Abstract
Introduction
We developed a new smartphone application to deliver an automated external defibrillator (AED) to out-of-hospital cardiac arrest scene. The aim of this study was to evaluate whether an AED could be delivered earlier with or without an application in a simulated randomized controlled trial.
Methods
Participants, who were asked to work as bystanders, were randomly assigned to either an application group or control group and were asked to bring an AED in both groups. The bystanders in the application group sent a signal notification using the application to two responders, who were stationed within 200 meters of the arrest scene, to carry an AED. The primary outcome was the AED delivery time by either the bystander or his/her responder.
Results
In total, 61 bystanders were eligible and randomized to either the application group (32) or the control group (29). The 52 with time data were available and analyzed. The AED delivery time by either the bystander or his/her responder was significantly shorter in the application group than in the control group [133.6 (44.4) seconds vs. 202.2 (122.2) seconds, P = 0.01].
Conclusions
In this simulation-based trial, AED delivery time was shortened by our newly developed smartphone application for the bystander to ask nearby responders to find and bring an AED to the cardiac arrest scene (UMIN-Clinical Trials Registry 000016506).
Key Words: Cardiac arrest, cardiopulmonary resuscitation, automated external defibrillator, social media technology, simulation
Sudden cardiac arrest is a major public health problem in the developed world with approximately 70,000 cases occurring every year in Japan.1–5 The “chain of survival” is a pathway of care for cardiac arrest patients and is the major contribution to the improved survival after out-of-hospital cardiac arrest (OHCA).3,6 Early cardiopulmonary resuscitation (CPR) and shocks with the automated external defibrillator (AED) before the arrival of ambulance vehicles are essential to increase survival after OHCA.7–11 However, despite recurrent updates of the guidelines for CPR and the spread of the “chain- f survival,” many areas have suboptimal survival rates, remaining low at approximately 10%.12,13
Japan is one of the most advanced countries where the cumulative number of public access AEDs exceeded 500,000 in 2014.14 The latest population-based report has shown that AED shocks before the arrival of ambulances contribute to improving outcomes of OHCAs.15 However, only 4.5% patients of witnessed OHCA of cardiac origin received AED shocks before the arrival of ambulances in Japan.13 One of the possible reasons for this low proportion of AED use may be the difficulty for lay rescuers witnessing cardiac arrests to find a nearby AED and provide CPR, whereas it would be difficult for rescuers who can provide CPR and use an AED to find the cardiac arrest scene. To resolve this problem, the 2015 International Consensus on CPR and Emergency Cardiovascular Care Science with Treatment Recommendations encourages to use social media technologies to increase CPR and AED use by lay rescuers.16 A recent study showed that social media technology could contribute to increasing the number of bystanders before arrival of paramedics and the frequency of bystander CPR in the real setting.17 However, it is still unknown how much time from an OHCA occurrence to an AED shock delivery such an innovative system would shorten. We developed a new smartphone application that sends a signal indicating the locations of the OHCA and AEDs on the smartphone display of the responders.
The aim of this study was to evaluate the effectiveness of this new application using a simulated cardiac arrest scenario.
METHODS
Study Design
We conducted a scenario-based randomized controlled study on March 17 and 18, 2015.
Study Setting
The study was conducted in the Kyoto University Uji campus, which had an area of 0.22 km2 and 13 AEDs approximately 300 meters apart from each other. All AEDs, which bystanders or responders could reach in the area of this study, were registered in the application.
Smartphone Application
The researchers of this study and Coaido, Inc, developed a smartphone application that can send a signal notification about an occurrence of OHCA to the nearby smartphones. It indicates the location of the OHCA event and nearby AEDs on the display of a smartphone (Fig. 1). When bystander who has installed this application in his/her smartphone encounters with an OHCA event, he/she activates the application and sends a signal notification to the responders. Responders' application is activated automatically. When receiving the notification, which is not a text message but alert, the responders try to find a nearby AED and bring it to the OHCA scene according to the information on the display. The bystander also can know the location of nearby AEDs and bring an AED by himself/herself using the application.
FIGURE 1.
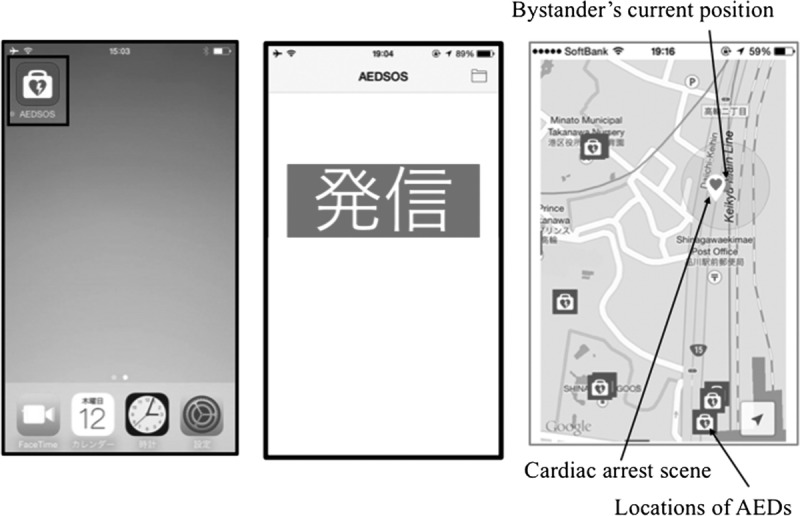
Three points of the application working. A, Bystanders who encounter out-of-hospital cardiac arrest patient activate the application. B, After activating the application, bystanders push call button. C, Map indicating bystander’s current position, location of cardiac arrest, and nearby AEDs were shown on the screen.
Study Participants
Two types of participants 18 years or older who would act as a “bystander” and a “responder” were recruited from the general public. Those who were unable to carry an AED were excluded because of their physical disabilities.
For bystanders, persons who were not familiar with the area of Kyoto University Uji campus were invited through the local CPR training networks and billboard advertisements in February and March 2015. For responders, persons who were familiar with the area of Kyoto University Uji campus including faculty, staff, and students of Kyoto University were invited via billboard advertisements and Kyoto University Web site during the same period. In addition, we explained an outline, a role of responders, a length of time commitment, and an incentive of this study to the candidates of responders during the prebriefing.
Randomization
We asked bystanders and responders about their age, sex, and previous CPR training before randomization. Because physical differences in sex have an influence on AED delivery,18 bystanders were randomly assigned to either the intervention group (application group) or the control group in a 1:1 ratio using permuted blocks after stratification by sex. A computer-generated randomization list was provided by an independent biostatistician. The allocation was notified to the bystanders at the trial site just before the trial.
Intervention
Five OHCA scenarios with different locations were prepared. Four locations were outside the building, and one was on the second floor in a building. All locations were within 150 (50) meters of the nearest AEDs. The researchers decided the order of the provided scenarios in advance, considering the time schedule.
One bystander and two responders were stationed for each scenario. Then, smartphones with the application were provided to the bystanders and the responders in the application group. On the other hand, only one bystander with no smartphones was stationed for each scenario in the control group. We explained how to use the application to the bystanders and responders in the application group before starting the trial. To teach bystanders how to use the application without using the actual smartphone that had this application installed, we provided an approximately 10-minute presentation with illustrations. We asked responders to attend 1 hour before the evaluation on the day of the trial and taught them using the actual smartphone that had this application installed.
In each scenario, the bystander encountered an OHCA event and was asked to bring an AED by the witness. Using a case-based scenario, bystanders were taken to their respective OHCA locations by the researchers and given the following: “Imagine, someone collapsed in front of you. He does not respond at all. I will perform CPR. So, please look for and bring an AED as soon as possible!” After the presentation, the AED delivery time and the travel distance by bystanders and responders were measured. The bystander in the application group activated the smartphone application and sent a signal notification to the two responders to carry an AED, and then, the bystander himself/herself also looked for a nearby AED using the application. All the responders were stationed in several staying places within 200 meters of the OHCA scene during the evaluation, but they were not informed when they would receive the signal notification and where the arrest would occur. Only two of the responders in each scenario were informed when they would receive the signal notification a few minutes before the evaluation. The AED delivery time and travel distance of responders from the bystanders' encounter with an OHCA event to the responders' arrival at the scene were recorded by the researchers. After receiving the signal notification from the bystander, the responders looked for an AED in the neighborhood and carried it to the OHCA scene using the application (Fig. 2A). Bystanders in the control group looked for a nearby AED by themselves without the application (Fig. 2B).
FIGURE 2.
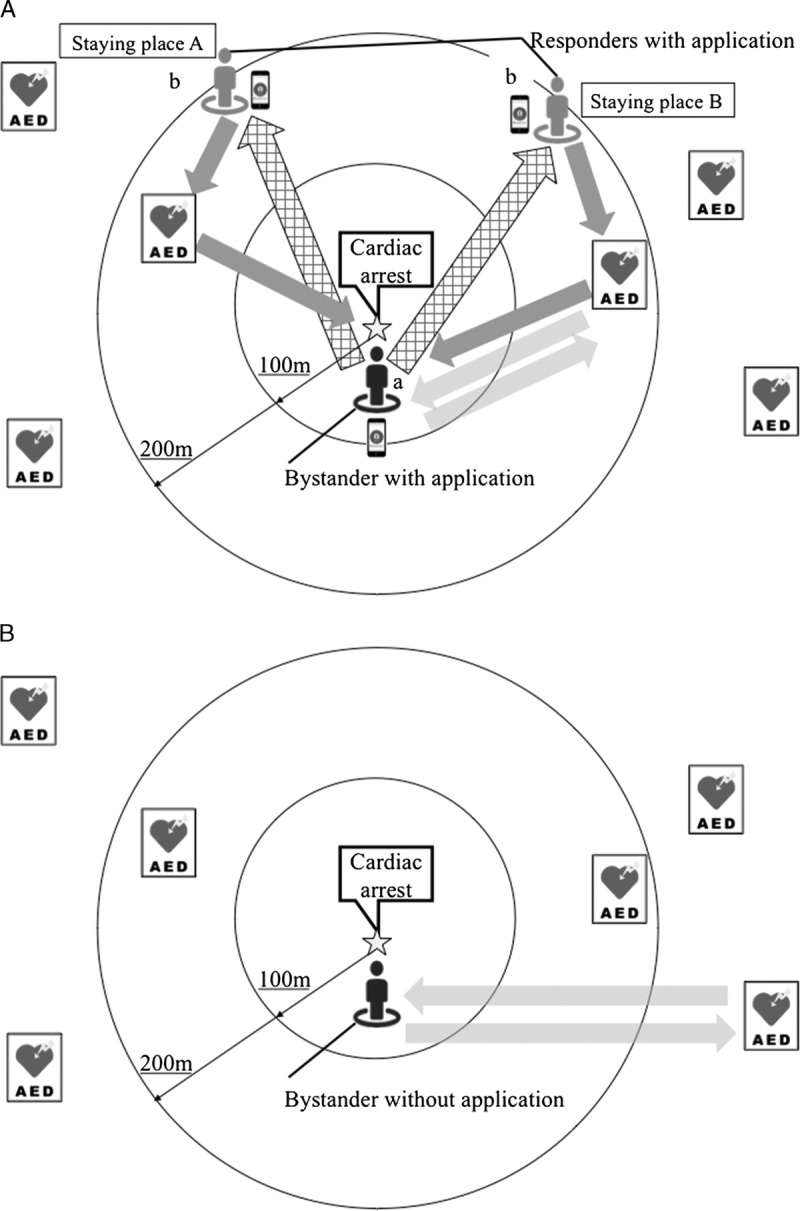
Simulation settings. A, The bystander (a) sent a signal notification to two responders using the application. After receiving the signal notification, the responders (b) looked for an AED in the neighborhood and carried it to the OHCA scene using the application. The bystander (a) himself/herself looked for an AED using the application. B, Bystander (b) looked for an AED by himself/herself without the application.
Data Collection
We placed photos of AED in the location of each AED instead of real AEDs and asked bystanders and responders to bring the photo to the scene as a real AED. A mannequin [Little Anne, Laerdal (Laerdal Medical, Stavanger, Norway)] was regarded as a cardiac arrest patient, and its arranged location was considered as the cardiac arrest scene.
Bystanders' AED delivery time from the AED requirement to the AED arrival at the scene and the travel distances from the OHCA scene to an AED location and from the AED location to the OHCA scene were recorded by the researcher who followed the bystander with a stopwatch and a pedometer. Responders' AED delivery time and travel distance from the responders' staying place to an AED location and from the AED location to the OHCA scene were also recorded by the researcher who followed the respective responders with a stopwatch and a pedometer. We calculated the travel distance based on the stride of the followers multiplied by the steps in the pedometers.
During the data collection, these researchers did not help the bystanders and responders looking for an AED and carrying it to the OHCA scene. Bystanders and responders were allowed to ask lay persons in the Kyoto University Uji campus about AED locations when they wanted to know the location of nearby AED.
Primary Outcome and Secondary Outcomes
The primary outcome was the shorter AED delivery time by either the bystander or the responders. The secondary outcomes were the AED delivery time by the bystander or the responders. Travel distance of the bystander or the responders was also evaluated as secondary outcome. The application has two functions. Firstly, the application shows a map of nearby AED locations on smartphone to find a nearby AED by bystander (function 1). Secondly, the bystander encountered an OHCA event and asked the responders to bring an AED using the application (function 2). We would like to evaluate these two functions, respectively. The AED delivery time by the bystander as secondary outcome was for evaluating function 1. In addition, the AED delivery time by the responders as secondary outcome was for evaluating function 2. The shorter AED delivery time by either the bystander or the responders as primary outcome was for evaluating function 1 and function 2.
Ethical Consideration
The study was carried out under the Declaration of Helsinki from the World Medical Association, the act on the Protection of Personal Information and the Ethical Guidelines for Epidemiological Research of Japan.19,20 Participants submitted their written informed consent before participation. The research protocol was approved by the ethics committee of Kyoto University Graduate School of Medicine. The clinical trial number is UMIN Clinical Trials Registry 000016506.
Statistical Analysis
We assumed that the application would cause a 30% reduction in AED delivery time referring to previous articles and the quality of the application.21 Based on 0.8 power to detect a significant difference (P = 0.05, two-sided), 29 participants were required for each study group. To compensate for possible absences, the sample size was estimated to be 60 in total.
Baseline characteristics and outcomes were compared between the groups using χ2 test for categorical variables and Student t test for numerical variables. A two-way analysis of variance for continuous variables was conducted to adjust for sex. All of the tests were two-tailed, and a P value of less than 0.05 was considered statistically significant. Statistical analyses were performed using SPSS Version 22.0J (IBM Corp, Armonk, NY).
RESULTS
Participants' Flow and Baseline Characteristics
A total of 61 volunteers participated in this trial as bystanders. All of them were eligible and randomly assigned to either the application group (n = 32) or the control group (n = 29). Four bystanders in the application group and three in the control group did not attend the trial because of their health problems, urgent business, or other reasons. We failed to obtain data from two bystanders in the application group because of our simple technical errors, and the remaining 26 (81.3%) in the application group and 26 (89.7%) in the control group were involved in the final analysis of primary outcome (Fig. 3). Similarly, the travel distance of five bystanders in the application group and three in the control group were not obtained by the technical errors. Although we recognized that one problem is shortage of the number of participants, we stopped enrolling additional subjects before hitting estimated sample size for the following reasons. We spent several months preparing for this study such as obtaining permission to use university facilities. Kyoto University allowed us to use the facilities for this study during the students' spring break; however, we could not add another period. In addition, we thought that it would be difficult to evaluate the application in the same situation, if we did not conduct this study at once.
FIGURE 3.
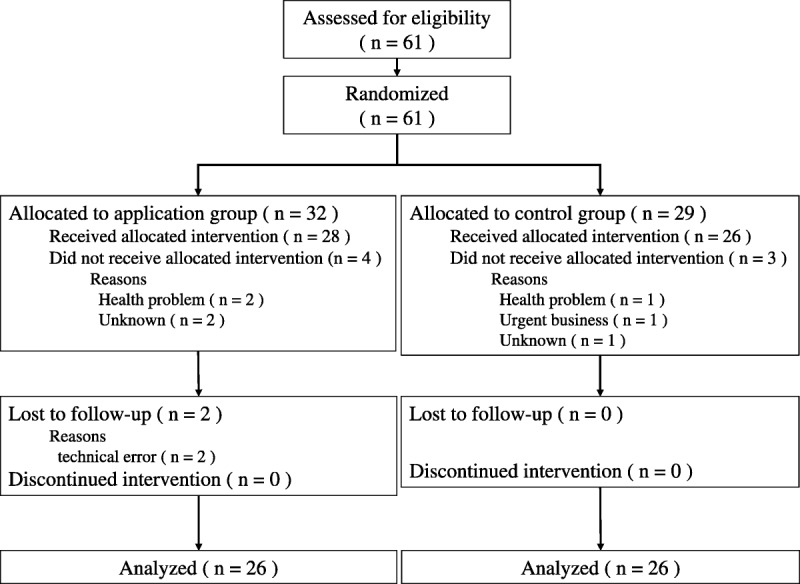
Participants’ (bystanders’) flow.
Fifteen volunteers applied for the trial as responders. All of them were eligible, and two of them per each scenario were assigned as responders independent of the allocation of the bystanders.
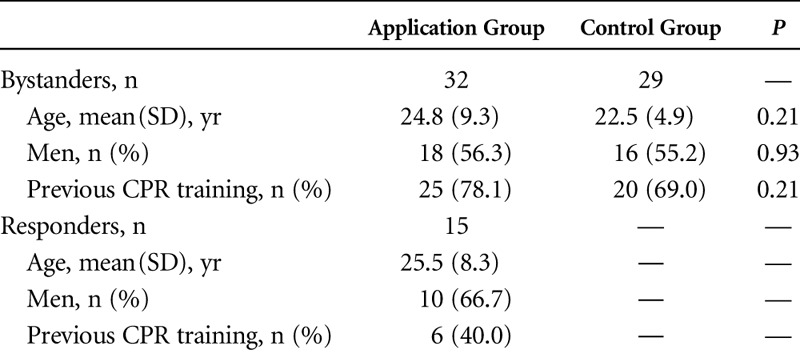
Baseline characteristics of bystanders and responders are shown in Table 1. There were no significant differences in age, sex, and previous CPR training between the bystanders in the two groups.
TABLE 1.
Baseline Characteristics of Bystanders and Responders
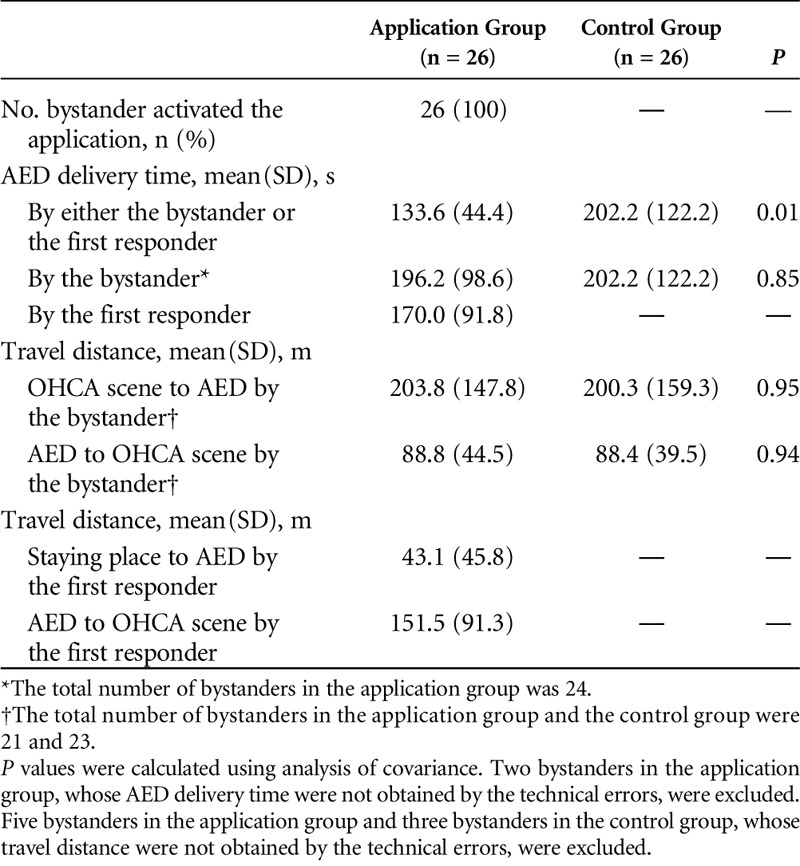
Time and Travel Distance for AED Delivery
We carried out from 9:00 am to 6:00 pm during 2 days. First day, it was fine but it was raining on the second day late in the afternoon. All the bystanders in this study could push SOS button to activate the application. All the responders were able to react to the signal notification from the bystanders in the application group, and all of them could find the AED using the application. Table 2 shows the primary outcome and secondary outcomes of the trial according to the intervention. The AED delivery time by either the bystander or the responders was significantly shorter in the application group than in the control group [133.6 (44.4) seconds vs. 202.2 (122.2) seconds, P = 0.01], whereas the AED delivery time by the bystander was similar in both groups [196.2 (98.6) seconds vs. 202.2 (122.2) seconds, P = 0.83]. The travel distance from the OHCA scene to an AED location by the bystander [203.8 (147.8) m vs. 200.3 (159.3) m, P = 0.95] and from an AED location to the OHCA scene [88.8 (44.5) m vs. 88.4 (39.5) m, P = 0.94] was similar in both groups.
TABLE 2.
The AED Delivery Time and Travel Distance
DISCUSSION
In this simulation randomized controlled trial, the AED delivery time by either the bystander or the responders was about 1 minute shorter in the application group than in the control group. Although bystanders in the application group were able to use the map of nearby AEDs on smartphone to deliver an AED by himself/herself, the AED delivery time by the bystander was similar in both groups. Thus, recruiting responders on the scene using the application can be regarded as an important factor to reduce AED delivery time. The responders to the signal notification from the application would play a pivotal role in delivering an AED.
The approach to shorten the time to resuscitation by lay rescuers in real practices has been tried with the development of social media technology.22–26 We developed the “Mobile AED Map” to find a nearby AED and evaluated the time for AED delivery and travel distance in our previous study, but we failed to prove its effectiveness.21 Insufficient quality of the AED map displayed on cell phones and bothersome handling procedure was the main possible explanations for the negative trial result. Because smartphone specifications is making remarkable advances, the quality of smartphone applications has become worth using in emergency settings.22–26 Technical advances of smartphones would be one of the reasons to show the effectiveness of our new application. A recent clinical study demonstrated that the use of mobile application could shorten the time of AED delivery and CPR by lay rescuers, comparing with text message-based system.27 In real practice, responders called by applications would be familiar with nearby setting, and it could be easier for them to find and bring a nearby AED to the OHCA scene than the first responder who are not familiar with the area.
In this simulation trial, the responders waited in a staying place within 200 meters of the OHCA scene. A previous clinical randomized study with a mobile-phone positioning system in which responders received the alarm within 500 meters of the OHCA scene successfully demonstrated to increase the proportion of bystander CPR from 48% (172/360 patients) to 62% (188/305 patients).20 Appropriate distance from an OHCA scene to nearby responders would be different depending on the number of registered responders near the arrest scene. In addition, because this was a simulation study, all responders reacted to the signal notification from the application. Another previous report in real setting showed that 68% of lay persons received the signal from the social media technology, but only 16.5% of them arrived at an OHCA scene.23 Before our new application is introduced into the real world, the appropriate distance of signal delivery and the number of registered responders should be estimated considering actual situations referring to such simulation studies. It is also essential to ensure the safety of resuscitation procedures and to avoid excess burden for lay responders.
This study has several limitations. First, this was a simulation study in an ideal setting to evaluate the effectiveness of this application. Second, the results might not be generalized because most bystanders and responders were young adults who are familiar with smartphone and are rush to the scene. We need a clinical research involving various bystanders and responders in real emergency settings. Third, as in previous studies evaluating smartphone application, the results may not be reproduced in other smartphone because they depend on the performance of the smartphone. Because this study was an open randomized controlled trial, we were not able to conceal the allocation to both participants and researchers. To minimize this bias, we notified the allocation to participants at the trial site just before the trial. In addition, to keep the quality of interventions, a simulation-scenario was written down every word in detail and a pretraining of outcome measurement to researchers was carried out in advance.
CONCLUSIONS
Automated external defibrillator delivery time could be shortened by our newly developed smartphone application for the bystanders to ask nearby responders to find and bring an AED to the cardiac arrest scene.
ACKNOWLEDGMENTS
The authors thank Mie Imanaka and Chisako Naito for their contribution in recruitments of bystanders and responders. The authors also thank Miyuki Yazawa, Noriko Furuita, and Masaru Funagoshi at Kyoto University and Shunsuke Saito at Osaka Medical College for collecting data. The authors are also deeply indebted to all of the bystanders and responders in this study for their indispensable cooperation and support.
Footnotes
The authors declare no conflict of interest.
Coaido, Inc, which developed this new smartphone application, provided a small fund to carry out this trial, but all authors did not receive any personal wages or other benefits from it. Coaido, Inc, had no role in study design, data collection, data analysis, data interpretation, and article writing.
REFERENCES
- 1.Nolan JP, Hazinski MF, Aickin R, et al. Part1: executive summary 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2015;95:e1–e31. [DOI] [PubMed] [Google Scholar]
- 2.Monsieurs KG, Nolan JP, Bossaert LL, et al. European resuscitation council guidelines for resuscitation 2015: section 1. executive summary. Resuscitation 2015;95:1–80. [DOI] [PubMed] [Google Scholar]
- 3.Neumar RW, Shuster M, Callaway CW, et al. Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S315–S367. [DOI] [PubMed] [Google Scholar]
- 4.Chung SP, Sakamoto T, Lim SH, et al. The 2015 Resuscitation Council of Asia (RCA) guidelines on adult basic life support for lay rescuers. Resuscitation 2016;105:145–148. [DOI] [PubMed] [Google Scholar]
- 5.Japan Resuscitation Council, Japan Resuscitation Council. 2015 Japanese Guidelines for Emergency Care and Cardiopulmonary Resuscitation. Tokyo: Igaku shoin; 2016. [Google Scholar]
- 6.Cummins RO, Ornato JP, Thies WH, et al. Improving survival from sudden cardiac arrest: the “chain of survival” concept. A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation 1991;83:1832–1847. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura T, Iwami T, Kawamura T, et al. Nationwide public-access defibrillation in Japan. N Engl J Med 2010;362:994–1004. [DOI] [PubMed] [Google Scholar]
- 8.Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2307–2315. [DOI] [PubMed] [Google Scholar]
- 9.Iwami T, Kitamura T, Kiyohara K, et al. Dissemination of chest compression–only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation 2015;132:415–422. [DOI] [PubMed] [Google Scholar]
- 10.Nakahara S, Tomio J, Ichikawa M, et al. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA 2015;314:247–254. [DOI] [PubMed] [Google Scholar]
- 11.Iwami T, Nichol G, Hiraide A, et al. Continuous improvements in “chain of survival” increased survival after out-of-hospital cardiac arrests a large-scale population-based study. Circulation 2009;119:728–734. [DOI] [PubMed] [Google Scholar]
- 12.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2015;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 13.Reports from Fire and Disaster Management Agency of Japan 2016 (in Japanese). Available at: http://www.fdma.go.jp/neuter/topics/kyukyukyujo_genkyo/h28/01_kyukyu.pdf. Accessed December 23, 2016.
- 14.Japan Heart Foundation website about report on a study on social system development to improve survival from emergency cardiovascular disease using automated external defibrillator, 2015 (in Japanese). Available at: http://www.jhf.or.jp/aed/spread.html. Accessed December 14, 2016.
- 15.Kitamura T, Kiyohara K, Sakai T, et al. Public-access defibrillation and out-of- hospital cardiac arrest in Japan. N Engl J Med 2016;375:1649–1659. [DOI] [PubMed] [Google Scholar]
- 16.Finn JC, Bhanji F, Lockey A, et al. Part 8: education, implementation, and teams 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2015;95:e203–e224. [DOI] [PubMed] [Google Scholar]
- 17.Ringh M, Rosenqvist M, Hollenberg J, et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2316–2325. [DOI] [PubMed] [Google Scholar]
- 18.The reports from Japan Sport Agency, 2016. Available at: http://www.mext.go.jp/sports/b_menu/toukei/chousa04/tairyoku/kekka/k_detail/1396900.htm. Accessed November 22, 2017.
- 19.WMA Declaration of Helsinki - ethical principles for medical research involving human subjects. Available at: http://www.wma.net/en/30publications/10policies/b3/index.html. Accessed December 14, 2016. [PubMed]
- 20.Ethical Guidelines for epidemiological research of Japan. Available at: https://www.niph.go.jp/wadai/ekigakurinri/guidelines.pdf. Accessed December 14, 2016.
- 21.Sakai T, Iwami T, Kitamura T, et al. Effectiveness of the new “Mobile AED Map” to find and retrieve an AED: a randomised controlled trial. Resuscitation 2011;82:69–73. [DOI] [PubMed] [Google Scholar]
- 22.Scholten AC, van Manen JG, van der Worp WE, et al. Early cardiopulmonary resuscitation and use of automated external defibrillators by laypersons in out-of-hospital cardiac arrest using an SMS alert service. Resuscitation 2011;82:1273–1278. [DOI] [PubMed] [Google Scholar]
- 23.Zijlstra JA, Stieglis R, Riedijk F, et al. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation 2014;85:1444–1449. [DOI] [PubMed] [Google Scholar]
- 24.Brooks SC, Simmons G, Worthington H, et al. The Pulse Point Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation 2016;98:20–26. [DOI] [PubMed] [Google Scholar]
- 25.Rea T, Blackwood J, Damon S, et al. A link between emergency dispatch and public access AEDs: Potential implications for early defibrillation. Resuscitation 2011;82:995–998. [DOI] [PubMed] [Google Scholar]
- 26.Sakai T, Kitamura T, Nishiyama C, et al. Cardiopulmonary resuscitation support application on a smartphone—randomized controlled trial. Circ J 2015;79:1052–1057. [DOI] [PubMed] [Google Scholar]
- 27.Caputo ML, Muschietti S, Burkart R, et al. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: a comparison with SMS-based system notification. Resuscitation 2017;114:73–78. [DOI] [PubMed] [Google Scholar]


