Abstract
Background
Additive manufacturing (AM) has emerged as a serious planning, strategy, and education tool in cardiovascular medicine. This review describes and illustrates the application, development and associated limitation of additive manufacturing in the field of cardiology by studying research papers on AM in medicine/cardiology.
Methods
Relevant research papers till August 2018 were identified through Scopus and examined for strength, benefits, limitation, contribution and future potential of AM. With the help of the existing literature & bibliometric analysis, different applications of AM in cardiology are investigated.
Results
AM creates an accurate three-dimensional anatomical model to explain, understand and prepare for complex medical procedures. A prior study of patient’s 3D heart model can help doctors understand the anatomy of the individual patient, which may also be used create training modules for institutions and surgeons for medical training.
Conclusion
AM has the potential to be of immense help to the cardiologists and cardiac surgeons for intervention and surgical planning, monitoring and analysis. Additive manufacturing creates a 3D model of the heart of a specific patient in lesser time and cost. This technology is used to create and analyse 3D model before starting actual surgery on the patient. It can improve the treatment outcomes for patients, besides saving their lives. Paper summarised additive manufacturing applications particularly in the area of cardiology, especially manufacturing of a patient-specific artificial heart or its component. Model printed by this technology reduces risk, improves the quality of diagnosis and preoperative planning and also enhanced team communication. In cardiology, patient data of heart varies from patient to patient, so AM technologies efficiently produce 3D models, through converting the predesigned virtual model into a tangible object. Companies explore additive manufacturing for commercial medical applications.
Keywords: 3D printing, 3D scanning, Additive manufacturing, Artificial heart, Cardiology
1. Introduction
Regarding diseases, one of the biggest killers is cardiovascular disease, and millions of people required help in the issue of cardiovascular every year. Additive manufacturing helps to provide a better quality of life and speedy recovery of these patients.1, 2 It is an emerging and crucial adjunctive tool which can help cardiologists and cardiac surgeons for intervention and surgical planning, monitoring and analysis. Current applications of this technology are in device innovation, teaching tools, procedural planning and functional flow models.3, 4, 5
Additive manufacturing technologies are used to print 3D physical object from 3D digital file. A virtual design file is created from the CAD file using 3D modelling program/scanner or other scanning technologies like computed tomography (CT), magnetic resonance imaging (MRI). Further, Data is converted into a 3D physical model by using various AM technologies. The print material creates 3D model layer by layer, and this process is also called rapid prototyping.6, 7, 8
3D printed model has a unique purpose which allows the surgeon to envision and practice preoperatively. At all level of skill and experience, it is meaningful to surgeons depending on the specific circumstance. Imaging of the patient is done by using various scanning technologies that create the virtual 3D model and then importing the image file in a standard triangulate language (STL) format. The customised heart model is printed quickly by using various AM technologies which can be used further for clinical translation.9, 10 First, we make image acquisition and then go for virtual reconstruction and manufacturing.11, 12
For preoperative evaluation, it is a promising tool that helps in medical education and hemodynamic simulation. It increases operative success and reduces operative risk. The decision of 3D cardiac model seems arbitrary because in interventional procedure cardiologist's perception can be different. In future practical clinical trials are possible by using AM in cardiovascular diseases treatment.13, 14
Additive manufacturing has been revolutionising cardiovascular surgery, as in the new study taken by Texas A&M University; it combines Virtual reality (VR), high-resolution CT scan, vascular robotics systems and 3D printing for proper implementation in cardiology. This technology is used to provide a better standard of care and saves money. It supports treatment and creates holistic treatment plans.15, 16
In patient-specific anatomies, it is used to evaluate stent placement. 3D printed models have some advantages over conventional platforms. In printing methods and materials; there is a rapid pace of advancement of principal drivers in the development.17, 18
Additive manufacturing helps in creating a 3D model of the heart of a specific patient. Now treating doctor can understand the pathology and anatomic variations better which may be encountered during actual surgery or intervention. The scientists have manufactured an artificial heart which is made up of silicone, and it almost beats like a human heart but with a limited life. The step is closer to the replacement of a damaged human heart, and there will be no requirement of transplant. In worldwide, about 26 million people are suffering from heart failure, and there is a shortage of donors. Additive manufacturing technologies make custom artificial hearts that can solve the long-term problem.19
In cardiology, it is difficult to predict the outcome of heart valve replacement for cardiovascular surgical procedures. There are four valves in the heart which are responsible for maintaining the unidirectional blood flow during opening and closing depending upon the pressure difference on each side. The entry of blood flow from atria to ventricles by two atrioventricular (AV) valves (tricuspid and mitral) and the two semilunar (SL) valves (pulmonary and aortic) are present in arteries leaving the heart.20 Precise information about these valves is required. Through the applications of AM, it accurately communicates information about the status of the heart/valves and helps in several improvements.7, 21, 22
Thus, Additive manufacturing is used to improve patient-specific surgical planning with the help of data captured by CT and MRI. This technology saves time, improves surgical accuracy and outcomes. During complex surgical cases, model printed by this technology is helpful for the surgical team, teaching surgery practices and demonstration. For complex congenital heart disease, surgical planning is challenging due to the high variability of patients. It better understands the anatomical structures of the patient heart. It is a powerful tool before performing complicated surgery and interventions that play an important role in day-to-day clinical care.23, 24, 25
2. Need for the study
In today's globalised world, every industry needs customisation and innovation in products and services. In this study, we analyse and describe how the surgeon and patient can benefit by implementing this technology in the management of cardiovascular diseases. It has opened a new path to improve the golden hands of a heart surgeon. AM gives an idea about stabilising heart muscle during operation, short development time and care for the patient. It provides a good co-operation between surgeon and suture. This technology provides a possibility of physical manipulation of the cardiac model in vitro which improves safety and may reduce operating time for complex cardiac surgeries. It provides knowledge of customised cardiac valves and helps its printing using biological/adaptable materials. Doctors can check the status of an outer and inner layer of the heart wall and quickly determines the health of the heart. The study provides awareness to cardiology surgeon about preoperative evaluation, hemodynamic simulation and development of tools/devices. Heart operation becomes safer and faster.
3. Benefits of using additive manufacturing in cardiology
AM is used to design and print a customised heart. From a digital file, it directly fabricates graspable objects. The various benefits of AM for cardiologists are as follows:
-
I.
Tangible heart model and its components are easily printed by AM technologies that are useful for the patient to review the heart and vessel anatomy.
-
II.
For a complicated case, the benefit of 3D printed model is to see the anatomy of the heart from different angles and understand the anatomical positions of the vessels.
-
III.
For explaining the planned procedure to patients, the anatomical 3D model is also beneficial to understand much better during invention that what will happen.
-
IV.
In teaching, the 3D printed model becomes more accessible to explain. They can touch and turn it around. It is a most important educational tool because it gives more information as compared to 2D or 3D images on a screen.
-
V.
3D printed model is also beneficial for pre-surgical training which saves lives, improving outcomes and offering new treatments.
4. Research status
4.1. Research status of additive manufacturing in cardiology
Search using the keyword as “additive manufacturing” “cardiology”, identified only six published articles. Three articles of 2017 and again three articles till August 2018 are published. Different Journals Academic radiology, Annals of biomedical engineering, International journal on interactive design and manufacturing, Journal of biomechanics, Netherlands heart Journal, Trends in biotechnology published one article each. Engineering and medical fields have an equal contribution of 30%. Biology field contributes 20%, chemical engineering contributes 10%, and Mathematics field again have the equal contribution of 10%. Additive manufacturing employs different 3D printing technologies to accomplish different types of requirements.
4.2. Research status of 3D printing in cardiology
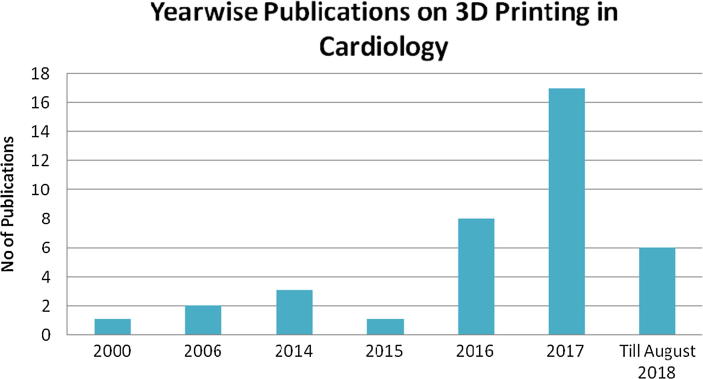
In Cardiology, application of 3D printing is proliferating and is subject of intense research. We explored the research material using Scopus on the use of 3D printing in cardiology. Around 38 research articles were identified by searching keywords as “3D printing” “cardiology”. The first article was published in 2000. Again, after a long gap, three articles were published in 2014, In the year 2015, one article published, and there is an increment of research publications in 2016 where eight articles are published. Sixteen articles published in 2017 and till August 2018, six articles were published in this ongoing year as shown in Fig. 1.
Fig. 1.
3D printing in cardiology: Year wise publication (Source: Scopus).
JACC cardiovascular imaging journal has highest publications of two articles and rests various other journals published one research articles by each.
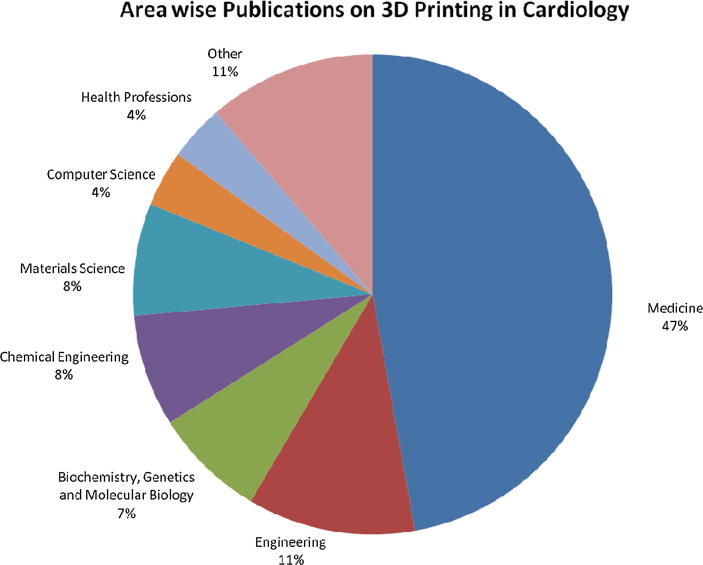
Fig. 2 shows the area wise research on additive manufacturing in cardiology, and we found that the field of medicine has a significant contribution in this area which is 47%. Engineering contributes 11%, Biochemistry, Genetics and Molecular Biology contribute 7%, chemical engineering and materials science 8% contribution by each field, Again Computer science and health professions have an equal contribution of 4% by each field. Other fields also have 11% of the contribution, and this includes physics and astronomy, social sciences, chemistry and mathematics.
Fig. 2.
3D printing in cardiology: Area wise contribution (Source: Scopus).
As evident through Scopus, this technology seems to have broad applications in the medical field, and the same is also helping in the specific area of cardiology.
5. Steps of Additive manufacturing towards its adoption
AM uses a 3D computer model to create a 3D physical model by adding layer by layer of material. Medical AM uses a 3D medical image to create solid replicas of patient heart/its parts. Significant steps used by AM in cardiology as discussed in Table 1:
Table 1.
Steps of Additive Manufacturing toward making heart/its parts.
| S No | Steps | Description | Benefits | References |
|---|---|---|---|---|
| 1 | Image acquisition |
|
|
Gómez-Ciriza, et al.26, Giannopoulos et al.27, Ripley et al.28 |
| 2 | Segmentation |
|
|
Dankowski et al.29, Mosadegh et al.30 |
| 3 | Computer-aided design |
|
|
Hu et al.21, Haleem and Javaid31, Jacobs et al.32 |
| 4 | Rapid prototyping (3D printing) |
|
|
Schrot et al.33, Ngan et al.34, Birbara et al.35, Farooqi and Mahmood36, Javaid and Haleem37 |
| 5 | Clinical translation |
|
|
Campbell and Weiss38, Hadeed et al.39 |
Additive manufacturing is at the crossroads of CAD, non-invasive diagnostic imaging, structural heart intervention, printer and materials engineering. Cardiovascular applications of additive manufacturing development include the use of patient-specific 3D models for exploration of the valve, vessel function, surgical and catheter-based procedural planning.40, 41 3D printed model is manufactured from various imaging that provides a direct manipulation, haptic feedback to enhance the understanding of underlying pathologies and cardiovascular anatomies. 3D printed heart/valves help surgeon for patient counselling. In heart surgery when valves replacement does not fit properly, the 3D printed model allows the surgeon to test for fit. Now the surgeon can practice the procedure to achieve successful operation.
6. Criteria’s for adopting when using Additive manufacturing for the production of an artificial heart/components
In the current scenario, a 3D artificial heart model can be quite helpful for a cardiologist. Edition of scanned data is done according to the required shape and dimensions, and finally, one can obtain a printed model. This printed model is gainfully used towards solving the complex surgical problem and fulfils the deficiencies of the cardiology area with lesser time and cost. Table 2 discusses various criteria's regarding the printing of the heart or its components with its achievements and limitations. These issues can be taken up by using additive manufacturing in the printing of an artificial heart.
Table 2.
Criteria’s in using AM for the production of artificial heart/components.
| S No | Criteria | Achievements | Limitation | References |
|---|---|---|---|---|
| 1 | Ease of design |
|
|
Cheng et al.42, Zhang and Joshi43, Olivier et al.44 |
| 2 | Material |
|
|
Cunico and Carvalho45, Fahad et al.46 |
| 3 | Colour |
|
|
Chromy and Zalud47, Dahake et al.48 |
| 4 | Efficiency |
|
|
Gibson et al.49, Rengier et al.50, Salmi et al.51 |
| 5 | Speed |
|
|
Swann52, Tukuru et al.53, O'Malley et al.54, Schievano et al.55 |
| 6 | Model Dimensions |
|
|
Negi et al.56, Vaezi et al.57, Wang et al.58 |
| 7 | Cost |
|
|
Yap et al.59; Zhang et al.60, Melchels et al.61, Tuomi et al.62 |
| 8 | Accuracy |
|
|
Arrieta et al.63, Balazic and Kopac64, Mallepree and Bergers65, Kernan and Wimsatt66 |
| 9 | Ease of use |
|
|
Chimento et al.67, Hieu et al.68, Salmi et al.69 |
| 10 | Simulation before or after medication |
|
|
Pandit et al.70, Chiumenti et al.71 |
For design and development of a heart model, additive manufacturing is a useful tool which provides a better understanding of patient to the surgeon. A model can be well designed using scanning devices/supporting software which is ease of use and improved efficiency/accuracy. Heart model shows real understanding regarding actual pathology in the heart/associated body components. This knowledge can help in reduced time spent on invasive surgery and develops a clear communication among the surgical team members. Thus, a printed model can allow cardiologists learn about the problem on the structure of hearts and deliver better treatment.
7. Types of applications of additive manufacturing in cardiology
In many cases, there is a requirement of customised 3D heart model of the patient. AM fulfils this requirement at an economical price. This novel technology is also medically used in various areas of medicine like maxillofacial and orthopaedic surgery that helps to reduce surgical time. In cardiology, surgeons can study and practice their hands on the 3D printed patient anatomy. Thus, AM has various applications in interventional structural heart disease as discussed in Table 3.
Table 3.
Different types of applications of AM in the area of cardiology.
| S No | Clinical Applications | Description | References |
|---|---|---|---|
| 1 | Aortic pathology |
|
Gosnell et al.72, Wolf et al.73 |
| 2 | Atrial septal defect closure |
|
Mathur et al.74; Perez-Arjona75 |
| 3 | Stent angioplasty in pulmonary venous baffle obstruction |
|
Gosnell et al.72; Shiraishi et al.76, Dickinson et al.77 |
| 4 | Percutaneous mitral annuloplasty |
|
Sodian et al.78, Noecker et al.79, Pellegrino et al.80 |
| 5 | Pulmonary valve implantation |
|
Kim et al.81, Sodian et al.82 |
| 6 | Transcatheter aortic valve implantation |
|
Otton et al.83, Kiraly et al.84 |
| 7 | Structural interventional cardiology training |
|
Farooqi et al.85, Costello et al.15 |
| 8 | Teaching tools |
|
Torres et al.86, Javaid and Haleem87 |
| 9 | Procedural planning |
|
Jacobs et al.32, Shiraishi et al.88, Schmauss et al.89 |
| 10 | Functional flow models |
|
Sacks et al.20, Vukicevic et al.23 |
| 11 | Device innovation |
|
Lazkani et al.90, Green et al.91, Olivieri et al.92 |
| 12 | Treatment of arrhythmia |
|
Miller93, Farooqi et al.36 |
Doctors can use a 3D heart model to guide a tricky heart valve replacement. This technology helps simulate the procedure and rapid development of new medical tools/devices that are helpful for individual patients. Heart model allows preoperative simulation of a specific patient. It holds educational promise for a high-risk operation which was a challenge to teach. 3D printed models are rigid, semi-rigid, single- colour and having multi-colour that easily fulfils the needs of the clinical team. We can section a heart in any plane and can rotate in all axes on screen. By using AM technology, we can see heart precisely and analyse it before an interventional procedure/actual surgery.94, 95 Patient 3D heart models can be stored in a follow-up appointment/records.96 Surgeons take advantages of additive manufacturing technologies to solve complex medical problems due to its flexibilities of design and manufacturing.
8. Major finding through the study
Additive Manufacturing provides a useful contribution in the area of cardiology, starting from imaging to clinical translation, it has a useful role, and the same is presented below:
-
i.
Research on applications of this technology in cardiology is increasing; Search of the literature showed that medicine is the most common field where research on AM is rapidly progressing.
-
ii.
AM helps converting a predesigned virtual model into a physical object and acts as an efficient, supportive tool for medical education that reduces operative risk.
-
iii.
Additive manufacturing follows five steps in cardiology by its application, i.e. image acquisition, segmentation, computer-aided design, rapid prototyping and clinical translation to create an artificial 3D heart.
-
iv.
3D printed model provides excellent communication between patient and health professionals. The patient can understand the illness better and take a more informed and empowered decision.
-
v.
AM helps provide a walk-through planning tool to the cardiac surgeon before complicated surgery that can make the procedure safer and faster.
-
vi.
AM helps the surgeons to create a customised action plan which gives an idea of what to expect by studying patient's accurate replica of cardiovascular tissue.
-
vii.
AM can potentially help in designing an artificial heart that will closely resemble the human heart. It is at a nascent stage and requires innovation in medical tools/ devices to fabricate customised artificial heart rapidly.
-
viii.
Additive manufacturing has various applications in Aortic pathology, Atrial septal defect closure, proper patients for pulmonary valve implantation, procedural planning, teaching tool and device innovation.
-
ix.
Due to various attributes of AM such as design, colour, efficiency, speed, cost and accuracy, it has the potential to revolutionise the practice of cardiac intervention and surgery.
9. Limitations and future directions
AM provides less tangible benefits in specific areas. It does not provide information about blood loss, blood clot; chest wound infection, and metabolic abnormalities. Before the printed 3D model, an accurate and precise medical image is required. The technology involves cost and time in addition to the standard care of patients.
However, the future growth of technology will overcome present-day challenges. AM has the potential for congenital heart disease and simulation of structural interventions. In the broadest sense, it will enhance multidisciplinary collaboration involving clinical cardiologists, radiologists, cardiac catheterisation specialists, and surgeons. AM may become a ubiquitous and essential tool to fabricate customised implantable medical devices that improve existing therapeutic interventions. In future, these 3D printing technologies could print a 3D heart model by using smart materials which can change their shape and functionalities concerning time. These are called 4D printing technologies. These technologies can easily print heart, kidney and liver by the input of smart material with high flexibility with perfect fit and matches genetically. These models can grow in the patient body as per patient growth. It could also manufacture smart cardiac tube that can grow in patient body with the help of body heat concerning time. This new rapidly growing technology can well be used in continuous quality control, perform precise surgery and expands frontiers of modern medicine.
10. Conclusion
Additive manufacturing is emerging as an important tool in the field of medicine especially cardiology. It easily fabricates a three-dimensional physical model of the heart of a specific patient in a short time, using various specialised technologies from previously acquired scanned virtual image. Three-dimensional scanned images created by CT and MRI can be examined in the form of a realistic and tangible object. This can be used to examine the complexity of diseased anatomy in a given patient. This technology easily fulfils various requirements of cardiology due to its flexibility in design and manufacturing of specific patient 3D models. Research in this field is continuously increasing and will take over various challenges which were not previously possible by other conventional manufacturing technologies. It has the potential to be of immense help to the cardiologists and cardiac surgeons for intervention and surgical planning, monitoring and analysis. A prior study of the patient's heart model can lead to better pre-procedure planning, enhanced team communication, and improved outcomes. In future, these technologies can use the smart material as input and could take over the challenge of heart replacement of patient and save millions of lives. The paper summarised additive manufacturing applications particularly in cardiology, especially manufacturing of a patient-specific model of heart or its components.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Egyptian Society of Cardiology.
Contributor Information
Abid Haleem, Email: ahaleem@jmi.ac.in.
Mohd Javaid, Email: mjavaid@jmi.ac.in.
Anil Saxena, Email: anil.saxena@hotmail.com.
References
- 1.Yang D.H., Kang J.W., Kim N., Song J.K., Lee J.W., Lim L.H. Myocardial 3-dimensional printing for septal myectomy guidance in a patient with obstructive hypertrophic cardiomyopathy. Circulation. 2015;132:300–301. doi: 10.1161/CIRCULATIONAHA.115.015842. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto J.S., Morris J.M., Foley T.A. Three-dimensional physical modeling: applications and experience at Mayo Clinic. Radiographics. 2015;35:1989–2006. doi: 10.1148/rg.2015140260. [DOI] [PubMed] [Google Scholar]
- 3.Giannopoulos A.A., Steigner M.L., George E. Cardiothoracic applications of 3-dimensional printing. J Thorac Imaging. 2016;31:253–272. doi: 10.1097/RTI.0000000000000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meier L.M., Meineri M., Hiansen J.Q., Horlick E.M. Structural and congenital heart disease interventions: the role of three-dimensional printing. Neth Heart J. 2017;25:65–75. doi: 10.1007/s12471-016-0942-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olivieri L.J., Su L., Hynes C.F. DS7. “Just-in-time” simulation training using 3D printed cardiac models after congenital cardiac surgery. World J Pediatr Congenit Heart Surg. 2016;7:164–168. doi: 10.1177/2150135115623961. [DOI] [PubMed] [Google Scholar]
- 6.Markert M., Weber S., Lueth T.C. A beating heart model 3D printed from specific patient data. Conf Proc IEEE Eng Med Biol Soc. 2007;4472–4475 doi: 10.1109/IEMBS.2007.4353332. [DOI] [PubMed] [Google Scholar]
- 7.Witschey W.R., Pouch A.M., McGarvey J.R. Three-dimensional ultrasound-derived physical mitral valve modelling. Ann Thorac Surg. 2014;98:691–694. doi: 10.1016/j.athoracsur.2014.04.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valverde I. Three-dimensionalprinted cardiac models: applications in the field of medical education, cardiovascular surgery, and structural heart interventions. Rev EspCardiol. 2017 doi: 10.1016/j.rec.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Weber S., Sodian R., Markert M., Reichart B., Daebritz S., Lueth T.C. 3D printing of anatomical heart models for surgical planning in cardiac surgery. Int J CARS. 2007;2:171–173. [Google Scholar]
- 10.Riesenkampff E., Rietdorf U., Wolf I. The practical clinical value of three-dimensional models of complicated congenitally malformed hearts. J Thorac Cardiovasc Surg. 2009;138:571–580. doi: 10.1016/j.jtcvs.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 11.Greil G.F., Wolf I., Kuettner A. Stereolithographic reproduction of complex cardiac morphology based on high spatial resolution imaging. Clin Res Cardiol. 2007;96:176–185. doi: 10.1007/s00392-007-0482-3. [DOI] [PubMed] [Google Scholar]
- 12.Kurup H.K., Samuel B.P., Vettukattil J.J. Hybrid 3D printing: a game-changer in personalized cardiac medicine? Expert Rev Cardiovasc Ther. 2015;13:1281–1284. doi: 10.1586/14779072.2015.1100076. [DOI] [PubMed] [Google Scholar]
- 13.Javaid M., Haleem A. Additive manufacturing applications in medical cases: a literature-based review. Alexandria J Med. 2017 [Google Scholar]
- 14.Mahmood F., Owais K., Taylor C. Three-dimensional printing of mitral valve using echocardiographic data. JACC Cardiovasc Imaging. 2015;8:227–229. doi: 10.1016/j.jcmg.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Costello J.P., Olivieri L.J., Su L. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit Heart Disease. 2015;10:185–190. doi: 10.1111/chd.12238. [DOI] [PubMed] [Google Scholar]
- 16.Schmauss D., Haeberle S., Hagl C., Sodian R. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-centre experience. Eur J Cardiothorac Surg. 2015;47:1044–1052. doi: 10.1093/ejcts/ezu310. [DOI] [PubMed] [Google Scholar]
- 17.Biglino G., Capelli C., Koniordou D. Use of 3D models of congenital heart disease as an education tool for cardiac nurses. Congenit Heart Dis. 2017;12:113–118. doi: 10.1111/chd.12414. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino P.L., Fassini G., Di Biase M., Tondo C. Left atrial appendage closure guided by 3D printed cardiac reconstruction: emerging directions and future trends. J Cardiovasc Electrophysiol. 2016;27:768–771. doi: 10.1111/jce.12960. [DOI] [PubMed] [Google Scholar]
- 19.Tanner C. Is the end of donor transplants in sight? Scientists create a 3D-printed silicone artificial heart that beats like the real organ. Mail online. 2017 [Google Scholar]
- 20.Sacks M.S., Yoganathan A.P. Heart valve function: a biomechanical perspective. Phil Trans Roy Soc B: Biol Sci. 2007;362:1369–2139. doi: 10.1098/rstb.2007.2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu A., Wilson T., Ladak H., Haase P., Fung K. Three-dimensional educational computer model of the larynx: voicing a new direction. Arch Otolaryngol Head Neck Surg. Am Med Assoc. 2009;135:677–681. doi: 10.1001/archoto.2009.68. [DOI] [PubMed] [Google Scholar]
- 22.Moore T., Madriago E.J., Renteria E.S. Co-registration of 3D echo and MR data to create physical models of congenital heart malformations. J Cardiovasc Magn Reson. 2015;17 198. [Google Scholar]
- 23.Vukicevic M., Mosadegh B., Min J.K., Little S.H. Cardiac 3D printing and its future directions. JACC Cardiovasc Imaging. 2017;10:171–184. doi: 10.1016/j.jcmg.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ballard D.H., Trace A.P., Ali S. Clinical applications of 3D printing: primer for radiologists. Acad Radiol. 2018;25:52–65. doi: 10.1016/j.acra.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riccardo F., Marco G., Aurelio C. 3D printing of the aortic annulus based on cardiovascular computed tomography: preliminary experience in pre-procedural planning for aortic valve sizing. J Cardiovasc Comp Tomogr. 2018 doi: 10.1016/j.jcct.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 26.Gómez-Ciriza G., Hussain T., Gómez-Cía T., Valverde I. Potential of 3D-printed models in planning structural interventional procedures. Inter Cardiol. 2015;7:1–5. [Google Scholar]
- 27.Giannopoulos A.A., Mitsouras D., Yoo S.J., Liu P.P., Chatzizisis Y.S., Rybicki F.J. Applications of 3D printing in cardiovascular diseases. Nat Rev Cardiol. 2016;13:701–718. doi: 10.1038/nrcardio.2016.170. [DOI] [PubMed] [Google Scholar]
- 28.Ripley B., Kelil T., Cheezum M.K. 3D printing based on cardiac CT assists anatomic visualization before transcatheter aortic valve replacement. J Cardiovasc Comput Tomogr. 2015 doi: 10.1016/j.jcct.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dankowski R., Baszko A., Sutherland M. 3D heart model printing for preparation of percutaneous structural interventions: description of the technology and case report. Kardiol Pol. 2014;72(6):546–551. doi: 10.5603/KP.2014.0119. [DOI] [PubMed] [Google Scholar]
- 30.Mosadegh B., Xiong G., Dunham S., Min J.K. Current progress in 3D printing for cardiovascular tissue engineering. Biomed Mater. 2015 doi: 10.1088/1748-6041/10/3/034002. 10. 10.1088/1748-6041/10/3/034002. [DOI] [PubMed] [Google Scholar]
- 31.Haleem A., Javaid M. 3D scanning applications in medical field: a literature-based review. Clin Epidemiol Global Health. 2018 [Google Scholar]
- 32.Jacobs S., Grunert R., Mohr F.W., Falk V. 3D-Imaging of cardiac structures using 3D heart models for planning in heart surgery: a preliminary study. Interact Cardiovasc Thorac Surg. 2008;7:6–9. doi: 10.1510/icvts.2007.156588. [DOI] [PubMed] [Google Scholar]
- 33.Schrot J., Pietila T., Sahu A. State of the art: 3D printing for creating compliant patient-specific congenital heart defect models. J Cardiovasc Magn Reson. 2014;16(Suppl. 1):W19. [Google Scholar]
- 34.Ngan E.M., Rebeyka I.M., Ross D.B. The rapid prototyping of anatomic models in pulmonary atresia. J Thorac Cardiovasc Surg. 2006;132:264–269. doi: 10.1016/j.jtcvs.2006.02.047. [DOI] [PubMed] [Google Scholar]
- 35.Birbara N.S., Otton J.M., Pather N. 3D modelling and printing technology to 3 produce patient-specific 3D models. Heart Lung Circulation. 2017 doi: 10.1016/j.hlc.2017.10.017. [DOI] [PubMed] [Google Scholar]
- 36.Farooqi K.M., Saeed O., Zaidi A. 3D printing to guide ventricular assist device placement in adults with congenital heart disease and heart failure. JACC Heart Fail. 2016;4:301–311. doi: 10.1016/j.jchf.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 37.Javaid M., Haleem A. Additive manufacturing applications in orthopaedics: a review. J Clin Orthopaed Trauma. 2018 doi: 10.1016/j.jcot.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Campbell P.G., Weiss L.E. Tissue engineering with the aid of inkjet printers. Expert Opin Biol Ther. 2007;7:1123–1127. doi: 10.1517/14712598.7.8.1123. [DOI] [PubMed] [Google Scholar]
- 39.Hadeed K., Acar P., Dulac Y., Cuttone F., Alacoque X., Karsenty C. Cardiac 3D printing for better understanding of congenital heart disease. Arch Cardiovasc Disease. 2018;111:1–4. doi: 10.1016/j.acvd.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Schaffer M. Springer; London: 2013. Spectrum of congenital cardiac defects. Pediatric and congenital cardiology, cardiac surgery and intensive care; pp. 1419–11123. [Google Scholar]
- 41.Singhal A.J., Shetty V., Bhagavan K.R. Improved surgery planning using 3-D printing: a case study. Indian J Surg. 2015 doi: 10.1007/s12262-015-1326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng L., Zhang P., Biyikli E., Bai J., Robbins J., To A. Efficient design optimization of variable-density cellular structures for additive manufacturing: theory and experimental validation. Rapid Prototyping J. 2017;23:660–677. [Google Scholar]
- 43.Zhang G., Tsou Y., Rosenberger A.L. Reconstruction of the Homunculus skull using a combined scanning and stereolithography process. Rapid Prototyping J. 2000;6:267–275. [Google Scholar]
- 44.Olivier D., Borros S., Reyes G. Application-driven methodology for new additive manufacturing materials development. Rapid Prototyping J. 2014;20:50–58. [Google Scholar]
- 45.Cunico M.W.M., Carvalho J.D. Development of acrylate-based material using a multivariable approach: additive manufacturing applications. Rapid Prototyping J. 2014;20:121–132. [Google Scholar]
- 46.Fahad M., Dickens P., Gilbert M. Novel polymeric support materials for jetting based additive manufacturing processes. Rapid Prototyping J. 2013;19:230–239. [Google Scholar]
- 47.Chromy A., Zalud L. Robotic 3D scanner as an alternative to standard modalities of medical imaging. Springer Plus. 2014;3:1–10. doi: 10.1186/2193-1801-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dahake S.W., Kuthe A.K.M., Mawale M.B., Bagde A.D. Applications of medical rapid prototyping assisted customized surgical guides in complex surgeries. Rapid Prototyping J. 2016;22:934–946. [Google Scholar]
- 49.Gibson I., Cheung L.K., Chow S.P. The use of rapid prototyping to assist medical applications. Rapid Prototyping J. 2006;12:53–58. [Google Scholar]
- 50.Rengier F., Mehndiratta A., Von Tengg-Kobligk H. 3D printing based on imaging data: a review of medical applications. Int J Comput Assist Radiol Surg. 2010;5:335–341. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 51.Salmi M., Paloheimo K.S., Tuomi J., Wolff J., Mäkitie A. Accuracy of medical models made by additive manufacturing (rapid manufacturing) J Cranio-Maxillofacial Surg. 2013;41:603–609. doi: 10.1016/j.jcms.2012.11.041. [DOI] [PubMed] [Google Scholar]
- 52.Swann S. Integration of MRI and stereolithography to build medical models: a case study. Rapid Prototyping J. 1996;2:41–46. [Google Scholar]
- 53.Tukuru N., Gowda S.K.P., Ahmed S.M., Badami S. Rapid prototype technique in medical field. Res J Pharm Technol. 2008;1:341–344. [Google Scholar]
- 54.O'Malley F.L., Millward H., Eggbeer D., Williams R., Cooper R. The use of adenosine triphosphate bioluminescence for assessing the cleanliness of improve materials used in medical applications. Addit Manuf. 2016;9:25–29. [Google Scholar]
- 55.Schievano S., Migliavacca F., Coats L. Percutaneous pulmonary valve implantation based on rapid prototyping of right ventricular outflow tract and pulmonary trunk from MR data. Radiology. 2007;242:490–497. doi: 10.1148/radiol.2422051994. [DOI] [PubMed] [Google Scholar]
- 56.Negi S., Dhiman S., Sharma R.K. Basics and applications of rapid prototyping medical models. Rapid Prototyping J. 2014;20:256–267. [Google Scholar]
- 57.Vaezi M., Chua C.K., Chou S.M. Improving the process of making rapid prototyping models from medical ultrasound images. Rapid Prototyping J. 2012;18:287–298. [Google Scholar]
- 58.Wang C.S., Wang W.H.A., Lin M.C. STL rapid prototyping bio-CAD model for CT medical image segmentation. Comput Ind. 2010;61:187–197. [Google Scholar]
- 59.Yap Y.L., Tan Y.S.E., Tan H.K.J. 3D printed bio-models for medical applications. Rapid Prototyping J. 2017;23:227–235. [Google Scholar]
- 60.Zhang Z., Joshi S. Slice data representation and format for multi-material objects for additive manufacturing processes. Rapid Prototyping J. 2017;23:149–161. [Google Scholar]
- 61.Melchels F.P.W., Feijen J., Grijpma D.W. A review of stereolithography and its applications in biomedical engineering. Biomaterials. 2010;31:6121–6130. doi: 10.1016/j.biomaterials.2010.04.050. [DOI] [PubMed] [Google Scholar]
- 62.Tuomi J., Paloheimo K.S., Vehviläinen J. A novel classification and online platform for planning and documentation of medical applications of additive manufacturing. Surg Innov. 2014;21:553–559. doi: 10.1177/1553350614524838. [DOI] [PubMed] [Google Scholar]
- 63.Arrieta C., Uribe S., GrezJorge R. Quantitative assessments of geometric errors for rapid prototyping in medical applications. Rapid Prototyping J. 2012;18:431–442. [Google Scholar]
- 64.Balazic M., Kopac J. Improvements of medical implants based on modern materials and new technologies. J Achieve Mater Manuf Eng. 2007;25:31–34. [Google Scholar]
- 65.Mallepree T., Bergers D. Accuracy of medical RP models. Rapid Prototyping J. 2009;15:325–332. [Google Scholar]
- 66.Kernan B.T., Wimsatt J.A. Use of a stereolithography model for accurate, preoperative adaptation of a reconstruction plate. J Oral Maxillofac Surg. 2000;58:349–351. doi: 10.1016/s0278-2391(00)90071-5. [DOI] [PubMed] [Google Scholar]
- 67.Chimento J., Highsmith M.J., Crane N. 3D printed tooling for thermoforming of medical devices. Rapid Prototyping J. 2011;17:387–392. [Google Scholar]
- 68.Hieu L.C., Zlatov N., Sloten J.V. Medical rapid prototyping applications and methods. Assembly Autom. 2005;2:284–292. [Google Scholar]
- 69.Salmi M., Tuomi J., PaloheimoKaija S. Patient-specific reconstruction with 3D modelling and DMLS additive manufacturing. Rapid Prototyping J. 2012;18:209–214. [Google Scholar]
- 70.Pandit A., Sekhar R., Revanur R.K. Simulation mechanism development for additive manufacturing. Mater Today: Proc. 2017;4:7270–7278. [Google Scholar]
- 71.Chiumenti M., Lin X., Cervera M., Lei W., Zheng Y., Huang W. Numerical simulation and experimental calibration of additive manufacturing by blown powder technology. Part I: thermal analysis. Rapid Prototyping J. 2017;23:448–463. [Google Scholar]
- 72.Gosnell J., Pietila T., Samuel B.P., Kurup H.K.N., Haw M.P., Vettukattil J.J. Integration of computed tomography and three-dimensional echocardiography for hybrid three-dimensional printing in congenital heart disease. J Digit Imaging. 2016;29:665–669. doi: 10.1007/s10278-016-9879-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wolf I., Boettger T., Rietdorf U. Visualization. Image-Guided Proced Display. 2006;2006(6141):175–183. [Google Scholar]
- 74.Mathur M., Patil P., Bove A. The role of 3D printing in structural heart disease: all that glitters is not gold. JACC Cardiovasc Imaging. 2015;8:987–988. doi: 10.1016/j.jcmg.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 75.Perez-Arjona E., Dujovny M., Park H. Stereolithography: neurosurgical and medical implications. Neurol Res. 2003;25:227–236. doi: 10.1179/016164103101201337. [DOI] [PubMed] [Google Scholar]
- 76.Shiraishi I., Kajiyama Y., Yamagishi M., Hamaoka K. Images in cardiovascular medicine. Stereolithographic biomodelling of congenital heart disease by multislice computed tomography imaging. Circulation. 2006;113:733–734. doi: 10.1161/CIRCULATIONAHA.105.538801. [DOI] [PubMed] [Google Scholar]
- 77.Dickinson K.J., Matsumoto J., Cassivi S.D. Individualizing management of complex oesophagal pathology using three dimensional printed models. Ann Thorac Surg. 2015;100:692–697. doi: 10.1016/j.athoracsur.2015.03.115. [DOI] [PubMed] [Google Scholar]
- 78.Sodian R., Weber S., Markert M. Stereolithographic models for surgical planning in congenital heart surgery. Ann Thorac Surg. 2007;83:1854–1857. doi: 10.1016/j.athoracsur.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 79.Noecker A.M., Chen J.F., Zhou Q. Development of patient-specific three-dimensional pediatric cardiac models. ASAIO J. 2006;52:349–353. doi: 10.1097/01.mat.0000217962.98619.ab. [DOI] [PubMed] [Google Scholar]
- 80.Pellegrino P.L., Fassini G., Biase M.D., Tondo C. Left atrial appendage closure guided by 3D printed cardiac reconstruction: emerging directions and future trends. Tech Technol Innov. 2016 doi: 10.1111/jce.12960. [DOI] [PubMed] [Google Scholar]
- 81.Kim M.S., Hansgen A.R., Wink O., Quaife R.A., Carroll J.D. Rapid prototyping: a new tool in understanding and treating structural heart disease. Circulation. 2008;117:2388–2394. doi: 10.1161/CIRCULATIONAHA.107.740977. [DOI] [PubMed] [Google Scholar]
- 82.Sodian R., Weber S., Markert M. Pediatric cardiac transplantation: three-dimensional printing of anatomic models for surgical planning of heart transplantation in patients with univentricular heart. J Thorac Cardiovasc Surg. 2008;136:1098–1099. doi: 10.1016/j.jtcvs.2008.03.055. [DOI] [PubMed] [Google Scholar]
- 83.Otton J.M., Spina R., Sulas R. Left atrial appendage closure guided by 3D-printed cardiac reconstruction. JACC Cardiovasc Interv. 2015;8:1004–1006. doi: 10.1016/j.jcin.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 84.Kiraly L., Tofeig M., Jha N.K., Talo H. Three-dimensional printed prototypes refine the anatomy of post-modified Norwood-1 complex aortic arch obstruction and allow presurgical simulation of the repair. Interact Cardiovasc Thorac Surg. 2016;22:238–240. doi: 10.1093/icvts/ivv320. [DOI] [PubMed] [Google Scholar]
- 85.Farooqi K.M., Mahmood F. Innovations in preoperative planning: insights into another dimension using 3D printing for cardiac disease. J Cardiothorac Vasc Anesth. 2017 doi: 10.1053/j.jvca.2017.11.037. [DOI] [PubMed] [Google Scholar]
- 86.Torres K., Staskiewicz G., Sniezynski M., Drop A., Maciejewski R. Application of rapid prototyping techniques for modelling of anatomical structures in medical training and education. Folia Morphol. 2011;70:1–4. [PubMed] [Google Scholar]
- 87.Javaid M., Haleem A. Current status and challenges of additive manufacturing in orthopaedics: an overview. J Clin Orthopaed Trauma. 2018 doi: 10.1016/j.jcot.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shiraishi I., Yamagishi M., Hamaoka K., Fukuzawa M., Yagihara T. Simulative operation on congenital heart disease using rubber-like urethane stereolithographic models based on 3D datasets of multislice computed tomography. Eur J Cardiothorac Surg. 2010;37:302–306. doi: 10.1016/j.ejcts.2009.07.046. [DOI] [PubMed] [Google Scholar]
- 89.Schmauss D., Juchem G., Weber S., Gerber N., Hagl C., Sodian R. Three-dimensional printing for perioperative planning of complex aortic arch surgery. Ann Thorac Surg. 2014;97:2160–2163. doi: 10.1016/j.athoracsur.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 90.Lazkani M., Bashir F., Brady K. Postinfarct VSD management using 3D computer printing assisted percutaneous closure. Indian Heart J. 2015;67:581–585. doi: 10.1016/j.ihj.2015.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Green S.M., Klein A.J., Pancholy S. The current state of medical simulation in interventional cardiology: a clinical document from the Society for Cardiovascular Angiography and Intervention’s (SCAI) Simulation Committee. Catheter Cardiovasc Interv. 2013;83:37–46. doi: 10.1002/ccd.25048. [DOI] [PubMed] [Google Scholar]
- 92.Olivieri L.J., Krieger A., Loke Y.H., Nath D.S., Kim P.C., Sable C.A. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Soc Echocardiogr. 2015;28:392–397. doi: 10.1016/j.echo.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 93.Miller B. Washington University in St Louis; 2014. 3-D printer creates transformative device for heart treatment. [Google Scholar]
- 94.Peltola S.M., Melchels F.P., Grijpma D.W., Kellomaki M. A review of rapid prototyping techniques for tissue engineering purposes. Ann Med. 2008;40:268–280. doi: 10.1080/07853890701881788. [DOI] [PubMed] [Google Scholar]
- 95.Vukicevic M., Mosadegh B., Min J.K., Little S.H. Cardiac 3D printing and its future directions. JACC: Cardiovasc Imaging. 2017;10:171–184. doi: 10.1016/j.jcmg.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mashari A., Knio Z., Jeganathan J. Hemodynamic testing of patient-specific mitral valves using a pulse duplicator: a clinical application of three-dimensional printing. J Cardiothorac Vasc Anesth. 2016;30:1278–1285. doi: 10.1053/j.jvca.2016.01.013. [DOI] [PubMed] [Google Scholar]