 (0)a | 0 (0)a |
| Tracheostomy with ventilator | 7 (7.1) | 20.0 (6.7–48.2) | 0 (0)a | 4 (57)d | — | 0 (0)a | 2 (33)c | 6 (86)e | 1 (14)b | 0 (0)a | 0 (0)a | 1 (14)b | 0 (0)a | 1 (14)b |
| Tracheostomy without ventilator | 7 (7.1) | 55.3 (16.8–127.4) | 0 (0)a | 0 (0)a | 0 (0)a | — | 1 (14)b | 6 (86)e | 0 (0)a | 0 (0)a | 1 (14)b | 2 (29)c | 0 (0)a | 0 (0)a |
| Gastrojejunostomy or jejunostomy tube | 12 (12.2) | 38.2 (9.3–71.8) | 2 (17)b | 3 (25)b | 1 (8)b | 1 (8)b | — | 0 (0)a | 1 (8)b | 0 (0)a | 1 (8)b | 3 (25)b | 0 (0)a | 2 (17)b |
| Gastrostomy tube | 77 (78.6) | 33.3 (6.8–63.4) | 7 (9)b | 17 (23)b | 6 (8)b | 6 (8)b | 0 (0)a | — | 2 (3)b | 0 (0)a | 9 (12)b | 2 (3)b | 2 (3)b | 7 (9)b |
| Ileostomy and/or colostomy | 3 (3.1) | 16.2 (13.6–28.2) | 0 (0)a | 1 (33)c | 1 (33)b | 0 (0)b | 1 (33)c | 2 (67)d | — | 0 (0)a | 0 (0)a | 1 (33)c | 0 (0)a | 0 (0)a |
| Nasogastric or nasojejunal tube | 4 (4.1) | 3.0 (0.8–12.1) | 0 (0)a | 3 (75)d | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | — | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a |
| Baclofen pump | 11 (11.2) | 54.7 (15.9–63.7) | 1 (10)b | 1 (9)b | 0 (0)a | 1 (9)b | 1 (9)b | 9 (82)e | 0 (0)a | 0 (0)a | — | 0 (0)a | 0 (0)a | 1 (9)b |
| Central venous catheter | 6 (6.1) | 29.9 (9.9–48.9) | 0 (0)a | 1 (17)b | 1 (17)b | 2 (33)c | 3 (50)c | 2 (33)c | 1 (17)b | 0 (0)a | 0 (0)b | — | 0 (0)a | 0 (0)a |
| Vagal nerve stimulator | 2 (2.0) | 12.7 (5.0–20.4) | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | 2 (100)e | 0 (0)a | 0 (0)a | 0 (0)a | 0 (0)a | — | 0 (0)a |
| Ventricular shunt | 11 (11.2) | 78.0 (25.2–120.1) | 0 (0)a | 0 (0)a | 1 (9)b | 0 (0)a | 2 (18)b | 7 (64)d | 0 (0)a | 0 (0)a | 1 (9)b | 0 (0)a | 0 (0)a | — |
—, not applicable.
0%
>0%–25%
26%–50%
51%–75%
>75%
Device Complication ED Visits
A total of 228 ED visits among 64 CMC (median [IQR] per CMC was 0 [0–1]) were identified in the year before enrollment. Interrater reliability for the first and second 50 random encounters as well as overall consensus ratings are shown in Table 3. Final κ was 0.89 for ED, with 31% overall designated as related to device complications in most circumstances. Only 2% of ED visits were rated “Uncertain.”
TABLE 3.
Consensus Ratings and Interrater Reliability for Hospitalizations or ED Visits due to Device Complications
| ED Visits, N = 228 | Hospitalizations, N = 258 | |
|---|---|---|
| Scale rating, No. cases (%) | ||
| 0: Encounter due to original device placement | 0 (0.0) | 15 (5.8) |
| 1: Encounter unrelated to device complication in most circumstances | 153 (67.1) | 194 (75.2) |
| 2: Uncertain | 5 (2.2) | 5 (1.9) |
| 3: Encounter related to device complication in most circumstances | 70 (30.7) | 44 (17.1) |
| κ, first 50 encounters | 0.62 | 0.77 |
| κ, second 50 encounters | 0.89 | 0.94 |
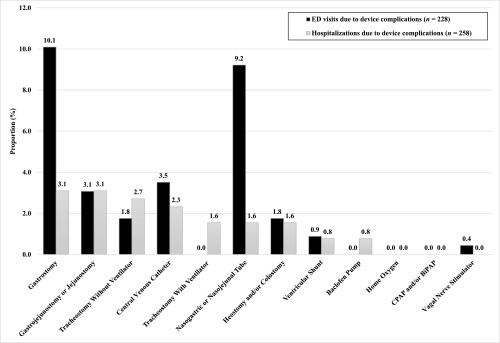
The proportion of ED visits that were due to device complications for each device are shown in Fig 1. The devices whose complications accounted for the largest proportion of total ED visits were gastrostomy tubes (10.1% of all ED visits), nasogastric and/or nasojejunal tubes (9.2%), and central venous catheters (3.5%). Together, these 3 devices accounted for nearly one-fourth of all-cause ED visits.
FIGURE 1.
Proportion of all ED visits and hospitalizations due to specific device complications.
Bivariate associations were observed between ED visits for device complications and the presence of specific devices (central venous catheters, gastrostomy tube, ileostomy and/or colostomies), race and/or ethnicity, number of scheduled medications, and presence of in-home personal care and/or respite workers (Table 4). In multivariate analyses (Table 5), no child and family, health care, or severity of illness variables were significantly associated with encounters being due to device complications. However, ED visits were more likely to be for any device complication when patients had central venous catheters (adjusted odds ratio [aOR] 3.2 [95% confidence interval (CI) 1.1–9.5]).
TABLE 4.
Associations Between Encounter Characteristics and ED Visits or Hospitalizations due to Any Device Complications: Unadjusted Regressions
| Characteristic | Any Device Complication ED Visit | Any Device Complication Hospitalization |
|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Device presenta | ||
| Baclofen pump | 1.1 (0.3–3.9) | 0.6 (0.1–2.5) |
| BiPAP and/or CPAP | 0.6 (0.1–5.1) | 1.5 (0.4–5.7) |
| Central venous catheter | 6.4 (1.9–21.2)** | 6.6 (2.1–20.6)** |
| Gastrostomy | 0.4 (0.2–0.7)** | 0.7 (0.4–1.4) |
| Gastrojejunostomy or jejunostomy | 1.8 (0.9–3.7) | 3.9 (1.8–8.4)** |
| Home oxygen | 0.6 (0.2–1.3) | 1.1 (0.5–2.4) |
| Ileostomy and/or colostomy | 4.0 (1.5–10.9)** | 2.0 (0.6–6.8) |
| Nasogastric or nasojejunal tube | 1.1 (0.3–4.7) | — |
| Tracheostomy without ventilator | 1.9 (0.5–7.1) | 3.7 (1.4–9.8)** |
| Tracheostomy with ventilator | 0.7 (0.2–2.5) | 4.2 (1.7–10.2)** |
| Vagal nerve stimulator | 0.2 (0.0–1.9) | — |
| Ventricular shunt | 1.0 (0.3–3.4) | 2.1 (0.8–5.7) |
| No. devices | 1.0 (0.7–1.4) | 1.6 (1.2–2.2)** |
| Race and/or ethnicity | ||
| White, non-Hispanic | Ref | Ref |
| Black or African American, non-Hispanic | 0.2 (0.0–2.0) | 1.3 (0.4–4.4) |
| Hispanic (any race) | 0.4 (0.2–0.8)* | — |
| Complex chronic conditions | 1.0 (0.8–1.2) | 1.2 (1.0–1.5) |
| ED visits (past y) | 1.1 (1.0–1.2) | 1.0 (0.9–1.1) |
| Scheduled medications | 0.9 (0.9–1.0)* | 1.0 (1.0–1.1) |
| Any care received outside institution | ||
| Yes | Ref | Ref |
| No | 1.4 (0.7–2.9) | 1.5 (0.7–3.2) |
| Additional resources, therapies | ||
| Occupational therapy | 0.7 (0.4–1.4) | 0.6 (0.3–1.2) |
| Speech therapy | 0.6 (0.3–1.2) | 0.9 (0.4–1.8) |
| Physical therapy | 0.7 (0.3–1.4) | 0.5 (0.3–1.0)* |
| Personal care and/or respite worker | 0.4 (0.2–0.9)* | 1.9 (0.9–3.7) |
| Early intervention or individualized education plan | 0.7 (0.4–1.2) | 1.1 (0.6–2.3) |
—, not applicable.
Device present or absent at the time of encounter.
P < .05; ** P < .01.
TABLE 5.
Associations Between Encounter Characteristics and ED Visits or Hospitalizations due to Any Device Complications: Adjusted Regressions
| Characteristic | Any Device Complication ED Visit | Any Device Complication Hospitalization |
|---|---|---|
| aORa (95% CI) | aORb (95% CI) | |
| Device presentc | ||
| Gastrojejunostomy or jejunostomy | — | 3.3 (1.5–7.5)** |
| Tracheostomy without ventilator | — | 4.5 (1.7–7.5)** |
| Tracheostomy with ventilator | — | 8.1 (2.3–28.5)** |
| Central venous catheter | 3.2 (1.1–9.5)* | — |
—, not applicable.
ED visit models adjusted for type of device, race and/or ethnicity, number of scheduled medications, and presence of a personal care and/or respite worker. Only significant associations are shown.
Hospitalization models adjusted for type of device, number of devices, and presence of physical therapy. Only significant associations are shown.
Device present or absent at the time of encounter.
P < .05; ** P < .01.
Device Complication Hospitalizations
A total of 258 hospitalizations among 81 CMC (median [IQR] per CMC was 0 [0–1]) were identified in the year before enrollment. Final κ was 0.94 for hospitalizations, suggesting excellent agreement. Overall, 17% of hospitalizations were designated as related to device complications in most circumstances. Only 2% of hospitalizations were rated as “Uncertain.” Nearly 6% of CMC hospitalizations were related to original device placement.
The proportion of hospitalizations that were due to device complications for each device are shown in Fig 1. The devices whose complications accounted for the largest proportion of total hospitalizations were gastrostomy tubes (3.1%), gastrojejunostomy and/or jejunostomy tubes (3.1%), or tracheostomies without ventilator (2.7%), which, when taken together, accounted for nearly 10% of all-cause hospitalizations.
Bivariate associations were also observed between hospitalizations for device complications and specific devices (central venous catheters, gastrojejunostomy and/or jejunostomy, tracheostomy with or without ventilator), number of devices, and receipt of physical therapy. In multivariate analyses (Table 5), no child and family, health care, or severity of illness variables were significantly associated with hospitalizations being due to device complications. However, hospitalizations were more likely to be for any device complications when patients had gastrojejunostomy and/or jejunostomy tubes (aOR 3.3 [95% CI 1.5–7.5]) or tracheostomies with or without ventilator use (aOR 8.1 [95% CI 2.3–28.5] and aOR 4.5 [95% CI 1.7–7.5], respectively).
Discussion
This study represents some of the first data to rigorously quantify ED visits and hospitalizations due to device complications within a cohort of CMC, and we highlight that 3 specific devices (central venous catheters, gastrostomy tubes, and nasogastric and/or nasojejunal tubes) accounted for nearly one-fourth of all ED visits. We observed that most CMC are assisted by multiple devices and that encounters due to device complications comprise a substantial subset of overall ED and hospital encounters, accounting for >30% of all-cause ED encounters and >17% of all-cause hospitalizations in our sample. Therefore, 1 potential strategy to reduce overall CMC use may be to focus on reducing device complications. These findings will be used in future research to study changes in device complication–related ED and hospital use over time and to study interventions to lower CMC hospitalizations by reducing these device complication encounters.
One of the only other studies in which researchers quantified the contribution of device complications to CMC hospital use contained an observation of a smaller, albeit sizable, proportion.3 We suspect the lower rate of 9% identified in that study compared with our rate of 17% was due to at least 3 factors: first, they evaluated events after enrollment into complex care, which might prevent some visits; second, they identified device complications using diagnosis and procedure codes, which may have lower sensitivity than more comprehensive chart review; and third, their study included all CMC encounters, whereas our study included only encounters among children assisted by devices.
As an initial step to better understanding these visits, we aimed to uncover their associations with child and/or family, health care, and severity of illness characteristics. Despite including a relatively broad set of predictors, we did not find associations between device complication visits and child and/or family or health care variables. Determining whether this observation was driven by a true lack of association or limited power is an important next step with larger samples. Instead, the presence of specific devices themselves appeared to have the strongest independent relationships with device complication–related encounters: central venous catheters for ED visits and gastrojejunostomy tubes and tracheostomies for hospitalizations.
From a clinical perspective, many of our current paradigms may necessitate ED or hospital encounters for complications of these 3 devices. For example, jejunostomy tube problems such as obstruction or dislodgement are relatively common yet difficult to manage outside of the hospital.26 Children assisted by these devices often have no safe alternative routes for hydration, nutrition, or medication administration. Furthermore, replacement frequently requires involvement of interventional radiology or pediatric surgery, who can have limited availability on nights, holidays, and weekends. As a result, CMC may be hospitalized until needed services are available. Eliminating these hospitalizations likely requires tube maintenance strategies that minimize complications, specific institutional care pathways to expedite replacement during “off-hours,” and new equipment or techniques27 that could support safe replacement by families and ambulatory providers.
Many of these same concepts are paralleled for children hospitalized with tracheostomy or central venous catheter complications. In 1 study, researchers evaluated hospitalizations after beginning mechanical ventilation and found that 40% of children were rehospitalized for complications within 12 months of discharge.19 Similarly, hospital readmissions due to bacterial respiratory tract infections occurred in 36% of children over a median 275 days after tracheostomy placement in a large study.28 When looking at all reasons for readmission posttracheostomy, 92% were unplanned and 64% were associated with acute respiratory illness.29 Children with central venous catheters also frequently have clinical triggers directing them to seek ED care (eg, fever). Because of the potential need for evaluation in such circumstances, reducing ED visits for central venous catheter complications might require the development of alternatives for these evaluations outside of the ED. Whether novel clinical decision rules could guide when urgent evaluation for cultures and empirical antibiotics could safely be avoided (eg, when a viral source is highly likely) is not known.
There were at least 2 important domains from our conceptual models (Supplemental Table 6)14,30 unavailable in this analysis: health care system support for families and self-efficacy to manage medical devices. Subsequent prospective research should aim to incorporate the presence and quality of education and ongoing support available to CMC caregivers and whether device-complications can be reduced with specific educational or support interventions. The role primary care providers can play in preventing or managing these complications would benefit from additional study. For example, improving communication around anticipatory guidance and contingency planning for these devices may prove effective. Personal care workers, which our data suggest could be protective of ED visits, may be valuable to include in future intervention research. This would be consistent with a large case-control study in which researchers observed that receipt of home nursing was associated with less postdischarge hospital use31 and a related study revealing that medical devices comprised a large proportion of challenges identified by home nurses.32 Lastly, clarifying relationships between device-complication encounters and measures of caregiver health literacy, skill and confidence to manage these devices would be valuable next steps.
Building on this work to identify device-complication encounters, an important next step will be to quantify the extent to which these visits are preventable. Researchers for 1 prospective study assessed preventability of unscheduled ICU admissions by chart review and found that 19% of admissions in the technology-assisted chronic illness group were potentially preventable,33 although it is not clear how many of those were due to device complications.
We suspect that device complications likely reflect a spectrum of preventability. For example, among patients with tracheostomies, admission for tracheitis may be avoidable either by prevention altogether (ie, reliable supplies and high-quality tracheostomy care) or by rapid identification and timely initiation of outpatient treatment at the onset of symptoms. Whether a ventriculoperitoneal shunt malfunction can be prevented, on the other hand, is less clear.34,35 Reliable and valid approaches to assign preventability to these encounters are needed. Identifying the potentially preventable subset of device complication encounters would support design and testing of more precise interventions.
Complex care programs, which promise to reduce CMC ED and hospital use through intensive care coordination and medical comanagement,36 provide a potential strategy to reduce device-complication encounters. By focusing on reducing caregiver unmet needs for personal and community resources, consistent access to supplies and knowledgeable providers, and proactive crisis planning, complex care programs offer several potential mechanisms for reducing these visits.7,14,30,37 As a future study, we plan to evaluate the change in device-complication visits after enrollment into our complex care program and compared with a propensity-matched CMC cohort.
This study should be interpreted with several limitations in mind. First, findings from our single-center, complex care program population may not generalize to other programs or patients. Our population demographics reflect this region of the country and may not generalize to regions with different demographics. Similarly, the sample’s relative homogeneity likely limited power to detect associations between sociodemographics and device-complications. Second, we identified patients at the time of referral or enrollment into our program, which might select a recent period of illness instability and be less representative of other times in the natural history of their condition. Third, our chart reviews were labor-intensive and developing feasible approaches to identify device-complication visits from larger data sources and diverse clinical settings is an important future step. EHR research methods like natural language processing may allow for more efficient study over larger patient populations. Fourth, although we reviewed Epic’s Care Everywhere function, we may not have captured all ED and inpatient encounters since many children received at least some care outside the institution. Fifth, we did not assess cost of visits related to device complications. Future researchers should estimate savings achieved through interventions designed to reduce visits related to device complications. Finally, in the absence of a gold standard definition for medical device assistance, our threshold for device inclusion was Feudtner’s definition of technology dependence.23 Applying this definition, however, is subject to investigator bias. As such, we may have underestimated total visits due to device complications by excluding certain devices that are more transiently used and less consistently identified in the EHR (eg, insufflation and/or exsufflation machines, suction or nebulizer machines, and adaptive equipment such as orthotics or wheelchairs). Although our rating scale for device complications had high interrater reliability across 3 reviewers and went through several rounds of revisions, it is still possible that some encounters may have been coded differently by different reviewers.
Despite these limitations, this work has a number of important implications. Based on their volume and potential modifiability, device-complication visits represent a high-yield subset of CMC encounters. Three devices accounted for nearly one-fourth of ED visits in CMC with devices and may be productive targets for focused intervention. Beyond lowering health services use, interventions designed to eliminate device-complication visits might plausibly improve other meaningful and related outcomes. For example, the activities to reduce device complications could inherently lead to improvements in caregiver self-efficacy and caregiving stress. Experiencing fewer device complications may translate to less caregiver-missed work or CMC-missed school. A focus on reducing device complications may prove to be a valuable approach to more generally improving CMC care quality, experience, and value.
Footnotes
Ms Nackers assisted with project conceptualization and study design, collected data and conducted preliminary analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Ehlenbach assisted with project conceptualization, data collection, and data interpretation as well as critical revisions of the manuscript; Drs Kelly and Werner assisted with data interpretation and critically revised the manuscript; Ms Warner coordinated and supervised data collection and critically reviewed the manuscript; Dr Coller conceptualized and designed the study, oversaw data analysis, and drafted the initial manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the Clinical and Translational Science Award program, through the National Institutes of Health National Center for Advancing Translational Sciences, grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry JG, Hall M, Neff J, et al. Children with medical complexity and Medicaid: spending and cost savings [published correction appears in Health Aff (Millwood). 2015;34(1):189]. Health Aff (Millwood). 2014;33(12):2199–2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry JG, Agrawal R, Kuo DZ, et al. Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. J Pediatr. 2011;159(2):284–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berry JG, Hall M, Cohen E, O’Neill M, Feudtner C. Ways to identify children with medical complexity and the importance of why. J Pediatr. 2015;167(2):229–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuo DZ, Houtrow AJ; Council on Children With Disabilities. Recognition and management of medical complexity. Pediatrics. 2016;138(6):e20163021. [DOI] [PubMed] [Google Scholar]
- 7.Coller RJ, Nelson BB, Sklansky DJ, et al. Preventing hospitalizations in children with medical complexity: a systematic review. Pediatrics. 2014;134(6). Available at: www.pediatrics.org/cgi/content/full/134/6/e1628 [DOI] [PubMed] [Google Scholar]
- 8.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011;165(11):1020–1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuo DZ, Melguizo-Castro M, Goudie A, Nick TG, Robbins JM, Casey PH. Variation in child health care utilization by medical complexity. Matern Child Health J. 2015;19(1):40–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heaton J, Noyes J, Sloper P, Shah R. Families’ experiences of caring for technology-dependent children: a temporal perspective. Health Soc Care Community. 2005;13(5):441–450 [DOI] [PubMed] [Google Scholar]
- 13.Thomson J, Shah SS, Simmons JM, et al. Financial and social hardships in families of children with medical complexity. J Pediatr. 2016;172:187–193.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson BB, Coller RJ, Saenz AA, et al. How avoidable are hospitalizations for children with medical complexity? Understanding parent perspectives. Acad Pediatr. 2016;16(6):579–586 [DOI] [PubMed] [Google Scholar]
- 15.Spratling R. Understanding the health care utilization of children who require medical technology: a descriptive study of children who require tracheostomies. Appl Nurs Res. 2017;34:62–65 [DOI] [PubMed] [Google Scholar]
- 16.Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124(2):563–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graf JM, Montagnino BA, Hueckel R, McPherson ML. Pediatric tracheostomies: a recent experience from one academic center. Pediatr Crit Care Med. 2008;9(1):96–100 [DOI] [PubMed] [Google Scholar]
- 18.Okido AC, Pina JC, Lima RA. Factors associated with involuntary hospital admissions in technology-dependent children [in Portuguese]. Rev Esc Enferm USP. 2016;50(1):29–35 [DOI] [PubMed] [Google Scholar]
- 19.Kun SS, Edwards JD, Ward SL, Keens TG. Hospital readmissions for newly discharged pediatric home mechanical ventilation patients. Pediatr Pulmonol. 2012;47(4):409–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chien YH, Tsao PN, Chou HC, Tang JR, Tsou KI. Rehospitalization of extremely-low-birth-weight infants in first 2 years of life. Early Hum Dev. 2002;66(1):33–40 [DOI] [PubMed] [Google Scholar]
- 21.Silva DT, Hagan R, Sly PD. Home oxygen management of neonatal chronic lung disease in Western Australia. J Paediatr Child Health. 1995;31(3):185–188 [DOI] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feudtner C, Villareale NL, Morray B, Sharp V, Hays RM, Neff JM. Technology-dependency among patients discharged from a children’s hospital: a retrospective cohort study. BMC Pediatr. 2005;5(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feudtner C, Levin JE, Srivastava R, et al. How well can hospital readmission be predicted in a cohort of hospitalized children? A retrospective, multicenter study. Pediatrics. 2009;123(1):286–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fortunato JE, Darbari A, Mitchell SE, Thompson RE, Cuffari C. The limitations of gastro-jejunal (G-J) feeding tubes in children: a 9-year pediatric hospital database analysis. Am J Gastroenterol. 2005;100(1):186–189 [DOI] [PubMed] [Google Scholar]
- 27.Schlager A, Arps K, Siddharthan R, Rajdev P, Heiss KF. The “omega” jejunostomy tube: a preferred alternative for postpyloric feeding access. J Pediatr Surg. 2016;51(2):260–263 [DOI] [PubMed] [Google Scholar]
- 28.Russell CJ, Thurm C, Hall M, Simon TD, Neely MN, Berry JG. Risk factors for hospitalizations due to bacterial respiratory tract infections after tracheotomy. Pediatr Pulmonol. 2018;53(3):349–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu H, Mamey MR, Russell CJ. Factors associated with 30-day all-cause hospital readmission after tracheotomy in pediatric patients. Int J Pediatr Otorhinolaryngol. 2017;103:137–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coller RJ, Nelson BB, Klitzner TS, et al. Strategies to reduce hospitalizations of children with medical complexity through complex care: expert perspectives. Acad Pediatr. 2017;17(4):381–388 [DOI] [PubMed] [Google Scholar]
- 31.Gay JC, Thurm CW, Hall M, et al. Home health nursing care and hospital use for medically complex children. Pediatrics. 2016;138(5):e20160530. [DOI] [PubMed] [Google Scholar]
- 32.Wells S, O’Neill M, Rogers J, et al. Nursing-led home visits post-hospitalization for children with medical complexity. J Pediatr Nurs. 2017;34:10–16 [DOI] [PubMed] [Google Scholar]
- 33.Dosa NP, Boeing NM, Ms N, Kanter RK. Excess risk of severe acute illness in children with chronic health conditions. Pediatrics. 2001;107(3):499–504 [DOI] [PubMed] [Google Scholar]
- 34.Hain PD, Gay JC, Berutti TW, Whitney GM, Wang W, Saville BR. Preventability of early readmissions at a children’s hospital. Pediatrics. 2013;131(1). Available at: www.pediatrics.org/cgi/content/full/113/1/e171 [DOI] [PubMed] [Google Scholar]
- 35.Stein SC, Guo W. Have we made progress in preventing shunt failure? A critical analysis. J Neurosurg Pediatr. 2008;1(1):40–47 [DOI] [PubMed] [Google Scholar]
- 36.Mosquera RA, Avritscher EB, Samuels CL, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312(24):2640–2648 [DOI] [PubMed] [Google Scholar]
- 37.Kuo DZ, Berry JG, Glader L, Morin MJ, Johaningsmeir S, Gordon J. Health services and health care needs fulfilled by structured clinical programs for children with medical complexity. J Pediatr. 2016;169:291–296.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]